Abstract
In recent years, an overlap in biologic and clinical features has been identified between classic Hodgkin lymphoma (CHL) and primary mediastinal large B-cell lymphoma (PMBL). Further strengthening this relationship is the identification of lymphomas with clinical and morphologic features transitional between the two, known as gray zone lymphomas (GZL). However, this diagnostic gray zone is not just of theoretical interest: it presents a practical problem, as the treatment approaches for CHL traditionally differ from those for aggressive B-cell lymphomas. This article reviews the treatment approach for mediastinal lymphomas, including CHL of the nodular sclerosis subtype (CHL-NS), PMBL, and mediastinal GZL. Though several trials have evaluated different regimens with or without radiation in PMBL and CHL-NS, there is a lack of prospective experience in treating GZL because of the rarity of these tumors. Historical data indicate that they have done poorly with traditional approaches developed for the treatment of either CHL or diffuse large B-cell lymphoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the era of modern immunophenotypic and molecular genetic techniques, most cases of lymphoma can be diagnosed and classified as one of the currently recognized distinct disease entities. There are some lymphomas, however, with histologic, biologic, and clinical features overlapping between various types of lymphomas. The 4th edition of the World Health Organization (WHO) Classification of Tumours of Haematopoietic and Lymphoid Tissues in 2008 recognized these problematic cases for the first time and in so doing included the category “B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and classical Hodgkin lymphoma,” known more commonly as “gray zone lymphoma” (GZL) [1••] (Table 1).
Interrelationships among mediastinal lymphomas. Primary mediastinal large B-cell lymphoma (PMBL), classic Hodgkin lymphoma of the nodular sclerosis subtype (CHL-NS), and mediastinal gray zone lymphomas are all thought to be derived from a thymic B cell. In a given patient, differing histologic patterns can be seen at different times, suggesting plasticity in tumor cell phenotype and gene expression. Composite lymphomas of CHL-NS and PMBL may also be seen
The term “gray zone lymphoma” has been generically used to denote a group of lymphomas at the histologic and biologic interface between various lymphomas [2]. It has been used in the context of classic Hodgkin lymphoma (CHL) and non-Hodgkin lymphoma (NHL), as well as in nodular lymphocyte-predominant Hodgkin lymphoma (NHPHL) and B-cell lymphomas, most commonly T-cell/histiocyte-rich large B-cell lymphoma (TCHRLBCL). Equally, synchronous and metachronous lymphomas of discordant histologies can involve a combination of HL and NHL. An analogous but unrelated issue involves cases in which there may be diagnostic uncertainty but not true biologic overlap, such as Hodgkin/Reed Sternberg (HRS)—like cells encountered in both benign and malignant conditions. For the purposes of this review, we will limit the use of the term “gray zone lymphoma” to those cases in which morphologic, biologic, and clinical features suggest overlap between primary mediastinal B-cell lymphoma (PMBL), a subtype of diffuse large B-cell lymphoma (DLBCL), and CHL (Fig. 1).
Significant advances have been made in recent years regarding the origin of the neoplastic cell in CHL, the Hodgkin/Reed-Sternberg cell (HRS). Recent evidence shows that it is a B cell in all or nearly all cases. It is not surprising, therefore, if CHL is derived from an altered B lymphocyte, that areas of overlap with B-cell NHL should occur both biologically and clinically [3]. The HRS cell is a crippled B cell, incapable of immunoglobulin secretion and, with additional suppression, of many other aspects of the B-cell program [4•]. The biologic and molecular events leading to this state are complex and not fully resolved [5, 6]. These events may occur in the context of a relatively normal immune system, as seen in most patients with CHL, or in the setting of immunodeficiency [7–11]. The study of lymphomas at the interface of CHL and NHL may provide insight into the pathogenesis of de novo CHL and the molecular and cellular events distinguishing it from NHL.
Clinical Presentation
PMBL and CHL of the nodular sclerosis subtype (CHL-NS) have a number of clinical characteristics in common. Both tend to present in the third to fourth decade of life with a female predominance. The tumor is usually a bulky anterior mediastinal mass involving the thymus gland. Superior vena caval syndrome is seen frequently in PMBL, but it is much less common in CHL. Both synchronous and metachronous presentations of PMBL and CHL-NS have been reported in the literature [12]. GZL has a male predominance, but its similarity to PMBL and CHL in presentation further accentuates the close relationship between these lymphomas [12].
Morphologic and Immunophenotypic Features
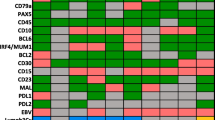
As previously described, PMBL and CHL-NS have strikingly similar clinical presentations with some morphologic overlap, but importantly for diagnostic purposes, they have several non-overlapping, distinctive pathologic features. The diagnosis of CHL-NS is typified by a nodular growth pattern with broad bands of fibrosis and lacunar variants of HRS cells that have a characteristic immunophenotype. The cells are positive for CD30, negative for CD45, and positive for CD15 in 85% of cases. Expression of B-cell–associated antigens is weak and heterogeneous in the neoplastic cells of CHL, with often negative CD79a, weak or variable CD20 expression, and weak expression of PAX5 [13, 14]. Immunoglobulin expression is absent, and transcription factors governing immunoglobulin production, such as OCT2 and BOB1, are frequently negative [15, 16].
PMBL was first described from a review of 184 adult NHL cases in 1980. A cohort of 17 cases that presented as a mediastinal mass with diffuse aggressive histology was identified [17]. The features of PMBL have been well characterized since then [18–20]. Histologically, this lymphoma is characterized by an infiltrate of large cells with round or lobulated nuclei and abundant clear cytoplasm. There is background fine, compartmentalizing sclerosis. Occasional HRS-like cells can be seen, and although the architecture is usually diffuse, a minority of cases (30%) may show focal nodularity. Necrosis, a characteristic feature of CHL, is seen in 25% of cases [21]. The immunophenotype of PMBL resembles that of a mature B cell expressing CD20 and pan–B-cell markers such as CD79a, but interestingly, the tumor cells lack surface immunoglobulin expression, unlike most B-cell neoplasms [22, 23]. The B-cell–associated transcription factors PAX5, BOB1, and OCT2 are strongly expressed [23]. CD30 is expressed in most cases, although the intensity varies [18, 21]. The cells are variably positive for the germinal center markers CD10 and BCL6, and CD23 is positive in over 85% of cases, suggesting a thymic B-cell origin [24, 25].
GZL presents with pleomorphic tumor cells that often sheet-out and grow in a diffusely fibrotic stroma. Tumor cells can be reminiscent of PMBL or CHL, with a broad spectrum of cytologic appearance in different areas of the tumor. Clusters of cells similar to lacunar cells or even HRS cells may be seen in a background resembling PMBL. The inflammatory infiltrate is usually sparse, but scattered eosinophils, lymphocytes, and histiocytes may be present. The immunophenotypic features of GZL are also intermediate [12, 26]. Neoplastic cells typically express CD45. CD20 and CD79a are frequently positive on the majority of tumor cells. CD30 is positive and CD15 may be expressed as well. Immunoglobulin expression is absent, resembling both CHL and PMBL. The transcription factors PAX5, OCT2, and BOB1 are positive in most cases, but the tumor cells can present a pattern with transitional features between CHL and PMBL, particularly with asynchrony between morphology and immunophenotype. GZL can present with a Hodgkin-like morphology and a phenotypic pattern of PMBL (CD20++, CD15-). Alternatively, the lymphoma can present with a PMBL-like morphology and a Hodgkin phenotype, with expression of CD30 and CD15 and loss of CD20 and CD79a.
A related phenomenon, but technically not considered a form of GZL, is composite lymphoma, with some areas resembling CHL and other areas showing sheets of large B cells characteristic of PMBL. The inflammatory background and pattern of sclerosis usually correspond to the appearance of the neoplastic cells, resembling either CHL or PMBL, respectively [1••].
Biologic Characteristics
From a biologic perspective, gene expression profiling studies have revealed that PMBL and CHL-NS share a common gene expression signature [27, 28]. Additionally, a number of common genetic aberrations in PMBL and CHL further underscore their close relationship [29]. PMBLs show frequent gains of gene regions on chromosome 9p and 2p that were also described in CHL but have rarely been detected in other DLBCLs. A recent study of chromosomal aberrations for 2p16.1, 9p24.1, and 8q24 in children with PMBL found that the frequencies of investigated loci were similar to those in adults [30••]. Of note, one case of pediatric GZL that was accessible for genetic studies did not reveal any alterations.
The exact molecular mechanisms responsible for the transformation of a B cell to an HRS cell are not fully understood. Recent studies have suggested that downregulation of the B-cell program in CHL may be responsible for tumorigenesis, and these modifications may be controlled at the epigenetic level [31, 32•]. GZLs, mediastinal composite lymphomas, and mediastinal sequential lymphomas represent a unique resource to study this question, as the cells appear to be able to undergo re-programming of their phenotype during the disease course. A recent large-scale methylation analysis showed a close epigenetic relationship between GZL, CHL-NS, and PMBL, but remarkable differences from DLBCL. Moreover, principal component analysis indicated that GZL did not cluster with either CHL or PMBL; it demonstrated a unique epigenetic signature for GZL, validating its inclusion in the WHO classification as a separate disease [33••]. Importantly, GZL could be distinguished from CHL-NS and PMBL by differential methylation of selected CpG islands, and a class prediction model could be established to segregate the various entities. Thus, the epigenetic signature of these lymphoma entities not only may be useful in establishing new diagnostic tools and in clarifying the pathogenesis of these lymphomas, but also may help to identify possible targets for future therapies. Although material is limited because of the rarity of GZL, further studies are urgently needed to explore this entity in more detail. Gene expression profiling and cytogenetic or molecular genetic studies may be of value for a more comprehensive understanding of disease pathogenesis and for establishing new and more effective therapies for those patients.
Clinical Management
Though much progress has been made recently in better defining and elucidating mediastinal lymphomas, their histologic and molecular heterogeneity poses a clinical challenge. Several trials have evaluated different regimens with or without radiation in PMBL and CHL-NS, but there is a lack of prospective experience in treating GZL because of the rarity of these tumors. Some perspective may be gained from treatment results reported for “anaplastic large-cell lymphoma Hodgkin-like”—many of which cases today would be classified as “GZL” or “B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and classical HL.” Prior reports indicated that these cases responded poorly to standard therapy approaches [1••, 34].
Nodular Sclerosis Hodgkin Lymphoma
Most studies that have investigated outcome in CHL-NS have not specifically evaluated patients presenting with mediastinal disease, but have included different disease sites. One early study did evaluate 80 patients with bulky mediastinal disease who were treated with six cycles of MOPP (mechlorethamine, vincristine, procarbazine, and prednisone)/ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine) followed by mantle-field radiation therapy [35]. This was an effective treatment for this group, and at 15 years’ follow-up, the disease-free survival was 76% in those with stage I or II disease. Another study evaluating MOPP alone in massive mediastinal disease demonstrated a very high relapse rate and suggested that these patients should be treated with combined-modality therapy [36]. Some later studies, after the time that ABVD was considered standard, compared ABVD alone versus ABVD with radiation in patients with nonbulky disease. One such study, by Straus et al., evaluated 152 untreated, unselected Hodgkin lymphoma patients with clinical stage 1A, 1B, IIA, IIB, and IIIA nonbulky disease, prospectively randomizing them to six cycles of ABVD alone or six cycles of ABVD followed by radiation [37]. At 60 months, rates of complete remission were similar between the two groups, and there was no statistically significant difference in freedom from progression or overall survival (OS). Another study, done by the National Cancer Institute of Canada Clinical Trials Group and the Eastern Cooperative Oncology Group, prospectively compared ABVD chemotherapy alone versus combined-modality therapy in 399 patients with nonbulky stage I to stage IIA disease [38]. At 4 years’ follow-up, there was no difference in OS, but freedom from disease progression was superior in the patients allocated to radiation therapy. Though neither study specifically enrolled patients with mediastinal presentations and both included other sites of disease, the Straus study suggests that patients with nonbulky disease may do well with chemotherapy alone [37]. Interestingly, although the rate of disease progression in the other study was higher in the arm treated with ABVD alone, this advantage was offset by deaths from other causes in the radiation arm [38].
At this time, combined-modality therapy is standard for the treatment of early-stage, bulky mediastinal disease. For patients with nonbulky mediastinal disease, optimal therapy is more controversial. There is emerging evidence that chemotherapy alone may be adequate, though some studies suggest a slightly higher relapse rate than for patients who receive consolidation radiation. This potential increased risk of relapse must be offset by the serious long-term effects from radiation treatment, such as breast cancer and secondary tumors, and by the high salvageability of patients with relapse [39]. In addition, these studies were done without the incorporation of FDG-PET imaging; a number of new clinical trials are currently evaluating its role in identifying patients who may not need radiation treatment. As CHL-NS appears to be responsive to dose intensity, studies are also ongoing using more intense chemotherapy regimens, which may obviate the need for radiation [40].
Primary Mediastinal B-cell Lymphoma
Just like CHL-NS, PMBL also has a predilection for young females and tends to stay confined to the mediastinum. It has historically been associated with a good outcome, although most patients are managed with combined-modality therapy and the use of mediastinal radiation brings with it a high risk of secondary tumors and cardiac complications, as with CHL-NS. Early studies evaluating chemotherapy in PMBL suggested that most patients required consolidation radiation. In one of these studies, 50 untreated patients received MACOP-B (methotrexate, leucovorin, doxorubicin, cyclophosphamide, vincristine, prednisone, bleomycin) and at the end of therapy, 66% had persistently positive gallium scans, suggesting active disease. Following consolidation radiotherapy, however, only 19% of patients had a positive gallium scan, and 80% were event-free at 39 months’ median follow-up [41]. This study suggested that radiotherapy was necessary following chemotherapy, and most approaches that were investigated subsequently involved the empiric use of consolidation radiation. As regards the optimal regimen for this disease, MACOP-B and VACOP-B (etoposide, doxorubicin, cyclophosphamide, vincristine, prednisone, bleomycin) in a retrospective analysis yielded a superior outcome compared to CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone), suggesting that dose intensity may be important in PMBL [42]. Most of these studies were done in the era before rituximab, however. Since then, a number of studies have examined the impact on outcome of adding rituximab to chemotherapy. A recent subgroup analysis of the prospective, randomized, phase III Mabthera International Trial (MInT) examined the role of rituximab in combination with CHOP-like regimens for PMBL outcomes. The rituximab arm was clearly superior in terms of 3-year event-free survival (78% vs 52% in the chemotherapy-alone arm), but no statistically significant difference in OS was detected because of small numbers [43]. Of importance in interpreting these data, however, is the fact that preplanned radiotherapy was administered to 67% of patients in the chemotherapy arm and 73% in the rituximab arm. Currently, the standard treatment for PMBL consists of immunochemotherapy, with regimens like R-CHOP, followed by involved-field radiation, but the outcome remains suboptimal because of treatment failure in up to 25% of patients.
Based on evidence that dose intensity is important in PMBL, DA-EPOCH-R (Dose-adjusted etoposide, vincristine, doxorubicin, cyclophosphamide, prednisone, rituximab), a dose-intense regimen without radiation treatment, has been investigated [44–46]. In a recent update of 40 patients with untreated PMBL, the event-free survival was 95% and OS was 100%. Only two patients required consolidation radiation treatment, and no patients have relapsed [47]. More than 50% of patients had bulky disease. These results suggest that DA-EPOCH-R obviates the need for radiation in almost all patients with PMBL, thus eliminating the risk of associated long-term toxicities.
Mediastinal Gray Zone Lymphoma
Because of their rarity and relatively recent recognition, only one prospective study has reported the outcome of these mediastinal lymphomas, which have features intermediate between PMBL and CHL-NS [47]. Historically, these diseases (often included under the diagnosis of “anaplastic large-cell lymphoma Hodgkin-like”) have had a poor clinical outcome and short median survivals with standard therapy [34]. In one retrospective study, in which patients received either a CHL or NHL regimen, the 5-year event-free survival was inferior to that reported by the International Database on Hodgkin’s Disease for CHL, suggesting that they had more chemoresistant biology [34]. In one updated report, 16 patients with GZL treated prospectively with the DA-EPOCH-R regimen—despite clinical characteristics similar to those of the PMBL cohort—had a significantly inferior event-free survival (45%) and OS (75%) at a median follow-up of 4 years, and 37% required consolidation mediastinal radiation [47]. Studies are under way to explore the biologic basis for their poor clinical responsiveness; factors may include bulky disease and poor vascularization of these large tumors, which often have extensive areas of necrosis. It is hoped that improved biologic insights may lead to the development of more effective therapies. Recent studies provide some insights into the mechanisms involved in modulating the plasticity of the neoplastic B cell [33••], and the tumor microenvironment is also an emerging prognostic factor in lymphomas, including CHL [48••, 49]. Moreover, having new biologic tools to diagnose GZL could help to accurately identify those patients requiring distinctive management.
Conclusions
The overlapping clinical, morphologic, and immunophenotypic features of CHL-NS, PMBL, and GZL emphasize the close clinicopathologic relationship between these mediastinal B-cell lymphomas and their likely derivation from a thymic B cell. Molecular profiling studies have confirmed that PMBL and CHL-NS share a third of their genes and furthermore provide evidence that they are related diseases at opposite ends of a continuum, between which lie “gray zone lymphomas” with features intermediate between both entities. Despite these similarities, there are fundamental differences between these lymphomas with respect to their biology and clinical differences in terms of their response to therapy and their prognosis with standard therapies.
The outcome for patients with PMBL who receive the DA-EPOCH-R regimen is now excellent, and it obviates the need for radiation treatment in almost all patients. Patients with bulky mediastinal CHL-NS should receive combined-modality therapy in the absence of evidence that radiation can be avoided, but future strategies in clinical trials should focus on obviating its need. There is controversy regarding the optimal management of nonbulky CHL-NS, but some studies suggest that chemotherapy alone may be feasible, and this is also being evaluated prospectively. GZLs appear to be biologically more similar to CHL-NS, and they have a relatively poor outcome with both HL and NHL regimens. Currently, for CD20-positive GZL, immunochemotherapy with rituximab followed by radiation treatment is a reasonable approach.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance•• Of major importance
•• Campo E, Swerdlow SH, Harris NL, et al. The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications. Blood. Feb 7 2011 (Epub ahead of print). This review discusses new concepts introduced into the 2008 WHO classification, including the concept of mediastinal gray zone lymphomas.
Rudiger T, Jaffe ES, Delsol G, et al. Workshop report on Hodgkin’s disease and related diseases (‘grey zone’ lymphoma). Ann Oncol. 1998;9 Suppl 5:S31–8.
Jaffe ES, Zarate-Osorno A, Medeiros LJ. The interrelationship of Hodgkin’s disease and non-Hodgkin’s lymphomas–lessons learned from composite and sequential malignancies. Semin Diagn Pathol. 1992;9:297–303.
• Kuppers R. The biology of Hodgkin’s lymphoma. Nat Rev Cancer 2009;9:15–27. This article is an excellent review on the biology of Hodgkin’s lymphoma.
Kanzler H, Kuppers R, Hansmann ML, Rajewsky K. Hodgkin and Reed-Sternberg cells in Hodgkin’s disease represent the outgrowth of a dominant tumor clone derived from (crippled) germinal center B cells. J Exp Med. 1996;184:1495–505.
Stein H, Marafioti T, Foss HD, et al. Down-regulation of BOB.1/OBF.1 and Oct2 in classical Hodgkin disease but not in lymphocyte predominant Hodgkin disease correlates with immunoglobulin transcription. Blood. 2001;97:496–501.
Andrieu JM, Roithmann S, Tourani JM, et al. Hodgkin’s disease during HIV1 infection: the French registry experience. French Registry of HIV-associated Tumors. Ann Oncol. 1993;4:635–41.
Levine AM. Hodgkin’s disease in the setting of human immunodeficiency virus infection. J Natl Cancer Inst Monogr 1998:37–42.
Bellas C, Santon A, Manzanal A, et al. Pathological, immunological, and molecular features of Hodgkin’s disease associated with HIV infection. Comparison with ordinary Hodgkin’s disease. Am J Surg Pathol. 1996;20:1520–4.
Kamel OW, Weiss LM, van de Rijn M, Colby TV, Kingma DW, Jaffe ES. Hodgkin’s disease and lymphoproliferations resembling Hodgkin’s disease in patients receiving long-term low-dose methotrexate therapy. Am J Surg Pathol. 1996;20:1279–87.
Kumar S, Fend F, Quintanilla-Martinez L, et al. Epstein-Barr virus-positive primary gastrointestinal Hodgkin’s disease: association with inflammatory bowel disease and immunosuppression. Am J Surg Pathol. 2000;24:66–73.
Traverse-Glehen A, Pittaluga S, Gaulard P, et al. Mediastinal gray zone lymphoma: the missing link between classic Hodgkin’s lymphoma and mediastinal large B-cell lymphoma. Am J Surg Pathol. 2005;29:1411–21.
Schmid C, Pan L, Diss T, Isaacson PG. Expression of B-cell antigens by Hodgkin’s and Reed-Sternberg cells. Am J Pathol. 1991;139:701–7.
Zukerberg LR, Collins AB, Ferry JA, Harris NL. Coexpression of CD15 and CD20 by Reed-Sternberg cells in Hodgkin’s disease. Am J Pathol. 1991;139:475–83.
Loddenkemper C, Anagnostopoulos I, Hummel M, et al. Differential Emu enhancer activity and expression of BOB.1/OBF.1, Oct2, PU.1, and immunoglobulin in reactive B-cell populations, B-cell non-Hodgkin lymphomas, and Hodgkin lymphomas. J Pathol. 2004;202:60–9.
Foss HD, Reusch R, Demel G, et al. Frequent expression of the B-cell-specific activator protein in Reed-Sternberg cells of classical Hodgkin’s disease provides further evidence for its B-cell origin. Blood. 1999;94:3108–13.
Lichtenstein AK, Levine A, Taylor CR, et al. Primary mediastinal lymphoma in adults. Am J Med. 1980;68:509–14.
Higgins JP, Warnke RA. CD30 expression is common in mediastinal large B-cell lymphoma. Am J Clin Pathol. 1999;112:241–7.
Moller P, Lammler B, Eberlein-Gonska M, et al. Primary mediastinal clear cell lymphoma of B-cell type. Virchows Arch A Pathol Anat Histopathol. 1986;409:79–92.
Paulli M, Strater J, Gianelli U, et al. Mediastinal B-cell lymphoma: a study of its histomorphologic spectrum based on 109 cases. Hum Pathol. 1999;30:178–87.
Pileri SA, Zinzani PL, Gaidano G, et al. Pathobiology of primary mediastinal B-cell lymphoma. Leuk Lymphoma. 2003;44 Suppl 3:S21–6.
Moller P, Moldenhauer G, Momburg F, et al. Mediastinal lymphoma of clear cell type is a tumor corresponding to terminal steps of B cell differentiation. Blood. 1987;69:1087–95.
Pileri SA, Gaidano G, Zinzani PL, et al. Primary mediastinal B-cell lymphoma: high frequency of BCL-6 mutations and consistent expression of the transcription factors OCT-2, BOB.1, and PU.1 in the absence of immunoglobulins. Am J Pathol. 2003;162:243–53.
Calaminici M, Piper K, Lee AM, Norton AJ. CD23 expression in mediastinal large B-cell lymphomas. Histopathology. 2004;45:619–24.
Salama ME. Rajan Mariappan M, Inamdar K, Tripp SR, Perkins SL. The value of CD23 expression as an additional marker in distinguishing mediastinal (thymic) large B-cell lymphoma from Hodgkin lymphoma. Int J Surg Pathol. 2010;18:121–8.
Garcia JF, Mollejo M, Fraga M, et al. Large B-cell lymphoma with Hodgkin’s features. Histopathology. 2005;47:101–10.
Rosenwald A, Wright G, Leroy K, et al. Molecular diagnosis of primary mediastinal B cell lymphoma identifies a clinically favorable subgroup of diffuse large B cell lymphoma related to Hodgkin lymphoma. J Exp Med. 2003;198:851–62.
Savage KJ, Monti S, Kutok JL, et al. The molecular signature of mediastinal large B-cell lymphoma differs from that of other diffuse large B-cell lymphomas and shares features with classical Hodgkin lymphoma. Blood. 2003;102:3871–9.
Green MR, Monti S, Rodig SJ, et al. Integrative analysis reveals selective 9p24.1 amplification, increased PD-1 ligand expression, and further induction via JAK2 in nodular sclerosing Hodgkin lymphoma and primary mediastinal large B-cell lymphoma. Blood. 2010;116:3268–77.
•• Oschlies I, Burkhardt B, Salaverria I, et al. Clinical, pathological and genetic features of primary mediastinal large B-cell lymphomas and mediastinal gray zone lymphomas in children. Haematologica 2011;96:262–8. This is a recent clinical study of mediastinal lymphomas in children, and is a useful comparison with the adult experience.
Hertel CB, Zhou XG, Hamilton-Dutoit SJ, Junker S. Loss of B cell identity correlates with loss of B cell-specific transcription factors in Hodgkin/Reed-Sternberg cells of classical Hodgkin lymphoma. Oncogene. 2002;21:4908–20.
• Ehlers A, Oker E, Bentink S, Lenze D, Stein H, Hummel M. Histone acetylation and DNA demethylation of B cells result in a Hodgkin-like phenotype. Leukemia 2008;22:835–41. This study provides insight into mechanisms of inducing a Hodgkin’s-like phenotype through gene methylation and gene silencing.
•• Eberle FC, Rodriguez-Canales J, Wei L, et al. Methylation profiling of mediastinal gray zone lymphoma reveals a distinctive signature with elements shared by classical Hodgkin’s lymphoma and primary mediastinal large B-cell lymphoma. Haematologica 2011;96:558–66. This is the first biological study of gray zone lymphomas. It provides insight into the plasticity of immunophenotype and morphology of these tumors, and their transitional appearance.
Cazals-Hatem D, Andre M, Mounier N, et al. Pathologic and clinical features of 77 Hodgkin’s lymphoma patients treated in a lymphoma protocol (LNH87): a GELA study. Am J Surg Pathol. 2001;25:297–306.
Longo DL, Glatstein E, Duffey PL, et al. Alternating MOPP and ABVD chemotherapy plus mantle-field radiation therapy in patients with massive mediastinal Hodgkin’s disease. J Clin Oncol. 1997;15:3338–46.
Longo DL, Russo A, Duffey PL, et al. Treatment of advanced-stage massive mediastinal Hodgkin’s disease: the case for combined modality treatment. J Clin Oncol. 1991;9:227–35.
Straus DJ, Portlock CS, Qin J, et al. Results of a prospective randomized clinical trial of doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) followed by radiation therapy (RT) versus ABVD alone for stages I, II, and IIIA nonbulky Hodgkin disease. Blood. 2004;104:3483–9.
Meyer RM, Gospodarowicz MK, Connors JM, et al. Randomized comparison of ABVD chemotherapy with a strategy that includes radiation therapy in patients with limited-stage Hodgkin’s lymphoma: National Cancer Institute of Canada Clinical Trials Group and the Eastern Cooperative Oncology Group. J Clin Oncol. 2005;23:4634–42.
Castellino SM, Geiger AM, Mertens AC, et al. Morbidity and mortality in long-term survivors of Hodgkin lymphoma: a report from the Childhood Cancer Survivor Study. Blood. 2011;117:1806–16.
Diehl V, Franklin J, Pfreundschuh M, et al. Standard and increased-dose BEACOPP chemotherapy compared with COPP-ABVD for advanced Hodgkin’s disease. N Engl J Med. 2003;348:2386–95.
Zinzani PL, Martelli M, Magagnoli M, et al. Treatment and clinical management of primary mediastinal large B-cell lymphoma with sclerosis: MACOP-B regimen and mediastinal radiotherapy monitored by (67)Gallium scan in 50 patients. Blood. 1999;94:3289–93.
Todeschini G, Secchi S, Morra E, et al. Primary mediastinal large B-cell lymphoma (PMLBCL): long-term results from a retrospective multicentre Italian experience in 138 patients treated with CHOP or MACOP-B/VACOP-B. Br J Cancer. 2004;90:372–6.
Rieger M, Osterborg A, Pettengell R, et al. Primary mediastinal B-cell lymphoma treated with CHOP-like chemotherapy with or without rituximab: results of the Mabthera International Trial Group study. Ann Oncol. 2011;22:664–70.
Wilson WH, Grossbard ML, Pittaluga S, et al. Dose-adjusted EPOCH chemotherapy for untreated large B-cell lymphomas: a pharmacodynamic approach with high efficacy. Blood. 2002;99:2685–93.
Wilson WH, Gutierrez M, O’Connor P, et al. The role of rituximab and chemotherapy in aggressive B-cell lymphoma: a preliminary report of dose-adjusted EPOCH-R. Semin Oncol. 2002;29:41–7.
Dunleavy K, Pittaluga S, Tay K, et al. Comparative clinical and biological features of primary mediastinal B-cell lymphoma (PMBL) and mediastinal grey zone lymphoma (MGZL). ASH Annual Meeting Abstracts. 2009;114:106.
Dunleavy K, Pittaluga S, Shovlin M. Untreated Primary Mediastinal B-cell (PMBL) and Mediastinal Grey Zone (MGZL) Lymphomas: Comparison of biological features and clinical outcome following DA-EPOCH-R without radiation [abstract]. Submitted, 11th International Conference on Malignant Lymphoma, Lugano; 2011.
•• Steidl C, Lee T, Shah SP, Farinha P, et al. Tumor-associated macrophages and survival in classic Hodgkin’s lymphoma. N Engl J Med 2010;362:875–85. This study explores the importance of tumor microenvironment in classic Hodgkin’s lymphoma and shows that tumor-associated macrophages are prognostically relevant.
Steidl C, Shah SP, Woolcock BW, et al. MHC class II transactivator CIITA is a recurrent gene fusion partner in lymphoid cancers. Nature. 2011;471(7338):377–81.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Additional information
The article project number is a Z01 number ZIA SC 000550 for intramural studies.
Rights and permissions
About this article
Cite this article
Grant, C., Dunleavy, K., Eberle, F.C. et al. Primary Mediastinal Large B-Cell Lymphoma, Classic Hodgkin Lymphoma Presenting in the Mediastinum, and Mediastinal Gray Zone Lymphoma: What is the Oncologist To Do?. Curr Hematol Malig Rep 6, 157–163 (2011). https://doi.org/10.1007/s11899-011-0090-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-011-0090-1