Abstract
Persons living with HIV/AIDS (PLHA) of color are under-represented in AIDS clinical trials (ACTs), which may limit the generalizability of research findings and denies many individuals access to high levels of care and new treatments available through ACTs. Disproportionately low rates of recruitment in health care settings and by providers are a major barrier to ACTs for this group. Moreover, PLHA of color are more likely than their white peers to decline to participate, mainly due to fear and mistrust (although willingness is also high), negative social norms about ACTs, and difficulty navigating the unfamiliar ACT system. We describe a small number of successful behavioral and structural interventions to increase the participation of PLHA of color in screening for and enrollment into ACTs. HIV care settings, clinical trials sites, and trial sponsors are uniquely positioned to develop procedures, supports, and trials to increase the proportion of PLHA of color in ACTs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Racial/Ethnic Disparities in HIV/AIDS
The HIV epidemic increasingly affects African-American and Latino/Hispanic individuals in the United States. African-Americans make up 13% of the US population, but 48% of prevalent HIV/AIDS cases [1]. Latinos/Hispanics are also over-represented among HIV/AIDS cases: they comprise 12% of the population, but 17% of prevalent HIV/AIDS cases. Moreover, persons living with HIV/AIDS (PLHA) from African-American and Latino racial/ethnic backgrounds, referred to in this article as “PLHA of color,” are more likely to suffer the ill effects of HIV/AIDS than their white peers, including greater morbidity and earlier mortality [2]. Further, racial/ethnic disparities in HIV/AIDS incidence, prevalence, morbidity, and mortality are increasing [1, 3]
Racial/Ethnic Disparities in AIDS Clinical Trials
AIDS clinical trials (ACTs) are research studies to evaluate promising therapies to fight HIV infection, treat the complications of antiretroviral therapy, prevent and treat the opportunistic infections and cancers associated with HIV/AIDS, and reconstitute HIV-damaged immune systems [4]. ACTs are critical to the development of new medications and treatment regimens. Through involvement in ACTs, individuals living with HIV/AIDS can gain access to promising new treatments, and access a level of care and support services that may not otherwise be available to those of limited resources [5]. While Latinos have historically been modestly under-represented in trials [5], the greatest disproportionality is found among African-Americans, who comprise approximately 48% of all PLHA but only 30% of ACT participants [1, 4]. Further, these disparities have not improved over the past two decades [4]. Indeed, the Underrepresented Populations Committee of the Adult AIDS Clinical Trials Group at the National Institute of Allergy and Infectious Diseases has made substantial progress in exposing and reducing ACT disparities [6•, 7]. Yet barriers to ACTs are complex and persistent for PLHA of color, as we describe below.
The Importance of ACTs in the Treatment of HIV/AIDS
The disproportionately low inclusion of PLHA of color in ACTs has been criticized on at least two levels. First, insufficient involvement of PLHA of color may limit the generalizability of research findings to these populations [8, 9]. The disproportionately low representation of PLHA of color has led to concerns about the precision of estimates of clinical efficacy and adverse effects of many therapies for HIV/AIDS and related complications in these populations [9, 10]. For example, patients in clinic settings often fail to achieve the high initial or sustained virologic response to highly active antiretroviral therapy (HAART) typically seen in patients who participate in ACTs [11]. Second, at the level of the individual patient, persons with poor access to ACTs are denied supplementary attention and care available through ACTs as well as access to new treatments and prophylaxis [5, 9, 10, 12, 13]. For some patients, ACTs may represent their best opportunity for life-extending, state-of-the-art therapies, particularly for individuals with poor access to services [9]. In addition to an ethical mandate to reduce disparities in ACTs, increasing the numbers of PLHA of color in ACTs is vital to advance scientific knowledge and improve diagnosis, development of preventive strategies, and treatment for PLHA of color [8–10, 13–15].
Description of the Multi-level Barriers to ACT Screening and Enrollment Experienced by PLHA of Color
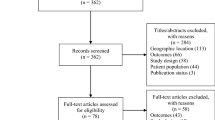
PLHA enter ACTs through a screening process. Screening typically begins with a medical history interview and physical examination, followed by a small number of additional visits for evaluation and testing to determine eligibility. Those found eligible for ACTs, typically the minority of those screened because of the strict inclusion and exclusion requirements (an estimated 13–49% of those screened [11, 16]), then have an opportunity to enroll. In the following section we describe the barriers that PLHA of color experience to ACTs through the process of screening and enrollment.
Barrier #1: Low Rates of Recruitment and Referral
A major reason why PLHA of color are under-represented in ACTs is that they are unlikely to ever be recruited for or referred to ACTs, and much less likely to be recruited or referred compared to their white peers [17, 18, 19•], including by HIV/AIDS primary care providers, who are typically the main source of referrals to ACTs [8, 9]. A growing literature suggests that provider beliefs about patients, including patients of color, influence their behavior with these patients, and this plays a role in racial/ethnic disparities in health [20]. Medical providers who deliver HIV primary care have been found to assume that PLHA of color are less interested in joining ACTs than whites, and in turn, are less likely to refer them to ACTs [8, 18].
Second, as research studies, the success of ACTs is dependent on patients’ rigorous adherence to study requirements. Providers are often hesitant to refer PLHA of color to ACTs because they are concerned about their patients’ abilities to adhere to protocols [8, 21, 22]. While in many cases PLHA may indeed not be appropriate for ACTs, this pre-screening by providers raises questions. First, it is difficult for clinicians to predict an individual’s future adherence with accuracy, and demographic characteristics are not good predictors of adherence [23, 24]. Further, adherence can vary over time, by treatment, and by context [25]. In our own research to reduce racial/ethnic disparities in ACTs, for example, we found that adherence to health care appointments is at least in part a reaction to the organizational setting where the patient receives care. In the case of PLHA of color who receive care at busy community-based organizations and clinics in hospitals, appointments typically begin late and patients are often double-booked. Therefore, patients have found they can arrive late or not show at all without penalty. However, when it comes time to consider ACTs, providers may assume that patients will not be adherent to ACTs because they are poorly adherent to medical visits. Yet patients indicate that their adherence to medical appointments is in large measure a rational response to the clinic’s practices. Although we have not examined adherence to HAART and its potential relationship to adherence to ACTs, we do know that very little research has been conducted on how to maximize adherence to ACTs for PLHA of color.
The same concerns regarding adherence that appear to influence the referral decisions of primary health care providers and the organizations serving PLHA of color may also come into play for AIDS clinical trials units (ACTUs). As part of study inclusion/exclusion criteria, ACT investigators are given discretion by trial sponsors to use clinical judgement to exclude patients who they believe are not good study candidates. These criteria include investigators’ judgment of substance use and loosely defined “social conditions” that lead investigators to believe that patients may not comply with the study protocol. For example, in an anonymous survey, ACTU research nurses and study coordinators expressed concerns about the capacity for PLHA of color to adhere to trial dosing schedules and required follow-up visits (investigators were not surveyed) [6•]. Moreover, these research clinicians reported being more comfortable enrolling white men in clinical trials than PLHA of color. This raises the possibility that ACTUs may exclude potentially eligible PLHA of color because of assumptions about social and behavioral barriers to adherence.
HIV/AIDS and substance use are “twin epidemics” [26], and substance use appears to play a significant role in ACT disparities in ways that may not always be apparent. Active alcohol and/or drug abuse are associated with poor adherence to HAART [8], but there is substantial variability among substance-using populations regarding their ability to achieve high adherence [27]. Providers are understandably hesitant to refer individuals with substance use problems to ACTs, as they may not benefit from trials nor achieve the high levels of adherence necessary in trials. However, in contrast to the problematic use of substances (that is, high frequency and/or quantity use that causes mental, physical, or social harm to the user), the non-problematic use of substances (that is, low-to-moderate frequency and/or quantity of use that does not cause mental, physical, or social harm to the user) does not necessarily present a barrier to trial participation and high levels of adherence. Yet providers may be ill equipped to make a determination of an individual’s suitability for an ACT with respect to substance use, particularly during short health care visits [28]. Moreover, providers may not have the time or training to distinguish between past and current substance use or abuse, the former not being a reason to exclude an individual from ACTs [29]. This suggests that health care providers may benefit from support and resources to better pre-screen patients for substance use problems that would interfere with ACT participation, including assessments using structured validated instruments or tools.
Barrier #2: When Invited to Participate in Trials, PLHA of Color May Be More Likely to Decline
Even when approached for trials, PLHA of color are more likely than their white peers to decline to participate [19•]. It is well documented that PLHA of color, particularly African-Americans, have great distrust of and hold negative attitudes toward ACTs, stemming partly from a legacy of past research studies in which patients were mistreated [8, 30, 31]. At the same time, PLHA of color also express high levels of interest in and willingness to participate in ACTs [17, 32, 33], particularly if a study is recommended by a primary care provider [34•, 35•]. Furthermore, knowledge of ACTs tends to be poor, particularly for those with inconsistent health care utilization patterns, and this serves as an additional barrier to ACTs [29]. Practical barriers and life circumstances may also interfere with ACT screening and enrollment, including lack of access to transportation and other pressing life problems related to poverty [9, 10, 36]. Over half of HIV-infected women have minor-age children, and family responsibilities and childcare may be experienced as greater priorities than ACTs [37]. As noted above, substance use is also a barrier. Until recently, ACTs have had restrictive criteria for substance use, whether the individual used in the past or present [9, 10]. Although individuals with historical substance use and current non-problematic substance use are now actively recruited into ACTs, PLHA are not typically aware of this shift in inclusion criteria, and avoid ACTs as a result, fearing stigma and exclusion [29].
Social influences impede access to ACTs among PLHA of color. Peer norms, social comparisons, modeling and reinforcement, and social interactions have powerful effects on individuals’ behaviors, including health behaviors [38, 39]. Among PLHA of color, social networks comprised of other PLHA of color, family, and friends also evidence a lack of information about and negative or mixed attitudes toward ACTs, contributing to negative social norms regarding ACTs. This results in a lack of support for ACTs among social network members, and concerns that one will experience social stigma related to ACT participation, which interfere with participation in ACTs [36].
Barrier #3: PLHA of Color May Be Less Likely to Be Found Eligible for Trials
Data are emerging that suggest that when screened, PLHA of color may be less likely to be found eligible for ACTs than their white peers [16], although this aspect of ACT disparities is understudied. Restrictive eligibility criteria of many ACTs, particularly therapeutic trials, has been cited as contributing to the lower likelihood of trial eligibility among PLHA of color [11]. In our own work with a mixed-gendered sample of predominantly PLHA of color presenting for screening to an ACTU, patients who were not prescreened by physicians for eligibility as is typical, we found an eligibility rate of only 13% for 30 ACTG and industry-sponsored trials [16]. The main reasons for ineligibility were mismatches between patients’ laboratory values (such as viral load, CD4), HAART and medical histories, and the requirements stipulated by the trials’ protocol enrollment criteria. Further, a recent analysis of the Women’s Interagency HIV Study (WIHS), the largest representative sample of HIV-infected women in the United States (including the proportional representation of women of color and those with past and current substance use), found that over half of the women in the WIHS cohort would have been excluded from participating in 20 key ACTG studies based on protocol enrollment criteria [11].
Barrier #4: PLHA of Color May Find the ACT System Foreign and Hard to Navigate
PLHA often experience structural barriers to ACT screening and enrollment [33]. Clinical trials units may be located in settings that are separate from clinics, and may have policies and procedures that differ from clinics, and thus may be difficult for PLHA to navigate [10]. The location, atmosphere, and procedures of a clinical trials unit may also be experienced as unfamiliar, which contributes to fear and mistrust [5, 40]. As noted by researchers in other disease categories (eg, stroke, cancer), misunderstandings between the patient and clinical trials units are common, particularly among populations less familiar with and less trusting of medical research [41].
Interventions to Reduce Barriers to ACTs for PLHA of Color
While the persistent racial/ethnic disparities in ACTs, and the factors that underlie these disparities, have been well described, the science of behavioral interventions to ameliorate these barriers is in its infancy. The multi-level and complex nature of barriers to ACTs for PLHA of color signal the need for interventions at a range of levels of influence, including policy, structural, organizational, social network, and individual-level strategies, as well as for interventions that operate simultaneously at multiple levels of influence.
Two clinic-based interventions are described in the literature. Freedberg and colleagues [42] developed a brief structural intervention. In this study, based in an inner-city hospital-based HIV clinic, all PLHA (regardless of the patient’s sociodemographic characteristics or potential eligibility) were provided with culturally sensitive information about ACTs during the patient’s first visit. While the intervention has not been evaluated in a randomized controlled trial, the brief intervention reduced disparities in ACT participation by race, risk behavior, and gender when compared to a historical cohort at the same clinic [42]. El-Sadr and colleagues [10] developed a multi-level outreach program to increase recruitment, enrollment, and adherence to study protocols among PLHA of color and women. The program included culturally sensitive informational materials about ACTs, outreach workers who made home visits when needed, transportation for patients for study visits, social work services for referrals to necessary, ancillary services (eg, mental health, housing), and peer support groups to assist patients with adherence to study protocols [10]. While El-Sadr and colleagues did not report efficacy data, the multi-level nature of the program directly targeted the types of barriers to recruitment and retention of PLHA of color to ACTs described above and therefore has promise as an intervention approach.
Our own work has focused on peer-driven intervention strategies to increase the participation of PLHA of color in ACTs in an urban environment. In response to the multi-level barriers experienced to ACTs among this group, the intervention (with the field name “the ACT2 Project”) was designed to target barriers at the levels of individuals (such as poor knowledge and high mistrust of ACTs, co-existing with great willingness to explore ACTs), their social networks (namely, peer norms regarding avoidance of medical research), and also social and structural impediments associated with health care providers and ACT settings. As described above, screening is a critical gateway to gaining access to ACTs. Further, screening yields indirect benefits to PLHA of color, including improvements in HIV health knowledge and the opportunity to contribute to research. This minimal-risk exchange may also reduce PLHA’s fears of ACTs, and establish a relationship between the PLHA and ACT unit. Yet, as reviewed above, PLHA of color are screened for ACTs at disproportionately low rates [43•]. Thus, the ACT2 Project’s primary outcome was ACT screening. Enrollment in trials is also being explored as a secondary outcome. However, enrollment patterns are complicated by the fact that the number and type of ACTs vary over time, and therefore to enter a trial, a participant’s health status, readiness to participate (and endorsement of the primary care provider in most cases), and an available and appropriate trial must all match at the same point in time.
Peer-driven intervention (PDI) is an effective, culturally appropriate, and low-cost intervention methodology that taps into six critical elements of behavior change: knowledge, skill building, motivation, peer influence, social norms, and repetition [44]. In the PDI model, individuals participate in facilitated intervention activities targeting critical mediators of behavior change (eg, knowledge, self-efficacy, motivation) and then independently educate up to three peers, for which compensation is provided. The PDI model hypothesizes that through peer education an individual’s own commitment to engage in the targeted health outcome behavior is strengthened because the act of educating peers is a public affirmation of the behavior. Peer education also entails repetition of the intervention’s core messages and may result in internalization of them. Thus, peer education increases individuals’ mastery of the intervention content [44]. Further, PDI attempts to alter network social norms through successive waves of recruitment and peer education [45]. PDI has been used successfully with PLHA to increase medication adherence [46] and reduce HIV-related sexual and drug use risk behavior [44].
The ACT2 intervention’s theoretical mechanisms of action (that is, how behavior change is hypothesized to come about) are grounded in the theory of normative regulation [47], which posits that the behaviors of individuals are amplified through their social groups, as well as motivational interviewing, a method for enhancing intrinsic motivation to change by exploring and resolving ambivalence [48], and social cognitive theory, which emphasizes individual and social-contextual influences on behavior [49]. The intervention is comprised of three group sessions (5.5 h total), three peer education experiences, and a brief (30 min) individual session conducted on the AIDS clinical trials unit to overcome structural barriers to ACTs. The study is currently in the final stages of evaluation in a randomized controlled trial, where participants in the control arm received a time-matched and attention-matched health education intervention. The study’s primary outcome is screening for ACTs to the point of determining eligibility. Importantly, the screening end point is modeled on the typical “real world” experience: PLHA must take initiative for screening and do not receive a financial incentive for screening, suggesting they attend because motivation to explore screening and ACTs is high.
Description of Sample and Preliminary Results
We present here data on the first 342 participants enrolled in the study. Participants ranged in age from 26 to 74 years with a mean of 49 years (SD = 7.3 years), and 43.9% were female. Almost all (91.5%) were people of color (64.9% African-American, 26.6% Latino/Hispanic). About two thirds recruited or recruited/educated at least one peer (64.9%). The majority was on antiretroviral therapy (66.1%) and reported their viral load levels as undetectable (67.4%). Only 19.6% had been screened for ACTs in the past. Preliminary data indicate that the ACT2 intervention is potent: approximately half (46.0%) of participants in the ACT2 intervention arm were screened, compared to less than 2% of those in the control arm. Enrollment results are in process but also promising. To date, of those screened, approximately 45% have been found eligible for a biomedical observational research study and almost all (approximately 90%) have entered the study. Approximately 9% have been found eligible for a therapeutic trial, and half have entered the trial. Thus, the ACT2 intervention approach is highly efficacious in increasing rates of screening for ACTs among PLHA of color, the critical gateway to enrollment in ACTs and an important outcome even independent of enrollment. Furthermore, preliminary data indicate that the ACT2 intervention also has a potent effect on increasing rates of participation in biomedical studies and clinical trials among PLHA of color.
Conclusions
PLHA of color evidence high willingness to participate in ACTs combined with numerous serious barriers to ACTs operating at the levels of individual PLHA, their social networks, their health care providers, the organizations that serve them, clinical trials units, and the types of trials and studies’ inclusion criteria. The small but growing literature on interventions to address racial/ethnic disparities in ACTs suggests some promising avenues for reducing these barriers through behavioral/social and structural interventions. Increasing access to screening through outreach in communities and service settings, and conducting behavioral intervention to reduce barriers to screening, are critical aspects of eliminating ACT racial/ethnic disparities, as screening is the gateway to ACT participation, a low-risk activity, and also has numerous indirect benefits to PLHA. The fact that barriers to ACTs are long-standing, complex, rooted in culture and social norms for PLHA of color, and also in the perceptions and practices of HIV care providers and ACT study clinicians, suggests that screening for ACTs should be regular, routine, and involve health care providers. Further, given the complex barriers to ACTs experienced by PLHA of color, support and assistance through screening, enrollment, and trial participation is recommended to foster positive outcomes including the high levels of adherence to trial protocols [10]. Further, ACTs and clinical trials units can also play a role in reducing ACT racial/ethnic disparities. As noted by Gandhi and colleagues [11], reducing subjective eligibility criteria may have the effect of broadening demographic and clinical representativeness of trials participants. Further, reducing the penalties to trial sites for losses to follow-up and less than perfect adherence would very likely increase the willingness of clinical trials units to recruit and enroll a more diverse population [6•]. Similarly, there is a need to develop trials targeting PLHA of color by such means as oversampling PLHA of color [10], modifying eligibility requirements [50], focusing on the clinical entities that are over-represented in PLHA of color, including HIV-associated nephropathy, and examining for racial/ethnic differences in drug metabolism and adverse events of anti-HIV treatments. We acknowledge that these recommendations are challenging. However, interventions that target organizations and/or multiple levels of influence simultaneously, including the types of approaches described in this article, have promise for increasing the representation of diverse racial/ethnic groups in ACTs.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report, 2008, Vol. 20. Available at http://www.cdc.gov/hiv/topics/surveillance/resources/reports/. Accessed June 23, 2010.
Centers for Disease Control and Prevention. HIV/AIDS among African-Americans. Available at http://www.cdc.gov/hiv/pubs/Facts/afam.htm. Accessed March 28, 2005.
Rubin MS, Colen CG, Link BG: Examination of inequalities in HIV/AIDS mortality in the United States from a fundamental cause perspective. Am J Public Health 2010, 100:1053–1059.
National Institute of Allergy and Infectious Diseases (NIAID). HIV Infection in Minority Populations. Available at http://www.niaid.nih.gov/topics/HIVAIDS/Understanding/Population%20Specific%20Information/Pages/minorityPopulations.aspx. Accessed February 28, 2010.
Gifford AL, Cunningham WE, Heslin KC, et al.: Participation in research and access to experimental treatments by HIV-infected patients. N Engl J Med 2002, 346:1373–1382.
• King WD, Defreitas D, Smith K, et al.: Attitudes and perceptions of AIDS clinical trials group site coordinators on HIV clinical trial recruitment and retention: A descriptive study. AIDS Patient Care STDS 2007, 21:551–563. AIDS clinical trials site coordinators and research nurses were surveyed for this study that evaluated their attitudes about and recruitment practices for HIV-positive people of color, women, and injection drug users.
National Institute of Allergy and Infectious Diseases (NIAID). Strategic plan for addressing health disparities: Fiscal years 2002–2006. Available at http://www.niaid.nih.gov/healthdisparities/NIAID_HD_Plan_Final.pdf. Accessed April 26, 2006.
Cargill VA, Stone VE: HIV/AIDS: A minority health issue. Med Clin North Am 2005, 89:895–912.
Parada J: The changing face of AIDS. Minority Health Today 2000, 1:9–17.
El-Sadr W, Capps L: The challenge of minority recruitment in clinical trials for AIDS. JAMA 1992, 267:954–957.
Gandhi M, Ameli N, Bacchetti P, et al.: Eligibility criteria for HIV clinical trials and generalizability of results: The gap between published reports and study protocols. AIDS 2005, 19:1885–1896.
King WD, Wong MD, Shapiro MF, et al.: Does racial concordance between HIV-positive patients and their physicians affect the time to receipt of protease inhibitors? J Gen Intern Med 2004, 19:1146–1153.
Stone V, Mauch M, Steger K, et al.: Race, gender, drug use, and participation in AIDS clinical trials. Lessons from a municipal hospital cohort. J Gen Intern Med 1997, 12:150–157.
Hussain-Gambles M: Ethnic minority under-representation in clinical trials. Whose responsibility is it anyway? J Health Organ Manag 2003, 17:138–143.
Stolberg SG: Racial disparity is found in AIDS clinical studies. New York Times. 2002:A24, May 2.
Marshak A, Costantini G, Middleton S, et al.: Screening for AIDS clinical trials in the project ACT cohort of racial/ethnic minorities and women in New York City: substantial interest but low eligibility. Presented at the 4th International AIDS Society Conference. Sydney, Australia; July 22–27, 2007.
DeFreitas D: Race and HIV clinical trial participation. J Natl Med Assoc 2010, 102:493–499.
Stone VE, Mauch MY, Steger KA: Provider attitudes regarding participation of women and persons of color in AIDS clinical trials. J Acquir Immune Defic Syndr Hum Retrovirol 1998, 19:245–253.
• Sullivan PS, McNaghten AD, Begley E, et al.: Enrollment of racial/ethnic minorities and women with HIV in clinical research studies of HIV medicines. J Natl Med Assoc 2007, 99:242–250. This article describes participation in clinical research studies of HIV medicines among women and people of color from 15 states.
van Ryn M: Research on the provider contribution to race/ethnicity disparities in medical care. Med Care 2002, 40:I140–I151.
Cotton DJ, Finkelstein DM, He W, Feinberg J: Determinants of accrual of women to a large, multicenter clinical trials program of human immunodeficiency virus infection. The AIDS Clinical Trials Group. J Acquir Immune Defic Syndr 1993, 6:1322–1328.
Murphy TF: Women and drug users: the changing faces of HIV clinical drug trials. QRB Qual Rev Bull 1991, 17:26–32.
Stone VE: Strategies for optimizing adherence to highly active antiretroviral therapy: lessons from research and clinical practice. Clin Infect Dis 2001, 33:865–872.
Bangsberg DR, Hecht FM, Clague H, et al.: Provider assessment of adherence to HIV antiretroviral therapy. J Acquir Immune Defic Syndr 2001, 26:435–442.
van Dijk L, Heerdink ER, Somai D, et al.: Patient risk profiles and practice variation in nonadherence to antidepressants, antihypertensives and oral hypoglycemics. BMC Health Serv Res 2007, 7:51.
National Commission on Acquired Immune Deficiency Syndrome: The Twin Epidemics of Substance Use and HIV. Available at http://www.dogwoodcenter.org/references/studies91F.html. Accessed June 24, 2010.
Wood E, Montaner JS, Bangsberg DR, et al.: Expanding access to HIV antiretroviral therapy among marginalized populations in the developed world. AIDS 2003, 17:2419–2427.
Abrams Weintraub T, Saitz R, Samet JH: Education of preventive medicine residents: alcohol, tobacco, and other drug abuse. Am J Prev Med 2003, 24:101–105.
Gwadz M, Leonard N, Riedel M, et al.: Project ACT: A pilot intervention to increase screening for AIDS clinical trials among racial/ethnic minorities and women in New York City. Presented at the XVI International AIDS Conference. Toronto, Canada; August 13–18, 2006.
Gamble VN: A legacy of distrust: African Americans and medical research. Am J Prev Med 1993, 9:35–38.
Shavers-Hornaday VL, Lynch CF, Burmeister LF, Torner JC: Why are African Americans under-represented in medical research studies? Impediments to participation. Ethn Health 1997, 2:31–45.
Gwadz MV, Leonard NR, Nakagawa A, et al.: Gender differences in attitudes toward AIDS clinical trials among urban HIV-infected individuals from racial and ethnic minority backgrounds. AIDS Care 2006, 18:786–794.
Wendler D, Kington R, Madans J, et al.: Are racial and ethnic minorities less willing to participate in health research? PLoS Med 2006, 3:e19.
• Adeyemi OF, Evans AT, Bahk M: HIV-infected adults from minority ethnic groups are willing to participate in research if asked. AIDS Patient Care STDS 2009, 23:859–865. This article describes factors influencing participation in HIV research among people of color.
• Volkmann ER, Claiborne D, Currier JS: Determinants of participation in HIV clinical trials: The importance of patients’ trust in their provider. HIV Clin Trials 2009, 10:104–109. This study explores factors that increase people’s willingness to participate in AIDS clinical trials and preferred means of conveying information about trials.
Mills E, Wilson K, Rachlis B, et al.: Barriers to participation in HIV drug trials: A systematic review. Lancet Infect Dis 2006, 6:32–38.
Brown-Peterside P, Chiasson MA, Ren L, Koblin BA: Involving women in HIV vaccine efficacy trials: Lessons learned from a vaccine preparedness study in New York City. J Urban Health 2000, 77:425–437.
Flay B, Petraitis J: The theory of triadic influence. In Advances in Medical Sociology, vol IV. Edited by Albrecht G. Greenwich, CT: JAI Press; 1994:19–44.
Latkin C: Outreach in natural settings: the use of peer leaders for HIV prevention among injecting drug users’ networks. Public Health Rep 1998, 113(Suppl 1):151–159.
Andersen JW, Fass R, van der Horst C: Factors associated with early study discontinuation in AACTG studies, DACS 200. Contemp Clin Trials 2007, 28:583–592.
Gorelick PB, Harris Y, Burnett B, Bonecutter FJ: The recruitment triangle: reasons why African Americans enroll, refuse to enroll, or voluntarily withdraw from a clinical trial. An interim report from the African-American Antiplatelet Stroke Prevention Study (AAASPS). J Natl Med Assoc 1998, 90:141–145.
Freedberg KA, Sullivan L, Georgakis A, et al.: Improving participation in HIV clinical trials: Impact of a brief intervention. HIV Clin Trials 2001, 2:205–212.
• Gwadz MV, Cylar K, Leonard NR, et al.: An exploratory behavioral intervention trial to improve rates of screening for AIDS clinical trials among racial/ethnic minority and female persons living with HIV/AIDS. AIDS Behav 2010, 14:639–648. This article describes a pilot behavioral intervention that was efficacious at increasing rates of ACT screening among people of color and women living with HIV/AIDS.
Broadhead RS, Heckathorn DD, Weakliem DL, et al.: Harnessing peer education networks as an instrument for AIDS prevention. Public Health Rep 1998, 113(Suppl 1):42–57.
Heckathorn DD, Broadhead RS, Anthony DL, Weakliem DL: AIDS and social networks: HIV prevention through network mobilization. Sociol Focus 1999, 32:159–179.
Broadhead RS, Heckathorn DD, Altice FL, et al.: Increasing drug users’ adherence to HIV treatment: Results of a peer-driven intervention feasibility study. Soc Sci Med 2002, 55:235–246.
Heckathorn D: Respondent-driven sampling: A new approach to the study of hidden population. Soc Probl 1997, 44:174–199.
Miller W, Rollnick S: Motivational Interviewing: Preparing People for Change, edn 2. New York: Guilford; 2002.
Bandura A: Social Foundations of Thought and Action. Englewood Cliffs, NJ: Prentice Hall; 1986.
Ethier KA, Rodriguez MR, Fox-Tierney RA, et al.: Recruitment in AIDS clinical trials: Investigation of sociodemographic and psychosocial factors affecting participation in clinical research. AIDS Behav 1999, 3:219–230.
Acknowledgments
Funding for this study was provided by the National Institute of Allergy and Infectious Diseases, National Institutes of Health (1 R01 AI070005) and the Center for Drug Use and HIV Research (P30DA011041), funded by the National Institute on Drug Abuse at the National Institutes of Health. We would like to acknowledge the men and women who participated in the ACT1 and ACT2 Projects, and Dr. Usha Sharma (Program Officer) and Dr. Vanessa Elharrar (Medical Officer), Division of AIDS, National Institute of Allergy and Infectious Diseases. The project is dedicated to the memory of Keith Cylar, Co-founder and Co-CEO of Housing Works (1958–2004), and former Housing Works PI, The ACT1 Project.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gwadz, M.V., Colon, P., Ritchie, A.S. et al. Increasing and Supporting the Participation of Persons of Color Living with HIV/AIDS in AIDS Clinical Trials. Curr HIV/AIDS Rep 7, 194–200 (2010). https://doi.org/10.1007/s11904-010-0055-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-010-0055-3