Abstract
The BCR-ABL1 oncogenic tyrosine kinase can transform pluripotent hematopoietic stem cells and initiate chronic myeloid leukemia in chronic phase (CML-CP), a myeloproliferative disorder characterized by excessive accumulation of mature myeloid cells. Patients in CML-CP usually respond to treatment with ABL1 tyrosine kinase inhibitors (TKIs) such as imatinib, though some patients who respond initially may become resistant later. CML-CP leukemia stem cells (LSCs) are intrinsically insensitive to TKIs and thus survive in the long term. These LSCs or their progeny may at some stage acquire additional genetic changes that cause the leukemia to transform further, from CML-CP to a more advanced phase, which has been subclassified as either accelerated phase (CML-AP) or blastic phase (CML-BP). CML-BP is characterized by a major clonal expansion of immature progenitors, which have either myeloid or lymphoid features. CML-BP responds poorly to treatment and is usually fatal. This review discusses the role of genomic instability leading to blastic transformation of CML and proposes some novel therapeutic approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Before the era of tyrosine kinase inhibitors (TKIs), patients who presented with chronic myeloid leukemia in chronic phase (CML-CP) progressed to a more accelerated phase (CML-AP) after a median interval of about 5 years. CML-AP patients might still respond to treatment for months or years, but eventually they developed a very aggressive blast phase (CML-BP), after which the median survival was about 6 months. Some patients progressed directly to BP without an intermediate phase of acceleration.
Although continued use of TKIs to treat CML-CP may indeed prevent CML-BP in a large population of patients, between 15% and 20% of patients, most of whom will have been classified as nonresponders, may still progress to CML-BP [1]. Additional cytogenetic aberrations such as +Ph, +8, i(17q) and +19, if present at diagnosis, are associated with increased risk of progression to CML-AP/BC [2•]. In addition, the ability of TKIs to render residual CML-CP cells “inactive” rather than to eradicate them entirely suggests that CML-BP still may occur even in “responding” patients [3, 4]. Moreover, it has been reported that a rare sudden BP may occur in an unpredictable fashion in CML-CP patients who appear to be responding to imatinib treatment [5].
Chromosomal Aberrations Associated with CML Blast Phase
CML-BP is associated with dramatic changes in the leukemia cell phenotype: enhanced “stemness,” uncontrolled proliferation and invasion, abrogated differentiation, and early resistance to TKIs [6, 7]. At present, the molecular mechanisms responsible for these extensive changes are still uncertain; most likely, they involve activation of oncogenic factors, inactivation of tumor suppressors, or both. These changes may arise through mutagenesis in TKI-refractory CML-CP cells.
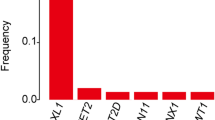
Accumulation of various chromosomal aberrations and mutations is believed to be responsible for the transition of a relatively benign CP to the aggressive BP [8]. The frequency of additional chromosomal abnormalities is about 7% in CML-CP and increases to 40–70% in the advanced phases of disease, as evaluated by standard cytogenetic analysis [9]. A deep-sequencing study of CML-BP patients revealed mutations in almost 77% of cases [10]. Numeric chromosomal changes were detected at a 50-fold higher frequency and structural changes at a 12-fold higher frequency in CML-BP, compared with CML-CP. More sensitive comparative genomic hybridization (CGH) and single-nucleotide polymorphism (SNP) analyses detected multiple genetic aberrations already in CP, but BP patients carried much more complex karyotypes [11, 12]. This observation suggests that genomic instability is an early event in CML.
Patients from the pre-imatinib and imatinib eras have displayed similar types of genetic aberrations that mostly involve the presence of additional chromosomes, gene deletions, and insertions or point mutations [13–15, 16•]. At the molecular level, the most common mutations (other than these in BCR-ABL1 kinase domain) in myeloid BP are detected in 20–30% of cases in the tumor suppressor gene p53 [i(17q) and t(1;17) associated with the loss of p53, and point mutations in p53] and in 38% of cases in the transcription factor RUNX1 (also known as AML1) [t(1;21)] [15, 17, 18]. Chromosomal aberrations are found more frequently in lymphoid than in myeloid CML-BP and resemble those found in B-cell acute lymphoblastic leukemia (B-ALL) [9]. Deletions of the CDKN2A/B and IKZF1 (Ikaros) genes were found in 50–55% of patients with lymphoid BP [18–21]. Moreover, BCR-ABL1-mediated stimulation of activation-induced cytidine deaminase (AID) leads to a hypermutator phenotype, CML-lymphoid BP, and imatinib resistance [22].
Other aberrations found in CML-BP patients involve additional chromosomes (+Ph, +8, +19), t(3;21) and t(7;11) generating AML-1/EVI1 and NUP98/HOXA9 fusion oncogenes respectively, translocations and inversions associated with AML/myelodysplasia [inv(3), t(15;17)], loss-of-heterozygosity (LOH) at 14q32, homozygous mutations/deletions of pRB, inactivating point mutations in p53 and in ICSBP, gain-of-function mutations in GATA-2 and RAS, and mutations in PRDM16. Numerous SNPs have been reported in additional genes regulating cell differentiation, such as GATA-3 and RUNX1 in myeloid CML-BP [23], but these results await confirmation. Recently, aberrations in genes that are mutated in BCR-ABL1-negative myeloproliferative neoplasms (CBL, CBLB, TET2, ASXL1, IDH1/2) have been reported in CML-AP/BP patients [24]. However, these aberrations may represent passenger mutations not affecting the disease progression [25].
Experimental findings support the conclusion that genetic aberrations contribute to malignant progression of CML. For example, loss of p53 led to a CML-BP-like disorder in mice [26]. CDKN2a gene loss enhanced oncogenicity in mouse models of BCR-ABL1-induced ALL [27]. Co-expression of BCR-ABL1 and NUP98/HOXA9 caused CML-BP-like disease in mice [28]. GATA-2 gain-of-function mutations, partial deletions of PMRD16 and RUNX1, and expression of RUNX1/PMRD16 detected in CML-myeloid BP may disturb myelomonocytic differentiation, strongly suggesting their involvement in acute myeloid transformation [23, 29].
Moreover, genetic aberrations associated with CML-BP progression likely play a role in TKI resistance [30], causing a high risk of treatment failure [31]. For example, additional chromosomal aberrations, loss of p53, and CDKN2A and RUNX1 abnormalities may be responsible for disease persistence during imatinib treatment [27, 32–34].
Role of TKI-Resistant Mutations in BCR-ABL1 Kinase in CML-BP Progression
Point mutations in BCR-ABL1 kinase have been detected in 50–90% of patients displaying resistance to imatinib, including about 23% of imatinib-naive patients [35]. Moreover, the application of second-generation TKIs in imatinib-resistant cases led to selection of additional resistance mutations [36]. Third-generation TKIs such as DCC-2036 and ponatinib are currently in clinical trials [37], but (similarly to imatinib and second-generation TKIs) it is likely that BCR-ABL1 kinase mutants resistant to third-generation TKIs will develop, perhaps because of the emergence of resistant clones carrying BCR-ABL1 kinase compound mutations [38]. Altogether, CML cells are elusive targets even for the most advanced therapies [39].
TKI-resistant BCR-ABL1 mutants exhibit altered kinase activity, substrate utilization, and transformation potency and are associated with clonal cytogenetic evolution, which may affect disease progression [35, 40]. Likewise, the presence of mutations in BCR-ABL1 kinase was associated with greater likelihood of disease progression, which suggests enhanced genomic instability in these cells [41]. For example, frequent EVI1 translocations were found in TKI-resistant BCR-ABL1 kinase mutant clones in patient who progressed to myeloid BP [42].
The Complexity of CML-BP
Specific CML-BP-associated genetic alterations are relatively common, but no one lesion occurs in the majority of CML-BP patients, so it is unlikely that any one specific secondary genetic aberration can be defined as “the culprit” causing disease progression. More likely, CML-BP results from the accumulation of a critical number or combination of different mutations. It can be speculated that CML-BP is a multistep, time-dependent process initiated by mechanisms both dependent and independent of BCR-ABL1, which cause DNA damage associated with inefficient and unfaithful DNA repair in CML-CP, facilitating the accumulation of additional genetic changes that lead to the selection of CML-BP clones [7].
Because there is a direct correlation between levels of BCR-ABL1 kinase expression and the frequency of clinically relevant BCR-ABL1 mutations [43, 44], unrestrained and increasing BCR-ABL1 kinase activity may promote or contribute to clonal evolution, thereby leading to CML-BP [45]. This effect may occur at the level of leukemia stem cells (LSCs) (which display innate or acquired TKI resistance), leukemic progenitor cells (LPCs), or both; the LPCs may have developed resistance and expanded during TKI therapy [11, 46]. Thus, we can speculate that prevention or effective treatment of CML-BP will be achieved only if novel therapeutic strategies can be developed that are capable of interfering with the molecular networks (both dependent and independent of BCR-ABL1) that allow clonal expansion and are responsible for acquired “stemness,” impaired differentiation, and increased genomic instability in CML-BP.
Genomic Instability Facilitates CML-BP
Genomic instability usually results from an aberrant cellular response to enhanced DNA damage. In CML cells, these mechanisms can be modulated by BCR-ABL1 kinase or can be kinase-independent.
Enhanced DNA Damage
Much endogenous DNA damage arises from intermediates of oxygen reduction called reactive oxygen species (ROS), such as superoxide radical anion (•O −2 ), which may lead to the production of hydrogen peroxide (H2O2) and hydroxyl radical (•OH). BCR-ABL1-transformed cell lines and CD34+ CML cells contain, on average, two to six times more ROS than their normal counterparts (more than normal in CML-CP, and even more in CML-BP) [45, 47, 48]; the mitochondrial respiratory chain, enhanced glucose uptake, and NADPH oxidase may play a role in this phenomenon [49]. ROS can cause damage to all nucleobases and deoxyribose residues in DNA, freeing nucleotides that generate oxidized bases and DNA double-strand breaks (DSBs) [50]. The number of oxidative “hits” to DNA (for example, 7,8-dihydro-8-oxo-2′-deoxyguanosine, 8-oxoG) per normal human cell per day is about 104, and normal cells contain about 50 DSBs per cell per cell cycle. CD34+ CML cells display about three to eight times more oxidized nucleobases and four to eight times more DSBs [45, 47, 48].
DNA damage could also be directly induced by the ionizing radiation and genotoxic drugs used as part of a conditioning regimen in hematopoietic transplantation for CML patients. BCR-ABL1-positive cells accumulate more irradiation-induced and drug-induced DNA lesions than normal cells, thus generating chromosomal aberrations [51•, 52].
Unfaithful and Inefficient DNA Repair
Cellular DNA repair systems act to remove DNA damage and ultimately preserve the informational integrity of the genome. If too much damage is inflicted, the apoptotic pathways are activated to eliminate cells with irreparable and potentially mutagenic DNA lesions [53]. Leukemia cells are tolerant to DNA damage due to BCR-ABL1-mediated protection from apoptosis, modulation of the response to DNA damage, or both [54]. Moreover, FOXO3a, a critical mediator of resistance to physiologic oxidative stress, localizes in the nuclei of LSCs in the murine model of CML-CP, suggesting another mechanism of protection from the toxic effects of ROS [55].
Defective or inefficient repair of ROS-induced oxidized DNA bases and DSBs may lead to a variety of point mutations and chromosomal aberrations. CD34+ CML cells display a malfunctioning mismatch repair pathway, which can facilitate accumulation of point mutations [56]. BCR-ABL1 also promotes mutagenic nucleotide excision repair (NER) [57] and stimulates DSB repair, but the fidelity of the repair mechanisms (homologous recombination repair [HRR], nonhomologous end-joining [NHEJ], and single-strand annealing [SSA]) is compromised [45, 48, 58–60]. In BCR-ABL1–positive cells, point mutations were introduced during usually faithful HRR, extensive nucleobase loss was associated with NHEJ, and enhanced SSA generated large deletions. Overexpression and tyrosine phosphorylation of RAD51, a key element in HRR responsible for strand invasion and pairing, may result in aberrant HRR. Deregulation of DNA ligase IIIα, Werner helicase/exonuclease, DNA-end-processing factor CtIP, and Artemis may contribute to excessive loss of DNA bases during NHEJ in BCR-ABL1-positive cells.
Genomic Instability in Leukemia Stem Cells and Leukemic Progenitor Cells
The (9;22) translocation may represent a random event or may result from pre-existing conditions associated with genomic instability in hematopoietic stem cells. Therefore, additional genetic aberrations accumulated during the course of CML may be promoted by BCR-ABL1 kinase and also by a pre-existing abnormality responsible for the formation of t(9;22)(q34;q11). The former statement is supported by reports that BCR-ABL1 kinase-positive cells acquire more oxidative DNA lesions (8-oxoG, DSBs) than normal counterparts in response to endogenous ROS and genotoxic treatment [47, 48], and that the kinase can inhibit some DNA repair mechanisms (e.g., mismatch repair) and stimulate other mechanisms (NER, HRR, NHEJ, and SSA) at the cost of their fidelity [61]. However, the pre-existing condition cannot be ruled out because chromosome abnormalities were detected in t(9;22)(q34;q11)-negative metaphases appearing during imatinib therapy in patients with newly diagnosed CML-CP [36]. Genomic instability may also depend, at least partially, on the presence of BCR-ABL1 protein, even if it does not express kinase activity. This speculation is supported by the reports that survival of CML-CP LSCs is promoted by BCR-ABL1 protein, not the kinase activity [62], and that BCR-ABL1-induced adhesion defects are tyrosine kinase-independent [63].
Genomic instability in CML-CP most likely occurs in the LSC-enriched CD34+CD38− population and/or the LPC-rich CD34+ population, as TKI-resistant BCR-ABL1 mutants and chromosomal aberrations have been detected in both subpopulations [44, 46, 52]. CML-CP can progress to either myeloid or lymphoid BP (or sometimes a mixed myeloid/lymphoid phenotype), and chromosomal abnormalities are documented in both phenotypes [64], suggesting that genomic instability may occur at the LSC level, the LPC level, or both.
Genomic Instability in CML Cells in the Era of TKIs
Because BCR-ABL1 kinase induces genomic instability [8], imatinib and other TKIs should prevent the accumulation of additional genetic changes in CML cells. In fact, imatinib reduced ROS, oxidative DNA damage, point mutations, and other genetic aberrations in BCR-ABL1-positive cell lines and BCR-ABL1 transgenic mice [47, 48, 65]. Nevertheless, imatinib-treated CML patients continue to accumulate point mutations (including those causing resistance to other TKIs) and chromosomal aberrations [14, 29, 36, 66].
There are several possible explanations for persistent genomic instability during TKI treatment. First, the effect of TKIs on BCR-ABL1 kinase-induced signaling may be obscured by growth factors, usually resulting in incomplete inhibition or even stimulation of signaling pathways, such as those involving STAT5, AKT, and MAPK [67, 68]. Second, imatinib may exert mutagenic activity to induce centrosome and chromosome aberrations [69]. The appearance of cytogenetic aberrations in t(9;22)(q34;q11)-negative cells following imatinib therapy supports this hypothesis [70]. Third, if CML-CP cells display an active, pre-existing genomic instability responsible for the generation of t(9;22), this process should be independent of BCR-ABL1 kinase and will continue generating errors despite treatment [36].
Inhibition of Genomic Instability in CML-CP to Prevent CML-BP
At diagnosis, most CML-CP patients do not have mutations or a “critical” combination of aberrations causing either TKI resistance or disease progression. Nevertheless, some TKI-treated patients develop mutations and chromosomal aberrations, even though imatinib efficiently antagonizes genomic instability in experimental CML models. Prevention of genomic instability may be critical for a better therapeutic effect or even eradication of CML, given several facts: (1) BCR-ABL-negative patients, as assessed by reverse transcriptase PCR, may have up to 106 CML cells; (2) CML-CP patients can have about 5 × 107 CD34+ cells displaying innate imatinib resistance [71]; and (3) CD34+CD38− LSCs in CML-CP can expand in the presence of imatinib and acquire TKI-resistant BCR-ABL1 kinase mutations and additional chromosomal aberrations [46].
ROS-induced oxidative DNA damage is often detected in CML-BP, resulting in both clinically relevant BCR-ABL1 mutations and chromosomal aberrations (i.e., aneuploidy, translocations, and truncations) [47, 51•]. Antioxidants can diminish ROS-mediated oxidative DNA damage and reduce the appearance of TKI-resistant mutations and chromosomal aberrations [45, 47, 48]. The combination of imatinib and an antioxidant has exerted a synergistic/additive antimutagenic effect [47], so it is possible that the combination of a TKI and antioxidants may prevent CML-BP by reducing the appearance of TKI-resistant clones and the accumulation of genetic aberrations.
Conclusions
We postulate that elevated levels of DNA damage, combined with defective or inefficient DNA repair in LSCs, LPCs, or both, can generate mutations and chromosomal aberrations in CML-CP LSCs or LPCs, causing resistance to TKIs and progression toward CML-BP. TKI-refractory LSCs and LPCs may be like ticking time bombs that eventually explode to produce a CML-BP clone. However, some crucial questions have yet to be answered: Does malignant progression originate from CML-CP LSCs, LPCs, or both? What are the molecular mechanisms driving genomic instability in LSCs or LPCs? Is the acquisition of self-renewal, impaired differentiation, and increased genomic instability of CML-BP stem cells or progenitor cells solely dependent on BCR-ABL1? It is highly plausible that in CML-CP, BCR-ABL1-induced genomic aberrations and BCR-ABL1-independent pre-existing genetic lesions may function as amplifiers of a genetically unstable phenotype, and thereby predispose CML to blastic transformation by affecting “stemness,” survival, proliferation, and differentiation of the LSCs, the LPCs, or both.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Foroni L, Gerrard G, Nna E, et al. Technical aspects and clinical applications of measuring BCR-ABL1 transcripts number in chronic myeloid leukemia. Am J Hematol. 2009;84:517–22.
• Fabarius A, Leitner A, Hochhaus A, et al. Impact of additional cytogenetic aberrations at diagnosis on prognosis of CML: long-term observation of 1151 patients from the randomized CML Study IV. Blood. 2011;118:6760–8. This report demonstrated the importance of screening patients at diagnosis for additional chromosomal aberrations, which may predict an increased probability of malignant progression.
Barnes DJ, Melo JV. Primitive, quiescent and difficult to kill: the role of non-proliferating stem cells in chronic myeloid leukemia. Cell Cycle. 2006;5:2862–6.
Corbin AS, Agarwal A, Loriaux M, et al. Human chronic myeloid leukemia stem cells are insensitive to imatinib despite inhibition of BCR-ABL activity. J Clin Invest. 2011;121:396–409.
Tantiworawit A, Power MM, Barnett MJ, et al. Long-term follow-up of patients with chronic myeloid leukemia in chronic phase developing sudden blast phase on imatinib therapy. Leuk Lymphoma. 2011 Dec 22 (Epub ahead of print).
Calabretta B, Perrotti D. The biology of CML blast crisis. Blood. 2004;103:4010–22.
Perrotti D, Jamieson C, Goldman J, et al. Chronic myeloid leukemia: mechanisms of blastic transformation. J Clin Invest. 2010;120:2254–64.
Skorski T. BCR/ABL, DNA damage and DNA repair: implications for new treatment concepts. Leuk Lymphoma. 2008;49:610–4.
Bacher U, Haferlach T, Hiddemann W, et al. Additional clonal abnormalities in Philadelphia-positive ALL and CML demonstrate a different cytogenetic pattern at diagnosis and follow different pathways at progression. Cancer Genet Cytogenet. 2005;157:53–61.
Grossmann V, Kohlmann A, Zenger M, et al. A deep-sequencing study of chronic myeloid leukemia patients in blast crisis (BC-CML) detects mutations in 76.9% of cases. Leukemia. 2011;25:557–60.
Brazma D, Grace C, Howard J, et al. Genomic profile of chronic myelogenous leukemia: imbalances associated with disease progression. Genes Chromosomes Cancer. 2007;46:1039–50.
Khorashad JS, De Melo VA, Fiegler H, et al. Multiple sub-microscopic genomic lesions are a universal feature of chronic myeloid leukaemia at diagnosis. Leukemia. 2008;22:1806–7.
Yamamoto M, Kakihana K, Kurosu T, et al. Clonal evolution with inv(11)(p15q22) and NUP98/DDX10 fusion gene in imatinib-resistant chronic myelogenous leukemia. Cancer Genet Cytogenet. 2005;157:104–8.
Fabarius A, Haferlach C, Muller MC, et al. Dynamics of cytogenetic aberrations in Philadelphia chromosome positive and negative hematopoiesis during dasatinib therapy of chronic myeloid leukemia patients after imatinib failure. Haematologica. 2007;92:834–7.
Roche-Lestienne C, Deluche L, Corm S, et al. RUNX1 DNA-binding mutations and RUNX1-PRDM16 cryptic fusions in BCR-ABL+ leukemias are frequently associated with secondary trisomy 21 and may contribute to clonal evolution and imatinib resistance. Blood. 2008;111:3735–41.
• Haferlach C, Bacher U, Schnittger S, et al. Similar patterns of chromosome abnormalities in CML occur in addition to the Philadelphia chromosome with or without tyrosine kinase inhibitor treatment. Leukemia. 2010;24:638–40. This work demonstrates that imatinib treatment does not prevent the accumulation of additional chromosomal aberrations in CML-CP patients.
Lanza F, Bi S. Role of p53 in leukemogenesis of chronic myeloid leukemia. Stem Cells. 1995;13:445–52.
Mullighan CG, Miller CB, Radtke I, et al. BCR-ABL1 lymphoblastic leukaemia is characterized by the deletion of Ikaros. Nature. 2008;453:110–4.
Mullighan CG, Williams RT, Downing JR, et al. Failure of CDKN2A/B (INK4A/B-ARF)-mediated tumor suppression and resistance to targeted therapy in acute lymphoblastic leukemia induced by BCR-ABL. Genes Dev. 2008;22:1411–5.
Nakayama H, Ishimaru F, Avitahl N, et al. Decreases in Ikaros activity correlate with blast crisis in patients with chronic myelogenous leukemia. Cancer Res. 1999;59:3931–4.
Sill H, Goldman JM, Cross NC. Homozygous deletions of the p16 tumor-suppressor gene are associated with lymphoid transformation of chronic myeloid leukemia. Blood. 1995;85:2013–6.
Klemm L, Duy C, Iacobucci I, et al. The B cell mutator AID promotes B lymphoid blast crisis and drug resistance in chronic myeloid leukemia. Cancer Cell. 2009;16:232–45.
Zhang SJ, Ma LY, Huang QH, et al. Gain-of-function mutation of GATA-2 in acute myeloid transformation of chronic myeloid leukemia. Proc Natl Acad Sci U S A. 2008;105:2076–81.
Makishima H, Jankowska AM, McDevitt MA, et al. CBL, CBLB, TET2, ASXL1, and IDH1/2 mutations and additional chromosomal aberrations constitute molecular events in chronic myelogenous leukemia. Blood. 2011;117:e198–206.
Roche-Lestienne C, Marceau A, Labis E, et al. Mutation analysis of TET2, IDH1, IDH2 and ASXL1 in chronic myeloid leukemia. Leukemia. 2011;25:1661–4.
Skorski T, Nieborowska-Skorska M, Wlodarski P, et al. Blastic transformation of p53-deficient bone marrow cells by p210bcr/abl tyrosine kinase. Proc Natl Acad Sci U S A. 1996;93:13137–42.
Williams RT, Roussel MF, Sherr CJ. Arf gene loss enhances oncogenicity and limits imatinib response in mouse models of Bcr-Abl-induced acute lymphoblastic leukemia. Proc Natl Acad Sci U S A. 2006;103:6688–93.
Dash AB, Williams IR, Kutok JL, et al. A murine model of CML blast crisis induced by cooperation between BCR/ABL and NUP98/HOXA9. Proc Natl Acad Sci U S A. 2002;99:7622–7.
Deluche L, Joha S, Corm S, et al. Cryptic and partial deletions of PRDM16 and RUNX1 without t(1;21)(p36;q22) and/or RUNX1-PRDM16 fusion in a case of progressive chronic myeloid leukemia: a complex chromosomal rearrangement of underestimated frequency in disease progression? Gene Chromosomes Cancer. 2008;47:1110–7.
Lahaye T, Riehm B, Berger U, et al. Response and resistance in 300 patients with BCR-ABL-positive leukemias treated with imatinib in a single center: a 4.5-year follow-up. Cancer. 2005;103:1659–69.
Cortes J, O’Dwyer ME. Clonal evolution in chronic myelogenous leukemia. Hematol Oncol Clin North Am. 2004;18:671–84.
Wendel HG, de Stanchina E, Cepero E, et al. Loss of p53 impedes the antileukemic response to BCR-ABL inhibition. Proc Natl Acad Sci U S A. 2006;103:7444–9.
Miething C, Grundler R, Mugler C, et al. Retroviral insertional mutagenesis identifies RUNX genes involved in chronic myeloid leukemia disease persistence under imatinib treatment. Proc Natl Acad Sci U S A. 2007;104:4594–9.
Kim TD, Turkmen S, Schwarz M, et al. Impact of additional chromosomal aberrations and BCR-ABL kinase domain mutations on the response to nilotinib in Philadelphia chromosome-positive chronic myeloid leukemia. Haematologica. 2010;95:582–8.
Willis SG, Lange T, Demehri S, et al. High-sensitivity detection of BCR-ABL kinase domain mutations in imatinib-naive patients: correlation with clonal cytogenetic evolution but not response to therapy. Blood. 2005;106:2128–1237.
Cortes J, Jabbour E, Kantarjian H, et al. Dynamics of BCR-ABL kinase domain mutations in chronic myeloid leukemia after sequential treatment with multiple tyrosine kinase inhibitors. Blood. 2007;110:4005–11.
Santos FP, Quintas-Cardama A. New drugs for chronic myelogenous leukemia. Curr Hematol Malig Rep. 2011;6:96–103.
Eide CA, Adrian LT, Tyner JW, et al. The ABL switch control inhibitor DCC-2036 is active against the chronic myeloid leukemia mutant BCR-ABLT315I and exhibits a narrow resistance profile. Cancer Res. 2011;71:3189–95.
Skorski T. BCR-ABL1 kinase: hunting an elusive target with new weapons. Chem Biol. 2011;18:1352–3.
Griswold IJ, MacPartlin M, Bumm T, et al. Kinase domain mutants of Bcr-Abl exhibit altered transformation potency, kinase activity, and substrate utilization, irrespective of sensitivity to imatinib. Mol Cell Biol. 2006;26:6082–93.
Soverini S, Martinelli G, Rosti G, et al. ABL mutations in late chronic phase chronic myeloid leukemia patients with up-front cytogenetic resistance to imatinib are associated with a greater likelihood of progression to blast crisis and shorter survival: a study by the GIMEMA Working Party on Chronic Myeloid Leukemia. J Clin Oncol. 2005;23:4100–9.
Paquette RL, Nicoll J, Chalukya M, et al. Frequent EVI1 translocations in myeloid blast crisis CML that evolves through tyrosine kinase inhibitors. Cancer Genet. 2011;204:392–7.
Schultheis B, Szydlo R, Mahon FX, et al. Analysis of total phosphotyrosine levels in CD34+ cells from CML patients to predict the response to imatinib mesylate treatment. Blood. 2005;105:4893–4.
Barnes DJ, Palaiologou D, Panousopoulou E, et al. Bcr-Abl expression levels determine the rate of development of resistance to imatinib mesylate in chronic myeloid leukemia. Cancer Res. 2005;65:8912–9.
Cramer K, Nieborowska-Skorska M, Koptyra M, et al. BCR/ABL and other kinases from chronic myeloproliferative disorders stimulate single-strand annealing, an unfaithful DNA double-strand break repair. Cancer Res. 2008;68:6884–8.
Jiang X, Saw KM, Eaves A, et al. Instability of BCR-ABL gene in primary and cultured chronic myeloid leukemia stem cells. J Natl Cancer Inst. 2007;99:680–93.
Koptyra M, Falinski R, Nowicki MO, et al. BCR/ABL kinase induces self-mutagenesis via reactive oxygen species to encode imatinib resistance. Blood. 2006;108:319–27.
Nowicki MO, Falinski R, Koptyra M, et al. BCR/ABL oncogenic kinase promotes unfaithful repair of the reactive oxygen species-dependent DNA double-strand breaks. Blood. 2004;104:3746–53.
Rodrigues MS, Reddy MM, Sattler M. Cell cycle regulation by oncogenic tyrosine kinases in myeloid neoplasias: from molecular redox mechanisms to health implications. Antioxid Redox Signal. 2008;10:1813–48.
Beckman KB, Ames BN. Oxidative decay of DNA. J Biol Chem. 1997;272:19633–6.
• Koptyra M, Cramer K, Slupianek A, et al. BCR/ABL promotes accumulation of chromosomal aberrations induced by oxidative and genotoxic stress. Leukemia. 2008;22:1969–72. This report documents that elevated levels of reactive oxygen species are responsible for accumulation of additional chromosomal aberrations in BCR-ABL1 leukemia cells.
Dierov J, Sanchez PV, Burke BA, et al. BCR/ABL induces chromosomal instability after genotoxic stress and alters the cell death threshold. Leukemia. 2009;23:279–86.
Bernstein C, Bernstein H, Payne CM, et al. DNA repair/pro-apoptotic dual-role proteins in five major DNA repair pathways: fail-safe protection against carcinogenesis. Mutat Res. 2002;511:145–78.
Skorski T. Oncogenic tyrosine kinases and the DNA-damage response. Nat Rev Cancer. 2002;2:351–60.
Naka K, Hoshii T, Muraguchi T, et al. TGF-beta-FOXO signalling maintains leukaemia-initiating cells in chronic myeloid leukaemia. Nature. 2010;463:676–80.
Stoklosa T, Poplawski T, Koptyra M, et al. BCR/ABL inhibits mismatch repair to protect from apoptosis and induce point mutations. Cancer Res. 2008;68:2576–80.
Canitrot Y, Falinski R, Louat T, et al. p210 BCR/ABL kinase regulates nucleotide excision repair (NER) and resistance to ultraviolet (UV) radiation. Blood. 2003;102:2632–7263.
Slupianek A, Schmutte C, Tombline G, et al. BCR/ABL regulates mammalian RecA homologs, resulting in drug resistance. Mol Cell. 2001;8:795–806.
Sallmyr A, Tomkinson AE, Rassool FV. Up-regulation of WRN and DNA ligase IIIalpha in chronic myeloid leukemia: consequences for the repair of DNA double-strand breaks. Blood. 2008;112:1413–23.
Salles D, Mencalha AL, Ireno IC, et al. BCR-ABL stimulates mutagenic homologous DNA double-strand break repair via the DNA-end-processing factor CtIP. Carcinogenesis. 2010;32:27–34.
Nieborowska-Skorska M, Stoklosa T, Datta M, et al. ATR-Chk1 axis protects BCR/ABL leukemia cells from the lethal effect of DNA double-strand breaks. Cell Cycle. 2006;5:994–1000.
Hamilton A, Helgason GV, Schemionek M, et al. Chronic myeloid leukemia stem cells are not dependent on Bcr-Abl kinase activity for their survival. Blood 2011, in press.
Wertheim JA, Forsythe K, Druker BJ, et al. BCR-ABL-induced adhesion defects are tyrosine kinase-independent. Blood. 2002;99:4122–30.
Johansson B, Fioretos T, Mitelman F. Cytogenetic and molecular genetic evolution of chronic myeloid leukemia. Acta Haematol. 2002;107:76–94.
Brain J, Saksena A, Laneuville P. The kinase inhibitor STI571 reverses the Bcr-Abl induced point mutation frequencies observed in pre-leukemic P190(Bcr-Abl) transgenic mice. Leuk Res. 2002;26:1011–6.
Nowak D, Ogawa S, Muschen M, et al. SNP array analysis of tyrosine kinase inhibitor (TKI) resistant chronic myeloid leukemia (CML) identifies heterogeneous secondary genomic alterations. Blood. 2010;115:1049–53.
Jorgensen HG, Allan EK, Jordanides NE, et al. Nilotinib exerts equipotent antiproliferative effects to imatinib and does not induce apoptosis in CD34+ CML cells. Blood. 2007;109:4016–9.
Konig H, Copland M, Chu S, et al. Effects of dasatinib on SRC kinase activity and downstream intracellular signaling in primitive chronic myelogenous leukemia hematopoietic cells. Cancer Res. 2008;68:9624–33.
Fabarius A, Giehl M, Frank O, et al. Induction of centrosome and chromosome aberrations by imatinib in vitro. Leukemia. 2005;19:1573–8.
Jabbour E, Kantarjian HM, Abruzzo LV, et al. Chromosomal abnormalities in Philadelphia chromosome negative metaphases appearing during imatinib mesylate therapy in patients with newly diagnosed chronic myeloid leukemia in chronic phase. Blood. 2007;110:2991–5.
Elrick LJ, Jorgensen HG, Mountford JC, et al. Punish the parent not the progeny. Blood. 2005;105:1862–6.
Acknowledgments
This work was supported in part by grants from the National Cancer Institute CA123014 and CA133646.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Skorski, T. Genetic Mechanisms of Chronic Myeloid Leukemia Blastic Transformation. Curr Hematol Malig Rep 7, 87–93 (2012). https://doi.org/10.1007/s11899-012-0114-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-012-0114-5