Abstract
Growing evidence supports that air pollution has become an important risk factor for developing diabetes mellitus. Understanding the contributing effect of air pollution in population studies, elucidating the potential mechanisms involved, and identifying the most responsible pollutants are all required in order to promulgate successful changes in policy and to help formulate preventive measures in an effort to reduce the risk for diabetes. This review summarizes recent findings from epidemiologic studies and mechanistic insights that provide links between exposure to air pollution and a heightened risk for diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
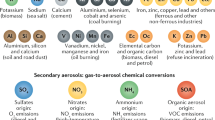
Anthropogenic air pollution, most notably particulate matter (PM) <2.5 μm in aerodynamic diameter (PM2.5), is a leading cause of global morbidity and mortality [1]. The majority of PM2.5 in the modern world derives from fossil fuel combustion (coal, oil, gas, and diesel) from a variety of sources (power generation, traffic, and industry). The evidence accrued over the past few decades indisputably shows that PM2.5 exposure is directly responsible for triggering a host of cardiovascular (CV) events including stroke, myocardial infarctions, and heart failure [2]. The most recent meta-analysis demonstrates that short-term exposure to higher PM2.5 levels increases the risk for myocardial infarction by approximately 2.5 % (per 10 μg/m3, which is roughly equal to 1 standard deviation in most European and North American countries) over the ensuing days [3]. However, mounting evidence supports that longer-term exposure (e.g., few years) has an exponentially greater impact on CV-related morbidity and mortality, increasing the risk by roughly 10–20 % [2, 4]. One explanation for this heightened adverse health effect is that persistent exposures promote the genesis of chronic disease states (e.g., atherosclerosis) incremental to the triggering of acute events [2]. In this regard, there is now substantial evidence that air pollution may potentiate the development of insulin resistance and hypertension [5, 6]. Indeed, a number of epidemiological studies have investigated the association between exposure to ambient air pollution and increased type 2 diabetes mellitus (T2DM) incidence, prevalence, morbidity, and mortality. Additional research has investigated whether people with diabetes are more susceptible to the effects of air pollutants. In support of these epidemiological associations, several controlled human and animal experiments have demonstrated plausible mechanisms linking insulin resistance with exposure to PM2.5. The purpose of this review is to provide an up-to-date summary of the evidence linking air pollution with T2DM.
Air Pollution and Diabetes Prevalence
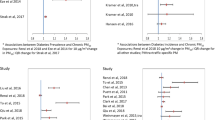
Several studies have reported a positive association between the exposure to ambient air pollution and the prevalence of T2DM (Table 1). Early evidence largely originated from ecologic and cross-sectional investigations [7, 8]. One of the first studies was conducted in Ontario, Canada [7]. Exposure to NO2 (metric of traffic-related pollution) was associated with increased odds of diabetes in women (OR = 1.04; 95 % CI = 1.00–1.08), but not men. The authors could not distinguish between type 1 and 2 diabetes; however, they speculated that the majority of study subjects had T2DM given the median age of the population (approximately 60).
One of the first (and largest) studies conducted in the USA assessed the relationship between PM2.5 and diabetes prevalence at the county level in 2004 and 2005 using data from the National Diabetes Surveillance System at the Centers for Disease Control and Prevention (CDC) [8]. Exposure to PM2.5 was estimated as the annual mean for each county, calculated by combining data from air quality monitors with a statistically fused air model obtained from the Environmental Protection Agency (EPA). In models adjusted for known risk factors, the authors reported a 1 % increase in diabetes prevalence (or 10,000 additional cases in a hypothetical population of 1,000,000 individuals) associated with a 10 μg/m3 increase in PM2.5.
In a more recent cross-sectional analysis of 6392 participants from 29–73 years of age in the Swiss Cohort Study on Air Pollution and Lung and Heart Diseases in Adults, the association between estimates of average PM10 and NO2 exposures over the 10 years preceding the health assessment survey was reported [9•]. Both pollutants were significantly associated with prevalent diabetes per 10 μg/m3 increase in the average home outdoor level (PM10 OR = 1.40, 95 % = CI 1.17–1.67; NO2 OR = 1.19, 95 % CI = 1.03–1.38). The associations with particle pollution were generally stronger than with NO2, even in the two-pollutant model.
Air Pollution and Diabetes Incidence
Prospective cohort studies have provided additional evidence of an association between ambient air pollutants and T2DM (Table 1). Kramer et al. examined the association between incident T2DM and traffic-related air pollution using data from the Study on the Influence of Air Pollution on Lung, Inflammation and Aging (SALIA) cohort in Germany [10]. Using questionnaires, information was collected on 1775 non-diabetic women who were 54–55 years old at baseline (1985–1995) and followed up until 2006. Complement factor C3c was measured at baseline and used as a marker for subclinical inflammation. Individual exposures to PM and NO2 were estimated using data from the State Environment Agency emissions inventory and air monitoring stations. Hazard ratios for incident T2DM increased by 15 % (95 % CI = 4–27) per interquartile range increase in traffic-related PM or by 15 % (95 % CI = 4–27) to 42 % (95 % CI = 16–73) per interquartile range increase in NO2. Women with high levels of C3c were more susceptible for PM-related excess risk of diabetes than women with low C3c levels.
Another study followed 51,818 participants of the Danish Diet, Cancer, and Health cohort in the Danish National Diabetes Register, which does not distinguish between T1DM and T2DM, from baseline to June 2006 [11]. NO2 levels were estimated at residential addresses of participants using the Danish AirGIS human exposure modeling system. After a mean follow-up of 9.7 years, the authors reported a borderline significant association between NO2 and confirmed cases of incident diabetes (HR = 1.04, 95 % CI = 1.00–1.08). Among confirmed diabetics, effects were enhanced in non-smokers (HR = 1.12, 95 % CI = 1.05–1.20) and physically active participants (HR = 1.10, 95 % CI = 1.03–1.16), suggesting that reductions in ambient air pollution exposures may particularly benefit individuals living healthier lifestyles. Results also indicated that women are at greater risk of diabetes associated with air pollution (HR = 1.07, 95 % CI = 1.01–1.13) compared to men (HR = 1.01, 95 % CI = 0.97–1.07).
In one of the few studies which investigated the association between incident T2DM and ambient air pollution exposure among African Americans, Coogan et al. followed a cohort of black women (the Black Women’s Health Study; n = 59,000) living in Los Angeles from 1995 to 2005 [12]. After 10 years of follow-up for the analytic T2DM sub-cohort (n = 3992), exposure to PM2.5 and NO2 was estimated at participants’ addresses using interpolation from monitoring station measurements and land use regression models. For a 10 μg/m3 increase in each pollutant, the incidence rate ratio (IRR) for T2DM was 1.63 (95 % CI = 0.78–3.44) for PM2.5 and 1.25 (95 % CI = 1.07–1.46) for NO2. These results suggest that exposure to air pollutants, particularly traffic-related air pollutants, increases the risk of T2DM.
Negative Epidemiological Studies
Given multiple limitations and potential methodological issues associated with performing epidemiologic studies linking air pollution with health effects (e.g., exposure misclassification, misdiagnoses of T2DM, under-powered sample sizes, residual confounding by covariates), it is not entirely unexpected that several studies would fail to find associations. Moreover, there may be variability in the risks due to a host of factors (e.g., biological susceptibility and pollution source/compositions) that lead to a true lack of a relationship in some circumstances. For example, Dikjema et al. examined the association between long-term exposure to traffic-related air pollution and T2DM prevalence in residents of a semi-rural area of the Netherlands aged 50–75 years (n = 8018) [13]. Exposure was characterized at the individual level based on each participant’s home address and included the following indicators: NO2 concentration from land use regression models, distance to the nearest main road, traffic flow at the nearest main road, and traffic in a 250 m circular buffer. For traffic within a 250 m buffer, prevalence of T2DM was non-significantly increased in the highest three quartiles of exposure compared to the lowest quartile (e.g., Q1 vs. Q2 adjusted OR = 1.25, 95 % CI = 0.99–1.59). The other metrics were not associated with diabetes.
The pooled analyses of the Nurses’ Health Study and the Health Professionals’ Follow-up Study also did not observe an association between T2DM incidence and exposure to PM [14]. Adjusted HRs for incident diabetes associated with an IQR increase of pollutants were 1.03 (95 % CI = 0.96–1.10) for PM2.5, 1.04 (95 % CI = 0.99–1.09) for PM10, and 1.04 (95 % CI = 0.99–1.09) for PM10–2.5. However, an increased association with distance to road, a proxy marker of exposure to traffic-related exposure, was reported among women; the adjusted HR for living <50 m versus ≥200 m from a roadway was 1.14 (95 % CI = 1.03–1.27) [14].
It is worth noting that differences between studies that found an association and those that did not may also relate to intrinsic dissimilarities in study methodology, particularly related to outcome assessment, exposure assessment, concomitant risk factors in the study population, and the overall prevalence of diabetes. Differences between men and women reported in some studies may relate to true differences in biologic susceptibility [1], but may also reflect other factors such as exposure assessment error typically larger in men who are more mobile day-to-day.
Air Pollution and Obesity
There have been two longitudinal cohort studies suggesting environmental pollutants contribute to the development of childhood obesity. In 3318 participants in Southern California, McConnell et al. analyzed the effect of secondhand smoke and near-roadway pollution exposure on obesity in children aged from 10 to 18 years. There was a 0.80 kg/m2 increase in attained BMI at age 18 years (95 % CI = 0.27–1.32) in children with high near-roadway pollution exposure and a 0.85 kg/m2 increase in BMI (95 % CI = 0.43–1.28) in children with a history of secondhand smoke exposure. BMI was 2.15 kg/m2 higher (95 % CI = 1.52, 2.77) among children with both high near-roadway pollution exposure and a history of secondhand smoke, suggesting combined exposures may have synergistic effects [15]. Another study in Southern California observed a positive association between traffic pollution and weight gain, with a 13.6 % increase in annual BMI growth when comparing the lowest to the highest tenth percentile of air pollution exposure [16]. It has also been reported that serum levels of leptin, a pro-inflammatory cytokine primarily produced by adipocytes, were positively associated with annual mean residential black carbon exposure, with a 12 % (95 % CI = 3 to 22 %) increase per interquartile increase (0.11 μg/m3) [17]. Consistent with these observations in humans, animal studies also indicate a role for PM2.5 in promoting obesity in both young [18] and adult [19] mice. An increase in visceral adiposity as evidenced by MRI imaging of fat mass, fat pad weight, and adipocyte size was found in mice exposed to concentrated ambient air [19]. Similar findings were obtained in young mice exposed to PM2.5 [18]. Together, these findings support the contention that chronic exposure to air pollution may predispose to weight gain.
Air Pollution and Insulin Resistance
Several reports have indicated that exposure to ambient air pollutants is associated with insulin resistance, one of the important underlying metabolic conditions predisposing to the development of T2DM [20, 21]. Kelishadi et al. conducted a population-based study of 374 children aged 10–18 years in Isfahan, Iran from November 2004 to 2005 [22]. Insulin resistance was assessed using the homeostasis model of insulin resistance (HOMA-IR). Air pollutant concentrations for CO, O3, NO2, SO2, and PM10 were obtained from three local monitoring stations, and air pollution scores were created using the Pollution Standard Index (PSI), which converted air quality measurements for all five pollutants into a daily combined score. After adjustment for confounders, insulin resistance was significantly associated with PSI in the highest quartile of exposure (Q1 vs. Q4 OR = 1.3, 95 % CI = 1.1–1.5) [22].
In another study conducted in Seoul, South Korea, the association between air pollutants and insulin resistance was evaluated using data from participants age 60 years and over (n = 560) in the Korean Elderly Environmental Panel (KEEP) study [23]. Insulin resistance was assessed using the HOMA-IR index, and exposure to air pollutants (PM10 and NO2) was estimated on an individual level using the nearest monitor approach. An IQR increase in NO2 (10.8 ppb) was significantly associated with HOMA-IR (0.72 increase, 95 % CI = 0.29–1.14), and the association was more apparent among participants who had a history of diabetes (2.78 increase, 95 % CI = 1.40–4.17) compared to those without a history of diabetes (0.48 increase, 95 % CI = 0.06–0.91). The associations with PM10 did not consistently reach statistical significance; the strongest association was observed with exposure occurring 4 days prior to the blood draw (0.14 increase, 95 % CI = −0.003–0.29).
A recent cohort study examined the association between long-term exposure to traffic-related air pollutants and insulin resistance in 397, 10-year-old children in two prospective German birth cohorts [24]. Insulin resistance was assessed using the HOMA-IR index, and individual level exposure to PM2.5, PM10, and CO2 was estimated using land use regression models. Insulin resistance increased by 17.0 % (95 % CI = 5.0–30.3) for a 2 SD increase in NO2 (10.6 μg/m3) and 18.7 % (95 % CI = 2.9–36.9) for every 2 SD increase in PM10 (6 μg/m3). Insulin resistance was also increased by 7.2 % (95 % CI = 0.8–14.0) per 500 m decrease in distance to a major road. The effect estimate for PM2.5 was elevated but did not reach statistical significance (8.6 % increase, 95 % CI = −5.7–25.0).
Finally, in a study conducted in southeast Michigan, Brook et al. demonstrated that estimated exposure to PM2.5 during the prior 5 days was associated with an increase in HOMA-IR [25]. A 10 μg/m3 increase in sub-acute exposure was associated with increased HOMA-IR (+0.7, 95 % CI = 0.1 to 1.3; p = 0.023) as well as a reduction in heart rate variability (standard deviation of normal-to-normal intervals [−13.1 ms, 95% CI = −25.3 to −0.9; p = 0.035]). No alteration in other outcomes (inflammatory markers and vascular function) occurred in relation to exposure. The findings suggest that ambient PM2.5, even at low levels, may reduce metabolic insulin sensitivity and supports the plausibility that air pollution could potentiate the development of DM via triggering autonomic imbalance.
Air Pollution and Diabetes-Related Morbidity
Several studies have shown an association between ambient air pollution and increased diabetes-related hospital admissions. In a recent case-crossover analysis of hospital admissions among Medicare enrollees in 121 US communities from 1999 to 2010, short-term exposure to PM2.5 was associated with an increase in hospitalization risks for diabetes (1.14 % increase, 95 % CI = 0.56–1.73 for a 10 μg/m3 increase in the 2 days average), along with an increased all-cause mortality risk (0.65 % increase, 95 % CI = 0.42–0.85). The association between short-term PM2.5 exposure and all-cause mortality was higher among Medicare enrollees that had a previous admission for diabetes, than among enrollees without a prior diabetes-related admission; however, this association did not reach nominal statistical significance [26].
In a study of hospitalization for acute serious complications of diabetes, coma, and ketoacidosis in Santiago, Chile between 2001 and 2008, the relative risk of hospitalization for diabetes associated with an interquartile range increase in each pollutant was 1.12 (95 % CI = 1.05–1.20) for NO2 (IQR = 27.94), 1.11 (95 % CI = 1.07–1.15) for PM10 (IQR = 34.00), and 1.11 (95 % CI = 1.06–1.16) for PM2.5 (IQR = 18.50), respectively [27].
Ambient air pollutants have also been linked with increases in other diabetes-related health complications. A recent cross-sectional investigation conducted by Tamayo et al. examined the association between residential PM10 and HbA1c levels in 9102 newly diagnosed T2DM patients (4356 women and 4746 men) in seven different regions in Germany [28]. HbA1c is an indicator of good metabolic control in diabetics; even small increases can negatively affect long-term morbidity and mortality. After adjusting for covariates, adjusted HbA1c was significantly lower in the lowest quartile of PM10 exposure in comparison to quartiles Q2–Q4 (Q1 vs. Q2 = −0.20, 95 % CI = −0.33–−0.08; Q1 vs. Q3 = −0.21, 95 % CI = −0.32–−0.09; Q1 vs. Q4 = −0.36, 95 % CI = −0.49–−0.22). In this study, T2DM patients demonstrated higher HbA1c levels when exposed to higher levels of air pollution, and therefore may be at higher risk for diabetes-related health complications and/or worse metabolic control.
In a study of diabetics in the Boston area (n = 64), exposure to particulates was associated with vasoconstriction of medium-sized conduit arteries, which is a predictor of cardiac risk and coronary artery vasomotor function [29]. Baseline brachial artery diameter (BAD) was negatively associated with black carbon (−0.02 mm, 95 % CI = −0.04–−0.003 for a 0.28 μg/m3 increase) and 5-day average exposure to ambient PM2.5 (−0.02 mm, 95 % CI = −0.05–0.01 for a 3.14 μg/m3 increase). In another study also conducted in the Boston area, among 270 adults with or at risk for diabetes, O’Neill and colleagues found 24-h exposure to PM2.5, SO2, black carbon and particle number were associated with decreased vascular reactivity among participants with diabetes, with stronger effects among those with type 2 versus type 1 [30]. Using a case-crossover design, 17 adults with T2DM were exposed to filtered air or elemental carbon ultra-fine particles for 2 h [31]. ECG (electrocardiogram) monitoring and analysis showed changes in heart rate and heart rate variability but no effects on repolarization or cardiac rhythm.
Air Pollution and Diabetes-Related Mortality
In a recently published prospective cohort analysis of 2.1 million adults from the 1991 Canadian census mortality follow-up study, Brook et al. reported a statistically significant increased risk for diabetes-related mortality (HR = 1.49, 95 % CI = 1.37–1.62) associated with a 10 μg/m3 increase in long-term PM2.5 exposure, even though exposure levels for the entire population were low (mean 8.7 μg/m3, SD 3.9 μg/m3) [32••]. Whereas a study of 52,061 participants in the Danish Diet, Cancer and Health cohort found a suggestion of increased risk for diabetes-related mortality associated with long-term measures to NO2 (mortality rate ratio: 1.31; 95% CI = 0.98, 1.76) for 10 μg/m3 increase with adjustment for confounders [33]. Positive association between diabetes-related mortality and increased acute exposure to NO2, CO, and SO2 was also reported by Goldberg and colleagues in a time series study conducted in Montreal [34].
Summary of Epidemiological Studies
These epidemiologic studies differ in study design, populations, types of pollutants, length of exposure, and endpoints selected, thus they are challenging to compare directly. In sum, they provide reasonably compelling evidence of an increased risk of diabetes and diabetes-related morbidity and mortality in association with exposure to ambient pollutants. Findings regarding gaseous indicators of traffic-related air pollution (e.g., NO2) appear to be at least as (or perhaps more) robust as PM associations, as a recent review and meta-analysis also concludes [35]. However, it is important to acknowledge that none of these studies were designed to specifically assess the risk for developing DM in relation to air pollution exposures. Thus, further studies (in particular a priori designed cohorts) are required to definitely confirm these epidemiological findings. Some studies suggest that women may be at higher risk. However, there are inconsistencies in the research to date and sex as well as susceptibility due to other factors (e.g., socioeconomic status, diet, obesity, and lifestyle) should be examined further. Future studies are also required to investigate specific aspects of the exposures most strongly linked to increased T2DM risk including the responsible sources (e.g., traffic), pollution types (e.g., gases vs. PM), particulate components (e.g., organic carbon, and metals), and durations of exposures required to instigate this metabolic disease-state.
Mechanistic Evidence
Human Studies
A few human studies have provided some insights into the mechanism whereby air pollutants might promote T2DM. There is some evidence that systemic inflammatory pathways and/or autonomic imbalance may be involved. Rioux et al. reported an association between plasma C-reactive protein concentrations and residence distance to a roadway or traffic density in T2DM patients [36]. In line with this, Khafaie et al. reported that there was a 9.34 and 7.77 % increase in C-reactive protein respectively in T2DM patients per 1 SD increase in SO2 and NOx concentrations in ambient air, suggesting the potential involvement of systemic inflammation in air pollution-mediated metabolic dysfunction. Moreover, the association was significantly higher among patients with a shorter diabetic history or without the use of anti-diabetic medication (statin and thiazolidinedione) [37]. In the Study on the influence of Air pollution on Lung function, Inflammation and Aging (SALIA, Germany), Teichert et al. assessed the plasma pro- and anti-inflammatory mediators as well as the fasting glucose/insulin levels in 363 female subjects. They found long-term exposure NO2 and NOx concentrations showed positive associations (NO2: OR = 1.465, 95 % CI = 1.049–2.046; NOx: OR = 1.409, 95 % CI = 1.010–1.967) with impaired glucose metabolism, although statistical significance was lost after correction for multiple comparisons. Circulating mediators do not have an effect on glucose metabolism as evidenced by the fact that adjustment for circulating mediators hardly affects observed ORs [38]. In a sub-acute exposure study, we found a 10 μg/m3 increase of PM2.5 was associated with a 0.7 increase in HOMA-IR (95 % CI = 0.1 to 1.3; p = 0.023) and a reduction in heart rate variability (standard deviation of normal-to-normal intervals [−13.1 ms, 95% CI = −25.3 to −0.9; p = 0.035]), suggesting the potential involvement of autonomic imbalance in air pollution-induced insulin resistance.
Animal Studies
A number of animal studies have been conducted to examine the toxicological effects of air pollution on metabolic pathology/physiology in an attempt to elucidate the underlying biological mechanisms responsible. In one of the first animal studies to verify the connection between air pollution and diabetes, Sun et al. used a whole body concentrated ambient PM system to expose wild-type C57BL/6 mice to filter air or concentrated PM2.5. In this study, impaired insulin sensitivity was confirmed among mice exposed to PM2.5 (mean = 72.7 μg/m3, exposure 6 h/day, 5 days a week for 24 weeks). In addition, PM2.5-exposed mice displayed increased visceral adiposity, enhanced systemic inflammation, and impaired vascular endothelial function [19]. In subsequent experiments, the same investigators evaluated the effect of PM2.5 (mean concentration = 111.0 μg/m3) exposure in young C57BL/6 mice (3 weeks old) fed concomitant normal or high-fat diet. Increased HOMA-IR was observed in normal chow-fed mice after only 10 weeks of exposure, with postprandial glucose approaching that seen with high fat diet-fed mice exposed to filtered air, suggesting an enhanced susceptibility to exposure early in life [18]. Further studies also supported that insulin resistance was induced in multiple organs in response to PM2.5 exposure evidenced by decreased aortic relaxation to insulin and reduced insulin signaling (Akt phosphorylation) in the aorta, liver, skeletal muscle, white adipose tissue, and brown adipose tissue [39, 40]. Consistent with these observations, Zheng et al. found impaired hepatic insulin signaling in response to PM2.5 exposure as evidenced by increased insulin receptor substrate 1 (IRS-1) serine phosphorylation at sites 1101 and 636 increased in the liver after 10 weeks of PM2.5 exposure [41]. In a recent study, Liu et al. extended these findings by demonstrating adverse effects of PM2.5 on insulin resistance in a genetically susceptible diabetic mouse model (KKAy) which occurs as early as 5 weeks of exposure [42]. Similar effects on insulin resistance have also observed in response to ozone, another important air pollutant associated with adverse human health effects. Acute ozone exposure to 1.0 ppm O3 but not 0.25 ppm caused glucose intolerance in rats of all ages, although time-course analysis indicates rapid glucose intolerance recovery 18-h post ozone exposure [43]. The mechanisms responsible for the insulin resistance appeared to be related to activation of the sympathetic nervous system in this latter study.
All the details of the underlying mechanisms whereby air pollutants, most of which are not able to cross the lung barrier, prove capable of mediating system metabolic effects remote from the site of inhalation remain to be fully elucidated. Nonetheless, the following pathways are believed to be involved in the pathophysiology of air pollution-mediated diabetes.
-
1.
Immune activation by air pollutants. Inflammation is widely believed to play a pivotal pathogenic role in insulin resistance and T2DM [44–46]. PM may directly activate innate immune cells in the lung via pattern recognition receptors (PRRs) such as Toll-like receptors (TLRs) and NOD-like receptors (NLR) [47–49], resulting in the release of inflammatory cytokines and chemokines [49, 50] and subsequent entrainment of an innate immune response with activation of adaptive immunity [51]. Leachable components such as transition metals and organic secondary intermediates generated in the lung may overflow into the circulation and trigger a systemic inflammatory response [49, 52, 53]. Using mice expressing YFP under the control of monocyte-specific promoter (c-fms), Sun et al. demonstrated that PM2.5 exposure enhanced monocyte adhesion in the microcirculation and their recruitment to adipose tissue [19]. In addition, exposure to air pollution skews macrophage activation from a protective type 2 response towards pathogenic type 1 response [18, 19, 54]. Exposure to PM2.5 increased F4/80+ macrophages in the adipose tissue, accompanied by elevated TNFα/IL-6 and reduced IL-10/N-acetyl-galactosamine specific lectin 1.
-
2.
Influences of ER stress. All three major pathways (IRE1α/XBP1, PERK/eIF2α/ATF4, and ATF6) have been suggested to be implicated in air pollution triggered responses. Watterson et al. reported that exposure to both PM2.5 and PM10 significantly increased ATF6 cleavage in human bronchial epithelial (BEAS-2B) cells [55]. Laing et al. demonstrated that PM2.5-induced ROS activated PERK/eIF2α-mediated ER stress, a process that was critical for PM2.5-induced apoptosis [56]. Similarly, it has been reported that UPR-associated proteins including ATF-4, GRP94, Hsp70, Hsp90, and BiP were significantly increased in human bronchial epithelial cells exposed to PM2.5 [54, 55]. It has been reported that IRE1α-mediated ER stress pathway was also activated in the adipose tissue of mice exposed to PM2.5 [57].
-
3.
Effects on glucose and lipid metabolism. CAP exposure has been shown to be associated with a significant increased the size of adipocytes [19, 57]. Consistent with this observation, expression of the genes involved in lipogenesis (Acaca), lipid transport (CD36), TG synthesis (dgat2), and adipocyte differentiation/lipid droplet formation (Smaf1, Ceacam1, Fsp27, Plin1, and Fit2) in white adipose tissue has been reported to be up-regulated by PM2.5 [57]. Xu et al. demonstrated that CAP exposure reduced the expression of brown adipocyte-specific genes and increased white adipocyte-specific genes in ApoE −/− mice [58]. Thus, exposure to air pollutants may adversely affect adipose tissue lipid metabolism and brown to white adipose conversion. Exposure to CAP also induced hepatic lipid deposition and reduced gluconeogenesis [40, 41]. Zheng et al. demonstrated that 10-week CAP exposure resulted in a nonalcoholic steatohepatitis-like phenotype and reduced hepatic glycogen storage in mice [41]. In accordance, CAP exposure was reported to be able to reduce O2 consumption and CO2 production in diabetes-prone mice, consistent with a reduction in metabolism. These effects were consistent with an impact of CAP on thermogenesis and might be attributed to the reduction of uncoupled protein-1 (UCP-1) expression in BAT [42]. In addition, PM2.5 exposure directly affects pathways involved in insulin resistance and glucose homeostasis, such as PPARα/PPARγ2, AKT, AMPK, IRS-1-mediated signaling, and glucose transporter GLUT4 [40, 41].
-
4.
Activation of central nervous system. Neuronal injury in the hypothalamic arcuate nucleus occurred within the first week of high fat feeding, suggesting an involvement of CNS in diet-induced obesity and IR [59]. PM particles may permeate the central nervous system via translocation along the olfactory nerve into the olfactory bulb and exert direct effects on CNS inflammation [60, 61]. Recent findings by Fonken et al. suggest that chronic PM2.5 exposure results in increased hippocampal inflammation and impairments in spatial learning memory and behavior [62]. Similarly, one may hypothesize that dysregulation of central circuits involved in metabolic control may provide a potential unified mechanism for air pollution-mediated metabolic effects. Findings from Ying et al. appear to suggest an important role of air-pollution in sympathetic activation and increased blood pressure that may result from CNS inflammation in the hypothalamus [63•]. These findings raise the possibility that CNS inflammation in key circumventricular areas may predispose to alterations in sympathetic control that may potentially drive alterations in blood pressure and insulin resistance. Although our results suggest an important role for CNS inflammation via IKKβ in PM2.5-mediated diabetes development, questions remain. The cell type(s) that are involved in the initiation of PM2.5-induced inflammatory responses in hypothalamus are currently not known. PM2.5 has been shown to permeate the CNS via translocation along the olfactory nerve into the olfactory bulb and exert direct effects on CNS inflammation [24, 45]. Alternatively, PM2.5 exposure may directly affect vagal afferents that may play an important role in modulation of pathways that affect cardiovascular and/or peripheral inflammatory responses [43].
Conclusions
Growing epidemiologic and experimental evidences suggest that air pollution is an important environmental risk factor for chronic metabolic diseases including T2DM. The pervasive and persistent effects of air pollution make it an important determinant of cardio-metabolic health at the public health level, potentially comparable to the established major risk factors for diabetes. Given the burgeoning growth of T2DM worldwide, health care providers, researchers, scientists, health, and environmental policy developers, as well as patients and the general public should be aware of this important emerging global public health concern.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–60. doi:10.1016/S0140-6736(12)61766-8.
Brook RD, Rajagopalan S, Pope 3rd CA, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–78. doi:10.1161/CIR.0b013e3181dbece1.
Mustafic H, Jabre P, Caussin C, Murad MH, Escolano S, Tafflet M, et al. Main air pollutants and myocardial infarction: a systematic review and meta-analysis. Jama. 2012;307(7):713–21. doi:10.1001/jama.2012.126.
Cesaroni G, Forastiere F, Stafoggia M, Andersen ZJ, Badaloni C, Beelen R, et al. Long term exposure to ambient air pollution and incidence of acute coronary events: Prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ. 2014;348:f7412. doi:10.1136/bmj.f7412.
Rajagopalan S, Brook RD. Air pollution and type 2 diabetes: Mechanistic insights. Diabetes. 2012;61(12):3037–45. doi:10.2337/db12-0190.
Zhao X, Sun Z, Ruan Y, Yan J, Mukherjee B, Yang F, et al. Personal black carbon exposure influences ambulatory blood pressure: Air pollution and cardiometabolic disease (AIRCMD-China) study. Hypertension. 2014;63(4):871–7. doi:10.1161/HYPERTENSIONAHA.113.02588.
Brook RD, Jerrett M, Brook JR, Bard RL, Finkelstein MM. The relationship between diabetes mellitus and traffic-related air pollution. J Occup Environ Med. 2008;50(1):32–8.
Pearson JF, Bachireddy C, Shyamprasad S, Goldfine AB, Brownstein JS. Association between fine particulate matter and diabetes prevalence in the USA. Diabetes Care. 2010;33(10):2196–201. doi:10.2337/dc10-0698.
Eze IC, Schaffner E, Fischer E, Schikowski T, Adam M, Imboden M, et al. Long-term air pollution exposure and diabetes in a population-based Swiss cohort. Environ Int. 2014;70:95–105. doi:10.1016/j.envint.2014.05.014. This work add further evidence showing an association between air pollution and diabetes. More importantly, the association could be observed even at low levels exposure which are below air quality guidelines.
Kramer U, Herder C, Sugiri D, Strassburger K, Schikowski T, Ranft U, et al. Traffic-related air pollution and incident type 2 diabetes: Results from the SALIA cohort study. Environ Health Perspect. 2010;118(9):1273–9. doi:10.1289/ehp.0901689.
Andersen ZJ, Raaschou-Nielsen O, Ketzel M, Jensen SS, Hvidberg M, Loft S, et al. Diabetes incidence and long-term exposure to air pollution: a cohort study. Diabetes Care. 2012;35(1):92–8. doi:10.2337/dc11-1155.
Coogan PF, White LF, Jerrett M, Brook RD, Su JG, Seto E, et al. Air Pollution and Incidence of Hypertension and Diabetes in African American Women Living in Los Angeles. Circulation. 2012. doi:10.1161/CIRCULATIONAHA.111.052753.
Dijkema MB, Mallant SF, Gehring U, van den Hurk K, Alssema M, van Strien RT, et al. Long-term exposure to traffic-related air pollution and type 2 diabetes prevalence in a cross-sectional screening-study in the Netherlands. Environ Health. 2011;10:76. doi:10.1186/1476-069X-10-76.
Puett RC, Hart JE, Schwartz J, Hu FB, Liese AD, Laden F. Are particulate matter exposures associated with risk of type 2 diabetes? Environ Health Perspect. 2011;119(3):384–9. doi:10.1289/ehp.1002344.
McConnell R, Shen E, Gilliland FD, Jerrett M, Wolch J, Chang CC et al. A longitudinal cohort study of body mass index and childhood exposure to secondhand tobacco smoke and air pollution: the southern California children’s health study. Environ Health Perspect. 2014.
Jerrett M, McConnell R, Wolch J, Chang R, Lam C, Dunton G, et al. Traffic-related air pollution and obesity formation in children: a longitudinal, multilevel analysis. Environ Health. 2014;13:49. doi:10.1186/1476-069X-13-49.
Wang Y, Eliot MN, Kuchel GA, Schwartz J, Coull BA, Mittleman MA, et al. Long-term exposure to ambient air pollution and serum leptin in older adults: Results from the MOBILIZE Boston study. J Occup Environ Med. 2014;56(9):e73–7. doi:10.1097/JOM.0000000000000253.
Xu X, Yavar Z, Verdin M, Ying Z, Mihai G, Kampfrath T, et al. Effect of early particulate air pollution exposure on obesity in mice: Role of p47phox. Arterioscler Thromb Vasc Biol. 2010;30(12):2518–27. doi:10.1161/ATVBAHA.110.215350.
Sun Q, Yue P, Deiuliis JA, Lumeng CN, Kampfrath T, Mikolaj MB, et al. Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation. 2009;119(4):538–46.
Muoio DM, Newgard CB. Mechanisms of disease: molecular and metabolic mechanisms of insulin resistance and beta-cell failure in type 2 diabetes. Nat Rev Mol Cell Biol. 2008;9(3):193–205. doi:10.1038/nrm2327.
Marx J. Unraveling the causes of diabetes. Science. 2002;296(5568):686–9. doi:10.1126/science.296.5568.686.
Kelishadi R, Mirghaffari N, Poursafa P, Gidding SS. Lifestyle and environmental factors associated with inflammation, oxidative stress and insulin resistance in children. Atherosclerosis. 2009;203(1):311–9. doi:10.1016/j.atherosclerosis.2008.06.022.
Kim JH, Hong YC. GSTM1, GSTT1, and GSTP1 polymorphisms and associations between air pollutants and markers of insulin resistance in elderly Koreans. Environ Health Perspect. 2012;120(10):1378–84. doi:10.1289/ehp.1104406.
Thiering E, Cyrys J, Kratzsch J, Meisinger C, Hoffmann B, Berdel D, et al. Long-term exposure to traffic-related air pollution and insulin resistance in children: Results from the GINIplus and LISAplus birth cohorts. Diabetologia. 2013;56(8):1696–704. doi:10.1007/s00125-013-2925-x.
Brook RD, Xu X, Bard RL, Dvonch JT, Morishita M, Kaciroti N, et al. Reduced metabolic insulin sensitivity following sub-acute exposures to low levels of ambient fine particulate matter air pollution. Sci Total Environ. 2013;448:66–71. doi:10.1016/j.scitotenv.2012.07.034.
Zanobetti A, Dominici F, Wang Y, Schwartz JD. A national case-crossover analysis of the short-term effect of PM2.5 on hospitalizations and mortality in subjects with diabetes and neurological disorders. Environ Health. 2014;13(1):38. doi:10.1186/1476-069X-13-38.
Dales RE, Cakmak S, Vidal CB, Rubio MA. Air pollution and hospitalization for acute complications of diabetes in Chile. Environ Int. 2012;46:1–5. doi:10.1016/j.envint.2012.05.002.
Tamayo T, Rathmann W, Kramer U, Sugiri D, Grabert M, Holl RW. Is particle pollution in outdoor air associated with metabolic control in type 2 diabetes? PLoS One. 2014;9(3):e91639. doi:10.1371/journal.pone.0091639.
Zanobetti A, Luttmann-Gibson H, Horton ES, Cohen A, Coull BA, Hoffmann B, et al. Brachial artery responses to ambient pollution, temperature, and humidity in people with type 2 diabetes: a repeated-measures study. Environ Health Perspect. 2014;122(3):242–8. doi:10.1289/ehp.1206136.
O'Neill MS, Veves A, Zanobetti A, Sarnat JA, Gold DR, Economides PA, et al. Diabetes enhances vulnerability to particulate air pollution-associated impairment in vascular reactivity and endothelial function. Circulation. 2005;111(22):2913–20. doi:10.1161/CIRCULATIONAHA.104.517110.
Vora R, Zareba W, Utell MJ, Pietropaoli AP, Chalupa D, Little EL, et al. Inhalation of ultrafine carbon particles alters heart rate and heart rate variability in people with type 2 diabetes. Part Fibre Toxicol. 2014;11(1):31. doi:10.1186/s12989-014-0031-y.
Brook RD, Cakmak S, Turner MC, Brook JR, Crouse DL, Peters PA, et al. Long-term fine particulate matter exposure and mortality from diabetes mellitus in Canada. Diabetes Care. 2013. doi:10.2337/dc12-2189. This is a study demonstrating long-term air pollution exposure, even at low levels, is associated with an increased risk of diabetes mortality.
Raaschou-Nielsen O, Sorensen M, Ketzel M, Hertel O, Loft S, Tjonneland A, et al. Long-term exposure to traffic-related air pollution and diabetes-associated mortality: a cohort study. Diabetologia. 2013;56(1):36–46. doi:10.1007/s00125-012-2698-7.
Goldberg SL, Chen L, Guerin A, Macalalad AR, Liu N, Kaminsky M, et al. Association between molecular monitoring and long-term outcomes in chronic myelogenous leukemia patients treated with first line imatinib. Curr Med Res Opin. 2013;29(9):1075–82. doi:10.1185/03007995.2013.812034.
Janghorbani M, Momeni F, Mansourian M. Systematic review and meta analysis of air pollution exposure and risk of diabetes. Eur J Epidemiol. 2014;29(4):231–42. doi:10.1007/s10654-014-9907-2.
Rioux CL, Tucker KL, Brugge D, Gute DM, Mwamburi M. Traffic exposure in a population with high prevalence type 2 diabetes—do medications influence concentrations of C-reactive protein? Environ Pollut. 2011;159(8–9):2051–60. doi:10.1016/j.envpol.2010.12.025.
Khafaie MA, Salvi SS, Ojha A, Khafaie B, Gore SS, Yajnik CS. Systemic inflammation (C-reactive protein) in type 2 diabetic patients is associated with ambient air pollution in Pune City. India Diabetes Care. 2013;36(3):625–30. doi:10.2337/dc12-0388.
Teichert T, Vossoughi M, Vierkotter A, Sugiri D, Schikowski T, Schulte T, et al. Association between traffic-related air pollution, subclinical inflammation and impaired glucose metabolism: Results from the SALIA study. PLoS One. 2013;8(12):e83042. doi:10.1371/journal.pone.0083042.
Xu X, Liu C, Xu Z, Tzan K, Zhong M, Wang A, et al. Long-term exposure to ambient fine particulate pollution induces insulin resistance and mitochondrial alteration in adipose tissue. Toxicol Sci. 2011;124(1):88–98. doi:10.1093/toxsci/kfr211.
Liu C, Xu X, Bai Y, Wang TY, Rao X, Wang A, et al. Air pollution-mediated susceptibility to inflammation and insulin resistance: Influence of CCR2 pathways in mice. Environ Health Perspect. 2014;122(1):17–26. doi:10.1289/ehp.1306841.
Zheng Z, Xu X, Zhang X, Wang A, Zhang C, Huttemann M, et al. Exposure to ambient particulate matter induces a NASH-like phenotype and impairs hepatic glucose metabolism in an animal model. J Hepatol. 2013;58(1):148–54. doi:10.1016/j.jhep.2012.08.009.
Liu C, Bai Y, Xu X, Sun L, Wang A, Wang TY, et al. Exaggerated effects of particulate matter air pollution in genetic type II diabetes mellitus. Part Fibre Toxicol. 2014;11:27. doi:10.1186/1743-8977-11-27.
Bass V, Gordon CJ, Jarema KA, MacPhail RC, Cascio WE, Phillips PM, et al. Ozone induces glucose intolerance and systemic metabolic effects in young and aged Brown Norway rats. Toxicol Appl Pharmacol. 2013;273(3):551–60. doi:10.1016/j.taap.2013.09.029.
Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444(7121):860–7. doi:10.1038/nature05485.
Despres JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444(7121):881–7. doi:10.1038/nature05488.
Horng T, Hotamisligil GS. Linking the inflammasome to obesity-related disease. Nat Med. 2011;17(2):164–5. doi:10.1038/nm0211-164.
Dostert C, Petrilli V, Van Bruggen R, Steele C, Mossman BT, Tschopp J. Innate immune activation through Nalp3 inflammasome sensing of asbestos and silica. Science. 2008;320(5876):674–7. doi:10.1126/science.1156995.
Bauer RN, Diaz-Sanchez D, Jaspers I. Effects of air pollutants on innate immunity: the role of Toll-like receptors and nucleotide-binding oligomerization domain-like receptors. J Allergy Clin Immunol. 2012;129(1):14–24. doi:10.1016/j.jaci.2011.11.004. quiz 5–6.
Kampfrath T, Maiseyeu A, Ying Z, Shah Z, Deiuliis JA, Xu X, et al. Chronic fine particulate matter exposure induces systemic vascular dysfunction via NADPH oxidase and TLR4 pathways. Circ Res. 2011;108(6):716–26. doi:10.1161/CIRCRESAHA.110.237560.
Goto Y, Ishii H, Hogg JC, Shih CH, Yatera K, Vincent R, et al. Particulate matter air pollution stimulates monocyte release from the bone marrow. Am J Respir Crit Care Med. 2004;170(8):891–7. doi:10.1164/rccm.200402-235OC.
Deiuliis JA, Kampfrath T, Zhong J, Oghumu S, Maiseyeu A, Chen LC, et al. Pulmonary T cell activation in response to chronic particulate air pollution. Am J Physiol Lung Cell Mol Physiol. 2011. doi:10.1152/ajplung.00261.2011.
Dominici F, Peng RD, Ebisu K, Zeger SL, Samet JM, Bell ML. Does the effect of PM10 on mortality depend on PM nickel and vanadium content? A reanalysis of the NMMAPS data. Environ Health Perspect. 2007;115(12):1701–3. doi:10.1289/ehp.10737.
Liberda EN, Cuevas AK, Gillespie PA, Grunig G, Qu Q, Chen LC. Exposure to inhaled nickel nanoparticles causes a reduction in number and function of bone marrow endothelial progenitor cells. Inhal Toxicol. 2010;22 Suppl 2:95–9. doi:10.3109/08958378.2010.515269.
Liu C, Ying Z, Harkema J, Sun Q, Rajagopalan S. Epidemiological and experimental links between air pollution and type 2 diabetes. Toxicol Pathol. 2013;41(2):361–73. doi:10.1177/0192623312464531.
Watterson TL, Hamilton B, Martin R, Coulombe Jr RA. Urban particulate matter causes ER stress and the unfolded protein response in human lung cells. Toxicol Sci. 2009;112(1):111–22. doi:10.1093/toxsci/kfp186.
Laing S, Wang G, Briazova T, Zhang C, Wang A, Zheng Z, et al. Airborne particulate matter selectively activates endoplasmic reticulum stress response in the lung and liver tissues. Am J Physiol Cell Physiol. 2010;299(4):C736–49. doi:10.1152/ajpcell.00529.2009.
Mendez R, Zheng Z, Fan Z, Rajagopalan S, Sun Q, Zhang K. Exposure to fine airborne particulate matter induces macrophage infiltration, unfolded protein response, and lipid deposition in white adipose tissue. Am J Transl Res. 2013;5(2):224–34.
Xu Z, Xu X, Zhong M, Hotchkiss IP, Lewandowski RP, Wagner JG, et al. Ambient particulate air pollution induces oxidative stress and alterations of mitochondria and gene expression in brown and white adipose tissues. Part Fibre Toxicol. 2011;8:20. doi:10.1186/1743-8977-8-20.
Thaler JP, Yi CX, Schur EA, Guyenet SJ, Hwang BH, Dietrich MO, et al. Obesity is associated with hypothalamic injury in rodents and humans. J Clin Invest. 2012;122(1):153–62. doi:10.1172/JCI59660.
Nakane H. Translocation of particles deposited in the respiratory system: a systematic review and statistical analysis. Environ Health Prev Med. 2012;17(4):263–74. doi:10.1007/s12199-011-0252-8.
Block ML, Elder A, Auten RL, Bilbo SD, Chen H, Chen JC, et al. The outdoor air pollution and brain health workshop. Neurotoxicology. 2012;33(5):972–84. doi:10.1016/j.neuro.2012.08.014.
Fonken LK, Xu X, Weil ZM, Chen G, Sun Q, Rajagopalan S et al. Air pollution impairs cognition, provokes depressive-like behaivors and alters hippocampal cytokine expression and morphology. Mol Psychiatry. 2011;16(10):987–95, 73. doi:10.1038/mp.2011.76
Ying Z, Xu X, Bai Y, Zhong J, Chen M, Liang Y, et al. Long-term exposure to concentrated ambient PM2.5 increases mouse blood pressure through abnormal activation of the sympathetic nervous system: a role for hypothalamic inflammation. Environ Health Perspect. 2014;122(1):79–86. doi:10.1289/ehp.1307151. This study demonstrated sympathetic activation in CNS mediates hypertensive action of chronic PM2.5 exposure.
Acknowledgments
This work was supported by the United States Environmental Protection Agency grant RD83479701 (S. Rajagopalan and R. Brook) and R01ES015146-06, R01ES019616-04, and R01ES017290-05 (S. Rajagopalan). J. Montresor-Lopez’ and R. Puett’s work was partially supported by grant R01ES019168 from the National Institute of Environmental Health Sciences (NIEHS), National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIEHS, NIH. The authors acknowledge Jessica Green-Barnes for her assistance with tables.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Xiaoquan Rao, Jessica Montresor-Lopez, Robin Puett, Sanjay Rajagopalan, and Robert D. Brook declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
No original research was performed for or presented in this review paper. Therefore, this article does not contain any studies with human or animal subjects performed by any of the authors. With regard to the authors’ human research cited in this paper, all procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000 and 2008. With regard to the authors’ animal study cited in this paper, all applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Pathogenesis of Type 2 Diabetes and Insulin Resistance
Rights and permissions
About this article
Cite this article
Rao, X., Montresor-Lopez, J., Puett, R. et al. Ambient Air Pollution: An Emerging Risk Factor for Diabetes Mellitus. Curr Diab Rep 15, 33 (2015). https://doi.org/10.1007/s11892-015-0603-8
Published:
DOI: https://doi.org/10.1007/s11892-015-0603-8