Abstract
Purpose of Review
In patients with prediabetes or type 2 diabetes, the use of thiazides as antihypertensive agents has been challenged because associated metabolic adverse events, including new-onset diabetes.
Recent Findings
These metabolic disturbances are less marked with low-dose thiazides and, in most but not all studies, with thiazide-like diuretics (chlorthalidone, indapamide) than with thiazide-type diuretics (hydrochlorothiazide). In post hoc analyses of subgroups of patients with hypertension and type 2 diabetes, thiazides resulted in a significant reduction in cardiovascular events, all-cause mortality, and hospitalization for heart failure compared to placebo and generally were shown to be non-inferior to other antihypertensive agents.
Summary
Benefits attributed to thiazide diuretics in terms of cardiovascular event reduction outweigh the risk of worsening glucose control in type 2 diabetes and of new-onset diabetes in non-diabetic patients. Thiazides still play a key role in the management of patients with type 2 diabetes and hypertension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diuretics have a major role in the treatment of arterial hypertension and congestive heart failure [1], two common comorbidities associated with type 2 diabetes (T2D) [2,3,4]. Most patients with T2D are overweight or obese and hypertension linked to obesity is characterized by fluid retention [5]. This observation paves the road to the use of diuretics in patients with T2D and hypertension, either as monotherapy or as a component of any combined therapy [6]. Diuretics belong to a heterogeneous family so that several compounds may be distinguished even within the thiazide pharmacological class [7, 8]. It is common to separate the thiazide-type diuretics (hydrochlorothiazide (HCTZ) as the reference compound [9]) from the so-called thiazide-like diuretics (chlorthalidone (CTD) and indapamide (IDP) [10, 11]).
Thiazide diuretics were the first efficient antihypertensive drugs with a good tolerance profile that significantly reduced cardiovascular (CV) morbidity and mortality in placebo-controlled clinical studies [12]. No study investigated specifically the effects of thiazide diuretics on CV complications and mortality in patients with T2D. Nevertheless, interesting, although limited, data could be derived from post hoc analyses in subgroups of T2D individuals having participated in several large CV outcomes studies that enrolled patients with arterial hypertension [13]. However, thiazides may also exert adverse metabolic effects that may aggravate several CV risk factors; of special interest, they have been suspected to increase the incidence of new-onset diabetes (NOD) in non-diabetic patients with hypertension [14,15,16]. In 1991, because the suspicion of an excess mortality associated with diuretic therapy in diabetes mellitus, it was concluded that “until there is a clinical trial showing a beneficial effect of diuretic treatment in diabetic patients, there is urgent need to reconsider its continued usage in this population” [17]. Nevertheless, in 2017, thiazide diuretics are still a common therapy in hypertensive patients with T2D. In the last couple of years, systematic reviews compared antihypertensive agents in patients with T2D and generally provided results that support the use of thiazide diuretics in this population [18•, 19••, 20•, 21•, 22•, 23•, 24••].
The main objectives of this updated narrative review devoted to the use of thiazide-type and thiazide-like compounds in patients with T2D are as follows: (1) to describe the adverse metabolic effects reported with thiazide diuretics and investigate to what extent thiazides may increase the risk of NOD or worsen the blood glucose control in T2D patients; (2) to analyze the effects of thiazide diuretics on CV outcomes in T2D patients with arterial hypertension; (3) to briefly discuss the results of thiazides in T2D patients with congestive heart failure and in patients with renal impairment and/or (micro)albuminuria; and finally (4) to compare thiazides with inhibitors of sodium-glucose cotransporters type 2 (SGLT2), a new class of glucose-lowering agents with diuretic properties.
Adverse Metabolic Effects of Thiazide Diuretics
Metabolic Effects of Thiazide-Type Versus Thiazide-Like Diuretics
A recent systematic review and meta-analysis of 26 randomized controlled trials (RCTs) involving 16,162 participants demonstrated that thiazide-type diuretics are associated with significant but small adverse effects on fasting plasma glucose (FPG) in hypertensive patients (mean difference, + 0.27 mmol/l; 95% confidence interval or CI 0.15 to 0.39). Patients receiving lower doses of thiazides (HCTZ or CTD ≤ 25 mg daily) had less change in FPG (+ 0.15 mmol/l; 95% CI 0.03 to 0.27) than those receiving higher doses (+ 0.60 mmol/l; 95% CI 0.39 to 0.82) [23•].
Another meta-analysis of 10 RCTs with low-dose thiazide-type and thiazide-like diuretics showed that the cumulative mean change of FPG was + 0.20 mmol/l for the diuretic arm versus + 0.12 mmol/l for the comparator arm, while the cumulative mean change of serum potassium was − 0.22 mmol/l for the diuretic arm versus + 0.05 mmol/l for the comparator arm [25]. A role of hypokalemia in the worsening of glucose tolerance in patients treated with HCTZ has long been suspected [26]. In a quantitative review of 59 clinical trials with 83 thiazide diuretic study arms, an inverse relationship was noticed between changes in glucose and potassium levels (Pearson’s correlation coefficient: − 0.54; 95% CI − 0.67 to − 0.36; p < 0.01) [27]. These data suggest that thiazide-induced hypokalemia is associated with increased blood glucose. Consequently, treatment of thiazide-induced hypokalemia may reverse glucose intolerance and possibly prevent the future development of diabetes [26]. This was confirmed in the PATHWAY-3 trial in non-diabetic patients, in whom the combination of amiloride, a potassium-sparing diuretic, with HCTZ prevents glucose intolerance while improving control of blood pressure compared with HCTZ monotherapy [28].
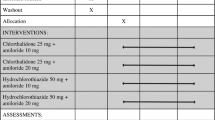
Head-to-head comparisons in RCTs demonstrate that both CTD and IDP are more potent antihypertensive agents than HCTZ at commonly prescribed doses without evidence for greater adverse metabolic effects (Table 1) [29]. This was confirmed in a recent meta-analysis of 12 head-to-head trials (five comparing IDP versus HCTZ and seven comparing CTD versus HCTZ). Using thiazide-like diuretics was superior to thiazide-type diuretics in reducing blood pressure without increasing the incidence of hypokalemia, hyponatremia, and any change of blood glucose (+ 0.13 mmol/l; 95% CI − 0.16 to 0.41, p = 0.39) and serum total cholesterol (Table 1) [20•].
Hydrochlorothiazide
According to a recent meta-analysis of parallel-design RCTs, 13 studies, involving 720 patients, compared the metabolic effects of HCTZ versus no-HCTZ hypertension treatment in patients with T2D [18•]. FPG (standardized mean difference (SMD) = + 0.27 mmol/l; 95% CI 0.11 to 0.43) and glycated hemoglobin (HbA1c) (+ 1.09%; 95% CI 0.47 to 1.72 or + 9.8 mmol/mol, 95% CI 4.2 to 15.5) significantly increased while high-density lipoprotein-cholesterol (HDL-C) (− 0.44 mmol/l; 95% CI − 0.81 to − 0.08) decreased in the patients treated with HCTZ [18•]. However, although low doses (12.5–25 mg/day) of HCTZ elevated serum glucose and worsened lipid profile, the magnitude of effects was small in most cases and probably of minor clinical significance [30].
HCTZ treatment worsened hepatic steatosis measured as hepatic triglyceride content, caused visceral fat accumulation, and reduced insulin sensitivity [31, 32]. Furthermore, HCTZ resulted in a slight but significant deterioration in endothelial function as assessed by flow-mediated vasodilation (FMD) of the brachial artery after 12 and 24 weeks of therapy, despite a significant improvement in blood pressure in hypertensive non-diabetic patients [33].
Chlorthalidone
In ALLHAT (Antihypertensive and Lipid-Lowering Heart Attack Trial) among non-diabetic hypertensive patients at baseline, FPG increased from 5.17 to 5.80 mmol/l after 4 years in the CTD group (12.5 to 25 mg/day); this increase was less marked in the lisinopril group (from 5.18 to 5.58 mmol/l, p < 0.001 vs CTD) but almost similar in the amlodipine group (from 5.17 to 5.73 mmol/l, p = 0.11 vs CTD) [34].
In the SHEP (Systolic Hypertension in the Elderly Program) trial, small effects of CTD (12.5 mg or 25 mg) compared with placebo were observed after 3 years of therapy with FPG (+ 0.20 mmol/l; p < 0.01), total cholesterol (+ 0.09 mmol/l; p < 0.01), and HDL-C (− 0.02 mmol/l; p < 0.01). Larger effects were seen with fasting levels of triglycerides (+ 0.9 mmol/l; P < 0.001), uric acid (+ 35 micromol/l; p < 0.001), and potassium (− 0.3 mmol/l; p < 0.001) [35].
Despite these metabolic changes, CTD improved endothelial function, reversed abnormal arteriolar structure, and slowed albumin permeation in hypertensive non-diabetic patients with metabolic syndrome [36].
Indapamide
In a 2-year Italian multicenter open-label study in non-diabetic patients with systemic hypertension, glucose tolerance was unchanged despite slight but significant reductions in serum potassium with IDP, 2.5 mg once daily. Total cholesterol, HDL-C, and serum triglycerides were unchanged, while uric acid increased significantly in patients receiving IDP [37].
Several studies investigated the metabolic effects of IDP in hypertensive patients with T2D and reported heterogeneous results [11]. The results in people with diabetes were inconclusive due to the small number of participants studied or obtained in different ethnic populations. In an open study in only 10 T2D patients with hypertension, no change in plasma glucose or insulin levels during an oral glucose tolerance test occurred at any time during 1-year therapy with IDP 2.5 mg/day [38]. However, in another open-label trial in 13 hypertensive T2D patients, both mean FPG and integrated glucose responses after an oral glucose load and HbA1c were significantly higher after 24 weeks of IDP therapy compared to baseline levels. In the same trial, IDP caused a slight but non-significant rise in the total triglyceride, total cholesterol, and low-density lipoprotein cholesterol levels, while HDL-C decreased [39]. A placebo-controlled RCT showed that a 3-month treatment with IDP (sustained-release formulation) in hypertensive T2D Chinese patients does not alter or aggravate lipid and glucose profiles and does not exert adverse effects of hypokalemia and hyperuricemia [40]. In a head-to-head trial in hypertensive diabetic patients receiving a background angiotensin-converting enzyme (ACE) inhibitor therapy, IDP 2.5 mg/day resulted in a comparable metabolic profile as compared to HCTZ 12.5 mg/day [41].
Of notable interest, a 6-month treatment with IDP was found to improve measures of endothelial and arterial functions and to increase longitudinal left ventricular function compared with HCTZ in patients with hypertension and T2D [42].
New-Onset Diabetes in Thiazide-Treated Patients
People with elevated blood pressure are at increased risk of diabetes and estimates are similar even after excluding individuals prescribed antihypertensive therapies [43]. Nevertheless, some CV and antihypertensive drugs such as thiazides and beta-blockers increase the risk of NOD diabetes [16, 44]. The potential for occurrence of NOD certainly needs consideration [45], but it is not an insurmountable challenge and must not compromise aggressive blood pressure control, which remains the primary tool for antihypertensive care [46]. Overall clinical benefit in terms of CV event reduction outweighs the risk of NOD [44] (see “Thiazide diuretics as antihypertensive agents”).
In the Japanese DIME (Diuretics In the Management of Essential hypertension) RCT, antihypertensive treatment with low-dose thiazide diuretics at 12.5 mg/day of HCTZ or equivalent was not be associated with an increased risk for NOD [47]. In an observational long-term (up to 40 years) survey of 15,089 hypertensive patients attending the Glasgow Blood Pressure Clinic, 1-in-8 hypertensive patients developed NOD, but mortality was increased only in the 1-in-20 who developed early NOD (no increase in those who developed late NOD) [48]. Furthermore, in this large study, antihypertensive drug use (especially proportion of thiazides) was not different in patients with NOD in comparison with patients who did not develop diabetes.
Careful overview of the literature gives conflicting results when considering the conclusions of systematic reviews and meta-analyses. On the one hand, some publications conclude that the use of thiazide diuretics is associated with the highest risk of NOD in hypertensive patients contrasting with the lowest risk when renin-angiotensin system (RAS) blockers are used [49, 50]. On the other hand, other papers do not support the hypothesis that thiazide diuretics are more strongly associated with the initiation of hypoglycemic therapy than are other antihypertensive agents [21•, 51, 52]. The reasons for such discrepancies are unclear but may result from differences in patient characteristics, type and dose of diuretics, criteria of definition of diabetes, and length of follow-up across the different studies.
According to a European society of hypertension position statement concerning the metabolic syndrome in hypertension, RAS blockers or even calcium channel blockers are preferable over diuretics in monotherapy. However, if a combination of drugs is required, low-dose diuretics can be used, although a combination of thiazide diuretics and beta-blockers should be avoided [53]. Few prospective trials have been conducted in the search of the ideal antihypertensive regimen in patients with obesity and the metabolic syndrome. Though caution exists regarding the use of thiazide diuretics due to potential metabolic derangements, there is insufficient data to show worsened CV outcomes in patients treated with these drugs [54, 55].
Thiazide Diuretics as Antihypertensive Agents
Thiazides in the General Population with Hypertension
Thiazide diuretics are one of the preferred pharmacologic treatments for hypertension. There are significant pharmacokinetic and pharmacodynamic differences between thiazide-type and thiazide-like diuretics. For instance, CTD is approximately 1.5 to 2.0 times as potent as HCTZ, and the former has a much longer duration of action [56]. Similarly, IDP sustained released has a smoother pharmacokinetic and pharmacodynamic profile compared to HCTZ [11]. A systematic COCHRANE review investigated the dose-related decrease in systolic and/or diastolic blood pressure due to thiazide diuretics (HCTZ, CTD, IDP) compared with placebo in the treatment of patients with primary hypertension (independently of the presence of diabetes) [57]. HCTZ has a dose-related blood pressure-lowering effect over the dose range 6.25 to 50 mg/day. For CTD and IDP, the lowest doses studied reduced blood pressure maximally. Due to the greater effect on systolic than on diastolic blood pressure, all thiazides diminish pulse pressure by 4 to 6 mmHg, a difference that exceeds the pulse pressure reduction achieved by RAS inhibitors or beta-blockers [57].
Most studies having investigated the effects of thiazide diuretics on CV outcomes have recruited hypertensive patients without diabetes. A network meta-analysis published in 2003 combined data from 42 clinical trials that included 192,478 patients randomized to major antihypertensive treatment strategies, including placebo. For all clinical outcomes, low-dose diuretics were superior to placebo: coronary heart disease (relative risk (RR), 0.79; 95% CI 0.69 to 0.92); congestive heart failure (RR, 0.51; 0.42 to 0.62); stroke (RR, 0.71; 0.63 to 0.81); CV events (RR, 0.76; 0.69 to 0.83); CV mortality (RR, 0.81; 0.73 to 0.92); and total mortality (RR, 0.90; 0.84 to 0.96). None of the first-line antihypertensive treatment strategies was significantly better than low-dose diuretics for any outcome [58]. The same authors concluded that based on the available data from the placebo-controlled trials evaluating low-dose diuretics, major health outcomes for CTD and other thiazide-like drugs appear to be similar [59].
In 2015, a pooled study of 19 RCTs compared thiazide diuretics (n = 56,802) versus other therapies (control n = 55,311) in patients with hypertension. Thiazide diuretic treatment was associated with reductions in the risks of CV events (odds ratio (OR) 0.86; p = 0.007) and heart failure (OR 0.62; p < 0.001), but no difference in strokes was noticed (OR 0.92; p = 0.438) or coronary heart disease (OR 0.95; p = 0.378) compared to controls [60•]. Further analysis showed that the observed benefits were mainly confined to thiazide-like diuretic therapy (CTD and IDP) rather than thiazide-type diuretics (chlorothiazide and HCTZ) with a significant reduction in the risk of CV events (OR 0.78; p < 0.001), heart failure (OR 0.57; p < 0.001), and stroke (OR 0.82; p = 0.016). This study suggests that use of thiazide diuretic in hypertensive patients results in a reduction in the risk of CV events. Moreover, thiazide-like diuretics have greater cardioprotective effect than thiazide-type diuretics, especially on heart failure [60•]. These results were confirmed in another meta-analysis of 21 RCTs (with > 480,000 patient-years) that specifically compared the effects of thiazide-type and thiazide-like diuretics with placebo or antihypertensive drugs on CV events and mortality in adult hypertensive patients [61•]. Thiazide-like diuretics resulted in a 12% additional risk reduction for CV events (p = 0.049) and a 21% additional risk reduction for heart failure (p = 0.023) when compared with thiazide-type diuretics [61•].
Thus, increasing evidence suggests inferiority of HCTZ in lowering blood pressure and CV outcomes in hypertensive patients when compared with other drugs in the same class, especially thiazide-like diuretics. Thus, CTD and IDP should be preferred over HCTZ in most hypertensive patients when diuretics are required for treatment of hypertension [62].
Patients with T2D and Hypertension
A recent overview of systematic reviews concluded that the available evidence supports treatment in people with T2D and systolic blood pressure more than 140 mmHg, using any of the major antihypertensive drug classes, including thiazide diuretics [22•]. Contrary to past recommendations, there is little or no further benefit in lowering systolic blood pressure below 130 mmHg in patients with T2D [63••]. According to the recent position statement by the American Diabetes Association [63••], initial treatment for hypertension in patients with diabetes should include drug classes demonstrated to exert CV protection. Among thiazide diuretics, CTD and IDP, two long-acting agents shown to reduce major CV events, are preferred [63••]. Although several blood pressure-lowering medications can beneficially be prescribed in hypertensive patients with T2D, it is generally recommended to initiate or include a RAS blocker, in patients with microalbuminuria or proteinuria [19••, 63••, 64].
However, in a meta-analysis of 19 RCTs that enrolled 25,414 participants with diabetes for a total of 95,910 patient years of follow-up, RAS blockers were not superior to other antihypertensive drug classes including thiazide diuretics in reducing the risk of hard CV endpoints and all-cause mortality (RR versus thiazides 0.99; 95% IC 0.90–1.08; results mainly driven by the ALLHAT data) [64]. This was confirmed in a network meta-analysis of 27 RCTs, comprising 49,418 participants, which showed no benefit of a single antihypertensive class in reduction of all-cause mortality and CV mortality in hypertensive patients with T2D [24••]. According to the 2017 standards of medical care in diabetes published by the American Diabetes Association, “among T2D patients without albuminuria for whom CV prevention is the primary goal of blood pressure control, a thiazide-like diuretic may be considered instead of or in addition to a RAS blocker” [65].
A meta-analysis of four placebo-controlled RCTs, published in 2000, investigated the effects of a thiazide-like diuretic—HCTZ or CTD—in subgroups of hypertensive patients with T2D [66]. It showed a reduction by 20% (p = 0.032) of major CV events (a composite of CV mortality, myocardial infarction, and stroke), mainly driven by a reduction in strokes (− 36%, p = 0.011), but no significant differences in CV mortality and all-cause mortality (Table 2) [66].
Since 2000, several publications have analyzed the effects of HCTZ, CTD, and IDP on CV outcomes and mortality in subgroups of hypertensive patients with T2D [13, 67,68,69,70,71,72,73] (Table 2). Overall, the results confirmed that thiazide diuretics are associated with a significant reduction in CV events and mortality when compared with placebo. When thiazide diuretics are compared with ACE inhibitors or calcium channel blockers, most RCTs reported no significant differences whatever the criterion considered. Thiazides were associated with a greater reduction in the rate of heart failure in some trials (Table 2).
In 2017, a meta-analysis compared CV outcomes with thiazide diuretics versus all antihypertensive agents (4–7 trials) [19••]. No significant differences were observed in the incidences of myocardial infarction, stroke, CV mortality, and all-cause mortality. A significant reduction in the rate of heart failure was noticed in patients treated with thiazides (Table 2). No differences between thiazide diuretics and other antihypertensive agents were observed in two composite endpoints: coronary heart disease plus stroke (OR 1.04; 95% IC 0.98 to 1.11) and coronary heart disease plus stroke plus heart failure (OR 0.97; 95% IC 0.93 to 1.02) [19••].
Studies with IDP in hypertensive patients with T2D are difficult to interpret because of the study designs [11]. In the NESTOR (Natrilix SR Versus Enalapril Study in Hypertensive Type 2 Diabetics With MicrOalbuminuRia) trial, IDP sustained release was not less effective than enalapril in reducing microalbuminuria and blood pressure in patients aged > 65 years of age with T2D and hypertension [74] and was more effective than enalapril in reducing BP in elderly diabetic hypertensive patients with marked sodium retention [75]. However, this 1-year study was not powered to study CV outcomes. In the HYVET (HYpertension in the Very Elderly Trial) study, antihypertensive treatment with IDP sustained release, with or without perindopril, in persons 80 years of age or older was associated with significant reductions in the rates of strokes (− 30%), death from any cause (− 21%), death from CV disease (− 23%), and heart failure (− 64%) after a mean follow-up of 1.8 years; however, less than 7% of patients had diabetes, a low number that does not allow a specific subanalysis [76]. In a subgroup analysis of the real-life, observational, PICASSO (Perindopril Plus Indapamide Combination Blood Pressure Reduction) study, 2762 hypertensive patients with T2DM or prediabetes unsuccessfully treated with antihypertensive agents were switched to a fixed-dose combination of perindopril 10 mg/IDP 2.5 mg; after 3 months, the perindopril-IDP combination resulted in significant reductions in office and 24-h ambulatory blood pressures, with a good tolerance profile; however, besides being an open-label study without a controlled group, PICASSO was too short to investigate CV outcomes [77].
The largest RCT designed to study the effect of IDP on CV outcomes in patients with T2D and hypertension was the ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron—MR-Controlled Evaluation) trial [69]. It investigated a fixed combination of perindopril 4 mg and IDP 1.25 mg compared to placebo on macrovascular and microvascular outcomes in 11,140 patients with T2D. The combined therapy resulted in a mean reduction in systolic blood pressure of 5.6 mmHg and diastolic blood pressure of 2.2 mmHg. After a mean follow-up of 4.3 years, the RR of a major macrovascular or microvascular event was significantly reduced: HR 0.91, 95% CI 0.83–1.00; p = 0.04. The separate reductions in macrovascular and microvascular events were almost similar but were not independently significant. Of note, the RRs of death from CV disease and death from any cause were significantly reduced (Table 2). However, because of the design of the study, it is impossible to dissociate the role of IDP from that of the ACE inhibitor perindopril on the beneficial effects reported in this trial, which was mainly designed to assess the effect of a more intensive blood pressure control [69].
Thiazides in Patients with T2D and Other Comorbidities
Thiazides and Heart Failure in T2D
Heart failure is becoming a major CV complication of T2D [4] and diuretic therapy is a part of the management plan in patients with heart failure. Of note, loop diuretics or mineralocorticoid antagonists rather than thiazide(like) agents are generally considered as the best option, in the absence of dedicated studies with the latter compounds. However, recent studies suggested that combination of loop diuretics with thiazide-type diuretics may be helpful in heart failure [78] or even investigated the additional role of thiazide-like diuretics in acute heart failure as a potential approach to an unmet need [79]. The ongoing CLOROTIC trial is a double-blind, randomized, placebo-controlled study to determine the effect of combined diuretic therapy (loop diuretics with thiazide-type diuretics) among patients with decompensated heart failure (but not exclusively diabetic patients) [80].
Thiazides in T2D Patients with Albuminuria and/or Renal Impairment
Diuretics are agents commonly used in diseases characterized by excess extracellular fluid, including chronic kidney disease (CKD) [81]. Besides their effect on extracellular fluid volume control, they are also able to reduce excretion of protein in urine and lessen the risk of developing hyperkalemia [81]. However, diuretic-related adverse events involve increase in uric acid, electrolyte disturbances, and metabolic (glucose, lipids) abnormalities, which may be of clinical relevance, especially in diabetic patients with CKD [81]. It is generally believed that loop diuretics should be preferred in patients (with or without diabetes) with renal impairment and that thiazide compounds are not sufficiently potent to cause meaningful natriuresis and diuresis in patients with CKD [82]. However, thiazides may be combined with loop diuretics [83]. Emerging evidence suggests that thiazide diuretics are effective as blood pressure-lowering drugs in patients with advanced CKD [84]. However, most of these studies were performed in non-diabetic patients.
In diabetic patients, a possible renoprotective effect of thiazide agents has been reported. Sodium restriction, either via low dietary intake or via HCTZ 50 mg/day, was shown to be an effective intervention to increase RAS blockade efficacy in T2D nephropathy [85]. The combination of HCTZ and loop diuretics improved blood pressure levels and decreased proteinuria even in T2D patients with advanced-stage nephropathy and severe edema [86]. A 12-week crossover study showed that IDP was equally effective as captopril in reducing blood pressure and albumin excretion rate (average reduction 30–40%) in diabetic patients with established microalbuminuria [87]. Similar results were reported in the NESTOR trial in which IDP sustained release was equivalent to enalapril in reducing microalbuminuria, with similar effective blood pressure reduction in patients with hypertension and T2D [88]. In the PREMIER (Preterax in albuminuria regression) trial, first-line treatment with low-dose combination perindopril/IDP induced a greater decrease in albuminuria than enalapril, partially independent of blood pressure reduction [89]. In the ADVANCE trial, the treatment benefits of a routine administration of a fixed combination of perindopril-IDP on CV and renal outcomes were consistent across all stages of CKD at baseline [90].
Thiazides and SGLT2 Inhibitors
Hydrochlorothiazide Versus SGLT2 Inhibitors
SGLT2 inhibitors by promoting glucosuria and natriuresis improve blood glucose control, reduce body weight, lower arterial blood pressure, and diminish serum uric acid levels [91]. In EMPA-REG OUTCOME in T2D patients with previous CV complications, empagliflozin reduced the incidence of the primary composite endpoint (CV mortality, non-fatal myocardial infarction non-fatal stroke), CV mortality, all-cause mortality, and hospitalization for heart failure (Table 2) [92]. A diuretic effect has been proposed to explain these favorable results [93], although this hypothesis may be challenged [94].
As recently reviewed [95], three studies compared the effects HCTZ 12.5 to 25 mg/day with those of a SGLT2 inhibitor in 4–12-week head-to-head trials: canagliflozin 300 mg/day [96], dapagliflozin 10 mg/day [97], and ertugliflozin (up to 25 mg/day) [98]. The blood pressure-lowering effect of SGLT2 inhibitors was almost similar to that observed with HCTZ, but without inducing significant changes in serum electrolyte levels or activation of the RAS; furthermore, SGLT2 inhibitors reduced serum uric acid levels [91], while an increase is commonly observed with HCTZ [14].
SGLT2 Inhibitors as Add-On to Thiazide Diuretics
No significant pharmacokinetic interactions have been reported between HCTZ and empagliflozin [99] or canagliflozin [24••]. Interactions with CTD or IDP have not been tested. When empagliflozin 25 mg was co-administered with HCTZ 25 mg, urinary glucose excretion remained high, 24-h urinary sodium excretion further increased, and the RAS was activated [100]. In both EMPA-REG OUTCOME study and CANVAS program, numerous T2D patients with an history of CV disease were already treated with a diuretic compound (around 40–45%), mostly thiazide or thiazide-like agents, at baseline and received a SGLT2 inhibitor or a placebo as add-on therapy. In EMPA-REG OUTCOME, no significant differences were observed in the reduction in CV composite endpoint (p = 0.72 for interaction patients with versus without diuretic) and CV mortality (p = 0.46 for interaction patients with versus without diuretic) whatever the presence or not of a diuretic at baseline [92]. In the CANVAS program, however, a marked reduction in the composite CV endpoint was observed with canagliflozin in patients receiving a diuretic at baseline (HR 0.66; 95% CI 0.59 to 0.79) contrasting with no reduction at all in patients without a diuretic as background therapy (HR 1.11; 95% CI 0.93 to 1.34), and the p value testing the interaction was highly significant (p < 0.001) [101]. The clinical significance of this difference remains unclear and such post hoc subgroup analysis should only be considered as exploratory. It may be speculated that patients already receiving a diuretic at baseline were those characterized by some degree of excessive extracellular fluid, a clinical condition that may be favorably influenced by the addition of a SGLT2 inhibitor.
Conclusion
Thiazide diuretics may be associated with metabolic disturbances, not only dyslipidemia and hyperuricemia but also impaired glucose tolerance and NOD in hypertensive patients who are already prone to develop T2D. Although the changes are rather limited with low-dose thiazides, all these metabolic abnormalities may be considered as CV risk factors, which could interfere with CV outcomes. For that reason, reluctance was expressed regarding the use of thiazide diuretics for the treatment of hypertension in patients with T2D. Nevertheless, thiazides are still commonly used in this population, either as initial monotherapy or more often as a key element of many combined antihypertensive therapies. Despite possible metabolic adverse effects, thiazides have shown better CV outcomes compared to placebo and almost similar CV outcomes compared to other antihypertensive medications not only in the non-diabetic population but also, and to a similar extent, in patients with T2D. Thiazide-like diuretics have been more extensively studied in patients with T2D than thiazide-type diuretics. CTD and IDP seem to have a better metabolic profile and may be associated with better CV outcomes as compared to the thiazide-type reference compound HCTZ.
References
Papers of particular interest, published recently, have been highlighted as: •Of importance •• Of major importance
Roush GC, Kaur R, Ernst ME. Diuretics: a review and update. J Cardiovasc Pharmacol Ther. 2014;19(1):5–13. https://doi.org/10.1177/1074248413497257.
Ferrannini E, Cushman WC. Diabetes and hypertension: the bad companions. Lancet. 2012;380(9841):601–10. https://doi.org/10.1016/S0140-6736(12)60987-8.
McMurray JJ, Gerstein HC, Holman RR, Pfeffer MA. Heart failure: a cardiovascular outcome in diabetes that can no longer be ignored. Lancet Diabetes Endocrinol. 2014;2(10):843–51. https://doi.org/10.1016/S2213-8587(14)70031-2.
Bahtiyar G, Gutterman D, Lebovitz H. Heart failure: a major cardiovascular complication of diabetes mellitus. Curr Diabetes Rep. 2016;16(11):116. https://doi.org/10.1007/s11892-016-0809-4.
Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116(6):991–1006. https://doi.org/10.1161/CIRCRESAHA.116.305697.
Grossman E, Verdecchia P, Shamiss A, Angeli F, Reboldi G. Diuretic treatment of hypertension. Diabetes Care. 2011;34(Suppl 2):S313–9. https://doi.org/10.2337/dc11-s246.
Sica DA, Carter B, Cushman W, Hamm L. Thiazide and loop diuretics. J Clin Hypertens (Greenwich). 2011;13(9):639–43. https://doi.org/10.1111/j.1751-7176.2011.00512.x.
Tamargo J, Segura J, Ruilope LM. Diuretics in the treatment of hypertension. Part 1: thiazide and thiazide-like diuretics. Expert Opin Pharmacother. 2014;15(4):527–47. https://doi.org/10.1517/14656566.2014.879118.
Rosendorff C. Why are we still using hydrochlorothiazide? J Clin Hypertens (Greenwich). 2011;13(12):867–9. https://doi.org/10.1111/j.1751-7176.2011.00566.x.
DiNicolantonio JJ, Bhutani J, Lavie CJ, O’Keefe JH. Evidence-based diuretics: focus on chlorthalidone and indapamide. Futur Cardiol. 2015;11(2):203–17. https://doi.org/10.2217/fca.14.83.
Robinson DM, Wellington K. Indapamide sustained release: a review of its use in the treatment of hypertension. Drugs. 2006;66(2):257–71. https://doi.org/10.2165/00003495-200666020-00011.
Salvetti A, Ghiadoni L. Thiazide diuretics in the treatment of hypertension: an update. J Am Soc Nephrol. 2006;17(4 Suppl 2):S25–9. https://doi.org/10.1681/ASN.2005121329.
Whelton PK, Barzilay J, Cushman WC, Davis BR, Iiamathi E, Kostis JB, et al. Clinical outcomes in antihypertensive treatment of type 2 diabetes, impaired fasting glucose concentration, and normoglycemia: Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2005;165(12):1401–9. https://doi.org/10.1001/archinte.165.12.1401.
Sica DA. Diuretic-related side effects: development and treatment. J Clin Hypertens (Greenwich). 2004;6(9):532–40.
Cooper-DeHoff RM. Thiazide-induced dysglycemia: it’s time to take notice. Expert Rev Cardiovasc Ther. 2008;6(10):1291–4. https://doi.org/10.1586/14779072.6.10.1291.
Fathallah N, Slim R, Larif S, Hmouda H, Ben Salem C. Drug-induced hyperglycaemia and diabetes. Drug Saf. 2015;38(12):1153–68. https://doi.org/10.1007/s40264-015-0339-z.
Warram JH, Laffel LM, Valsania P, Christlieb AR, Krolewski AS. Excess mortality associated with diuretic therapy in diabetes mellitus. Arch Intern Med. 1991;151(7):1350–6. https://doi.org/10.1001/archinte.1991.00400070114014.
• Lin JJ, Chang HC, Ku CT, Chen HY. Hydrochlorothiazide hypertension treatment induced metabolic effects in type 2 diabetes: a meta-analysis of parallel-design RCTs. Eur Rev Med Pharmacol Sci. 2016;20(13):2926–46. This meta-analysis concludes that while thiazide diuretics are still a recommended medication of hypertension therapy for type 2 diabetes, treatment with low-dose HCTZ should be attempted to evaluate the effectiveness and adverse metabolic effects.
•• Thomopoulos C, Parati G, Zanchetti A. Effects of blood-pressure-lowering treatment on outcome incidence in hypertension: 10—should blood pressure management differ in hypertensive patients with and without diabetes mellitus? Overview and meta-analyses of randomized trials. J Hypertens. 2017;35(5):922–44. https://doi.org/10.1097/HJH.0000000000001276. This systematic review compares the effects on cardiovascular and renal outcomes of blood pressure lowering by different drug classes in patients with and without diabetes mellitus.
• Liang W, Ma H, Cao L, Yan W, Yang J. Comparison of thiazide-like diuretics versus thiazide-type diuretics: a meta-analysis. J Cell Mol Med. 2017;21(11):2634–42. https://doi.org/10.1111/jcmm.13205. This comparative meta-analysis concludes that using thiazide-like diuretics is superior to thiazide-type diuretics in reducing blood pressure without increasing the incidence of metabolic disturbances.
• Yang Y, Xu H. Comparing six antihypertensive medication classes for preventing new-onset diabetes mellitus among hypertensive patients: a network meta-analysis. J Cell Mol Med. 2017;21(9):1742–50. https://doi.org/10.1111/jcmm.13096. This network meta-analysis concludes that hydrochlorothiazide exhibits a reliable performance in comparison with other antihypertensive agents although RAS blockers appear superior.
• Brunstrom M, Eliasson M, Nilsson PM, Carlberg B. Blood pressure treatment levels and choice of antihypertensive agent in people with diabetes mellitus: an overview of systematic reviews. J Hypertens. 2017;35(3):453–62. https://doi.org/10.1097/HJH.0000000000001183. This paper concludes that the available evidence supports treatment in people with type 2 diabetes and systolic blood pressure more than 140 mmHg, using any of the major antihypertensive drug classes, includinf thiazide diuretics.
• Zhang X, Zhao Q. Association of thiazide-type diuretics with glycemic changes in hypertensive patients: a systematic review and meta-analysis of randomized controlled clinical trials. J Clin Hypertens (Greenwich). 2016;18(4):342–51. https://doi.org/10.1111/jch.12679. This meta-analysis concludes that thiazide-type diuretics are associated with significant but small adverse glycemic effects in hypertensive patients and that a lower dose might reduce or avoid glycemic changes.
•• Remonti LR, Dias S, Leitao CB, Kramer CK, Klassman LP, Welton NJ, et al. Classes of antihypertensive agents and mortality in hypertensive patients with type 2 diabetes—network meta-analysis of randomized trials. J Diabetes Complicat. 2016;30(6):1192–200. https://doi.org/10.1016/j.jdiacomp.2016.04.020. This network meta-analysis concludes that there is no benefit of a single antihypertensive class in reduction of mortality in hypertensive patients with type 2 diabetes.
Mukete BN, Rosendorff C. Effects of low-dose thiazide diuretics on fasting plasma glucose and serum potassium-a meta-analysis. J Am Soc Hypertens. 2013;7(6):454–66. https://doi.org/10.1016/j.jash.2013.05.004.
Helderman JH, Elahi D, Andersen DK, Raizes GS, Tobin JD, Shocken D, et al. Prevention of the glucose intolerance of thiazide diuretics by maintenance of body potassium. Diabetes. 1983;32(2):106–11. https://doi.org/10.2337/diab.32.2.106.
Zillich AJ, Garg J, Basu S, Bakris GL, Carter BL. Thiazide diuretics, potassium, and the development of diabetes: a quantitative review. Hypertension. 2006;48(2):219–24. https://doi.org/10.1161/01.HYP.0000231552.10054.aa.
Brown MJ, Williams B, Morant SV, Webb DJ, Caulfield MJ, Cruickshank JK, et al. Effect of amiloride, or amiloride plus hydrochlorothiazide, versus hydrochlorothiazide on glucose tolerance and blood pressure (PATHWAY-3): a parallel-group, double-blind randomised phase 4 trial. Lancet Diabetes Endocrinol. 2016;4(2):136–47. https://doi.org/10.1016/S2213-8587(15)00377-0.
Roush GC, Ernst ME, Kostis JB, Tandon S, Sica DA. Head-to-head comparisons of hydrochlorothiazide with indapamide and chlorthalidone: antihypertensive and metabolic effects. Hypertension. 2015;65(5):1041–6. https://doi.org/10.1161/HYPERTENSIONAHA.114.05021.
Weir MR, Flack JM, Applegate WB. Tolerability, safety, and quality of life and hypertensive therapy: the case for low-dose diuretics. Am J Med. 1996;101(3A):83S–92S. https://doi.org/10.1016/S0002-9343(96)00271-9.
Price AL, Lingvay I, Szczepaniak EW, Wiebel J, Victor RG, Szczepaniak LS. The metabolic cost of lowering blood pressure with hydrochlorothiazide. Diabetol Metab Syndr. 2013;5(1):35. https://doi.org/10.1186/1758-5996-5-35.
Eriksson JW, Jansson PA, Carlberg B, Hagg A, Kurland L, Svensson MK, et al. Hydrochlorothiazide, but not Candesartan, aggravates insulin resistance and causes visceral and hepatic fat accumulation: the mechanisms for the diabetes preventing effect of Candesartan (MEDICA) Study. Hypertension. 2008;52(6):1030–7. https://doi.org/10.1161/HYPERTENSIONAHA.108.119404.
Muiesan ML, Salvetti M, Belotti E, Paini A, Rosei CA, Aggiusti C, et al. Effects of barnidipine in comparison with hydrochlorothiazide on endothelial function, as assessed by flow mediated vasodilatation in hypertensive patients. Blood Press. 2011;20(4):244–51. https://doi.org/10.3109/08037051.2011.561072.
Officers A, Coordinators for the ACRGTA, Lipid-Lowering Treatment to Prevent Heart Attack. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288(23):2981–97.
Savage PJ, Pressel SL, Curb JD, Schron EB, Applegate WB, Black HR, et al. Influence of long-term, low-dose, diuretic-based, antihypertensive therapy on glucose, lipid, uric acid, and potassium levels in older men and women with isolated systolic hypertension: the Systolic Hypertension in the Elderly Program. SHEP Cooperative Research Group. Arch Intern Med. 1998;158(7):741–51.
Dell'Omo G, Penno G, Del Prato S, Pedrinelli R. Chlorthalidone improves endothelial-mediated vascular responses in hypertension complicated by nondiabetic metabolic syndrome. J Cardiovasc Pharmacol Ther. 2005;10(4):265–72. https://doi.org/10.1177/107424840501000406.
Leonetti G, Rappelli A, Salvetti A, Scapellato L. Long-term effects of indapamide: final results of a two-year Italian multicenter study in systemic hypertension. Am J Cardiol. 1990;65(17):67H–H71. https://doi.org/10.1016/0002-9149(90)90347-4.
Harrower AD, McFarlane G. Antihypertensive therapy in diabetic patients. The use of indapamide. Am J Med. 1988;84(1B):89–91.
Osei K, Holland G, Falko JM. Indapamide. Effects on apoprotein, lipoprotein, and glucoregulation in ambulatory diabetic patients. Arch Intern Med. 1986;146(10):1973–7. https://doi.org/10.1001/archinte.1986.00360220131023.
Kuo SW, Pei D, Hung YJ, Hsieh AT, Wu LY, Hsieh CH, et al. Effect of indapamide SR in the treatment of hypertensive patients with type 2 diabetes. Am J Hypertens. 2003;16(8):623–8.
Krum H, Skiba M, Gilbert RE. Comparative metabolic effects of hydrochlorothiazide and indapamide in hypertensive diabetic patients receiving ACE inhibitor therapy. Diabet Med. 2003;20(9):708–12. https://doi.org/10.1046/j.1464-5491.2003.01023.x.
Vinereanu D, Dulgheru R, Magda S, Dragoi Galrinho R, Florescu M, Cinteza M, et al. The effect of indapamide versus hydrochlorothiazide on ventricular and arterial function in patients with hypertension and diabetes: results of a randomized trial. Am Heart J. 2014;168(4):446–56. https://doi.org/10.1016/j.ahj.2014.06.010.
Emdin CA, Anderson SG, Woodward M, Rahimi K. Usual blood pressure and risk of new-onset diabetes: evidence from 4.1 million adults and a meta-analysis of prospective studies. J Am Coll Cardiol. 2015;66(14):1552–62. https://doi.org/10.1016/j.jacc.2015.07.059.
Ong KL, Barter PJ, Waters DD. Cardiovascular drugs that increase the risk of new-onset diabetes. Am Heart J. 2014;167(4):421–8. https://doi.org/10.1016/j.ahj.2013.12.025.
Mancia G, Grassi G, Zanchetti A. New-onset diabetes and antihypertensive drugs. J Hypertens. 2006;24(1):3–10. https://doi.org/10.1097/01.hjh.0000194119.42722.21.
Alderman MH. New onset diabetes during antihypertensive therapy. Am J Hypertens. 2008;21(5):493–9. https://doi.org/10.1038/ajh.2008.17.
Ueda S, Morimoto T, Ando S, Takishita S, Kawano Y, Shimamoto K, et al. A randomised controlled trial for the evaluation of risk for type 2 diabetes in hypertensive patients receiving thiazide diuretics: Diuretics In the Management of Essential hypertension (DIME) study. BMJ Open. 2014;4(7):e004576. https://doi.org/10.1136/bmjopen-2013-004576.
Lip S, Jeemon P, McCallum L, Dominiczak AF, McInnes GT, Padmanabhan S. Contrasting mortality risks among subgroups of treated hypertensive patients developing new-onset diabetes. Eur Heart J. 2016;37(12):968–74. https://doi.org/10.1093/eurheartj/ehv557.
Elliott WJ, Meyer PM. Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis. Lancet. 2007;369(9557):201–7. https://doi.org/10.1016/S0140-6736(07)60108-1.
Nizamuddin M, Elliott WJ. Incident diabetes with antihypertensive drugs: updated network and Bayesian meta-analyses of clinical trial data. J Am Soc Hypertension. 2015;9(Suppl):e24. https://doi.org/10.1016/j.jash.2015.03.057.
Gurwitz JH, Bohn RL, Glynn RJ, Monane M, Mogun H, Avorn J. Antihypertensive drug therapy and the initiation of treatment for diabetes mellitus. Ann Intern Med. 1993;118(4):273–8. https://doi.org/10.7326/0003-4819-118-4-199302150-00005.
Barzilay JI, Cutler JA, Davis BR. Antihypertensive medications and risk of diabetes mellitus. Curr Opin Nephrol Hypertens. 2007;16(3):256–60. https://doi.org/10.1097/MNH.0b013e328057dea2.
Redon J, Cifkova R, Laurent S, Nilsson P, Narkiewicz K, Erdine S, et al. The metabolic syndrome in hypertension: European Society of Hypertension Position Statement. J Hypertens. 2008;26(10):1891–900. https://doi.org/10.1097/HJH.0b013e328302ca38.
Owen JG, Reisin E. Anti-hypertensive drug treatment of patients with and the metabolic syndrome and obesity: a review of evidence, meta-analysis, post hoc and guidelines publications. Curr Hypertens Rep. 2015;17(6):558. https://doi.org/10.1007/s11906-015-0558-9.
Arroll B, Kenealy T, Elley CR. Should we prescribe diuretics for patients with prediabetes and hypertension? BMJ. 2008;337(aug21 1):a679. https://doi.org/10.1136/bmj.a679.
Carter BL, Ernst ME, Cohen JD. Hydrochlorothiazide versus chlorthalidone: evidence supporting their interchangeability. Hypertension. 2004;43(1):4–9. https://doi.org/10.1161/01.HYP.0000103632.19915.0E.
Musini VM, Nazer M, Bassett K, Wright JM. Blood pressure-lowering efficacy of monotherapy with thiazide diuretics for primary hypertension. Cochrane Database Syst Rev. 2014;5:CD003824. https://doi.org/10.1002/14651858.CD003824.pub2.
Psaty BM, Lumley T, Furberg CD, Schellenbaum G, Pahor M, Alderman MH, et al. Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. JAMA. 2003;289(19):2534–44. https://doi.org/10.1001/jama.289.19.2534.
Psaty BM, Lumley T, Furberg CD. Meta-analysis of health outcomes of chlorthalidone-based vs nonchlorthalidone-based low-dose diuretic therapies. JAMA. 2004;292(1):43–4. https://doi.org/10.1001/jama.292.1.43-c.
• Chen P, Chaugai S, Zhao F, Wang DW. Cardioprotective effect of thiazide-like diuretics: a meta-analysis. Am J Hypertens. 2015;28(12):1453–63. https://doi.org/10.1093/ajh/hpv050. This meta-analysis concludes that thiazide-like diuretics have greater protective effect against cardiovascular events than thiazide-type diuretics, especially on heart failure.
• Olde Engberink RH, Frenkel WJ, van den Bogaard B, Brewster LM, Vogt L, van den Born BJ. Effects of thiazide-type and thiazide-like diuretics on cardiovascular events and mortality: systematic review and meta-analysis. Hypertension. 2015;65(5):1033–40. https://doi.org/10.1161/HYPERTENSIONAHA.114.05122. This systematic review concludes that the best available evidence seems to favor thiazide-like diuretics as the drug of choice when thiazide treatment is considered for hypertension.
Vongpatanasin W. Hydrochlorothiazide is not the most useful nor versatile thiazide diuretic. Curr Opin Cardiol. 2015;30(4):361–5. https://doi.org/10.1097/HCO.0000000000000178.
•• de Boer IH, Bangalore S, Benetos A, Davis AM, Michos ED, Muntner P, et al. Diabetes and hypertension: a position statement by the American Diabetes Association. Diabetes Care. 2017;40(9):1273–84. https://doi.org/10.2337/dci17-0026. This Position Statement is intended to update the assessment and treatment of hypertension among patients with diabetes, including advances in care.
Bangalore S, Fakheri R, Toklu B, Messerli FH. Diabetes mellitus as a compelling indication for use of renin angiotensin system blockers: systematic review and meta-analysis of randomized trials. BMJ. 2016;352:i438. https://doi.org/10.1136/bmj.i438.
American Diabetes Association. Standards of medical care in diabetes—2017. Diabetes Care. 2017;40(Suppl 1):S1–S135.
Lievre M, Gueyffier F, Ekbom T, Fagard R, Cutler J, Schron E, et al. Efficacy of diuretics and beta-blockers in diabetic hypertensive patients. Results from a meta-analysis. The INDANA Steering Committee. Diabetes Care. 2000;23(Suppl 2):B65–71.
Curb JD, Pressel SL, Cutler JA, Savage PJ, Applegate WB, Black H, et al. Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. Systolic Hypertension in the Elderly Program Cooperative Research Group. JAMA. 1996;276(23):1886–92. https://doi.org/10.1001/jama.1996.03540230036032.
Kostis JB, Wilson AC, Freudenberger RS, Cosgrove NM, Pressel SL, Davis BR, et al. Long-term effect of diuretic-based therapy on fatal outcomes in subjects with isolated systolic hypertension with and without diabetes. Am J Cardiol. 2005;95(1):29–35. https://doi.org/10.1016/j.amjcard.2004.08.059.
Patel A, MacMahon S, Chalmers J, Neal B, Woodward M, Billot L, et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet. 2007;370(9590):829–40. https://doi.org/10.1016/S0140-6736(07)61303-8.
Niskanen L, Hedner T, Hansson L, Lanke J, Niklason A, Group CS. Reduced cardiovascular morbidity and mortality in hypertensive diabetic patients on first-line therapy with an ACE inhibitor compared with a diuretic/beta-blocker-based treatment regimen: a subanalysis of the Captopril Prevention Project. Diabetes Care. 2001;24(12):2091–6.
Lindholm LH, Hansson L, Ekbom T, Dahlof B, Lanke J, Linjer E, et al. Comparison of antihypertensive treatments in preventing cardiovascular events in elderly diabetic patients: results from the Swedish Trial in Old Patients with Hypertension-2. STOP Hypertension-2 Study Group. J Hypertens. 2000;18(11):1671–5. https://doi.org/10.1097/00004872-200018110-00020.
Mancia G, Brown M, Castaigne A, de Leeuw P, Palmer CR, Rosenthal T, et al. Outcomes with nifedipine GITS or Co-amilozide in hypertensive diabetics and nondiabetics in Intervention as a Goal in Hypertension (INSIGHT). Hypertension. 2003;41(3):431–6. https://doi.org/10.1161/01.HYP.0000057420.27692.AD.
Weber MA, Bakris GL, Jamerson K, Weir M, Kjeldsen SE, Devereux RB, et al. Cardiovascular events during differing hypertension therapies in patients with diabetes. J Am Coll Cardiol. 2010;56(1):77–85. https://doi.org/10.1016/j.jacc.2010.02.046.
Puig JG, Marre M, Kokot F, Fernandez M, Jermendy G, Opie L, et al. Efficacy of indapamide SR compared with enalapril in elderly hypertensive patients with type 2 diabetes. Am J Hypertens. 2007;20(1):90–7. https://doi.org/10.1016/j.amjhyper.2006.05.018.
Zhang Y, Agnoletti D, Wang JG, Xu Y, Safar ME. Natriuresis and blood pressure reduction in hypertensive patients with diabetes mellitus: the NESTOR study. J Am Soc Hypertens. 2015;9(1):21–8. https://doi.org/10.1016/j.jash.2014.10.003.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887–98. https://doi.org/10.1056/NEJMoa0801369.
Farsang C. Efficacy and tolerability of fixed-dose combination of perindopril/indapamide in type 2 diabetes mellitus: PICASSO trial. Adv Ther. 2014;31(3):333–44. https://doi.org/10.1007/s12325-014-0107-y.
Jentzer JC, DeWald TA, Hernandez AF. Combination of loop diuretics with thiazide-type diuretics in heart failure. J Am Coll Cardiol. 2010;56(19):1527–34. https://doi.org/10.1016/j.jacc.2010.06.034.
Patterson JH, Adams KF Jr. Investigating the role of thiazide-like diuretics in acute heart failure: potential approach to an unmet need. J Card Fail. 2016;22(7):537–8. https://doi.org/10.1016/j.cardfail.2016.05.001.
Trullas JC, Morales-Rull JL, Casado J, Freitas Ramirez A, Manzano L, Formiga F, et al. Rationale and design of the “Safety and Efficacy of the Combination of Loop with Thiazide-type Diuretics in Patients with Decompensated Heart Failure (CLOROTIC) Trial”: a double-blind, randomized, placebo-controlled study to determine the effect of combined diuretic therapy (loop diuretics with thiazide-type diuretics) among patients with decompensated heart failure. J Card Fail. 2016;22(7):529–36. https://doi.org/10.1016/j.cardfail.2015.11.003.
Sica DA. Diuretic use in renal disease. Nat Rev Nephrol. 2011;8(2):100–9. https://doi.org/10.1038/nrneph.2011.175.
Izzo JL Jr, Tobe SW. Is there a preferred diuretic class for patients with renal impairment and hypertension? J Am Soc Hypertens. 2016;10(4):282–4. https://doi.org/10.1016/j.jash.2016.02.008.
Elliott WJ, Jurca S. Loop diuretics are most appropriate for hypertension treatment in chronic kidney disease. J Am Soc Hypertens. 2016;10(4):285–7. https://doi.org/10.1016/j.jash.2016.02.007.
Karadsheh F, Weir MR. Thiazide and thiazide-like diuretics: an opportunity to reduce blood pressure in patients with advanced kidney disease. Curr Hypertens Rep. 2012;14(5):416–20. https://doi.org/10.1007/s11906-012-0293-4.
Kwakernaak AJ, Krikken JA, Binnenmars SH, Visser FW, Hemmelder MH, Woittiez AJ, et al. Effects of sodium restriction and hydrochlorothiazide on RAAS blockade efficacy in diabetic nephropathy: a randomised clinical trial. Lancet Diabetes Endocrinol. 2014;2(5):385–95. https://doi.org/10.1016/S2213-8587(14)70030-0.
Hoshino T, Ookawara S, Miyazawa H, Ito K, Ueda Y, Kaku Y, et al. Renoprotective effects of thiazides combined with loop diuretics in patients with type 2 diabetic kidney disease. Clin Exp Nephrol. 2015;19(2):247–53. https://doi.org/10.1007/s10157-014-0981-2.
Donnelly R, Molyneaux LM, Willey KA, Yue DK. Comparative effects of indapamide and captopril on blood pressure and albumin excretion rate in diabetic microalbuminuria. Am J Cardiol. 1996;77(6):26B–30B. https://doi.org/10.1016/S0002-9149(97)89237-5.
Marre M, Puig JG, Kokot F, Fernandez M, Jermendy G, Opie L, et al. Equivalence of indapamide SR and enalapril on microalbuminuria reduction in hypertensive patients with type 2 diabetes: the NESTOR Study. J Hypertens. 2004;22(8):1613–22. https://doi.org/10.1097/01.hjh.0000133733.32125.09.
Mogensen CE, Viberti G, Halimi S, Ritz E, Ruilope L, Jermendy G, et al. Effect of low-dose perindopril/indapamide on albuminuria in diabetes preterax in albuminuria regression: PREMIER. Hypertension. 2003;41(5):1063–71. https://doi.org/10.1161/01.hyp.0000064943.51878.58.
Heerspink HJ, Ninomiya T, Perkovic V, Woodward M, Zoungas S, Cass A, et al. Effects of a fixed combination of perindopril and indapamide in patients with type 2 diabetes and chronic kidney disease. Eur Heart J. 2010;31(23):2888–96. https://doi.org/10.1093/eurheartj/ehq139.
Scheen AJ. Pharmacodynamics, efficacy and safety of sodium-glucose co-transporter type 2 (SGLT2) inhibitors for the treatment of type 2 diabetes mellitus. Drugs. 2015;75(1):33–59. https://doi.org/10.1007/s40265-014-0337-y.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28. https://doi.org/10.1056/NEJMoa1504720.
McMurray J. EMPA-REG—the “diuretic hypothesis”. J Diabetes Complicat. 2016;30(1):3–4. https://doi.org/10.1016/j.jdiacomp.2015.10.012.
Scheen AJ. Reappraisal of the diuretic effect of empagliflozin in EMPA-REG OUTCOME: comparison with classic diuretics. Diabetes Metab. 2016;42(4):224–33. https://doi.org/10.1016/j.diabet.2016.05.006.
Scheen AJ, Delanaye P. Effects of reducing blood pressure on renal outcomes in patients with type 2 diabetes: focus on SGLT2 inhibitors and EMPA-REG OUTCOME. Diabetes Metab. 2017;43(2):99–109. https://doi.org/10.1016/j.diabet.2016.12.010.
Devineni D, Vaccaro N, Polidori D, Rusch S, Wajs E. Effects of hydrochlorothiazide on the pharmacokinetics, pharmacodynamics, and tolerability of canagliflozin, a sodium glucose co-transporter 2 inhibitor, in healthy participants. Clin Ther. 2014;36(5):698–710. https://doi.org/10.1016/j.clinthera.2014.02.022.
Lambers Heerspink HJ, de Zeeuw D, Wie L, Leslie B, List J. Dapagliflozin a glucose-regulating drug with diuretic properties in subjects with type 2 diabetes. Diabetes Obesity Metab. 2013;15(9):853–62. https://doi.org/10.1111/dom.12127.
Amin NB, Wang X, Mitchell JR, Lee DS, Nucci G, Rusnak JM. Blood pressure-lowering effect of the sodium glucose co-transporter-2 inhibitor ertugliflozin, assessed via ambulatory blood pressure monitoring in patients with type 2 diabetes and hypertension. Diabetes Obesity Metab. 2015;17(8):805–8. https://doi.org/10.1111/dom.12486.
Heise T, Mattheus M, Woerle HJ, Broedl UC, Macha S. Assessing pharmacokinetic interactions between the sodium glucose cotransporter 2 inhibitor empagliflozin and hydrochlorothiazide or torasemide in patients with type 2 diabetes mellitus: a randomized, open-label, crossover study. Clin Ther. 2015;37(4):793–803. https://doi.org/10.1016/j.clinthera.2014.12.018.
Heise T, Jordan J, Wanner C, Heer M, Macha S, Mattheus M, et al. Acute pharmacodynamic effects of empagliflozin with and without diuretic agents in patients with type 2 diabetes mellitus. Clin Ther. 2016;38(10):2248–64 e5. https://doi.org/10.1016/j.clinthera.2016.08.008.
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57. https://doi.org/10.1056/NEJMoa1611925.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
No sources of funding were used to assist in the preparation of this manuscript. No conflicts of interest are directly relevant to the content of this manuscript.
A.J. Scheen has received lecturer/scientific advisor/clinical investigator fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Merck Sharp & Dohme, NovoNordisk, Sanofi, and Servier.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical Collection on Other Forms of Diabetes and Its Complications
Rights and permissions
About this article
Cite this article
Scheen, A.J. Type 2 Diabetes and Thiazide Diuretics. Curr Diab Rep 18, 6 (2018). https://doi.org/10.1007/s11892-018-0976-6
Published:
DOI: https://doi.org/10.1007/s11892-018-0976-6