Abstract
Type 2 diabetes (T2D) patients are twice as likely to experience depressive symptoms than people without T2D, resulting in greater economic burden, worse clinical outcomes, and reduced quality of life. Several overlapping pathophysiological processes including hypothalamic-pituitary-adrenal axis hyperactivity, sympathetic nervous system activation, and elevated pro-inflammatory biomarkers are recognized as playing a role between T2D and depressive symptoms. However, other neurobiological mechanisms that may help to further link these comorbidities have not been extensively reviewed. Reduced neuroplasticity in brain regions sensitive to stress (e.g., hippocampus) may be associated with T2D and depressive symptoms. T2D patients demonstrate reduced neuroplasticity including morphological/volumetric abnormalities and subsequent neurocognitive deficits, similar to those reported by patients with depressive symptoms. This review aims to summarize recent studies on morphological/volumetric abnormalities in T2D and correlated neurocognitive deficits. Modifying factors that contribute to reduced neuroplasticity will also be discussed. Integrating reduced neuroplasticity with other biological correlates of T2D and depressive symptoms could enhance future therapeutic interventions and further disentangle the bidirectional associations between these comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Impact of Diabetes and Depressive Symptoms
Patients with type 2 diabetes (T2D) are approximately two times more likely to experience symptoms of depression, such as depressed mood, anhedonia, fatigue, or sleep difficulties compared to individuals without T2D [1]. Research has suggested that the prevalence of depressive symptoms in patients with T2D ranges between 26 and 33 % [1–3]. The presence of comorbid T2D and depressive symptoms is associated with worsened blood glucose levels [4], greater severity of diabetes complications [5], decreased behavioral adherence to self-care regimens [6], and decreased generic- and diabetes-specific quality of life [7, 8]. Further, T2D and depressive symptoms are also associated with increased functional disability [9], risk of early mortality [10], and greater healthcare costs [11]. Thus, T2D and depressive symptoms represent an important target for research to improve clinical outcomes, decrease both direct and indirect healthcare costs, and reduce the morbidity associated with T2D and depressive symptoms.
Association Between Diabetes and Depressive Symptoms
Despite the significant burden associated with T2D and depressive symptoms, relatively little attention has been given to the biological processes underlying this association. Over the past 20–25 years, diabetes research in this area has focused on predominately epidemiological studies to elucidate the causality dilemma between T2D and depressive symptoms, and subsequently, less emphasis has been placed on identifying pathophysiological processes or cellular and molecular mechanisms underlying these comorbidities [12–16]. Current findings from several systematic reviews and meta-analyses [13–15] now show that the association between T2D and depressive symptoms appears to be bidirectional rather than unidirectional. The strength of the association between depressed mood and risk of incident diabetes appears to be more robust (i.e., ranging between 20 and 60 %) [12, 13, 16], compared to the association between diabetes and risk of depressed mood (i.e., 15 %) [12, 13]. As a result of these emergent findings, diabetes researchers have now begun to take a greater interest in identifying and examining the biological processes believed to mediate this bidirectional association [12–16]. However, the underlying pathophysiological processes associated with T2D and depressive symptoms are intricately related, and the literature spans across multiple medical subspecialties encompassing several interconnected biological factors.
Biological Processes Linking Diabetes and Depressive Symptoms: State of the Literature
Within the past 5 years, reviews by Champaneri and colleagues [17] and Stuart and Buane [18••] have outlined a putative series of biological processes which may play a key role in the pathophysiology of both T2D and the presence of depressive symptoms. These processes are based on mounting evidence from human and animal studies showing that inflammatory biomarkers, neuroendocrine upregulation associated with the hypothalamic-pituitary-adrenal (HPA) axis, and subsequent adrenocortical changes are associated with each of these comorbidities separately and, when integrated, may provide a common framework for understanding the frequently observed correlates between T2D and depressive symptoms [17, 18••]. For example, within T2D, a variety of epidemiological and mechanistic studies have shown that increased levels of glucocorticoids, catecholamines, and inflammatory biomarkers are positively correlated with insulin resistance, reduced insulin secretion from β-cells, BMI/waist circumference, increased lipolysis and circulating free fatty acids, and atherosclerotic processes in humans [19, 20]. Further, it has been well documented that people without diabetes reporting depressive symptoms often demonstrate increased levels of pro-inflammatory cytokines and acute-phase reactants, greater HPA axis activity, impaired glucocorticoid receptor expression and function, norepinephrine dysregulation, and reduced synthesis of serotonin through the shunting of tryptophan to the kynurenine pathway [21–23]. Figure 1a, b depicts many of the complex, interconnected associations between several biological processes in T2D and depressive symptoms.
Shared neurobiological pathways between T2D and depressive symptoms. a Pro-inflammatory cytokines signal the brain to release corticotrophin-releasing hormone (CRH), adrenocorticotropic hormone (ACTH), and glucocorticoids (GCs), such as cortisol and catecholamines. Pro-inflammatory cytokines can also disrupt the negative feedback inhibition of GCs through ↓ GC receptor expression and functioning. In addition to their effects on ↑ HPA axis hyperactivity, pro-inflammatory cytokines influence serotonin (5-HT) metabolism indirectly by stimulating enzymes that metabolize tryptophan such as indoleamine 2,3-dioxygenase (IDO). IDO can lead to a peripheral depletion of 5-HT since it shunts tryptophan into the catabolite kynurenine. The noradrenergic neurons that innervate the paraventricular nucleus (PVN) of the hypothalamus are believed to play a key role in HPA axis activation, given that the severing of their pathways eliminates HPA axis activation following immune challenges. Cytokines can have a long-lasting increase on noradrenaline release (NE) within the PVN, and they influence the release of NE through reduced expression of presynaptic α2-adrenoceptors in the PVN and reduced reuptake of NE from axon terminals. A2-adrenoceptors are an important receptor for negative feedback control of NE release, and decreases to the presynaptic expression of these receptors lead to exaggerated NE release within the brain. NE is rapidly degraded into various metabolites, such as 3-methoxy-4-hydroxyphenylglycol (MHPG). In the brain, MHPG is the primary NE metabolite, often indicating recent SNS activity. b Internal and external factors such as metabolic overload from excessive caloric intake, physical inactivity, age, stress, and genetic predisposition can affect the development and progression of both T2D and depressive symptoms through several of the following HPA axis-, neuroendocrine-, or inflammatory-related mechanisms. The co-localization of macrophages and visceral adipocytes can produce an increased amount of pro-inflammatory cytokines and free fatty acids (FFAs) which circulate via the portal and systemic vascular systems and contribute to the release of CRP from the liver and the development of insulin resistance in peripheral tissues (i.e., muscle tissue) through intracellular signaling mechanisms such as phosphoinositide 3-kinase (PI3K), Akt kinase, and translocation of glucose transporter 4 (GLUT4). The increased hepatic triglyceride-rich (TG) very low-density lipoprotein (VLDL) production seen in dyslipidemia can result from the large amounts of pro-inflammatory cytokines released from adipose tissue as well as an increase in the re-esterification of FFAs that occur from both enhanced lipolysis and increased hepatic fatty acid synthesis. Stimulation of HPA axis leads to the synthesis of GCs such as cortisol and catecholamines, which contribute to further lipolysis and FFA release. The presence of metabolic abnormalities such as dyslipidemia can also accelerate atherosclerotic processes since excess circulating lipid particles lead to increased lipid deposition and retention within the arterial wall, contributing to macrophage infiltration and pro-inflammatory cytokine release. Further, as levels of pro-inflammatory cytokines rise, they stimulate atherosclerosis through the induction of protein kinase C, NF-кB activation, and increased release of superoxides from phagocytes, all of which contribute to cellular functioning within the arterial wall. Within peripheral tissues, continued upregulation of GCs can decrease insulin sensitivity, inhibiting glucose uptake in adipocytes, increasing hepatic gluconeogenesis, sensitizing the liver to catecholamines and glucagon, and elevating blood glucose levels
Empirical studies that have investigated whether these proposed biological processes are associated with T2D and depressive symptoms among samples of patients with both T2D and depressive symptoms are scarce [24•, 25•]. Doyle and colleagues [24•] recently demonstrated that participants with T2D and self-reported depressive symptoms had significantly higher levels of interleukin-6 (IL-6) compared to participants with either T2D or depressive symptoms alone or among those without T2D and depressive symptoms in a large, elderly sample (i.e., 3009 participants; aged 70–79) from the Health, Aging, and Body Composition Study. Greater levels of C-reactive protein (CRP) were also observed among participants with T2D, but not among those with depressive symptoms, possibly suggesting differential associations between T2D and depressive symptoms may exist for various inflammatory markers [24•]. Another study by Alvarez and colleagues [25•] examined mean differences in levels of inflammation (i.e., CRP and tumor necrosis factor α [TNF-α]) and upregulated neuroendocrine markers (i.e., 24-h urine free and salivary cortisol) among a sample of T2D patients diagnosed with major depressive disorder (MDD), assessed through the use of a structured clinical interview. Results showed that T2D patients with MDD had significantly higher levels of CRP and 24-h urine free cortisol compared to T2D patients without MDD [25•]. Findings from these investigations [24•, 25•] represent the first empirical data confirming that specific biological factors, such as increased inflammation and glucocorticoid levels, are associated with T2D and depressive symptoms as theorized by contemporary pathophysiological models (Fig. 1, see also [17, 18••]). Further research is needed to determine if additional biological factors are also associated with T2D and depressive symptoms and to what degree these factors can be collectively examined along with inflammation [24•, 25•] and glucocorticoids [25•] to provide an improved framework for understanding the association between T2D and depressive symptoms.
Reduced Neuroplasticity
In recent years, researchers have postulated that reduced neuroplasticity could help to elucidate the link between T2D and depressive symptoms, yet this biological factor has received considerably less attention than other biomarkers in existing reviews [17, 18••]. Neuroplasticity refers to the ability of the brain to respond and adapt to environmental stressors or disease in regions associated with affective expression, learning and memory, and HPA axis regulation [26–31]. Exposure to both acute and chronic stressors has been shown to modulate neuroplasticity within brain regions that are especially sensitive to stress, such as the hippocampus and dentate gyrus. The dentate gyrus is part of the hippocampal formation and is one of only two brain regions that can regenerate neurons over the lifetime, a process referred to as neurogenesis [26, 32–34]. Evaluation of neuroplasticity can be done through a variety of strategies including morphological analysis, observed changes to synaptic transmission and/or electrophysiological properties of neurons, and altered neurochemistry and neuropharmacology [28]. Although neuroplastic changes are meant to be adaptive in the short term, in order to promote host survival, prolonged exposure to various neurotoxic factors such as stress, chronic HPA axis upregulation, and increased levels of inflammation can lead to allostatic overload [34] resulting in reduced expression of dendritic spines, synaptic proteins, and increased markers of apoptosis [28, 34].
Reduced Neuroplasticity and Depressive Symptoms
Examination of neuroplasticity through structural and functional magnetic resonance imaging (MRI and fMRI) techniques have consistently shown anatomical abnormalities in brain regions that are involved in affect regulation as well as alterations to the brain circuitry involved in affective processing. For example, findings from structural MRI studies within the depressed mood literature have provided ample support for reduced neuroplasticity including morphological changes indicative of non-specific pathologies, such as cortical atrophy and white and gray matter abnormalities [28, 31]. In addition, significant volumetric reductions in the hippocampus, amygdala, prefrontal cortex, anterior cingulate, and basal ganglia have been shown among those with depressed mood symptoms [26, 28, 35–37]. Increased white matter hyperintensities and reduced neuronal spine densities [26–28, 35] have also been observed among middle-aged and elderly individuals with depressive symptoms. Further, cellular alterations in postmortem biopsies of patients with a past history of depressive symptoms have revealed hippocampal atrophy and changes in the size, shape, and density of neuronal and glial cells [38].
Neurocognitive Deficits in the Context of Reduced Neuroplasticity and Depressive Symptoms
Patients with depressive symptoms also exhibit deficits in cognitive performance that can be attributed to the morphological changes in the hippocampus, amygdala, and prefrontal cortex as well as altered functional connectivity [39, 40, 41•, 42, 43]. A recent review by McIntyre and colleagues [41•] showed that cognitive deficits were common in patients with depressive symptoms and generally included reduced performance in executive functioning, attention, learning and memory, and information processing speed. In addition, fMRI studies have shown reduced resting-state functional connectivity within the default mode network (i.e., brain regions such as the posterior cingulate cortex, medial temporal lobe, and medial prefrontal cortex which are active at rest and suspended during cognitive tasks) which may be accompanied by insulin resistance [41•, 42, 43].
Evidence now suggests that individuals with T2D demonstrate reduced neuroplasticity including morphological/volumetric abnormalities [44••, 45–51, 52•, 53–60] and subsequent neurocognitive deficits and functional connectivity alterations that can be attributed to these structural changes [44••, 48, 50, 51, 54, 61, 62], not unlike those reported among patients with depressive symptoms only. However, no contemporary reviews have attempted to summarize this literature in T2D. Further, the degree to which reduced neuroplasticity impacts modifying factors associated with T2D and depressive symptoms such as glycemic control, HPA axis hyperactivity, and inflammation remains unknown.
This review will summarize recent empirical studies reporting on (1) morphological/volumetric abnormalities among patients with T2D and (2) co-occurring neurocognitive deficits correlated with these structural/volumetric abnormalities in T2D. Potential modifying factors that may contribute to reduced neuroplasticity will also be considered including neuroendocrine, inflammatory, and adrenocortical factors.
Methods
A search of PubMed and the Cochrane Library was conducted for all English language studies using human samples published within the last 5 years (i.e., January, 2009 to April, 2014) for various permutations of the following: depressive symptoms, depressed mood, MDD, diabetes, T2D, neuroplasticity, neurogenesis, neurodegeneration, structural and functional MRI/fMRI, white and gray matter abnormalities/hyperintensities, prefrontal cortex, hippocampus, and volumetric changes. Initial searches yielded a total of 72 abstracts that were examined for topic relevance and the presence of exclusion criteria including diagnosis of type 1 diabetes (T1D) or gestational diabetes, lack of methodological rigor, and lack of empirical findings (e.g., conceptual reviews, brief communications, and letters to the editor) along with articles where full text copies were unavailable. Abstracts on T1D and gestational diabetes were excluded because the pathogenic processes involved in these disorders may not be the same as in T2D. A total of 19 original research articles met the inclusion/exclusion criteria and were included in this review.
Morphological Neuroimaging Studies in T2D
Recent findings from structural neuroimaging studies have shown that T2D patients exhibit morphological abnormalities comparable to those found in patients with depressive symptoms, which includes both white and gray matter abnormalities (Table 1) [44••, 46, 50, 52•, 58, 59] as well as more specific reductions in hippocampal and prefrontal cortex volumes [45, 47, 48, 51, 53–55, 57, 58]. However, not all studies have shown consistent results, and non-significant findings were reported most often with white matter abnormalities [46, 51, 52•]. This may reflect differences in varying measurement strategies or possible systematic differences in sample characteristics.
In one of the largest population-based studies to date, Falvey and colleagues [52•] evaluated whether the presence of T2D was associated with gray matter volume and white matter hyperintensities for total brain and regions of interest associated with memory, executive functioning, and processing speed among 85 T2D and 223 healthy participants from the Health, Aging, and Body Composition Study, Healthy Brain Project. Results showed that T2D participants had smaller total brain volume, gray matter volume, and putamen volume along with greater brain atrophy compared to participants without T2D. Further, reduced fractional anisotropy (i.e., an index of diffusion tensor imaging which is a quantitative measure of the diffusion of water through a medium that conveys information on tissue integrity not visible on MRIs) was observed for total white matter, and greater mean diffusivities were shown for the hippocampus, dorsolateral prefrontal cortex, left posterior cingulate, and right putamen among participants with T2D. These results were further corroborated by the Framingham Offspring Study which demonstrated that T2D had a −1.24 % reduction in total cerebral brain volume compared to those without T2D [59].
At least two investigations have reported longitudinal changes over 3- and 4-year follow-up periods, respectively. De Bresser and colleagues [46] evaluated the effect of T2D on cerebral atrophy and white matter hyperintensities during a 4-year period among 55 T2D and 28 matched controls. For all participants, there was a significant change in cerebral atrophy and white matter hyperintensities over time, but participants with T2D had a larger increase in lateral ventricular volume compared to those without T2D. The authors also reported that increased age was associated with greater cerebral atrophy for all patients, but the presence of T2D was not associated with accelerated cerebral atrophy in T2D patients, a finding that remains in contrast to prior cross-sectional findings [59]. In a similar study, van Elderen and colleagues [51] examined the effect of T2D on brain atrophy over a 3-year period in an elderly (aged 70–82 years) sample of 89 T2D and 438 control participants. The authors showed that participants with T2D displayed greater levels of brain atrophy compared to control participants and there was a significant association between change in atrophy, fasting glucose levels, and use of insulin treatment, suggesting that glycemic control may modify the association between T2D and cerebral atrophy [51].
Modifying Effect of Glycemic Control on Morphological Abnormalities in T2D
Several investigations have examined the effect of glycemic control on morphological abnormalities in T2D [45, 48, 50, 57]. For example, Bruehl and colleagues [48] found that frontal lobe volume was associated with average HbA1c (mean HbA1c = 7.88 %), which remained significant after controlling for T2D duration. Although further longitudinal research is needed to determine the directionality of this association, the authors postulated that suboptimal glycemic control could damage the hippocampus and prefrontal cortex, which contain the greatest density of GC receptors [64]. Thus, damage to the hippocampus or prefrontal cortex could play a role in the regulation of the HPA axis and disinhibition of negative feedback mechanisms which stimulate the release of GCs such as cortisol.
More recent findings by Cui and colleagues [50] help to further elucidate the association between glycemic control and morphological abnormalities. In this study, the association between glycemic variability and brain atrophy was examined over the course of a 72-h period. The authors found that greater glycemic variability was strongly associated with gray matter atrophy in the limbic system and temporal-parietal lobes, including the cingulum insula and hippocampus, as well as worse cognitive performance on learning and memory tasks. These results demonstrate a connection between glycemic variability and altered central autonomic regulation since atrophy within the limbic system could negatively affect the central autonomic regulator (i.e., the suprachiasmatic nucleus within the hypothalamus), thus disrupting insulin secretion and glucose absorption mechanisms [50].
Modifying Effect of Adiponectin on Morphological Abnormalities in T2D
The adipocyte-derived protein, adiponectin, is a hormone that modulates glucose regulation and fatty acid oxidation [65]. It is postulated that low levels of adiponectin may be associated with decreased insulin sensitivity and neurodegenerative effects on neurons within the hippocampus [57]. At least one investigation [57] examined if varying levels of adiponectin were associated with hippocampal volume and insulin resistance in T2D. Masaki and colleagues [57] found that patients with low adiponectin levels demonstrated a smaller mean hippocampal volume compared to patients with normal levels of adiponectin. In addition, fasting glucose and insulin levels were both elevated among patients with low adiponectin.
Modifying Effect of Inflammatory Biomarkers on Morphological Abnormalities in T2D
C-reactive protein is an acute-phase reactant that is produced by the liver as part of the pro-inflammatory response. This protein helps white blood cells to recognize and clear pathogens or damaged cells from the body/host. Individuals with levels of CRP <1, 1–3, and >3 mg/L are at low, moderate, and high risk for future cardiovascular-related events according to the American Heart Association [66]. At least one investigation [45] examined the association between high-sensitivity CRP (hsCRP) levels, hippocampal atrophy, and insulin resistance among 45 Japanese participants with T2D stratified by elevated hsCRP (defined by >3.0 mg/dL) versus those with normal levels of hsCRP and below (≤3.0 mg/dL) [45]. Patients with elevated hsCRP were found to have significantly higher fasting glucose (r = 0.36, p < .02), insulin concentrations (r = 0.62, p < .0001), and insulin resistance (r = 0.69, p < .0001) as measured by the homeostasis model assessment index. In addition, elevated hsCRP was predictive of greater cerebral atrophy and worse insulin levels among participants. The authors speculated that hsCRP may interfere with several insulin signaling mechanisms, such as the expression of insulin receptors in the hippocampus and the insulin-sensitive GLUT4 transporter, which transports glucose across cellular membranes [45]. However, not all studies measuring inflammatory biomarkers have demonstrated significant results [57] including CRP, IL-6, and TNF-α.
Modifying Effect of Cortisol Awakening Response on Morphological Abnormalities in T2D
The cortisol awakening response (CAR) refers to the normal increase of cortisol after awakening that has been increasingly used as an index of adrenocortical activity in psychiatric and non-psychiatric populations as well as patients with T2D [17]. Buehl and colleagues [47] compared salivary diurnal cortisol profiles and CAR to hippocampal volumes among 18 T2D patients and 12 matched controls. Results indicated that T2D patients had significantly reduced hippocampal volumes which were associated with a blunted CAR (r = 0.55, p < .002), but not diurnal cortisol, even after adjustment for covariates. These findings are consistent with reports on abnormal HPA axis activity in T2D samples [17, 18••], although this is the first study to demonstrate that CAR is also associated with reduced hippocampal volume.
Modifying Effect of Endothelial Dysfunction on Morphological Abnormalities in T2D
The thin inner lining of blood vessels is comprised of endothelial cells which are capable of expressing proteins on the cell surface known as adhesion molecules. Several types of adhesion molecules exist and they allow white blood cells to adhere to endothelial cells in order to facilitate transmigration into the intima. One or more adhesion molecules are generally measured in order to obtain an indicator of endothelial dysfunction which is highly correlated with cardiovascular disease processes (e.g., atherosclerosis). Novak and colleagues [58] examined the association between adhesion molecules, white matter hyperintensities, and brain atrophy in 71 T2D participants and 76 without T2D. The authors found that serum soluble vascular and intercellular adhesion molecules (i.e., sVCAM and sICAM) were both significantly associated with increased cortical atrophy in the frontal, temporal, and parietal lobes. However, these associations were strongest for those with T2D. In addition, sICAM measurements were positively correlated with glucose levels, but not with average HbA1c values [58].
Morphological and Neurocognitive Deficit Studies in T2D
Despite the fact that neurocognitive deficits have been extensively studied in T2D, relatively few investigations have examined these cognitive deficits in the context of morphological/structural abnormalities (Table 2) [44••, 48, 50, 51, 54, 59–61, 67], with even fewer studies including patients with depressive symptoms [44••, 56]. Neurocognitive deficits have been examined broadly across four major domains—verbal/non-verbal memory, executive functioning, attention, and processing speed—when examining the association between cognitive performance and structural abnormalities (Table 2) [62]. Overall, T2D patients have performed worse on measures of attention [44••, 51, 59] and verbal/non-verbal learning [48, 50, 58] compared to controls, although non-significant results have been shown in other studies [48, 58, 59] across each of these domains, respectively. This may reflect differences in study sample sizes and choice of assessment measures. Performance on a brief cognitive screening was found to be associated with hippocampal atrophy in at least one investigation [54], although most researchers have reported non-significant findings [48, 50, 60]. Some of the most sensitive measures of performance associated with morphological abnormalities among T2D participants have included immediate non-contextual verbal memory tests such as word list learning/recall tests (e.g., Hopkins Verbal Learning Test or California Verbal Test) and tests of processing speed/reaction time [63]. Measures that are less likely to show significant differences between T2D patients and control groups included measures of visuospatial processing, auditory or visual attention, and executive functioning tests [63].
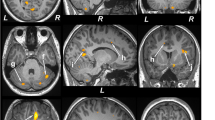
Morphological and Neurocognitive Deficit Studies in T2D with Comorbid Depressive Symptoms
To date, a limited number of investigations [44••, 56] have examined structural and functional changes in T2D patients with comorbid depressive symptoms. Ajilore and colleagues [44••] evaluated the effects of T2D and MDD on cortical gray matter thickness in the prefrontal cortex of 26 T2D + MDD participants, 26 T2D without MDD, and 20 healthy controls. The presence of MDD was established by study psychiatrists through the use of the structured clinical interview for the DSM-IV. Results showed that T2D + MDD patients had significantly reduced cortical gray matter in the medial superior frontal gyrus and the anterior cingulate compared to T2D without MDD and healthy controls. In participants with T2D + MDD, the presence of MDD was associated with a larger reduction in cortical gray matter in regions of interest compared to T2D without MDD who demonstrated smaller comparative reductions in gray matter thickness. Prior work by Kumar and colleagues [68] also showed similar volumetric reductions in gray matter within the anterior cingulate of T2D without MDD patients. Regarding cognitive performance, participants with T2D + MDD performed worse on tasks of attention compared to those with T2D without MDD and healthy controls.
Another investigation by Kumar and colleagues [56] examined white and gray matter regions of patients with T2D and MDD, the latter of which was diagnosed through the use of clinical interviews and the Hamilton Rating Scale among 16 T2D + MDD, 22 T2D without MDD, and 30 healthy controls. Primary findings indicated that patients with T2D + MDD had significantly smaller caudate nuclei compared to T2D without MDD and healthy controls. The authors reported that these findings were consistent with their prior research suggesting that patients with T2D + MDD had smaller prefrontal gray matter volumes. Further, measures of executive functioning and processing speed were also significantly lower among patients with T2D + MDD [68, 69].
Discussion
Findings from this review confirm that individuals with T2D demonstrate reduced neuroplasticity as indicated by morphological/volumetric abnormalities and subsequent neurocognitive deficits that can be attributed to these observed structural changes. T2D patients were shown to have white and gray matter abnormalities [44••, 46, 50, 52•, 58, 60] along with more specific reductions in hippocampal and prefrontal cortex volumes [45, 47, 48, 51, 53–55, 57, 58, 60]. Cognitive performance was also associated with these structural abnormalities, with T2D patients performing worse on measures of attention [44••, 51, 60] and verbal/non-verbal learning [48, 50, 59] compared to participants without T2D. These findings are comparable to those reported by studies examining reduced neuroplasticity and neurocognitive deficits among patients with depressive symptoms. Thus, reduced neuroplasticity appears to be an underlying biological factor associated with T2D and depressive symptoms, yet the literature on this topic remains poorly integrated, which has been a common limitation when examining biological factors associated with these comorbidities [24•, 25•]. Only a limited number of studies were identified in this review that examined reduced neuroplasticity among patients with both T2D and depressive symptoms. These investigations [44••, 56] showed that patients with T2D and depressive symptoms had significantly reduced cortical gray matter in the medial superior frontal gyrus and the anterior cingulate compared to T2D patients without depressive symptoms and healthy controls. Both of these regions contain neural circuitry that is implicated in the regulation of affective processing, cognition, and behavior. Further, the anterior cingulate region is also the locus of neurochemical aberrations associated with depressive symptoms (e.g., lower levels of glutamate/glutamine—an excitatory neurotransmitter involved in neural transmission). Additional research examining the effect(s) of structural changes within prefrontal and subcortical regions, particularly morphological/volumetric abnormalities within the medial superior frontal gyrus and the anterior cingulate, among patients with both T2D and depressive symptoms is warranted. Findings from this research may help to add to our growing understanding of the bidirectional pathophysiological processes associated with T2D and depressive symptoms and to identify potential biological targets for intervention.
This review also shows that reduced neuroplasticity is connected with several other biological processes associated with T2D and depressive symptoms. For example, significant associations emerged between reduced neuroplasticity and modifying factors such as glycemic control [45, 48, 50, 57], lower adiponectin [57], higher hsCRP [45], CAR [47], and endothelial dysfunction [57]. Among the few longitudinal studies examining reduced neuroplasticity [46, 51], at least one suggested that worse glycemic control was associated with a significant change in cerebral atrophy over a 3-year period [51]. This may help to establish a potential link between glycemic control and specific brain regions involved in the central autonomic processing of glucose which provides a promising area for future research with tangible translational benefits for both the prevention and treatment of T2D and depressive symptoms. Given that less than half of the studies reviewed included measurements of biological correlates of T2D and depressive symptoms in addition to reduced neuroplasticity (e.g., inflammation or cortisol), more research is needed to determine how integrating reduced neuroplasticity with other biological factors may enhance future therapeutic interventions and further disentangle the bidirectional associations between these comorbidities.
Several limitations exist within this literature which negatively impacts the inferences that can be drawn from this review. First, there is considerable heterogeneity among samples that limit the generalizability of the findings. The extent to which reduced neuroplasticity is a cause or consequence of various modifying factors cannot be determined given that the large majority of studies documented in this review are cross sectional which limits causal inferences. Longitudinal investigations are needed to better understand the order of effects between variables such as glycemic control and volumetric changes in the hippocampus and prefrontal cortex. Future investigations on morphological changes in T2D also need to include multiple assessments of potential modifying biological variables (e.g., inflammatory markers or cortisol) in order to further elucidate the association between these factors and T2D and depressive symptoms as well as to stabilize measurement data over multiple time points.
Conclusions
An emerging body of literature suggests that reduced neuroplasticity is a shared biological factor between T2D and depressive symptoms. Reduced neuroplasticity also appears to be correlated with several other biological factors (e.g., glycemic control, inflammation, adiponectin, cortisol, and endothelial dysfunction) believed to be closely associated with T2D and depressive symptoms. Whether reduced neuroplasticity is a cause or consequence of T2D and depressive symptoms has not been determined, yet the integration of neuroplasticity with other modifying biological factors will help to provide an improved framework for understanding the complex bidirectional association between T2D and depressive symptoms. Further research on reduced neuroplasticity in T2D and depressive symptoms, particularly in prefrontal and subcortical regions, is warranted to establish whether therapeutic interventions tailored towards improving neuroplasticity may enhance the treatment and prevention of these comorbidities. Thus, T2D and depressive symptoms represent an important target for research to improve clinical outcomes and quality of life, decrease overall healthcare costs, and reduce the significant morbidity associated with T2D and depressive symptoms.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069–78.
Gavard JA, Lustman PJ, Clouse RE. Prevalence of depression in adults with diabetes: an epidemiological evaluation. Diabetes Care. 1993;16:1167–78.
de Groot M, Doyle T, Hockman E, Wheeler C, Pinkerman B, Shubrook J, et al. Depression among type 2 diabetes rural Appalachian clinic attendees. Diabetes Care. 2007;30:1602–4.
Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, Clouse RE. Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care. 2000;23:934–42.
de Groot M, Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 2001;63:619–30.
Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes. Impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160:3278–85.
Jacobson AM, de Groot M, Samson JA. The effects of psychiatric disorders and symptoms on quality of life in patients with type I and type II diabetes. Qual Life Res. 1997;6(1):11–20.
Egede L, Osborn C. Role of motivation in the relationship between depression, self-care and glycemic control in adults with type 2 diabetes. Diabetes Educ. 2010;36(2):276–83.
Katon W, Von Korff M, Ciechanowski P, Russo J, Lin E, et al. Behavioral and clinical factors associated with depression among individuals with diabetes. Diabetes Care. 2004;27:914–20.
Katon W, Rutter C, Simon G, Lin EB, Ludman E, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28:2668–72.
Simon G, von Korff M, Barlow W. Health care costs of primary care patients with recognized depression. Arch Gen Psychiatry. 1995;52:850–6.
Penckofer S, Doyle T, Byrn, M, Lustman PJ. State of the science: depression and type 2 diabetes. W J Nurs Res. 2014;1–25.
Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan. Diabetes Care. 2008;31:2382–90.
Nefs G, Pouwer F, Denollet J, Pop V. The course of depressive symptoms in primary care patients with type 2 diabetes: results from the Diabetes, Depression, Type D Personality Zuidoost-Brabant (DiaDDZoB) study. Diabetologia. 2012;55:608–16.
Nouwen A, Winkley K, Twisk J, Lloyd CE, Peyrot M, Ismail K, et al. Type 2 diabetes as a risk factor for the onset of depression: a systematic review and meta-analysis. Diabetologia. 2010;53:2480–6.
Cosgrove MP, Sargeant LA, Griffin SJ. Does depression increase the risk of developing type 2 diabetes? Occup Med. 2008;58:7–14.
Champaneri S, Wand GS, Malhotra SS, Casagrande SS, Golden SH. Biological basis of depression in adults with diabetes. Curr Diabetes Rep. 2010;10:396–405.
Stuart MJ, Baune BT. Depression and type 2 diabetes: inflammatory mechanisms of a psychoneuroendocrine co-morbidity. Neurosci Biobehav Rev. 2012;36:658–76. Well written review paper that highlights several biological mechanisms associated with T2D and depression with a particular emphasis on cellular and molecular research.
Pickup JC. Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes. Diabetes Care. 2004;27:813–23.
Knol MJ, Twisk JWR, Beekman ATF, Heine RJ, Snoek FJ, Pouwer F. Depression as a risk factor for the onset of type 2 diabetes. A meta-analysis. Diabetologia. 2006;49:837–45.
Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol. 2006;27:24–31.
Ruhe HG, Mason NS, Schene AH. Mood is indirectly related to serotonin, norepinephrine and dopamine levels in humans: a meta-analysis of monoamine depletion studies. Mol Psychiatry. 2007;12:331–59.
Dantzer R, O’Connor JC, Freund GC, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nature. 2008;9:46–7.
Doyle TA, de Groot M, Harris T, Schwartz F, Strotmeyer ES, Johnson KC, et al. Diabetes, depressive symptoms, and inflammation in older adults: results from the Health, Aging, and Body Composition Study. J Psychosom Res. 2013;75:419–24. First empirical study to confirm that previously hypothesized markers of inflammation are elevated in participants with both T2D and self-reported depressive symptoms to a greater degree than participants with either disorder alone or people without T2D and depressive symptoms.
Alvarez A, Faccioli J, Guinzbourg M, Castex MM, Bayon C, Masson W. Endocrine and inflammatory profiles in type 2 diabetic patients with and without major depressive disorder. BMC Res Notes. 2013;6:61. Provides corroborating evidence that previously hypothesized markers of inflammation are elevated in participants with both T2D and clinically diagnosed MDD as well as the first reported evidence that 24-hour urine free cortisol levels are higher among participants with both disorders compared to participants with T2D alone.
Fossati P, Radtchenko A, Boyer P. Neuroplasticity: from MRI to depressive symptoms. Eur Neuropsychopharmacol. 2004;14(5):S503–10.
Reagan L. Diabetes as a chronic metabolic stressor: causes, consequences and clinical complications. Exp Neurol. 2012;233(1):68–78.
Ho N, Sommers MS, Lucki I. Effects of diabetes on hippocampal neurogenesis: links to cognition and depression. Neurosci Biobehav Rev. 2013;37:1346–62.
Maes M, Yirmyia R, Noraberg J, Brene S, Hibbein J, Perini G, et al. The inflammatory & neurodegenerative (I&ND) hypothesis of depression: leads for future research and new drug developments in depression. Metab Brain Dysfunct. 2009;24:27–53.
Koehl M, Abrous DN. A new chapter in the field of memory: adult hippocampal neurogenesis. Eur J Neurosci. 2011;33:1101–14.
Snyder JS, Soumier A, Brewer M, Pickel J, Cameron HA. A role for adult neurogenesis in spatial long-term memory. Neuroscience. 2011;130:843–52.
Black P. The inflammatory consequences of psychologic stress: relationship to insulin resistance, obesity, atherosclerosis and diabetes, type II. Med Hypotheses. 2006;67:879–91.
Black PH. The inflammatory response is an integral part of the stress response: implications for atherosclerosis, insulin resistance, type II diabetes and metabolic syndrome X. Brain Behav Immun. 2003;17(5):350–64.
McEwen BS. Protective and damaging effects of stress mediators: central role of the brain. Dialogues Clin Neurosci. 2006;8:367–81.
Konarski JZ, McIntyre RS, Kennedy SH, Rafi-Tari S, Soczynska JK, Ketter TA, et al. Volumetric neuroimaging investigations in mood disorders: bipolar disorder versus major depressive disorder. Bipolar Disord. 2008;10:1–37.
Eker C, Gonul AS. Volumetric MRI studies of the hippocampus in major depressive disorder: meanings of inconsistency and directions for future research. World J Biol Psychiatry. 2010;11:19–35.
Campbell S, MacQueen G. An update on regional brain volume differences associated with mood disorders. Curr Opin Psychiatr. 2006;19(1):25–33.
Stockmeier CA, Mahajan GJ, Konick LC, Overholser JC, Jurjus GJ, Meltzer HY, et al. Cellular changes in the postmortem hippocampus in major depression. Biol Psychiatry. 2004;56(9):640–50.
Fontan-Lozano A, Saez-Cassanelli JL, Inda MC, de los Santos-Artaga M, Sierra-Dominguez SA, Lopez-Lluch G, et al. Caloric restriction increases learning consolidation and facilitates synaptic plasticity through mechanisms dependent on NR28 subunits of the NMDA receptor. J Neurosci. 2007;27:10185–95.
Morris RG. Episodic-like memory in animals: psychological criteria, neural mechanisms and the value of episodic-like tasks to investigate animal models of neurodegenerative disease. Philos Trans R Soc Lond B Biol Sci. 2001;356:1453–65.
McIntyre RS, Cha DS, Soczynska JK, Woldeyohannes HO, Gallaugher LA, Kudlow P, et al. Cognitive deficits and functional outcomes in major depressive disorder: determinants, substrates, and treatment interventions. Depression Anxiety. 2013;30:515–27. One of the most comprehensive reviews of cognitive deficits and functional outcomes in depression.
Reiman EM, Chen K, Alexander GE, et al. Functional brain abnormalities in young adults at genetic risk for late-onset Alzheimer’s dementia. Proc Natl Acad Sci U S A. 2004;101:284–9.
Sheline YI, Raichle ME, Snyder AZ, et al. Amyloid plaques disrupt resting state default mode network connectivity in cognitively normal elderly. Biol Psychiatry. 2010;67:584–7.
Ajilore O, Narr K, Rosenthal J, Pham D, Hamilton L, Watari K, et al. Regional cortical gray matter thickness differences associated with type 2 diabetes and major depression. Psychiatry Res. 2010;184(2):63–70. Demonstrated that volumetric changes were greatest among patients with T2D + MDD compared to other groups/controls; one of only a few recent investigations to collect data from patients with both T2D + MDD.
Anan F, Masaki T, Shimomura T, Fujiki M, Umeno Y, Eshima N, et al. High-sensitivity C-reactive protein is associated with hippocampus volume in nondementia patients with type 2 diabetes. Metab Clin Exp. 2011;60:460–6.
de Bresser J, Tiehuis AM, van den Berg E, Reijmer YD, Jongen C. & jaap Kappelle, L et al.: progression of cerebral atrophy and white matter hyperintensities in patients with type 2 diabetes. Diabetes Care. 2010;33:1309–14.
Bruehl H, Wolf OT, Convit AA. Blunted cortisol awakening response and hippocampal atrophy in type 2 diabetes. Psychoneuroendocrinology. 2009a;34(6):815–21.
Bruehl H, Wolf OT, Sweat V, Tirsi A, Richardson S, Convit A. Modifiers of cognitive function and brain structure in middle-aged and elderly individuals with type 2 diabetes. Brain Res. 2009;1280:186–94.
Brundel M, van den Heuvel M, de Bresser J, jaap Kappelle L, jan Biessels G. Cerebral cortical thickness in patients with type 2 diabetes. J Neurol Sci. 2010;299:126–30.
Cui X, Abduljalil A, Manor BD, Peng C, Novak V. Multi-scale glycemic variability: a link to gray matter atrophy and cognitive decline in type 2 diabetes. PLoS One. 2014;9(1):e86284.
van Elderen SGC, de Roos A, de Craen AJM, Westendorp RGJ, Blauw GJ, Jukema JW. Progression of brain atrophy and cognitive decline in diabetes: a 3-year follow-up. Neurology. 2010;75:997–1002.
Falvey CM, Rosano C, Simonsick EM, Harris T, Strotmeyer ES, Satterfield S. Macro- and microstructural magnetic resonance imaging indices associated with diabetes among community-dwelling older adults. Diabetes Care. 2013;36:677–82. Provides results on structural abnormalities in T2D patients compared to controls using one of the largest population-based studies to date, the Healthy, Aging, and Body Composition Study.
Hapel R, Onopa R, Convit A. Type 2 diabetes affects brain health differentially in men and women. Diabetes Metab Res Rev. 2012;28(1):76–83.
Hayaski K, Kurioka S, Yamaguchi T, Morita M, Kanazawa I, Takase H, et al. Association of cognitive dysfunction with hippocampal atrophy in elderly Japanese people with type 2 diabetes. Diabetes Res Clin Pract. 2011;94:180–5.
Kamiyama K, Wada A, Suqihara M, Kurioka S, Hayashi K, Hayashi T, et al. Potential hippocampal region atrophy in diabetes type 2: a voxel-based morphometry VSRAD study. Jpn J Radiol. 2010;28(4):266–72.
Kumar A, Gupta R, Thomas A, Ajilore O, Hellemann G. Focal subcortical biophysical abnormalities in patients diagnosed with type 2 diabetes and depression. Arch Gen Psychiatry. 2009;66(3):324–30.
Masaki T, Anan F, Shimomura T, Fujiki M, Saikawa T, Yoshimatsu H. Association between hippocampal volume and serum adiponectin in patients with type 2 diabetes. Metab Clin Exp. 2012;61:1197–200.
Novak V, Zhao P, Manor B, Sejdic E, Alsop D, Abduljalil A, et al. Adhesion molecules, altered vasoreactivity, and brain atrophy in type 2 diabetes. Diabetes Care. 2011;34:2438–41.
Tan ZS, Beiser AS, Fox CS, Au R, Himali JJ, Debette S. Association of metabolic dysregulation with volumetric brain magnetic resonance imaging and cognitive markers of subclinical brain aging in middle-aged adults. Diabetes Care. 2011;34:1766–70.
Reijmer YD, van den Berg E, de Bresser J, Kessels RPC, Kappelle LJ, Algra A, et al. Accelerated cognitive decline in patients with type 2 diabetes: MRI correlates and risk factors. Diabetes Metab Res Rev. 2011;27:195–202.
Reijmer YD, Brundel M, de Bresser J, Kappelle LJ, Leemans A, Biessels GJ, et al. Microstructural white matter abnormalities and cognitive functioning in type 2 diabetes. Diabetes Care. 2013;36:137–44.
Musen G, Jacobson AM, Bolo NR, Simonson DC, Shenton ME, McCartney RL, et al. Resting-state brain functional connectivity is altered in type 2 diabetes. Diabetes. 2012;61:2375–9.
Zhou H, Lu W, Shi Y, Bai F, Chang J, Yuan Y, et al. Impairments in cognition and resting-state connectivity of the hippocampus in elderly subjects with type 2 diabetes. Neurosci Lett. 2010;473:5–10.
Caetano SC, Kaur S, Brambilla P, Nicoletti M, Hatch JP, Sassi RB, et al. Smaller cingulate volumes in unipolar depressed patients. Biol Psychiatry. 2006;59:702–6.
Diez JJ, Iglesias P. The role of the novel adipocyte-derived hormone adiponectin in human disease. Eur J Endocrinol. 2003;148(3):293–300.
Ridker PM. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation. 2003;107:363–9.
Wong RHX, Scholey A, Howe, PRC. Assessing premorbid cognitive ability in adults with type 2 diabetes mellitus: a review with implications for future intervention studies. Curr Diab Rep. (In Press).
Kumar A, Haroon E, Darwin C, Pham D, Ajilore O, Rodriguez G, et al. Gray matter prefrontal changes in type 2 diabetes detected using MRI. J Magn Reson Imaging. 2008;27(1):14–9.
Awad N, Gagnon M, Messier C. The relationship between impaired glucose tolerance, type 2 diabetes, and cognitive function. J Clin Exp Neuropsychol. 2004;26(8):1044–80.
Compliance with Ethics Guidelines
Conflict of Interest
Todd Doyle, Angelos Halaris, and Murali Rao declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Psychosocial Aspects
Rights and permissions
About this article
Cite this article
Doyle, T., Halaris, A. & Rao, M. Shared Neurobiological Pathways Between Type 2 Diabetes and Depressive Symptoms: a Review of Morphological and Neurocognitive Findings. Curr Diab Rep 14, 560 (2014). https://doi.org/10.1007/s11892-014-0560-7
Published:
DOI: https://doi.org/10.1007/s11892-014-0560-7