Abstract
Populations experiencing homelessness with diabetes may encounter barriers to accessing comprehensive diabetes care to manage the condition, yet it is unclear to what extent this population is able to access care. We reviewed the literature to identify and describe the barriers and facilitators to accessing diabetes care and managing diabetes for homeless populations using the Equity of Access to Medical Care Framework. An integrated review of the literature was conducted and yielded 10 articles that met inclusion criteria. Integrated reviews search, summarize, and critique the state of the research evidence. Findings were organized using the dimensions of a comprehensive conceptual framework, the Equity of Access to Medical Care Framework, to identify barriers and facilitators to accessing care and managing diabetes. Barriers included competing priorities, limited access to healthy food, and inadequate healthcare resources. Facilitators to care included integrated delivery systems that provided both social and health-related services, and increased patient knowledge. Recommendations are provided for healthcare providers and public health practitioners to optimize diabetes outcomes for this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over half a million people experienced homelessness on a single night across the USA in January 2015 [1]. Nearly a third of these individuals were in unsheltered locations, i.e., cars, abandoned buildings, or under bridges. Over a third of people experiencing homelessness were a part of a family with children under 18 years of age, and over 50 % were racial/ethnic minorities, including African Americans, Native Americans, and Hispanics. Males make up more than half of the homeless population, and almost 70 % of the population is over the age of 24. Since 2007, the number of homeless persons has declined by 13 %, including the number of homeless children (6 % decline).
Diabetes is a complex chronic condition that requires access to integrated and comprehensive health care, which may be challenging for populations experiencing homelessness. The homeless have higher unmet healthcare needs compared to housed persons and are also more likely to be uninsured [2]. Health care is often received at publicly funded healthcare centers or when admitted through an emergency department [2]. The prevalence of diabetes in the homeless population mirrors the general population with estimates ranging from 6.8 to 9.2 % in a recent review [2]. This estimate may be even higher if those experiencing homelessness are unaware of their diabetes status. In the general population, diabetes also disproportionately impacts minority groups such as African Americans and Hispanics [3, 4]. The racial/ethnic diagnosis of diabetes among people experiencing homelessness is not known; however, minority groups make up over half of the population. This raises concerns as to whether homelessness exacerbates these disparities. Furthermore, the prevalence of risk factors for type 2 diabetes in the homeless population, such as obesity and hypertension, also mirrors the general population [5•, 6], increasing the risk of developing the condition.
Homeless populations often encounter barriers to accessing healthcare services [7•]. Barriers include competing priorities (e.g., trouble finding food, shelter, clothing, and a place to wash and use the bathroom), lack of health insurance, and limited social support. Mental illness, such as mood and substance-related disorders, is also a major concern among homeless populations and results in higher than average hospitalization rates compared to the non-homeless [8]. It is unclear to what extent homeless persons with diabetes encounter barriers to diabetes care; however, research suggests that indigent populations including homeless patients face barriers to diabetes medication adherence, resulting in less than optimal health outcomes [9].
In addition to worse health outcomes, the inability to manage diabetes properly is associated with higher healthcare costs. In an examination of diabetes-related hospitalizations, a study found that 10.5 % were for uncontrolled diabetes [10]. Costs were significantly higher for admissions with uncontrolled diabetes as compared to those without ($11,505 vs. $5545, respectively). Notably, the reduction in diabetes-related prescription drug costs (probable cause—increased availability of generic drugs) has [11] reduced potential financial barriers to diabetes management. However, if healthcare access, and subsequently medication access, is not available to populations experiencing homelessness, this could result in preventable hospitalizations for uncontrolled diabetes and increased healthcare costs.
The Equity of Access to Medical Care Framework assesses how inequities in healthcare access arise [12]. The framework consists of five interdependent components that can enhance or impede healthcare access: (1) health policy; (2) characteristics of healthcare delivery systems (e.g., organization of care); (3) characteristics of vulnerable populations, including predisposing (e.g., demographic characteristics), enabling (e.g., financial/non-financial resources), and need-related factors (e.g., severity of disease, comorbid conditions); (4) utilization of health services; and (5) consumer/patient satisfaction with the care received. Identifying at what level vulnerable populations such as the homeless encounter barriers and facilitators to care can help develop and test appropriate interventions to improve access to care. Optimizing access to diabetes care for the homeless is especially important to promote health equity and improve health outcomes for this population. This framework is useful in that it illustrates specific factors that could be barriers or facilitators for homeless populations with diabetes.
To what extent homeless populations are able to access diabetes care and manage its associated symptoms is unclear. We reviewed the literature to identify and describe the barriers and facilitators to accessing diabetes care and managing diabetes for homeless populations using the Equity of Access to Medical Care Framework.
Methods
An integrative review of the literature was conducted to identify barriers and facilitators using the Equity of Access to Medical Care Framework. Integrative reviews are that seek to systematically search for, summarize, and critique the state of the research evidence [13]. Electronic searches of PubMed and the EBSCOHost platform databases were searched using variations of the following terms: diabetes, homeless, and access to care. Inclusion criteria were as follows: published on or after January 1, 1980, to April 30, 2016; published in the English language; research conducted in North America; and research related to access and self-management of diabetes for homeless populations with diabetes. All studies (randomized controlled trials, observational studies, prospective and retrospective cohort studies, case-control studies, and cross-sectional studies) were considered. Studies were excluded if the study population was war-displaced persons or refugees or if the research was a commentary or case report.
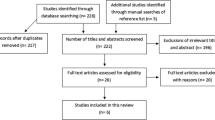
Two reviewers (BW, AL) assessed titles and abstracts to determine if full-text review was warranted; one reviewer (BW) reviewed full-text articles to determine final eligibility. Preliminary searches of title and abstract resulted in 99 document results, of which 31 were extracted for a full article review. A full article review was conducted to determine final eligibility based on the inclusion and exclusion criteria. Ten articles were identified for the final review based on these criteria. Figure 1 outlines the process used to identify articles. Findings were organized using the dimensions of the framework and summarized using Table 1.
Results
Health Policy
No articles were identified that examined health policy factors.
Healthcare Delivery Systems: Organization of Systems
Two articles identified system-level organization factors that could increase access to diabetes care and enhance diabetes self-management for homeless populations. Both used hemoglobin A1c (HbA1c) levels as a primary outcome measure.
Davachi and Ferrari examined the impact of a community-based diabetes management program for homeless persons and those in transitional housing in Canada [14]. The program focused on improving the quality of diabetes care by engaging key stakeholders (e.g., staff at homeless shelters, healthcare providers, and homeless persons). A version of the Chronic Care Model (CCM) for diabetes care was modified for homeless populations by addressing key determinants of health that were barriers to managing diabetes effectively. All activities occurred at a homeless shelter to increase access for those with diabetes and those with prediabetes as well as to disseminate diabetes prevention strategies to others (i.e., diabetes prevention classes and exercise programs, which were independent of the program). Only those who were diagnosed with diabetes were referred to the program. Program activities included demonstrations from project staff on healthier lifestyle choices (e.g., smaller portion sizes); one-on-one consultations with a nurse or dietitian; education related to blood glucose monitoring, medications, foot care, and oral hygiene; and interactive group sessions that emphasized patient empowerment and personal goal setting. Participants received donated pedometers to increase their physical activity. In addition, kitchen staff at the shelter provided those that used insulin with a bedtime snack.
In this study, 44 individuals consented to participate in the program; however, baseline and follow-up data were only available for 10 participants [14]. Of those 10 participants, at follow-up (3–12 months post-referral), there were significant improvements in fasting blood glucose (−4.0 mmol/L; p < 0.05) and mean HbA1c levels (−1.1 %; p < 0.05). In addition, participants were empowered to engage in the management of their diabetes. This involved the creation of a community garden, purchasing fruit trays, and a request for vending machines with healthier food options.
In the second study, O’Toole and others used a retrospective cohort study and modified components of the CCM to meet the needs of the homeless population [15]. Researchers investigated the effect of a primary care clinic tailored to the needs of homeless individuals on chronic disease outcomes and inappropriate emergency department (ED) use (i.e., visit for a non-emergency). Tailored components included the following: providing walk-in clinic hours; assigning patients with a primary care provider and nurse case manager who contacted patients for follow-up appointments and reminders; assessing patients during first visit and every quarter; integrating electronic medical records with built-in reminders to upcoming visits; offering on-site benefits assistance and employee referral services; building partnerships with local homeless shelters; and delivering patient education that promoted self-management.
Investigators compared 12-month chronic disease management outcomes (for diabetes, hypertension, and hyperlipidemia) and ED use between homeless patients attending a culturally tailored primary care clinic (intervention group; n = 79) and homeless patients visiting general internal medicine clinics at a Veterans Affairs medical center (control group; n = 98). The target HbA1c goal for diabetes patients were levels below 7.0 %. Clinical information was abstracted from electronic medical records.
Seven homeless patients in the intervention group had diabetes, and 13 had diabetes in the control group [15]. After the 12-month study period, HbA1c levels in the intervention group improved, on average, by −2.3 % (standard deviation [SD] ± 3.60) and increased by 0.2 % (SD ± 1.2) in the control group (p = 0.03). Patients in the intervention group also had fewer non-emergency ED visits than the control group at 12 months (18.5 and 38.6 %, respectively [p < 0.01]). While not statistically significant, there were more patients with diabetes who met the target goal in the intervention group compared to the control group (57.1 and 53.8 %, respectively [p = 0.76]).
Characteristics of Vulnerable Populations
Several articles addressed identified enabling and need-related factors that were barriers and/or facilitators to diabetes care and management for people experiencing homelessness.
Barriers and Enabling Factors
Factors that negatively influenced the ability of homeless persons to optimize diabetes outcomes were related to housing instability, competing priorities, and limited healthcare resources and food options. Enabling factors included the length of one’s diabetes diagnosis and increased patient knowledge of diabetes self-management.
Lautenschlager and Smith conducted a qualitative study to understand the perceptions concerning diabetes and its management among low-income and homeless American Indians with diabetes in an urban area [16]. They conducted eight focus groups with 40 low-income and homeless American Indian adults (ages 18–70 years) in Minnesota.
Among those who were homeless, there were several barriers to managing their diabetes [16]. This included limited access to glucometers, about which a participant stated: “I had lost all my stuff in storage because I was homeless for like maybe two years, so I lost a lot of stuff [including my monitor]…”. Regarding the importance of stable housing, a participant stated: “I think it’s important to have a home and be able to go to a doctor and I guess that’s, that’s always been my problem, just finding a place to stay, having a phone if they need to call you.” Other homeless participants identified the lack of health insurance and the inability to see a healthcare provider on a regular basis as barriers to effectively managing their diabetes. Participants staying at overnight shelters identified the inability to refrigerate insulin, the lack of control of the type of food that was available, and the inability to refrigerate perishable food as challenges.
Elder and Tubb conducted 45-min, semi-structured key informant interviews to examine barriers and facilitators to health for homeless patients with diabetes [17••]. Interviews were with social service providers (n = 6) and healthcare providers (n = 5) that served the homeless, as well as homeless patients with diabetes (n = 7). They used a convenience sample, and participants were compensated for their time with a gift card to a grocery store.
The mean age of homeless participants was 52 years, and 14 years was the mean length of time since being diagnosed with diabetes (SDs not reported) [17••]. The mean length of time for involvement with homeless clients/patients for social service providers and healthcare providers was 7 years. Enabling factors that served as barriers in the management of diabetes for the homeless included limited food choices, competing priorities, limited access to medication and healthcare services, and limited financial resources. When discussing limited food choices, one homeless participated stated that “meal choices are carb heavy, with lots of spaghetti and donuts.” Access to affordable healthy foods was also a barrier: “fruits and veggies are expensive and hard to find.” Finding food that did not spoil and were easy to carry also limited food options to items such as “chips.” Competing priorities were also barriers to optimizing health outcomes for homeless patients with diabetes. Participants stated that the transient lifestyle of people experiencing homelessness often lead to misplaced or lost items, including diabetes medications. Limited access to affordable medication and health services were also challenges. Storing medications at homeless shelter was also a concern: “[I] can only get my meds during a set time—if I miss it, I can’t get my meds.” The need to refrigerate diabetes medications was also a concern. When discussing limited financial resources, unemployment was raised as a challenge: “It’s hard to keep a job when your feet hurt all the time.”
Enabling factors identified as facilitators included access to free health care through the Health Care for the Homeless (HCH) programs and increased physical activity because of lack of transportation [17••]. Participants stated that although medicine through the HCH programs was free, selections were limited in scope and the pharmacy hours were not flexible.
Rojas-Guyler et al. administered a validated survey to 27 participants who were veterans and residing in a homeless shelter that only served homeless veterans [18]. The survey examined diabetes self-management, knowledge, and barriers related to diabetes care. Participants were recruited at the shelter for homeless veterans and signed an informed consent form. The survey consisted of 38 items and covered demographic information, diabetes self-management (seven Likert scale questions), diabetes knowledge (modified from the Diabetes Knowledge Test), attitudes related to diabetes (modified from the Diabetes Attitude Scale), and barriers to diabetes management (two open-ended questions). Survey questions were reviewed by an expert panel, which included a previously homeless person with diabetes. Software was used to ensure survey questions were at a fourth-grade reading level.
The mean age of participants was 53.7 (SD ± 4.7), and participants represented all branches of the US military [18]. The mean length of diagnosis was 8.2 years (SD not reported). Survey findings for self-management behavior for foot care were as follows: 66.7 % checked their feet daily; 70.3 % found it very easy/easy to check their feet; and 74.0 % felt it was very important/important to check their feet. Survey findings for self-management behavior for blood glucose monitoring were as follows: 63.0 % checked their blood sugar daily; 88.8 % found it very easy/easy to check their blood sugar; and 88.8 % felt it was very important/important to check their blood sugar. Survey findings for self-management behavior for eye care were as follows: 66.7 % had their eyes checked by a healthcare provider once a year; 85.2 % found it very easy/easy to access a provider to have their eyes checked; and 96.3 % felt it was very important/important to have their eyes checked by a provider. When self-management scores were aggregated, 74.1 % ranked high in diabetes self-management. Scores for the diabetes knowledge survey items were also high, with 74.1 % of participants having high knowledge levels. In a linear regression model, how long a participant had been diagnosed with diabetes was associated with high diabetes knowledge scores (b = 20.94, α = <0.037, R 2 = 0.220) and high self-management levels (b = −10.722, α = <0.037, R 2 = 0.220).
In the open-ended questions, participants felt that the shelter that was specifically designed for homeless veterans helped to improve the management of their diabetes: “This is home for me. The guys care about me and help me with my diabetes by telling me ‘hey—you takin’ your medicine?’ or ‘when’s the last time doc check you?’” [18]. Another participate wrote: “You go to these other shelters and you don’t feel good. You worry ‘bout if someone gonna take your meter [glucometer] when you’re sleeping ‘cause they been eyein’ you and it. You don’t rest at night.” In these responses, participants also noted the limited access to healthy foods to manage their diabetes as a barrier: “I don’t wanna complain ‘bout food ‘cause you eat what you can, but the food can’t be good for a diabetic. My doctor says to eat one way and I can’t because of shelter food.”
Hwang and Bugeja examined barriers to diabetes care among people experiencing homelessness at shelters for single adults across Toronto, Canada [19]. Shelter staff identified residents with diabetes and investigators posted recruitment flyers. Participants completed a face-to-face 20-min interview that consisted of questions related to demographic information, diabetes history, chronic disease history, mental health, drug use, healthcare access, and hospital use (n = 50). Questions were close- and open-ended; interviewers transcribed responses to open-ended questions verbatim. Qualitative responses were analyzed using a qualitative management program. Participants who provided a blood sample to obtain HbA1c levels were compensated with $5. An outcome measure was glycemic control using HbA1c levels; inadequate control was defined by the Canadian Diabetes Association as >140% of the upper limit of normal. Investigators received permission from administrators at the homeless shelters to conduct the study.
The median age of the 50 participants was 49 years; 76 % were between 40 and 59 years of age [19]. Type 2 diabetes was the most common type of diabetes (86 %), and 44 % had been diagnosed with diabetes for over 5 years. Of the 48 participants in whom researchers obtained HbA1c levels, 44 % had inadequate glycemic control. Over half currently took oral agents to manage their diabetes (62 %); 28 % used insulin; 2 % used both insulin and oral agents; and 8 % did not currently use any medication. Among those who took medication, 16 % found it difficult to store medications in a safe location. Regarding self-management, 42 % of participants were in possession of a glucometer at the time of the interview; however, only 34 % currently used it and only 24 % used it at least daily.
Participants identified several barriers to managing their diabetes in the qualitative responses related to access to healthy foods, ability to adhere to their medication regimen, and challenges related to being homeless [19]. More than half of the participants identified diet as a challenge to their diabetes care (64 %). One participant stated: “The food in the shelter has a lot of fat and is high in carbohydrate. I can’t control my diet here anyway, so I don’t bother measuring my blood sugar.” There was also an expressed lack of control: “I have no choice [in my diet] at the shelter, so I skip a large proportion of each meal.” Having to follow schedules set by shelter staff that made it challenging to take medication as prescribed was also a concern among participants (18 %). One participant commented: “I can’t schedule anything. I must revolve around the shelter schedule, so nothing is consistent.” Another participant stated: “I can’t time my insulin with my food; I’m supposed to take insulin half an hour before my meals and usually I can only get it 10 minutes before.” Some participants felt the daily stresses of being homeless exacerbated their diabetes (8 %). Theft of needles and syringes at the shelter by injection drug users was also a concern (6 %): “I hope that no one takes my insulin or my needles. I’m dealing with junkies and crackheads and they want the needles.” Additional barriers to diabetes care that participants identified included the lack of a medication benefit card (52 %) and health insurance coverage (24 %).
Need-Related Factors
Having comorbid complex health conditions was found to be a barrier and facilitator to diabetes care and management in two independent studies. Older age was also associated with having diabetes and comorbid complex conditions.
Participants in the study conducted by Elder and Tubb identified having a mental illness diagnosis and/or substance abuse was a facilitator to optimizing health outcomes for homeless persons with diabetes because it increased the availability of financial resources (e.g., social security insurance or Medicare) and additional social service support and healthcare referrals [17••]. In the study identifying barriers to diabetes care, Hwang and Bugeja found that research participants with a history of crack/cocaine use had worse glycemic control (as measured by HbA1c) than those who did not (73 and 35 %, respectively; p = 0.06) [19].
Having diabetes was associated with having additional chronic conditions in the homeless population [20]. Researchers identified factors associated with having one or more geriatric syndromes in a cohort of 250 homeless adults in Boston, MA. Participants were recruited from eight shelters and met the following inclusion criteria: 50 years or older; proficient in English; currently homeless; and provided written informed consent. Participants received a $5 gift card to a pharmacy to compensate them for their time. The burden of geriatric syndromes was based on the following: having fallen in the past year; having a cognitive and/or sensory impairment; frailty; major depression; and urinary incontinence. These syndromes were assessed using validated surveys. Ordinal logistic multivariable models estimated the association of patient characteristics (independent variables such as age, sex, diabetes, arthritis, drug use, etc.) with the total number of geriatric syndromes (ordinal score).
The mean age of participants was 56.2 (SD ± 5.3), and 16.0 % had diabetes [20]. In the logistic regression analysis, diabetes was significantly associated with having a higher number of geriatric syndromes (odds ratio [OR] 2.49; 95 % confidence interval [CI] 1.36, 4.57). The observed relationship between diabetes and number of geriatric syndromes remained significant in the model after adjusting for covariates (OR 2.28; 95 % CI 1.22, 4.26).
Asgary et al. examined factors associated with uncontrolled hypertension among homeless adults who received care at 10 different shelter-based clinics in New York City [21••]. They retrospectively reviewed medical charts of 210 patients, 177 of whom were homeless. The mean age of homeless patients was 55.1 (SD ± 11.1), and 35.1 % had a personal history of diabetes. Diabetes was significantly higher among homeless patients with controlled hypertension compared to those with uncontrolled hypertension (42.5 and 21.1 %, respectively [p < .01]) (uncontrolled hypertension defined as blood pressure levels of as 140/90 to 160/100 mmHg; or 160/100 mmHg or higher). In the unadjusted and adjusted logistic regression model, having diabetes was independently associated with better blood pressure control (unadjusted OR 0.35; 95 % CI 0.17, 0.70) (adjusted OR 0.38; 95 % CI 0.18, 0.81) (the model adjusted for age, health insurance status, mental illness, alcohol abuse, obesity, and hypercholesterolemia).
Utilization of Services
Several articles examined outcome measures related to the management of diabetes, including the use of a screening clinic to facilitate access to follow-up care for homeless patients and the use of an insulin pen for the homeless.
Macnee et al. conducted a process evaluation of a screening clinic for homeless patients to determine utilization [22]. Screening clinics were available for five specific health conditions/problems: hypertension, diabetes, anemia, tuberculosis, and foot problems. Evaluation of the service occurred over 9 months at an umbrella primary care clinic for the homeless that was open 3 days out of the week. Screening clinics were managed by nursing faculty and students. Staff administered a survey to obtain demographic information and a brief medical history. Hemoglobin A1c and capillary blood glucose readings were obtained from patients who attended the diabetes screening clinic.
During the study period, 219 patients attended one of the five screening clinics. The hypertension clinic had the highest attendance (n = 131), followed by the diabetes clinic (n = 58) [22]. Of those who attended the diabetes clinic, about half were ≤50 years of age and male (52 %). Twenty-nine percent of these patients had not previously utilized services at the clinic, and almost all (88 %) received follow-up care.
Wilk et al. assessed the effectiveness of an insulin pen delivery device in the management of diabetes among homeless persons visiting an HCH-funded clinic [23]. Patients diagnosed with diabetes mellitus were identified at the clinic and invited to participate in the 6-month study. Informed consent was obtained from 23 patients at the clinic. The baseline visit consisted of a survey to obtain demographic information and to understand challenges to the traditional syringe and needle to administer insulin (based on a list of challenges with the option to add challenges). Participants received an insulin pen and glucometer (note: Data from glucometers were not reported because of equipment malfunctions and/or failure of participants to bring them to follow-up visits throughout the study.). Hemoglobin A1c measurements were obtained at baseline, month 3, and month 6. Maintenance visits occurred every 2 weeks. At these visits, participants received new supplies and disposed of used needles/ cartridges. At month 6, participants completed a survey to understand the ease of using the pen in comparison to the traditional syringe and needle (based on a list of advantages with the option to add advantages). Participants utilized their usual source of care at the HCH clinic and participated in diabetes education classes.
The mean age of the 23 participants was 50 years (SD not reported) [23]. Most (91 %) had duration of diabetes between 2 and 16 years; one participant received a more recent diagnosis. At baseline, more than half of participants indicated that the traditional syringe and needle was difficult to use because of the following reasons: shots could not be administered with a meal; trouble maintaining a schedule because of movement in/out of shelters; and lack of privacy (n = 22). At month 6, most participants found the insulin pen easier to use based on the following reasons: ease of use; improved compliance to recommendations from healthcare provider; and increased accuracy of insulin doses. In addition, insulin for the pen device did not need to be refrigerated, an advantage for many participants. However, one participant noted that it was difficult to read the dosage on the pen’s dial. At baseline, the mean A1c was 10.4 % (SD ± 3.0 %) compared to 8.9 % (SD ± 1.9 %) at month 6 (p = 0.087).
In the study conducted by Hwang and Bugeja to identify barriers to diabetes care among homeless persons, most participants saw a healthcare provider on a regular basis for their diabetes (80 %; n = 40) and had seen a provider in the last 2 months (76 %; n = 76). Fewer received education related to diet for diabetes (36 %; n = 72) [19].
Consumer Satisfaction
No articles were found that examined patient satisfaction factors.
Discussion
This review summarizes the literature focused on barriers and facilitators to diabetes care for populations experiencing homelessness using the Equity of Access to Medical Care Framework. At the healthcare systems level, community-based and socially/culturally tailored care improved diabetes outcomes for homeless patients. Factors at the population level that were barriers to diabetes care and its management included competing priorities, limited food options, and limited access to healthcare resources. Population-level factors that improved diabetes outcomes were patient knowledge and the length of a diabetes diagnosis. Need-related factors for homeless populations that were associated with poor diabetes outcomes included having a history of substance abuse. In contrast, having a current mental illness or substance abuse diagnosis was associated with more optimal diabetes outcomes. While this study had a small sample size, this may be because care has already been facilitated for these patients who are already receiving care to control mental illness or substance abuse symptoms. Likewise, having diabetes was associated with better blood pressure control. The use of community-based screening clinics for diabetes and the use of an insulin pen were associated with increased healthcare utilization and diabetes management for homeless populations. Findings indicate that there is a paucity of research examining the influence of health policy and the perceptions of homeless patients regarding how this population accesses diabetes care and manages the condition.
This review identified conflicting findings related to need-related factors for the homeless. Elder and Tubb found that having a mental illness diagnosis and/or substance abuse facilitated access to diabetes care by increasing the availability of health-related and social services [17••], yet one study found that patients with a history of crack/cocaine use had worse glycemic control [19]. A previous study found that having a comorbid condition was both a facilitator and barrier to primary care for the homeless [7•, 24]. Since a previous history of drug use was associated with worse diabetes outcomes and those with a current diagnosis of mental illness or substance abuse had more favorable diabetes outcomes, this could indicate that homeless persons with current diagnoses for what providers may perceive as more complex conditions that requires immediate care are accessing care and diabetes is being treated as a secondary and periphery condition. That is, homeless persons with mental illness or substance abuse may have access to additional financial and non-financial resources than those without these conditions.
An integrative and comprehensive approach is needed to improve and optimize diabetes outcomes for people experiencing homelessness. This includes delivering tailored and socially appropriate care and building partnerships with key stakeholders such as healthcare providers, social workers, homeless shelter staff, and those experiencing homelessness. Clearly, this at-risk and underserved population are aware and concerned about access and ability to receive necessary care to manage their diabetes. Table 2 provides recommendations at multiple levels for those providing care for homeless persons with diabetes.
Deliver Tailored, Culturally Appropriate Care
Delivering health care that caters to the needs of homeless populations (e.g., flexible hours, shelter-based care) is one strategy to improve diabetes outcomes. There are several financial and non-financial barriers to care that the homeless face in accessing services, including lack of health insurance coverage and competing priorities [7•, 14]. Tailoring care can support efforts to overcome these barriers and meet the needs of the homeless. Diabetes is a complex condition that requires comprehensive and continuous care to ensure its proper management. This review identified several barriers for homeless populations with diabetes; however, adapting services appears to be an effective approach to increase access and improve diabetes management. Developing homeless-specific delivery systems can facilitate access to health services for groups with complex conditions such as diabetes [14, 15, 25, 26]. These systems can reduce ED use [15], increase the use of primary care services [15, 27], and increase patient satisfaction and patient-provider communication [26].
An intervention included in this review demonstrated that a tailored CCM can improve the management of diabetes and subsequently diabetes outcomes for homeless patients [15]. While the number of patients with diabetes was low and the number of patients with diabetes who met the target A1c goal of levels below 7.0 % was not significant, there was a significant improvement in A1c levels in the intervention group that was not seen in the control group.
An intervention that was not included in this review evaluated the effect of the application of patient-centered medical homes specifically tailored for vulnerable veteran populations (i.e., the homeless, women with post-traumatic stress disorder and/or sexual trauma, individuals with serious mental illnesses, and cognitively impaired older adults) on primary care access and chronic disease management [28]. Each clinic addressed four key components for each population: (1) increasing primary care access; (2) tailoring health care; (3) relying on effective case management by a registered nurse or social worker; and (4) promoting the delivery of culturally sensitive care. While this study did not examine diabetes outcomes for homeless patients, it did find that A1c levels improved significantly for patients who visited one of the four tailored clinics.
In addition, the use of insulin pens for the homeless appears to show promise with the homeless by overcoming previous barriers to the management of diabetes with the traditional syringe and needle [23]. Investigators noted that there was still no safe disposal of used needles; however, used needles from insulin pens may be a safer option because it reduces the risk of its use for illegal drug use. Furthermore, the cartridges of insulin did not need to be refrigerated, increasing the likelihood for people experiencing homelessness to manage their diabetes.
Build Partnerships with Stakeholders
Identifying key stakeholders to improve healthcare access and the management of diabetes for homeless populations is critical for sustainable efforts. One study included in the review demonstrated the importance of engaging key stakeholders to optimize health outcomes among those experiencing homelessness, specifically related to the delivery of diabetes care [14]. In many situations, when people are homeless they lack control over key elements of everyday activities, including when/where s/he will eat. By involving shelter staff in the delivery of the diabetes intervention, it provided an opportunity to provide bedtime snacks for those who were insulin-dependent [14].
In addition, participants in another study identified key enabling factors that present challenges to effectively managing diabetes, which included limited availability of appropriate diabetic foods at shelters and the inability to use the refrigerator to store insulin [16]. The diabetes management program discussed by Davachi and Ferrari demonstrates that it is key to engage homeless shelters to improve health outcomes for those with diabetes [14]. This can provide access to healthier food options and provide storage for those who depend on insulin.
Review Limitations
There are limitations to these findings. First, studies conducted in the USA and Canada were included in the review, and these populations may not be comparable, limiting the generalizability of the findings. Second, homeless veterans were the study sample for two studies. Needs of this population may be unique compared to non-veteran populations.
Conclusion
Healthcare access for populations experiencing homelessness must be a priority for policymakers, healthcare providers, and public health practitioners. Diabetes can be a debilitating condition; when uncontrolled, it can lead to more complex sequela conditions requiring a higher level of care at potentially greater costs. However, with proper access and management, these sequela, and their associated healthcare costs, are significantly more likely to be avoided, thereby helping patients live healthier and more productive lives. For homeless populations with diabetes, access and management is essential because of everyday environmental and social challenges. By creating a system that facilitates healthcare access by providing tailored care and building partnerships with key stakeholders, we can optimize health outcomes for homeless populations managing diabetes.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
US Department of Housing and Urban Development: The 2015 Annual Homeless Assessment Report (AHAR) to Congress, November 2015: Part 1 - Point-in-Time Estimates of Homelessness. Available at: https://www.hudexchange.info/resources/documents/2015-AHAR-Part-1.pdf. Accessed 17 Aug 2016.
Lebrun-Harris LA, Baggett TP, Jenkins DM, Sripipatana A, Sharma R, Hayashi AS, et al. Health status and health care experiences among homeless patients in federally supported health centers: findings from the 2009 patient survey. Health Serv Res. 2013;48(3):992–1017. doi:10.1111/1475-6773.12009.
Centers for Disease Control and Prevention: age-adjusted rates of diagnosed diabetes per 100 civilian, non-institutionalized population, by race, United States, 1980–2014. Available at: http://www.cdc.gov/diabetes/statistics/prev/national/figbyrace.htm. Accessed 19 Aug 2016.
Centers for Disease Control and Prevention: age-adjusted rates of diagnosed diabetes per 100 civilian, non-institutionalized population, by Hispanic origin, United States, 1997–2014. Available at: http://www.cdc.gov/diabetes/statistics/prev/national/figbyhispanic.htm. Accessed 19 Aug 2016.
Bernstein RS, Meurer LN, Plumb EJ, Jackson JL. Diabetes and hypertension prevalence in homeless adults in the United States: a systematic review and meta-analysis. Am J Public Health. 2015;105(2):e46–60. doi:10.2105/AJPH.2014.302330. This meta-analysis synthesized articles that provided the prevalence of diabetes and hypertension for homeless adults. A key finding was that there were no significant differences in prevalence rates for diabetes and hypertension between homeless populations and the general population.
Koh KA, Hoy JS, O’Connell JJ, Montgomery P. The hunger-obesity paradox: obesity in the homeless. J Urban Health. 2012;89(6):952–64. doi:10.1007/s11524-012-9708-4.
White BM, Newman SD. Access to primary care services among the homeless: a synthesis of the literature using the equity of access to medical care framework. J Prim Care Community Health. 2015;6(2):77–87. doi:10.1177/2150131914556122. This article was an integrative review identifying barriers and facilitators to primary care access for homeless populations. Competing priorities (e.g., the ability to find food and shelter) were major barriers to care for the homeless.
Karaca Z, Wong HS, Mutter RL. Characteristics of homeless and non-homeless individuals using inpatient and emergency department services, 2008: statistical brief #152. Healthcare Cost and Utilization Project. Rockville: Agency for Healthcare Research and Quality ; 2013.
Schectman JM, Schorling JB, Voss JD. Appointment adherence and disparities in outcomes among patients with diabetes. J Gen Intern Med. 2008;23(10):1685–7. doi:10.1007/s11606-008-0747-1.
Ahern MM, Hendryx M. Avoidable hospitalizations for diabetes: comorbidity risks. Dis Manag. 2007;10(6):347–55. doi:10.1089/dis.2007.106709.
Cunningham P, Carrier E. Trends in the financial burden of medical care for nonelderly adults with diabetes, 2001 to 2009. Am J Manag Care. 2014;20(2):135–42.
Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9(3):208–20.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53.
Davachi S, Ferrari I. Homelessness and diabetes: reducing disparities in diabetes care through innovations and partnerships. Can J Diabetes. 2012;36:8. doi: http://dx.doi.org/10.1016/j.jcjd.2012.04.015
O’Toole TP, Buckel L, Bourgault C, Blumen J, Redihan SG, Jiang L, et al. Applying the chronic care model to homeless veterans: effect of a population approach to primary care on utilization and clinical outcomes. Am J Public Health. 2010;100(12):2493–9. doi:10.2105/AJPH.2009.179416.
Lautenschlager L, Smith C. Low-income American Indians’ perceptions of diabetes. J Nutr Educ Behav. 2006;38(5):307–15.
Elder NC, Tubb MR. Diabetes in homeless persons: barriers and enablers to health as perceived by patients, medical, and social service providers. Soc Work Public Health. 2014;29(3):220–31. doi:10.1080/19371918.2013.776391. This article identifies barriers and facilitators to maintaining health for homeless persons with diabetes by conducting focus groups with patients, healthcare providers, and social service providers. Limited food choices and healthcare resources, as well as competing priorities were identified as barriers to maintaining health.
Rojas-Guyler L, Inniss-Richter ZM, Lee R, Bernard A, King K. Factors predictive of knowledge and self-management behaviors among male military veterans with diabetes residing in a homeless shelter for people recovering from addiction. The Health Educator. 2014;46(1):8.
Hwang SW, Bugeja AL. Barriers to appropriate diabetes management among homeless people in Toronto. CMAJ. 2000;163(2):161–5.
Brown RT, Kiely DK, Bharel M, Mitchell SL. Factors associated with geriatric syndromes in older homeless adults. J Health Care Poor Underserved. 2013;24(2):456–68. doi:10.1353/hpu.2013.0077.
Asgary R, Sckell B, Alcabes A, Naderi R, Schoenthaler A, Ogedegbe G. Rates and predictors of uncontrolled hypertension among hypertensive homeless adults using New York City shelter-based clinics. Ann Fam Med. 2016;14(1):41–6. doi:10.1370/afm.1882. This study found that homeless persons with hypertension and diabetes were more likely to better blood pressure control.
Macnee CL, Hemphill JC, Letran J. Screening clinics for the homeless: evaluating outcomes. J Community Health Nurs. 1996;13(3):167–77.
Wilk T, Mora PF, Chaney S, Shaw K. Use of an insulin pen by homeless patients with diabetes mellitus. J Am Acad Nurse Pract. 2002;14(8):372–9.
Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200–6.
O’Toole TP, Bourgault C, Johnson EE, Redihan SG, Borgia M, Aiello R, et al. New to care: demands on a health system when homeless veterans are enrolled in a medical home model. Am J Public Health. 2013;103 Suppl 2:S374–9. doi:10.2105/AJPH.2013.301632.
Kertesz SG, Holt CL, Steward JL, Jones RN, Roth DL, Stringfellow E, et al. Comparing homeless persons’ care experiences in tailored versus nontailored primary care programs. Am J Public Health. 2013;103 Suppl 2:S331–9. doi:10.2105/AJPH.2013.301481.
McGuire J, Gelberg L, Blue-Howells J, Rosenheck RA. Access to primary care for homeless veterans with serious mental illness or substance abuse: a follow-up evaluation of co-located primary care and homeless social services. Adm Policy Ment Health. 2009;36(4):255–64. doi:10.1007/s10488-009-0210-6.
O’Toole TP, Pirraglia PA, Dosa D, Bourgault C, Redihan S, O’Toole MB, et al. Building care systems to improve access for high-risk and vulnerable veteran populations. J Gen Intern Med. 2011;26 Suppl 2:683–8. doi:10.1007/s11606-011-1818-2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Brandi M. White, Ayaba Logan, and Gayenell S. Magwood declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Health Care Delivery Systems and Implementation in Diabetes
Rights and permissions
About this article
Cite this article
White, B.M., Logan, A. & Magwood, G.S. Access to Diabetes Care for Populations Experiencing Homelessness: an Integrated Review. Curr Diab Rep 16, 112 (2016). https://doi.org/10.1007/s11892-016-0810-y
Published:
DOI: https://doi.org/10.1007/s11892-016-0810-y