Abstract
Purpose of Review
Secondary sclerosing cholangitis is an emerging entity. Yet, because of the low incidence and varying etiologies of this disease, the literature is not robust. There are mainly case reports and small studies evaluating the disease. Our aim in this review is to bring the reader up to date with recent literature on secondary sclerosing cholangitis including the disease presentation, course, prognosis, and treatment options.
Recent Findings
Numerous case reports have been published the last 5 years on secondary sclerosing cholangitis. We have divided them into infectious, drug-induced, ischemic, obstructive, and autoimmune etiologies. The bulk of the literature describes secondary sclerosing cholangitis in the critically ill patient.
Summary
Secondary sclerosing cholangitis due to drugs or autoimmune causes seem to have the best prognosis. However, causes such as critical illness seem to have worse outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
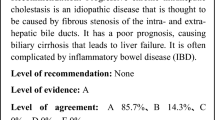
Sclerosing cholangiopathies, while rare, are becoming increasingly more recognized and described in the literature. They represent a number of variably progressive cholestatic diseases of the intrahepatic and/or extrahepatic ducts. Primary sclerosing cholangitis (PSC) is an idiopathic disease, often difficult to treat. Before making this diagnosis though, it is imperative to rule out secondary etiologies. Secondary sclerosing cholangitis (SSC) has an identifiable, sometimes reversible cause. Over the recent years, more sub-groups are being described as secondary etiologies. Most prominent appears to be immunoglobulin-G4 (IgG4)-positive sclerosing cholangitis (IgG4-SC). This is an inflammatory disease of the biliary tree characterized by elevated IgG4 levels and infiltration of IgG4+ plasma cells into the bile duct walls [1]. It seems to be another manifestation of IgG4-related disease and likely a separate entity, as suggested by the American Association for the Study of Liver Diseases [2]. For the purpose of this paper, we will not discuss IgG4-SC in detail. Instead, we will focus our efforts on the other etiologies of SSC.
SSC is a chronic disease characterized by biliary obstruction. It can be caused by infectious, immune-mediated, toxic, obstructive, or ischemic injury. A variety of specific etiologies have been identified in the past. The clinical outcomes are actually less favorable than PSC if not diagnosed in a timely manner [3].
This discussion will center on recent literature since 2012, although we will include some background as well. Many case reports have been published on SSC. However, the bulk of recent literature has been focused on sclerosing cholangitis in critically ill patients (SSC-CIP). This is a new, emerging etiology of sclerosing cholangitis that will be discussed in more length.
Etiology
There are a host of factors that can lead to SSC. Varying etiologies all seem to lead to chronic inflammation causing the sclerosing cholangitis. These include infections, drugs, ischemia, obstruction, and autoimmune disease (listed in Table 1). Table 1 is not an exhaustive list, but more reflects recent literature, which is what we will focus on below.
Choledochoduodenal Fistula
There have been two case reports of patients with choledochoduodenal fistula (CDF) developing SSC, which have not been described in the literature before. One patient was a 58-year-old man with prior manipulation of the common bile duct with a choledocholithotomy during open cholecystectomy. The following year he received living donor renal transplantation for diabetic nephropathy. Five months after transplant, he developed recurrent cholangitis. CDF was found on cholangiography and sclerosing cholangitis was proven on liver and bile duct biopsies. Within a year, the patient required deceased donor liver transplantation [4].
The other case involved a 27-year-old woman with Down’s syndrome and Celiac disease who presented with recurrent cholangitis. An upper endoscopy showed a duodenal bulb ulcer with stenosis at the duodenal sweep. There was evidence of a CDF on cholangiogram, as well as intrahepatic strictures suggestive of SSC. She underwent a Roux-en-Y hepaticojejunostomy, truncal vagotomy, antrectomy, and gastrojejunostomy to resolve her disease [5].
Echinococcosis
Prior case series have shown Echinococcus granulosus, or cystic hydatid disease, causing SSC. A group from Switzerland performed a retrospective study on patients with human alveolar echinococcosis (AE), which is caused by Echinococcus multilocularis, and a separate entity from cystic hydatid disease. Surgery can be part of first-line therapy in AE. In this study, investigators found that in those patients with unresected AE requiring benzimidazole therapy, 28% developed late biliary complications. SSC was defined as biliary disease occurring at least 3 years after initial diagnosis of AE. Potential risk factors of any liver surgery and length of benzimidazole therapy were identified by Pearsons’ correlation and linear regression analysis [6].
Drug-Induced
There have been a number of medications linked to SSC in the past, mostly as case reports. We describe a few below. One recent paper looked retrospectively at patients with drug-induced liver injury (DILI) to see if any had SSC. Investigators identified 102 patients with possible causal relationship of liver injury with an identified drug. Magnetic resonance cholangiopancreatography (MRCP) was performed in 25 patients. Ten patients (40% of those with MRCP) were found to have duct abnormalities. Four patients had only extrahepatic duct abnormalities, and six had both intrahepatic and extrahepatic duct abnormalities. Endoscopic retrograde cholangiopancreatography (ERCP) was performed in five patients, with similar findings to MRCP. Four of these patients underwent a liver biopsy, which was reported as changes compatible with DILI with histological features of cholestasis. The following drugs were implicated: amoxicillin-clavulanate (n = 3), sevoflurane (n = 2), amiodarone, infliximab, green tea extract, venlafaxine, and atorvastatin. All but one of these possible SSC patients had normal liver tests by the end of follow-up [7].
Chronic ketamine use has been described to cause SSC in a case series [8]. A case report was published in 2013, which detailed a 21-year-old man with chronic ketamine use who developed recurrent abdominal pain, fevers, and abnormal liver studies (mainly cholestatic liver injury). It should be noted that the patient had recurrent acute pyelonephritis as well. Nonetheless, a liver biopsy showed evidence of sclerosing cholangitis and no other etiology was identified. Liver tests improved with cessation of ketamine, leading the authors to believe this was the cause [9].
Celecoxib has been reported to cause biliary disease in case reports, including one patient requiring liver transplantation [10]. In 2013, a case report was published about a 34-year-old woman who presented with acute epigastric abdominal pain after using celecoxib for 3 weeks. Liver tests were noted to be abnormal with a mixed picture, including a total bilirubin of 3.4 units/L. No clear etiology was found on her initial workup, but a follow-up liver biopsy suggested sclerosing cholangitis. Her liver tests normalized 1 month after cessation of the drug, leading the authors to believe this was due to celecoxib [11].
Sclerosing cholangitis has been reported in patients treated with transcatheter arterial chemoembolization (TACE) with bleomycin-iodinated oil for liver cavernous hemangioma. Even though rare, a case report was published in 2014. The case involved a 44-year-old woman who underwent TACE with bleomycin-iodinated oil for liver cavernous hemangioma. Six years after treatment, she developed obstructive jaundice. Imaging studies showed a biliary stricture at the convergence of the left and right hepatic duct with right lobe atrophy. Exploratory surgery revealed the stricture, and suspected biliary malignancy. The patient underwent radical hepatic hilar resection, right side hemihepatectomy and Roux-en-Y hepaticojejunostomy. Surgical pathology showed sclerosing cholangitis in the portal area with no malignancy. The etiology was therefore thought to be due to TACE with bleomycin-iodinated oil [12].
Gallbladder Adenocarcinoma
A case report from 2013 described a 55-year-old man with SSC thought to be secondary to metastatic gallbladder adenocarcinoma. He presented with acute-onset lower back pain, abdominal pain, weight loss, and jaundice. He was found to have a primarily cholestatic liver injury with a total bilirubin of 7.7 mg/dl. Imaging studies showed a mass in the fundus of the gallbladder with portal and celiac lymphadenopathy, and no extrahepatic or intrahepatic duct dilation. An endoscopic ultrasound performed with fine needle aspiration of lymph nodes found adenocarcinoma, believed to be from the gallbladder mass. A subsequent liver biopsy showed benign tissue with evidence of biliary cholestasis. An ERCP was performed revealing multiple and severe diffuse strictures in the intrahepatic ducts suggestive of sclerosing cholangitis. The authors concluded that the SSC was due to the metastatic gallbladder adenocarcinoma [13].
Autoimmune Disease
Autoimmune disorders have been associated with SSC in the past, with minimal literature produced. Two recent publications described Behcet disease and sarcoidosis as causes of SSC. A case report published in 2013 details a 43-year-old man with a history of Behcet disease with recurrent thrombophlebitis who presented with acute-onset painless jaundice. Total bilirubin was 123 μmol/L on presentation. MRCP showed distension of the intrahepatic bile ducts with some distension and thickening zones of the main bile duct. A liver biopsy revealed cholestasis and fibrosis of portal spaces. Since other workup was negative, it was thought this was SSC. An ERCP revealed stenosis of the distal main bile duct and plastic stenting was performed. Ursodeoxycholic acid treatment was initiated. After the plastic stent was removed, the patient was followed up for 3 years with no recurrence of symptoms. The patient’s liver tests and imaging normalized [14].
Sarcoidosis commonly affects the liver, but there is only one prior report of necrotizing sarcoid granuloma involving the liver. In 2014, a case report was published about a 26-year-old man with chronic abdominal pain, pruritus, nausea, and vomiting. He was found to be jaundiced with a cholestatic liver injury. An upper endoscopy showed a gastric ulcer, and biopsies revealed chronic active gastritis and acute inflammation with focal granuloma. After an abdominal ultrasound showed gallbladder wall thickening, the patient had a cholecystectomy. A wedge liver biopsy performed during surgery showed granulomatous inflammation with areas of necrotizing granulomata. Further imaging with MRCP showed evidence of sclerosing cholangitis. He was thought to have SSC from sarcoidosis and was started on prednisone 40 mg once daily. He was followed for 1 year, with resolution of symptoms and decrease in total bilirubin from 8.6 to 1.4 mg/dL [15].
Hodgkin’s Lymphoma
Jaundice caused by Hodgkin’s lymphoma is rare. There is a case report from 2016 of a 38-year-old man who presented with jaundice, pruritus, nausea, vomiting, weight loss, and recurrent fevers for 1 month. His total bilirubin was 11.7 mg/dL at presentation. An MRCP showed multiple strictures in the intrahepatic and extrahepatic ducts. No clear etiology was found on workup, although he was taking herbal medicines and celecoxib. His condition worsened during follow-up with a total bilirubin rising to 26.1 mg/dL, and he was referred for liver transplantation. Because of the possibility of DILI, the patient was started on ursodiol 1200 mg per day, and given N-acetyl-cysteine. A liver biopsy followed and revealed changes compatible with either sclerosing cholangitis or drug-induced cholestasis. He was then started on prednisolone 50 mg per day. The patient gradually improved in regards to symptoms and liver tests after 3 months of prednisolone. His total bilirubin dropped to 1.3 mg/dL. However, after the therapy, he was found to have axillary and cervical lymphadenopathy on exam. Excisional lymph node biopsy revealed Hodgkin’s lymphoma and the patient was initiated on chemotherapy. After 18 months of follow-up, the total bilirubin was 0.6 mg/dL, but an MRCP still showed sclerosing cholangitis. Authors point out that it was unclear in this case what caused the sclerosing cholangitis [16].
Critically Ill Patients
SSC-CIP is an increasingly recognized disease, and likely under-diagnosed in the past. Several articles have been published on SSC-CIP in the past 5 years, including a few systematic reviews. We will attempt to focus on the primary literature for the scope of this section.
SSC-CIP is thought to arise from ischemic injury to the biliary tree. Several groups have looked into potential risk factors for developing the disease, which seem quite varied. Most cases seem to occur in patients after trauma, burns, cardiac/thoracic surgery, respiratory illness, and sepsis. Less reported illnesses leading to ICU admission include hemorrhagic shock, HELLP syndrome, pancreatitis, acute myocardial infarction, rhabdomyolysis, subarachnoid hemorrhage, and cerebral hemorrhage [17,18,19,20, 21•, 22]. Leonhardt et al. investigated a group of 16 patients with SSC-CIP. All patients had severe hemodynamic instability, defined as at least 60 min of mean arterial pressure (MAP) below 65 mmHg. These patients also required vasopressor support and mechanical ventilation. The mechanical ventilation duration was on average 25.5 ± 14.3 days [19]. Another study by Ben-Ari et al. examined four patients developing SSC-CIP after a major burn injury. All of these patients were on mechanical ventilation and required vasopressor support, with mention of all patients having repeated episodes of severe hypotension, defined as systolic blood pressure <70 mmHg [23]. A retrospective study by Weig et al. looked at a group of patients with severe acute respiratory distress syndrome (ARDS) due to H1N1 pneumonia. Twenty-one patients were analyzed, including 16 without SSC-CIP and 5 with SSC-CIP, and a comparison was made. Patients who developed SSC-CIP had a higher body mass (BMI), higher volume of intraperitoneal fat, and spent longer time in the prone position. Of note in this study, there was no difference in vasopressor use or dosage, arterial lactate level, need for renal replacement therapy (RRT), blood oxygen content, or mean arterial pressure (other than day of admission it was higher in SSC-CIP group) [21•].
It takes a considerable amount of time for SSC-CIP to develop. From a systematic review, it occurs in patients with an intensive care stay (45.8 ± 27.3 to 89.2 ± 75.5 days) before diagnosis of SSC-CIP [17]. There was a range of 33–106 days before onset of disease in the study of four burn patients by Ben-Ari et al. Mean peak laboratory values include the following: alkaline phosphatase 2484 ± 496.3 U/L, gamma-glutamyl transferase (GGT) 4045.2 ± 2056.6 U/L, and total bilirubin 19.7 ± 15.2 mg/dL [23]. The study by Leonhardt et al. of 16 patients had a mean intensive care stay of 39 ± 23.9 days. They found that at the time of diagnosis, liver tests show a cholestatic injury picture, seen at a median of 7 days after ICU admission. Alkaline phosphatase and GGT rose first in these SSC-CIP patients [19]. In a separate paper, but in the same group of patients, the authors also showed that 12/14 (no data for two patients) patients had recurrent cholangitis episodes. Also, 11/16 patients developed acute cholecystitis [24•]. Voigtlander et al. looked at 54 patients with SSC-CIP and found the following median laboratory values: alkaline phosphatase 1184 U/L, GGT 1029 U/L, alanine aminotransferase (ALT) 98 U/L, aspartate aminotransferase (AST) 99 U/L, and total bilirubin 9.4 mg/dL [22].
One retrospective study looked at the microbiological profile of bile in SSC-CIP patients compared to primary sclerosing cholangitis (PSC) patients. The study included a total of 169 patients (72 with SSC-CIP and 97 with PSC). Cultures were obtained during ERCP. The authors found in the SSC-CIP patients more Enterococcus faecium, Pseudomonas aeruginosa and non-albicans species of Candida compared to PSC patients. SSC-CIP patients also had higher incidence of drug- or multi-drug-resistant organisms [25]. A study by Voigtlander et al. had bile aspirated in 74% of the 54 patients. Ninety-eight percent of these bile aspirates grew organisms, which included E. faecium (48%) and E. faecalis (28%) [22].
Patients with SSC have similar imaging and ERCP findings as patients with PSC. We have included an image from an ERCP displaying an extrahepatic biliary stricture in a post-orthotopic liver transplantation (OLT) patient at our hospital (Fig. 1). A study by Voigtlander et al. had 54 patients, all of who had an ERCP. There were multiple diffuse intrahepatic bile duct strictures in 67% of patients; both intra- and extrahepatic strictures in 20%; and only extrahepatic duct changes in 6%. Biliary casts were present in 93% of patients. In this same study, 13/44 patients with ultrasound suggested SSC, and 7/9 patients with MRCP suggested SSC [22]. Leonhardt et al. had ultrasound scans of all 16 patients, with 7 patients showing dilatation of extrahepatic or intrahepatic ducts. During ERCP, 81% of these patients had only intrahepatic duct involvement, and 19% both intra- and extrahepatic duct abnormalities [24•]. In a small study of four burn patients by Ben-Ari et al., an MRCP was performed on three of the study patients, all of which showed irregular intrahepatic bile ducts with multiple strictures and dilatations [23].
SSC-CIP has been shown in prior literature to be a very progressive disease, even to liver cirrhosis. It has a poor prognosis, and treatment options are fairly limited [17]. In a study by Voigtlander et al. 27/54 of patients died during follow-up. Another six patients required OLT. The remaining 21 patients were compared to the 33 patients who either died or had OLT. A formal multivariate analysis showed an elevated model of end-stage liver disease (MELD) and need for RRT as independent risk factors for mortality in SSC-CIP [22]. In a report of four burn patients by Ben-Ari et al., the investigators reported two deaths from multi-organ failure and septic shock, one patient underwent OLT and one patient with less extensive disease did not progress and was alive at the end of the study [23]. The study by Leonhardt et al. reported 9/16 patients required OLT, with the earliest transplant occurring at 189 days from onset of cholestasis. Of these patients receiving OLT, there was 85% 1-year survival rate and 83% 3-year survival rate [24•]. One retrospective study examined 96 patients with SSC-CIP and found 56% died during their ICU stay. They looked closely at 21 SSC-CIP patients who received OLT with a median follow-up period after OLT of 82 months. These patients were compared to a control group of 60 patients with other causes of cirrhosis receiving OLT. In the SSC-CIP group, 6/21 patients died of biliary sepsis (83%) and HCC (17%) during follow-up. The SSC-CIP group when compared to the control OLT group had the following survival rates: 1 year was 100 versus 98%, 86 versus 92%, and 76 versus 87%, respectively [18].
Discussion
The bulk of the literature on SSC during the past 5 years has been focused on the emerging entity of SSC-CIP, which is where most of this discussion will center. However, there are also several case reports and retrospective studies of different etiologies, adding to the varied literature describing this disease. Because of the varying etiologies, the clinical course and prognosis can be variable. Etiologies such as drugs and autoimmune disease tend to have a better prognosis [7, 9, 11, 12, 14, 26]. However, causes such as critical illness seem to have worse outcomes [17, 18, 22, 23, 24•].
Infectious etiologies have been linked to the development of SSC in the past. The first two known reports of patients developing SSC from CDF were described recently. Both of these cases were likely caused, at least primarily, by recurrent infection of the biliary tree. There could also be a component of obstructive cholangiopathy. The first patient required liver transplantation due to the extent of her liver disease, and the second required surgery to resolve the CDF [4, 5]. A retrospective study looked at patients with human alveolar echinococcosis (AE) caused by Echinococcus multilocularis developing SSC, which was not described before [6]. After considering possible contributing factors identified as liver surgery and length of benzimidazole therapy, it was unclear what the role of the infectious agent was in the development of SSC.
Numerous drugs have been reported recently to cause SSC, with most patients recovering liver function after discontinuation of the drug. An interesting retrospective study reviewed patients diagnosed with DILI and attempted to determine if any had SSC. Out of 102 patients, they found 10 patients with the likely diagnosis of SSC. The implicated drugs included amoxicillin-clavulanate, sevoflurane, amiodarone, infliximab, green tea extract, venlafaxine, and atorvastatin. Only one patient, who was treated with infliximab, did not recover liver tests before the end of the study [7]. Case reports of ketamine, celecoxib, and TACE with bleomycin-iodinated oil were also reported [9, 11, 12].
Obstructive and autoimmune causes of SSC have been published in the past. A case report of metastatic gallbladder adenocarcinoma was described [13]. It is unclear in the case of Hodgkin’s lymphoma what caused the SSC, as liver tests improved with prednisolone before the diagnosis of Hodgkin’s lymphoma, and remained normal after treatment for the lymphoma. Despite normalization of the liver tests, imaging studies remained abnormal [16]. A patient with Behcet disease developed SSC, which responded to biliary stenting with normalization of liver tests [14]. Sarcoidosis was also shown to cause SSC in a case report, with improvement after steroid therapy [15].
SSC-CIP has become more recognized and published recently, leading to the conclusion that it has been under-diagnosed in the past. It is difficult to predict which intensive care patients will develop the disease since the reasons for ICU admission are so varied [17,18,19,20, 21•, 22]. Many studies have noted that perhaps mechanical ventilation, hemodynamic instability, and vasopressor requirements, could be contributing factors [19, 23]. However, these are factors present in most intensive care patients, and likely do not help in predicting disease. The SSC-CIP study by Weig et al. was unique because their patients not only had the same etiology of illness in H1N1 pneumonia, but they also had a comparison group (H1N1 ICU patients without SSC-CIP). They did not report a difference in mechanical ventilation, hemodynamic instability, and vasopressor requirements, between the two groups. However, they did find that the SSC-CIP patients had a higher BMI, higher volume of intraperitoneal fat, and spent longer time in the prone position [21•]. Perhaps patients with higher BMI and intraperitoneal fat should spend less time in the prone position. It has also been widely reported that it takes a considerable amount of time in ICU to develop SSC-CIP [17, 23], but this is likely flawed, as cholestatic liver injury is seen as soon as 7 days after ICU admission [19]. It is unclear why there is a possible delay in diagnosis, but potential factors include poor awareness of the disease, assumption of other diagnoses such as DILI or ischemic hepatitis, and lack of appropriate imaging early in the course. A few studies have shown that ultrasound does not detect the disease in many patients, which seems to be mainly intrahepatic duct disease [22, 24•]. Perhaps early cross-sectional imaging, or involving a gastroenterology specialist early, would be beneficial.
Even if SSC-CIP is diagnosed earlier, it is unclear if any treatment will alter the progression of disease. It appears that these patients have more Candida and drug-resistant bacteria in their bile, which should be considered when choosing anti-microbial therapy, and maybe whether to start anti-fungal therapy [25]. The majority of patients with SSC-CIP have intrahepatic duct disease only, which makes endoscopic therapy options more limited as well [22, 23, 24•]. ICU mortality of the disease is around 50–56% [18, 22]. Meanwhile, survival rates of SSC-CIP patients undergoing OLT are similar to other patients receiving OLT [18, 24•]. Taking all of this into account, it is possible that with more prompt recognition of SSC, these patients could be listed for OLT earlier in their disease process to improve their outcome.
References
Papers of particular interest, published recently, have been highlighted as: • Of mportance
Hubers LM, Beuers U. How to diagnose immunoglobulin G4-associated cholangitis: the jack-of-all-trades in the biliary tract. Viszeralmedizin. 2015 Jun;31(3):185–8.
Wiencke K, Boberg KM. Current consensus on the management of primary sclerosing cholangitis. Clin Res Hepatol Gastroenterol. 2011 Dec;35(12):786–91.
Imam MH, Talwalkar JA, Lindor KD. Secondary sclerosing cholangitis: pathogenesis, diagnosis, and management. Clin Liver Dis. 2013 May;17(2):269–77.
Chang W-T, Lin N-C, Hsia C-Y, Liu C-S, Tsai H-L, Loong C-C. Liver transplantation for a renal transplantation recipient with secondary sclerosing cholangitis by choledochoduodenal fistula. Asian J Surg. 2012 Jan;35(1):49–52.
Gromski MA, Fogel EL, Vuppalanchi R. Secondary Sclerosing cholangitis from spontaneous choledochoduodenal fistula. Clin Gastroenterol Hepatol. 2017 Mar;15(3):e71–2.
Frei P, Misselwitz B, Prakash MK, Schoepfer AM, Prinz Vavricka BM, Müllhaupt B, et al. Late biliary complications in human alveolar echinococcosis are associated with high mortality. World J Gastroenterol. 2014 May 21;20(19):5881–8.
Gudnason HO, Björnsson HK, Gardarsdottir M, Thorisson HM, Olafsson S, Bergmann OM, et al. Secondary sclerosing cholangitis in patients with drug-induced liver injury. Dig Liver Dis. 2015 Jun;47(6):502–7.
Lo RSC, Krishnamoorthy R, Freeman JG, Austin AS. Cholestasis and biliary dilatation associated with chronic ketamine abuse: a case series. Singap Med J. 2011 Mar;52(3):e52–5.
Turkish A, Luo JJ, Lefkowitch JH. Ketamine abuse, biliary tract disease, and secondary sclerosing cholangitis. Hepatol Baltim Md. 2013 Aug;58(2):825–7.
El Hajj II, Malik SM, Alwakeel HR, Shaikh OS, Sasatomi E, Kandil HM. Celecoxib-induced cholestatic liver failure requiring orthotopic liver transplantation. World J Gastroenterol. 2009 Aug 21;15(31):3937–9.
Nayudu SK, Badipatla S, Niazi M, Balar B. Cholestatic hepatitis with small duct injury associated with celecoxib. Case Rep Med. 2013;2013:315479.
Jin S, Shi X-J, Sun X-D, Wang S-Y, Wang G-Y. Sclerosing cholangitis secondary to bleomycin-iodinated embolization for liver hemangioma. World J Gastroenterol. 2014 Dec 14;20(46):17680–5.
Fan DS, Sorser SA, Gamarra RM. Secondary Sclerosing cholangitis due to gallbladder adenocarcinoma. Case Rep Gastroenterol. 2013 Jan;7(1):134–9.
Ben Slama Trabelsi A, Issaoui D, Ksiaa M, Souguir A, Mama N, Brahem A, et al. Sclerosing cholangitis in Behçet’s disease. Case Rep Med. 2013;2013:692980.
Momah N, Otesile A, Pawa R, Shedlofsky S. Sarcoidosis presenting as necrotizing sarcoid granulomatosis of the liver, sclerosing cholangitis, and gastric ulcer. ACG Case Rep J. 2014 Apr;1(3):164–6.
Abedi SH, Ghassami M, Molaei M, Mohsenifar Z, Mohammad Alizadeh AH. Secondary sclerosing cholangitis and Hodgkin’s lymphoma. Clin Med Insights Case Rep. 2015;8:83–7.
Kirchner GI, Rümmele P. Update on Sclerosing cholangitis in critically ill patients. Viszeralmedizin. 2015 Jun;31(3):178–84.
Voigtländer T, Jaeckel E, Lehner F, Manns MP, TO L. Liver transplantation for critically ill patients with secondary sclerosing cholangitis: outcome and complications. Liver Transpl. 2015 Oct;21(10):1295–9.
Leonhardt S, Veltzke-Schlieker W, Adler A, Schott E, Hetzer R, Schaffartzik W, et al. Trigger mechanisms of secondary sclerosing cholangitis in critically ill patients. Crit Care. 2015 Mar 31;19:131.
Lin T, Qu K, Xu X, Tian M, Gao J, Zhang C, et al. Sclerosing cholangitis in critically ill patients: an important and easily ignored problem based on a German experience. Front Med. 2014 Mar;8(1):118–26.
• Weig T, Schubert MI, Gruener N, Dolch ME, Frey L, Miller J, et al. Abdominal obesity and prolonged prone positioning increase risk of developing sclerosing cholangitis in critically ill patients with influenza A-associated ARDS. Eur J Med Res. 2012 Dec 22;17:30. This study looks at a specific group of patients with severe acute respiratory distress syndrome and compares those with and without secondary sclerosing cholangitis.
Voigtländer T, Negm AA, Schneider AS, Strassburg CP, Manns MP, Wedemeyer J, et al. Secondary sclerosing cholangitis in critically ill patients: model of end-stage liver disease score and renal function predict outcome. Endoscopy. 2012 Nov;44(11):1055–8.
Ben-Ari Z, Levingston D, Weitzman E, Haviv-Yadid Y, Cohen-Ezra O, Weiss P, et al. Secondary sclerosing cholangitis following major burn. Ann Hepatol. 2015 Oct;14(5):695–701.
• Leonhardt S, Veltzke-Schlieker W, Adler A, Schott E, Eurich D, Faber W, et al. Secondary sclerosing cholangitis in critically ill patients: clinical presentation, cholangiographic features, natural history, and outcome: A series of 16 cases. Medicine (Baltimore). 2015 Dec;94(49):e2188. A thorough evaluation of patients with secondary sclerosing cholangitis from critical illness, with examination of the natural history and outcomes.
Voigtländer T, Leuchs E, Vonberg R-P, Solbach P, Manns MP, Suerbaum S, et al. Microbiological analysis of bile and its impact in critically ill patients with secondary sclerosing cholangitis. J Inf Secur. 2015 May;70(5):483–90.
Voigtländer T, Alten T, Lehner F, Strassburg CP, Manns MP, Lankisch TO. Secondary sclerosing cholangitis following liver transplantation: a rare cause for graft failure. Z Gastroenterol. 2013 Mar;51(3):296–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Rolando Leal and John Brooling declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pancreas and Biliary Tract
Rights and permissions
About this article
Cite this article
Brooling, J., Leal, R. Secondary Sclerosing Cholangitis: a Review of Recent Literature. Curr Gastroenterol Rep 19, 44 (2017). https://doi.org/10.1007/s11894-017-0583-8
Published:
DOI: https://doi.org/10.1007/s11894-017-0583-8