Abstract
Purpose of Review
Lifestyle interventions (such as diet and physical activity) successfully limit excessive gestational weight gain and can reduce some adverse maternal events; however, benefit is variable and cost-effectiveness remains unclear. We aimed to review published cost-effectiveness analyses of lifestyle interventions compared with usual care on clinically relevant outcome measures. Five international and six grey-literature databases were searched from 2007 to 2018. Articles were assessed for quality of reporting. Data were extracted from healthcare and societal perspectives. Costs were adapted to the common currencies of Australia and the United Kingdom by adjusting for resource utilization, healthcare purchase price and changes in costs over time. Included studies were economic analyses of lifestyle interventions aiming to limit weight-gain during pregnancy and/or reduce risk of gestational diabetes, for women with a BMI of 25 or greater in pre- or early-pregnancy.
Recent Findings
Of the 538 articles identified, six were retained for review: one modelling study and five studies in which an economic analysis was performed alongside a randomized-controlled trial. Outcome measures included infant birth-weight, fasting glucose, insulin resistance, gestational weight-gain, infant respiratory distress syndrome, perceived health, cost per case of adverse outcome avoided and quality-adjusted life years (QALYs). Interventions were cost-effective in only one study.
Summary
Although many studies have investigated the efficacy of lifestyle interventions in pregnancy, few have included cost-effectiveness analyses. Where cost-effectiveness studies were undertaken, results were inconsistent. Secondary meta-analysis, taxonomy and framework research is now required to determine the effective components of lifestyle interventions and to guide future cost-effectiveness analyses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Women worldwide are entering pregnancy with increasingly higher weight [1, 2•], due to the obesogenic environments in which we live [3]. In addition, approximately 45% of pregnant women exceed the 2009 Institute of Medicine’s recommendations for gestational weight gain in pregnancy [4]. Higher weight at conception and higher than recommended weight gain during pregnancy can increase the risk of adverse maternal and infant outcomes [2•, 3, 5, 6]. Many of the lifestyle interventions designed to prevent excessive gestational weight gain in pregnancy are effective, with potential for improvements in other outcome measures of clinical relevance [7,8,9,10, 11••]. While research to determine which type of intervention is most effective is ongoing, successful interventions appear to be those in which diet counselling was combined with physical activity, and where women were supported by motivational counselling for weight management goal setting and weight monitoring [7, 12].
To date, the costs of effective interventions for many major public health priorities have not been well understood [13], and a lack of reliable data on the economic costs of individual intervention types is an impediment to funding effective interventions to address weight gain during pregnancy [14]. There is significant potential for improved health outcomes for both mother and infant through implementing lifestyle interventions to prevent excessive gestational weight gain, pregnancy complications and subsequent maternal obesity [11••], and these improved health outcomes have important economic consequences. For instance, obesity has been associated with 30% higher medical costs compared with costs for persons categorized as below a body mass index (BMI) of 25 [15], and higher costs may impact on maternal and infant medical care [16].
A lack of evidence for the economic costs of interventions to address weight gain in pregnancy is a barrier to funding implementation of lifestyle interventions to limit excessive gestational weight gain [14]. Understanding intervention costs, benefits and related health effects is imperative to provide decision makers with the requisite information to determine how best to translate research and facilitate implementation [17]. Hence, we aimed to conduct a systematic review of studies reporting cost-effectiveness analyses for interventions designed to reduce gestational weight gain and/or gestational diabetes mellitus (GDM) risk during pregnancy. This is the first study to qualitatively and quantitatively review the cost-effectiveness of interventions to limit gestational weight gain and adapt these studies into specific single currencies.
Method
This study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement. The review was registered prospectively with the International Register of Systematic Reviews (PROSPERO; CRD42018089087).
Information Sources
Relevant articles were sourced through a search of five academic databases: EMBASE and Medline via Ovid, Econlit and CINAHL via EBSCO and Web of Science. In order to identify studies that may not have been recorded in academic databases, six grey literature databases were also searched: ISPOR database, Cochrane trials, Cochrane Economic Evaluations, PDQ-evidence [18], Epistemonekos [19] and Google Scholar. These databases have been recommended as being sufficient for systematic reviews of economic analyses [20]. The search strategy was designed to identify all studies published in the English language between January 2007 and June 2018. (Preliminary searches revealed minimal studies that met inclusion criteria prior to this date and none that incorporated economic evaluation). Search terms for population and intervention were matched to those presented by the International Weight Management in Pregnancy Collaborative Network (I-WIP; Rogozińska et al. 2017). The search strategy for economic analyses used keywords and medical subject heading terms concerning cost, cost-effectiveness, cost-utility and health economic studies. The search was performed in June 2018. Search terms are presented in Appendix 1 along with a sample of the search in Appendix 1, Fig. S1.
Eligibility Criteria
Inclusion criteria were studies containing lifestyle behavioural interventions (such as healthy eating and physical activity) aiming to reduce gestational weight gain or lower risk for gestational diabetes mellitus in pregnant women with a BMI of 25 or more (consistent with a definition of being overweight or obese). All studies needed to provide cost estimates and state a cost year. Exclusion criteria were preconception or postpartum women, women with a BMI under 25 kg/m2, studies that did not provide a lifestyle intervention, studies where the comparator group received an alternative intervention and studies without outcomes pertaining to an economic analysis.
Study Selection
PRISMA reporting guidelines were used to select studies [21]. Publications were screened using the referencing program Covidence [22]. Titles and abstracts were screened against the inclusion/exclusion criteria by two authors (CB, RW). Potentially eligible papers were accessed in full text and assessed by two authors against the inclusion/exclusion criteria (CB, ZA). Differences of opinion were resolved by discussion and consensus. If required, a third person was consulted.
Data were extracted for the following categories: study population (maternal age, BMI, gestational age at recruitment), sample size, intervention, comparator, outcome, perspective (healthcare or societal) and study type. Cost and effect data were extracted separately for total medical costs and total indirect costs so that data could be analysed from both healthcare and societal perspectives.
Quality of Reporting
Quality of reporting was assessed using the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist [23]. It was expected that items 4, 7 and 10 from the CHEERS checklist (population, intervention/comparator and outcome measures) would be met by all studies, as these were required to meet the inclusion criteria. Some of the CHEERS criteria were only relevant to modelling studies and not to studies where cost-effectiveness is conducted alongside a randomized-controlled trial (RCT), and thus were not included in the overall score. Therefore, studies were given a percentage score for relevant questions.
Cost and Effect Data Extraction
Where a study presented cost data from a societal perspective, cost information from a healthcare perspective was also extracted. Cost data year was an inclusion requirement (CHEERS checklist item 14) [23]. Study effects were extracted for all available outcome measures.
Adaptation of Cost Data to UK and Australian Currencies
Costs were adapted from original currencies into Great Britain pounds (GBP) and Australian dollars (AUD). Cost data were adapted by the first author (CB) and reviewed by the final author (ZA), based on a methodology outlined in a study adapting costs for Switz erland [24]. Cost data for direct medical costs to Australia/UK were adapted in three stages: 1) data were corrected for level of resource utilization, 2) correction for differences in prices for healthcare services and 3) adjustment for the change in resource utilization and prices over time, as outlined in more detail below. After cost adaptation, incremental cost-effectiveness ratios (ICERs) were recalculated in AUD and GBP.
Resource Utilization
Healthcare resources vary across countries by quantity and type, such that healthcare consumers may receive differing treatments for the same condition, dependent on the country of residence. A correction is therefore applied to resource utilization, as calculated by the Organization for Economic Cooperation and Development (OECD). For this study, current expenditure on health, per capita for USD purchasing power parities was obtained [25].
Price of Healthcare Purchases
Monetary value for similar healthcare services often vary between countries. A price correction was conducted by using purchasing power parities to adjust for proportional costs for similar products between countries. Purchasing power parities for Gross Domestic Product (GDP) in national currency per USD was obtained from the OECD [26].
Change in Cost over Time
Corrections were subsequently made to adapt all studies to the same cost year. Annual healthcare growth rates were obtained from published sources. Australia’s annual healthcare growth rates were obtained from the Australian Institute of Health and Welfare [27]. Annual healthcare growth rates for the UK were obtained from the UK office for National Statistics [28]. Healthcare growth rates were expected to be suitable, as healthcare resources used for perinatal medical care may change over time, as well as increase in price over time. Costs for all studies were adapted to 2015, the latest year available.
Example of Cost Correction
To illustrate the above process of cost adaptation, the following example from Kolu et al. 2013 adapts Euros into Australian dollars. The total cost for controls was €6994 (year 2013), multiplied by 1.0083 (corrected for resource utilization), multiplied by 1.6952 (correction for purchase parity) and multiplied by 1.2641 (correction for change in cost over time), giving a value of AUD 15,112 (year 2015).
Willingness-to-Pay Thresholds
Cost-effectiveness for QALYs gained was based firstly on the study authors’ assessments. Secondly, when costs were recalculated, willingness-to-pay thresholds for UK and Australia were applied. The willingness-to pay threshold in the UK is generally agreed to be from GBP 20,000 to GPB 30,000 per quality adjusted life year (QALY) [29]. There is no formally accepted cost-effectiveness threshold in Australia; however, a willingness to pay threshold of around AUD 50,000 [30] is generally accepted, although new evidence around opportunity costs by Edney et al. suggested an appropriate threshold for cost per QALY gained to be approximately AUD 28,033 [31]. These thresholds were used to determine cost per QALY gained in this review. For maternal and infant outcomes, the willingness-to-pay threshold was defined as per author assessment.
Sensitivity Analyses
Sensitivity analyses as reported in included articles were investigated, to determine what types of sensitivity analyses were included, what aspects of the data were investigated and what conclusions the authors made.
Results
Systematic Approach to Study Selection
After duplicates were removed, a total of 538 abstracts were assessed, and 20 papers were retained for full text screening, as presented in Fig. 1. Six studies met all the criteria after full-text review. For the fourteen studies that were excluded, reasons for exclusion are displayed in Fig. 1, and excluded studies are presented in Appendix 2 Table S1.
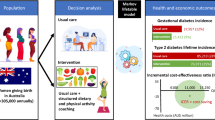
Study and Patient Characteristics
Five of the articles included in the current review were cost-effectiveness studies conducted in conjunction with an RCT; included countries were Australia [32], Finland [33], the Netherlands [34], the United Kingdom [35] and a multi-country site involving nine European countries based on Dutch costings [36]. One study was a modelling study and was based on individual patient-level data drawn from studies from a range of countries [8]. Three studies investigated women with a BMI of 25 kg/m2 or more [32,33,34]. Two studies included only women who were classified as affected by obesity (with a BMI of ≥ 29 [36] or ≥ 30 [35] kg/m2). One study presented data from all weight types, including sub-analyses for normal, overweight and obese groups [8]. Characteristics of included studies are presented in Table 1.
Study Quality
Studies were assessed using the CHEERS checklist criteria [23]; however, the questions pertaining to modelling were excluded for the RCT studies, as they were not relevant to the study design. All studies scored at least 95% on the CHEERS checklist.
Interventions
Four of the RCTs evaluated interventions that combined diet and physical activity programs, ranging from five individual sessions with up to four follow-up telephone calls [36], three individual sessions with three follow-up calls [32], five antenatal care visits added to the 15 visits received in standard care [33] and eight weekly sessions [35]. In one study, participants received an exercise only program, which included two sessions a week from commencement until delivery [34]. The modelling study [8] included sub-analyses for diet, physical activity and mixed interventions of various intensities. Most samples sizes were 100 or more, except for the physical exercise study which had less than 50 participants in the intervention group [34]. Control groups received care as usual, as per local standards. One study explicitly stated that diet and exercise advice was not included in care as per usual practice [32]. Some dietary and physical activity advice was included in care as usual in the study by Kolu et al. [33].
Cost Measurements
Direct costs (prenatal medical, birth, postnatal and infant) and indirect costs (work absenteeism) were compared across studies following cost adaptation, as described above. Three studies included costs from a societal perspective [33, 34, 36], but the available information meant that costs could also be calculated from a health care perspective. Hence, we were able to assess all studies from a healthcare perspective and three from a societal perspective. Infant costs were included in two studies [32, 33], and all four RCTs presented pre- and post-delivery costs separately. Cost estimates for the modelling study were informed by a systematic literature review [8]. Costs are presented in original currency in Appendix 4, Table S8.
From a healthcare perspective, when neonatal care was included (three studies) [32, 33, 35]), almost two-thirds of costs on average were associated with delivery (46–80%), just over 20% for neonatal care (15–29%) and less than 20% for remainder for prenatal care (5–29%) (see Appendix 5, Table S9). From a healthcare perspective and excluding neonatal care (all five RCT studies) [32,33,34,35,36]), delivery costs contributed to approximately 80% (56–93%) and prenatal care to just around 20% (6–44%) of total costs (see Appendix 5, Table S10). From a societal perspective (three studies, neonatal costs unavailable [33, 34, 36]), over one-third of costs were associated with productivity loss (24–50%), under half with delivery (28–62%) and less than 15% with prenatal care (6–26%). (see Appendix 5, Table S11).
Study Effects—QALYs
Three studies presented quality of life data using the EuroQol questionnaire (EQ-5D) [34,35,36], and one used the quality of life questionnaire (15D) measures [33]. The EQ-5D is a five-dimensional survey that contains the following components: mobility, self-care, usual activities, pain/discomfort and anxiety/depression [37]. The 15D measures 15 dimensions over 5 levels [38]. QALY estimates are shown in Table 2.
Study Effects—Infant and Maternal Outcomes
Seven (non-QALY) outcome measures were contained in the five studies (Table 3). These outcomes were fasting glucose (two studies) [34, 36], insulin resistance (two studies) [34, 36], gestational weight gain (one study) [36], perceived health (one study) [33], case of adverse maternal outcome avoided (one study) [8], infant birth weight (three studies) [32,33,34] and respiratory distress syndrome (one study) [32]. Further outcomes had been assessed in some trials, but were not included in the economic analysis due to lack of efficacy. For instance, Dodd et al. [32] measured gestational weight gain in their trial, but lack of efficacy meant that this measure was not reported in the cost-effectiveness analysis.
Costs Adapted to UK and Australian Currencies
Healthcare Perspective
Total costs from the five RCT studies [32,33,34,35,36] from a healthcare perspective ranged between GBP 220 and GBP 4624 per person (AUD 595–AUD 16,758) for intervention groups and between GBP 262 and GBP 4642 per person (AUD 711–AUD 12,852) for control groups. Higher overall costs were associated with the inclusion of delivery in the cost estimates.
Societal Perspective
Total costs from the three studies where data was presented from a societal perspective [33, 34, 36] ranged between GBP 166 and GBP 6481 per person (AUD 4,518–AUD 17,578) for intervention groups and between GBP 1257 and GBP 6205 per person (AUD 3664–AUD 16,830) for control groups. Again, higher overall costs were associated with including delivery in the cost estimates.
Intervention Costs
Intervention costs ranged between GBP 103 and 405 per person or 304 and 936 per person in Australian dollars (presented in original currency in Appendix 4, Table S8).
Cost-Effectiveness
Incremental Cost Effectiveness ratios (ICER), cost-effectiveness plane statistics and cost acceptability curve results by intervention for all outcome measures are presented in Table 4.
Cost-Effectiveness—Cost per QALY Gained
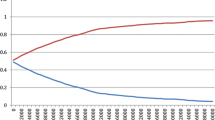
Incremental cost-effectiveness ratios of QALYs are displayed on a cost-effectiveness plane in GBP from a healthcare perspective in Fig. 2 (note that for papers presented from a societal perspective, results have been adjusted to that of a healthcare perspective, and cost adjusted to AUD and GBP). Of the four included studies reporting QALYs as an outcome measure, the Broekhuizen et al. study [36] presented three different interventions; therefore, six interventions are presented in this figure. Overall, two interventions were cost-effective (and cost-saving) and four were not cost-effective, as per the willingness-to-pay thresholds. The combined healthy eating and physical activity intervention from Broekhuizen et al. [36] was cost saving (i.e. lower cost, higher effect as compared with control group; savings of GBP 677 or AUD 1836, difference in QALYs of 0.02) (number 1 in Fig. 2). The healthy eating intervention in the Broekhuizen et al. [36] study was slightly cost saving and effect neutral (number 2 in Fig. 2). The intervention incorporating physical activity only in the same study had a neutral effect with cost savings of GBP 1120 or AUD 3039 (number 3 in Fig. 2). The mixed interventions described in studies by Kolu et al. and Poston et al. were both more expensive and more efficacious than the associated control groups, with neither study considered to be cost-effective in regard to a willingness-to-pay threshold of GBP 30,000. The Kolu et al. [33] intervention had an ICER of GBP 81,941 per QALY gained (AUD 241,151) compared with control (number 4 in Fig. 2). The Poston et al. [35] intervention had an ICER of GBP 344,014 per QALY gained compared with control (AUD 795,777) (number 6 in Fig. 2). The exercise only intervention in the Oostdam et al. [34] study was dominated by the control group (i.e. more costly and less effective) (number 5 in Fig. 2).
Results were similar in studies presenting outcomes from a societal perspective as compared with a healthcare perspective (presented in Appendix 3, Fig. S2). Of the three included studies that presented data from a societal perspective and included QALY as an outcome measure, the Broekhuizen et al. study [36]study presented three interventions [36]; therefore, there are five interventions included in this analysis. The Broekhuizen et al. combined healthy eating and physical activity intervention [36] was cost saving (savings of GBP 1034 and AUD 2805; effect difference of 0.02 QALYs). The Broekhuizen et al. healthy eating intervention was more costly and neither effective nor cost-effective (ICER of GBP 133470 or AUD 362,007 per QALY gained). The Broekhuizen et al. physical activity only intervention had a neutral effect with cost savings of GBP 740 and AUD 2008. The mixed intervention in the study by Kolu et al. [33] had an ICER of GBP 45,685 per QALY gained and was not cost-effective according to the above criteria. The exercise only intervention in the Oostdam et al. [34] study was dominated by the control group.
Cost Effectiveness—Maternal Outcomes
Fasting Glucose and Insulin Resistance
Two studies presented data on glucose metabolism, using two measures: fasting glucose and insulin resistance [34, 36], presented from a societal perspective. Broekhuizen et al. reported fasting glucose in the healthy eating combined with physical activity and physical activity only interventions and found that these interventions were more costly and more effective at lowering fasting glucose on average than care as usual. The healthy eating only intervention was more costly and less effective (fasting glucose increased). All interventions in this study were more costly and more effective for lowering insulin resistance [36]. It is important to note that effect differences between intervention groups and the control group were low across all three interventions: differences in groups compared with the control group for insulin resistance (HOMA-IR) were 0.0 for the combined intervention, − 0.1 for the healthy eating intervention and − 0.1 for the physical activity intervention; differences compared with controls in fasting glucose (mmol/l) were − 0.1 for the combined intervention, − 0.1 for the healthy eating intervention and − 0.1 for the physical activity intervention. The likelihood of being cost-effective was stated as being low for all interventions by the authors [36]. Oostdam et al. reported results where the highest percentage of estimates were in the northwest quadrant, suggesting that the intervention was dominated by usual care [34].
Other Maternal Outcome Measures
There were three further maternal outcome measures reported in the studies: gestational weight gain, perceived health and cost per adverse maternal outcome avoided (pre-eclampsia, gestational diabetes, pregnancy-induced hypertension, pre-term delivery, caesarean section, intrauterine death, large for gestational age, small for gestational age, neonatal intensive care unit admission). Preventing gestational weight gain was found to be more costly and more effective for the healthy eating combined with physical activity intervention in the Broekhuizen study, but authors stated that the intervention was unlikely to be cost-effective [36]. Preventing gestational weight gain was cost-effective neither for the physical activity only intervention nor for the healthy eating intervention [36]. The lifestyle intervention was not cost-effective for the perceived health visual analogue measure in the Kolu et al. study [33]. The modelling paper by Rogozinska et al. considered a range of health conditions in the assessment of cost per adverse maternal outcome avoided and found that there was no evidence of cost-effectiveness for the included interventions [8].
Cost-Effectiveness—Infant Outcomes
Infant Birth Weight
Three papers investigated infant birth weight; two studies in grams [33, 34] and one study in proportion of infants weighing over four kilogrammes at birth [32]. The results presented in Kolu et al. suggest that the intervention was not cost-effective for lowering infant birth weight [33]. In Oostdam et al. the ICER for lowering birth weight was less effective and more costly, and hence classified as dominated by the care as usual group. In Dodd et al.’s [32] intervention, the ICER for one additional infant with birth-weight over four kilogrammes was more effective and more costly; however, the authors stated that the intervention was cost neutral due to wide confidence intervals for costs reported in this study.
Other Infant Outcomes
Dodd et al. reported that the intervention was unlikely to be cost-effective for lowering the risk of respiratory distress syndrome [32]. Lack of cost-effectiveness was due to low probability of cost-effectiveness at the willingness to pay threshold.
Sensitivity Analyses
Sensitivity analyses were conducted in all studies. A summary of the different analyses can be found in Appendix 6, Table S12. All RCTs conducted bootstrapping [32,33,34,35,36]. Of these, three studies found no changes in conclusions [32,33,34]. The Broekhuizen study [36] found that the complete case analysis had higher total costs for two of the interventions compared with usual care in the main analysis. The authors concluded that these differences were not significantly different and did not change the overall study conclusions. The authors suggest that the result may have been due to selective drop-out of participants, as differences were found between participants whose data was complete versus incomplete, and that data with imputed values had higher validity. The Poston et al. [35] study used complete case analysis as the base case for their results. The full sample produced ICERs that were lower than the complete case analysis. Probabilistic sensitivity analysis was utilized to measure the joint uncertainty around cost and effect parameters in the modelling study [8], with findings suggesting that there were no significant differences in costs or effects for women with obesity or overweight between intervention and care as usual groups. A summary of the sensitivity analyses can be found in Table S9.
Discussion
Lifestyle interventions have demonstrated efficacy in limiting gestational weight gain and other clinical outcomes, as reflected in meta-analytical studies [10, 11••]. In this systematic review, though, the interventions in the included studies were mostly not cost-effective, primarily due to lack of efficacy over a range of outcome measures in the included studies. Specifically, in the synthesis of the available data on QALYs, only the intervention that used lifestyle coaching related to combined healthy eating and physical activity in the study by Broekhuizen et al. [36] showed cost effective (and in this case cost-saving) results. For the analysis of maternal and infant outcomes, most interventions were either clearly not cost-effective or cost-effectiveness depended on willingness to pay thresholds. Willingness to pay thresholds are difficult to determine for individual outcome types, which is one of the main reasons for the health economist’s preference for using quality of life scales such as QALYs to determine cost-effectiveness [39]. In two of the studies, where the willingness to pay threshold was in question, authors stated that outcomes were unlikely to be cost effective [32, 36]. This assessment was generally made on the basis of data from cost-effectiveness acceptability curve graphs. All included cost-effectiveness studies were rated as high quality on the CHEERS checklist.
The studies included in this review represent only a fraction of all studies conducted on the efficacy of lifestyle interventions to limit gestational weight gain, as most interventions lack cost-effectiveness analyses. Overall, much of the literature shows the benefits of lifestyle interventions; for instance, the meta-analysis from the i-WIP Collaborative group found a 24% reduction in cases of gestational diabetes mellitus attributable to lifestyle intervention in a synthesis of 81 studies [11••]. This recent comprehensive review and meta-analysis of the lifestyle intervention literature supports the efficacy of lifestyle interventions to limit excess weight gain in pregnancy and to reduce adverse maternal events, including gestational diabetes, hypertensive disorders of pregnancy and caesarean section [11••]. The significant results found in the meta-analysis highlight that the results of many of the individual studies were underpowered to demonstrate improved clinical outcomes beyond gestational weight gain; similarly, the cost-effectiveness studies presented in this review were underpowered to determine return on investment. Issues such as heterogeneity and low intervention penetration limit the value of single-study cost effectiveness analyses and suggest that cost effectiveness modelling needs to be completed on integrated meta-analysis data.
Although information from this review did not show cost-effectiveness for most interventions, where an economic analysis had been performed, the data did enable generation of aggregated cost data. Adaptation of cost-effectiveness results to common currencies permitted comparisons across studies and an approximation of cost-effectiveness for the UK and Australia. The largest proportion of total costs was from birth/delivery, suggesting that if there was an effect from interventions on lowering Caesarean section rates, this would have a significant impact on the cost-effectiveness of these lifestyle interventions. It is also important to consider the longer-term implications of higher than recommended weight gain in pregnancy. High infant birth weight and the risk of subsequent obesity for offspring, as well as increasing risk of overweight and obesity in mothers, are significant public health issues [40]. Studies that demonstrate the longer term benefits of healthy lifestyle in pregnancy will be needed to inform more accurate and complete cost effectiveness analyses.
Intervention costs are an integral part of cost-effectiveness analysis and were variable in the included studies. Interventions delivered remotely may be more cost-effective. A recent study by Redman et al. [41] found that significantly less women exceeded the Institute of Medicine guidelines [4] when they received a lifestyle intervention during pregnancy than those that did not. The similar results between lifestyle interventions delivered in person (56% exceeded recommendations) and remotely (58% exceeded recommendation) compared with the control group (85% exceeded recommendations), suggest that this intervention was as effective when delivered remotely. The costs of delivering this intervention remotely were less than half of those for delivering the intervention in person, suggesting that eHealth interventions may be more cost effective in this population. A systematic review and meta-analysis has found that eHealth lifestyle-focused interventions were modestly effective at reducing gestational weight gain [42].
Interventions implemented at low cost could offer significant public health benefits and savings, and further cost-effectiveness modelling studies on aggregate data are required. The cost-effectiveness study by Rogozinska et al [8] was modelled on individual patient data from a total of 36 studies. A further 89 papers were included in a follow up paper by The International Weight Management in Pregnancy Collaborative Group in 2017 [11••]; this analysis is currently being updated and expanded. It is intended that the updated meta-analysis will underpin an updated cost-effectiveness analysis. Further study is also being conducted on the components of the interventions, including use of the TIDieR checklist [43] and taxonomy analysis, to inform future cost effectiveness analyses. If cost-effectiveness is established, implementation science should be utilized for upscaling and delivery of the intervention in a public health context, via production of clinical guidelines and translation into clinical practice [44]. Investigation into intervention effectiveness should be accomplished through a systems thinking perspective, so as to address the barriers to lifestyle change that are inherent in pregnancy as a life-stage [45, 46].
Limitations
There were methodological limitations to this review. Although the search strategy was rigorous, followed established guidelines for systematic review of economic analyses [20] and included a thorough search of grey literature, there remains the possibility that relevant papers not published in English were missed, as well as the potential for bias due to unpublished papers. The authors note that two conference abstracts were found for economic evaluation articles that met the inclusion criteria, but had not yet been published (authors were contacted). A significant limitation of this study was that there were few studies meeting the inclusion criteria, as has been found in similar reviews [47].
Cost adaptation was both a strength and limitation in this study. Adaptation of cost to a single currency and cost-year allows comparison across studies. A limitation to this process is that cost estimates can be interpreted as only representing an estimate of the cost-effectiveness for that country, and thus attention is required when making claims about the results. It is worth noting that differences in changing costs over time (third adaptation section) between the UK and Australia meant that data changes may not be relative between the two costing adaptations. Finally, the short time horizon for assessed studies in the current review means that longer-term effects were not captured; consequently, this might underestimate the cost-effectiveness of interventions.
Conclusion
There is a large body of research investigating the efficacy of lifestyle interventions during pregnancy; however, few studies have included cost-effectiveness analyses. To date, published studies that have included a cost-effectiveness analysis have been performed on studies with limited efficacy. To improve our understanding of the cost-effectiveness of these interventions, there needs to be a better understanding of what types of interventions are most efficacious. This could be achieved using taxonomy research and integrated meta-analysis. Modelling of the aggregated costs and effects of these interventions is now required to enable a better understanding of the cost-effectiveness of lifestyle interventions in pregnancy. The implementation of cost-effective lifestyle interventions population-wide could have significant and long-term positive implications for intergenerational health.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Dinsdale S, Branch K, Cook L, Shucksmith J. “As soon as you’ve had the baby that’s it...” a qualitative study of 24 postnatal women on their experience of maternal obesity care pathways. BMC Public Health. 2016;16:1–13. https://doi.org/10.1186/s12889-016-3289-1.
• Goldstein RF, Abell SK, Ranasinha S, et al. Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA - J Am Med Assoc. 2017;317:2207–25. https://doi.org/10.1001/jama.2017.3635 Findings from this study establish the association between gestational weight gain and maternal and infant outcomes.
World Health Organization. (2018) Obesity. In: Heal. Top. http://www.who.int/topics/obesity/en/. Accessed 20 Feb 2018.
Institute of Medicine and National Research Council Committee to Reexamine IOM Pregnancy Weight Guidelines (2009) Re-examinng IOM Pregnancy Weight Guidelines. In: Rasmussen, K.M. Yaktine A, L. (eds) Weight gain during pregnancy: reexamining the guidelines. National Academies Press, Washington, DC.
Gaillard R. Maternal obesity during pregnancy and cardiovascular development and disease in the offspring. Eur J Epidemiol. 2015;30:1141–52. https://doi.org/10.1007/s10654-015-0085-7.
Cheney K, Farber R, Barratt AL, McGeechan K, de Vries B, Ogle R, et al. Population attributable fractions of perinatal outcomes for nulliparous women associated with overweight and obesity, 1990-2014. Med J Aust. 2018;208:119–25. https://doi.org/10.5694/mja17.00344.
Agha M, Agha RA, Sandell J (2014) Interventions to reduce and prevent obesity in pre-conceptual and pregnant women: a systematic review and meta-analysis. PLoS One 9:. https://doi.org/10.1371/journal.pone.0095132.
Rogozińska E, Marlin N, Jackson L, et al (2017) Effects of antenatal diet and physical activity on maternal and fetal outcomes: individual patient data meta-analysis and health economic evaluation. Health Technol Assess (Rockv) 21:. https://doi.org/10.3310/hta21410.
Farpour-Lambert NJ, Ells LJ, Martinez de Tejada B, Scott C (2018) Obesity and weight gain in pregnancy and postpartum: an evidence review of lifestyle interventions to inform maternal and child health policies. Front Endocrinol (Lausanne) 9:. https://doi.org/10.3389/fendo.2018.00546.
Walker R, Bennett C, Blumfield M, et al. Attenuating pregnancy weight gain—what works and why: a systematic review and meta-analysis. Nutrients. 2018;10:4–6. https://doi.org/10.3390/nu10070944.
•• The International Weight Management in Pregnancy Collaborative Group. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: meta-analysis of individual participant data from randomised trials. BMJ. 2017;358:j3119. https://doi.org/10.1136/bmj.j3119 This study quantifies the effect of lifestyle interventions on maternal and infant outcomes.
Hill B, Skouteris H, Fuller-Tyszkiewicz M. Interventions designed to limit gestational weight gain: a systematic review of theory and meta-analysis of intervention components. Obes Rev. 2013;14:435–50. https://doi.org/10.1111/obr.12022.
Neumann PJ, Farquhar M, Wilkinson CL, Lowry M, Gold M. Lack of cost-effectiveness analyses to address healthy people 2020 priority areas. Am J Public Health. 2016;106:2205–7. https://doi.org/10.2105/AJPH.2016.303361.
Dodd JM, Turnbull D, McPhee AJ, et al. Antenatal lifestyle advice for women who are overweight or obese: LIMIT randomised trial. Obstet Gynecol Surv. 2015;69:311–3. https://doi.org/10.1097/01.ogx.0000451478.28533.cf.
Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12:131–41. https://doi.org/10.1111/j.1467-789X.2009.00712.x.
Whiteman VE, Salemi JL, Mejia De Grubb MC, et al. Additive effects of pre-pregnancy body mass index and gestational diabetes on health outcomes and costs. Obesity. 2015;23:2299–308. https://doi.org/10.1002/oby.21222.
Rowlands I, Graves N, de Jersey S, McIntyre H, Callaway L. Obesity in pregnancy: outcomes and economics. Semin Fetal Neonatal Med. 2010;15:94–9. https://doi.org/10.1016/j.siny.2009.09.003.
PDQ- Evidence Database (2018) PDQ-evidence. https://www.pdq-evidence.org/
El-Khayat YM. Resource review. J Med Libr Assoc. 2017;105:431–2. https://doi.org/10.5195/jmla.2017.260.
Thielen FW, Van Mastrigt GAPG, Burgers LT, et al. How to prepare a systematic review of economic evaluations for clinical practice guidelines: database selection and search strategy development (part 2/3). Expert Rev Pharmacoecon Outcomes Res. 2016;16:705–21. https://doi.org/10.1080/14737167.2016.1246962.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339. https://doi.org/10.1136/bmj.b2700.
Veritas Health Innovation (2018) Covidence systematic review software. Available at www.covidence.org
Husereau D, Drummond M, Petrou S, et al. Consolidated health economic evaluation reporting standards (CHEERS)--explanation and elaboration: a report of the ISPOR health economic evaluations publication guidelines task force. Value Health. 2013;16:231–50. https://doi.org/10.1016/j.jval.2013.02.002.
Ademi Z, Tomonaga Y, Van Stiphout J, et al. Adaptation of cost-effectiveness analyses to a single country: the case of bariatric surgery for obesity and overweight. Swiss Med Wkly. 2018;148:1–13. https://doi.org/10.4414/smw.2018.14626.
Organisation for Economic Co-operation and Development (2018) Health spending (indicator). https://data.oecd.org/healthres/health-spending.htm. Accessed 2 Aug 2018.
Organisation for Economic Co-operation and Development (2018) Purchasing power parities (PPP) (indicator).
Australian Institute of Health and Welfare (2018) Health expenditure Australia 2016–17. Canberra.
Office for National Statistics (2018) Reference table 3: Growth rates and indices for public service healthcare inputs, quantity and quality adjusted output and productivity, 1995 to 2015. https://www.ons.gov.uk/economy/economicoutputandproductivity/publicservicesproductivity/datasets/growthratesandindicesforpublicservicehealthcareinputsquantityandqualityadjustedoutputandproductivity. Accessed 2 Aug 2018.
Appleby J, Devlin N, Parkin D. NICE’s cost effectiveness threshold. BMJ. 2007;335:358–9.
Paris V, Belloni A. Value in pharmaceutical pricing. OECD Heal Work Pap. 2013;63:1–74. https://doi.org/10.1787/5k43jc9v6knx-en.
Edney LC, Haji Ali Afzali H, Cheng TC, Karnon J. Estimating the reference incremental cost-effectiveness ratio for the Australian health system. Pharmacoeconomics. 2018;36:239–52. https://doi.org/10.1007/s40273-017-0585-2.
Dodd JM, Ahmed S, Karnon J, Umberger W, Deussen AR, Tran T, et al. The cost-effectiveness of providing antenatal lifestyle advice for women who are overweight or obese: the LIMIT randomised trial. BMC Obes. 2015;2:1–9. https://doi.org/10.1186/s40608-015-0046-4.
Kolu P, Raitanen J, Rissanen P, Luoto R (2013) Cost-effectiveness of lifestyle counselling as primary prevention of gestational diabetes mellitus: findings from a cluster-randomised trial PLoS One 8:. https://doi.org/10.1371/journal.pone.0056392.
Oostdam N, Bosmans J, Woulters MGAJ, et al (2012) Cost-effectiveness of an exercise program during pregnancy to prevent gestational diabetes: results of an economic evaluation alongside a randomised controlled trial BMC Pregnancy Childbirth 12
Poston L, Bell R, Briley AL, et al. Improving pregnancy outcome in obese women: the UK pregnancies better eating and activity randomised controlled trial. Program Grants Appl Res. 2017;5:1–414. https://doi.org/10.3310/pgfar05100.
Broekhuizen K, Simmons D, Devlieger R, van Assche A, Jans G, Galjaard S, et al. Cost-effectiveness of healthy eating and/or physical activity promotion in pregnant women at increased risk of gestational diabetes mellitus: economic evaluation alongside the DALI study, a European multicenter randomized controlled trial. Int J Behav Nutr Phys Act. 2018;15:1–12. https://doi.org/10.1186/s12966-018-0643-y.
Van Reenen M, Janssen B (2015) EQ-5D-5L user guide. Rotterdam.
Sintonen H (2018) The health state desctiptive system (questionnaire. In: 15d-instrument. http://www.15d-instrument.net/15d/the-health-state-descriptive-system/. Accessed 17 Dec 2018.
Gray AM, Clarke PM, Wolstenholme J, Wordsworth S. Applied methods of cost-effectiveness analysis in healthcare. Oxford: Oxford University Press; 2011.
World Health Organization (2016) Report of the commission on ending childhood obesity. Geneva.
Redman LM, Gilmore LA, Breaux J, et al. Effectiveness of SmartMoms, a novel eHealth intervention for Management of Gestational Weight Gain: randomized controlled pilot trial. JMIR Mhealth Uhealth. 2017;5:e133. https://doi.org/10.2196/mhealth.8228.
Lau Y, Klainin-Yobas P, Htun TP, Wong SN, Tan KL, Ho-Lim ST, et al. Electronic-based lifestyle interventions in overweight or obese perinatal women: a systematic review and meta-analysis. Obes Rev. 2017;18:1071–87.
Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:1–12. https://doi.org/10.1136/bmj.g1687.
Harrison CL, Skouteris H, Boyle J, Teede HJ. Preventing obesity across the preconception, pregnancy and postpartum cycle: implementing research into practice. Midwifery. 2017;52:64–70. https://doi.org/10.1016/j.midw.2017.06.003.
Skouteris H, Huang T, Millar L, et al. A systems approach to reducing maternal obesity: the health in preconception, pregnancy and postbirth (HIPPP) collaborative. Aust New Zeal J Obstet Gynaecol. 2015;55:397–400. https://doi.org/10.1111/ajo.12341.
Hill B, McPhie S, Moran LJ, Harrison P, Huang TT, Teede H, et al. Lifestyle intervention to prevent obesity during pregnancy: implications and recommendations for research and implementation. Midwifery. 2017;49:13–8. https://doi.org/10.1016/j.midw.2016.09.017.
Fitria N, van Asselt ADI, Postma MJ. Cost-effectiveness of controlling gestational diabetes mellitus: a systematic review. Eur J Health Econ. 2018;20:407–17. https://doi.org/10.1007/s10198-018-1006-y.
Funding
CB acknowledges funding support from the Australian Prevention Partnership Centre. BdC is a recipient of the National Heart Foundation (NHF future leader fellowship 100864). HT is a recipient of NHMRC Practitioner fellowship. BH is funded by an NHMRC Early Career Fellowship (GNT1120477).
Author information
Authors and Affiliations
Contributions
CB developed the search strategy, led the data collection and analysis and wrote the initial draft of the manuscript. ZA contributed in the design and scope of search strategy, advised on all aspects of the methodology and contributed expertise to the revision and editing of the manuscript. HS contributed to the conceptualization of the study, the design and scope of the search strategy and revised and edited the manuscript. BH contributed to reviewing data collection and revised and edited the manuscript. HT and BdC contributed to conceptualization of the study and revised and edited the manuscript. DL, RW and ST revised and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Cate Bailey, Helen Skouteris, Helena Teede, Briony Hill, Barbora De Courten, Ruth Walker, Danny Liew, Shakila Thangaratinam and Zanfina Ademi each declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Diabetes and Pregnancy
Electronic supplementary material
ESM 1
(DOCX 181 kb)
Rights and permissions
About this article
Cite this article
Bailey, C., Skouteris, H., Teede, H. et al. Are Lifestyle Interventions to Reduce Excessive Gestational Weight Gain Cost Effective? A Systematic Review. Curr Diab Rep 20, 6 (2020). https://doi.org/10.1007/s11892-020-1288-1
Published:
DOI: https://doi.org/10.1007/s11892-020-1288-1