Abstract
Consumer health technologies can educate patients about diabetes and support their self-management, yet usability evidence is rarely published even though it determines patient engagement, optimal benefit of any intervention, and an understanding of generalizability. Therefore, we conducted a narrative review of peer-reviewed articles published from 2009 to 2013 that tested the usability of a web- or mobile-delivered system/application designed to educate and support patients with diabetes. Overall, the 23 papers included in our review used mixed (n = 11), descriptive quantitative (n = 9), and qualitative methods (n = 3) to assess usability, such as documenting which features performed as intended and how patients rated their experiences. More sophisticated usability evaluations combined several complementary approaches to elucidate more aspects of functionality. Future work pertaining to the design and evaluation of technology-delivered diabetes education/support interventions should aim to standardize the usability testing processes and publish usability findings to inform interpretation of why an intervention succeeded or failed and for whom.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent years, there has been an explosion of self-management support systems and applications (“apps”) developed for patients with diabetes. Widespread consumer adoption and use of computers, the Internet, and mobile devices has created an opportunity to leverage these platforms to augment patient care. Technologies can offer an extended reach to patients by delivering diabetes education and self-care support (e.g., medication adherence reminders, mobile or web applications for monitoring and improving diet/physical activity) or by facilitating patients’ communication with providers or peers (e.g., patient web portals or asocial networking forums) in their everyday lives. While many healthcare systems and researchers assume technology-driven solutions (e.g., online portals for access to electronic health records, mobile phone applications) provide various benefits, including improved patient outcomes [1] and cost savings [1, 2], the effectiveness of these solutions has been mixed [3]. One explanation for a lack of effectiveness may be incomplete front-end formative research prior to evaluating the solutions’ effect on outcomes.
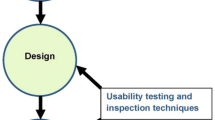
There is a continuum of necessary steps to ensure a technology-based solution is meaningful, useful, and engaging to end users, resulting in maximum benefit from utilization. These steps include conducting user-centered design research during the development phase and employing methods of usability testing prior to evaluating a technology-based intervention’s effect on patient outcomes. Researchers have been applying user-centered design principles [4] and to a lesser degree post-production usability testing. Borrowing from the fields of design/industrial engineering and human factors engineering, user-centered design involves understanding the needs, values, and abilities of users to improve the quality of users’ interactions with and perceptions of the technology [5, 6]. Once a technology-delivered solution has been developed (usually in an iterative fashion with direct user input), usability testing validates the product to determine how it meets user needs, such as ease of use (e.g., presence of technical glitches), accessibility (e.g., developed with simple language and clear instructions), and functionality (e.g., being used as intended) for the target audience with the ultimate goal of improving the spread and sustainability of use (i.e., continued user engagement across various settings) [5]. It is this second phase of usability testing that we are focused on in this manuscript.
There are several usability testing methods that have been adopted by healthcare and health services researchers. These often include qualitative assessments (i.e., focus groups or individual interviews) to learn about users’ experience and likeability of the system/application, system usage data that automatically captures objective use of the system/application, and usability questionnaires that gather users’ self-reported use along with ratings of satisfaction, ease of use, and desire to use the system/application and/or recommend it to others [7]. Still used, but to a lesser degree, are think aloud interviews, cognitive walkthroughs, heuristic evaluations, and other methods [7]. The goal of our review was to characterize methods for testing usability in the recent diabetes literature, describe the lessons learned across studies, and draw conclusions about how usability testing assists with user engagement and ultimately allows for testing a technology-delivered intervention as intended.
Methods
Data Sources and Search Strategy
In January 2014, a published literature search was conducted of technology-delivered interventions for patients with either type 1 or type 2 diabetes. We generated three lists of relevant key words that included diabetes-related terms (e.g., diabetes, diabetic), technology-related terms (e.g., technology, Internet, mobile, website, patient portal), and usability testing methods/terms (e.g., usability, think aloud, heuristic evaluation, cognitive walkthrough). The lists were intralinked with “OR” and interlinked with “AND” so that all candidate articles contained at least one diabetes-related, technology-related, and usability testing-related term. Hand searching reference lists of articles yielded additional studies for review.
Our search relied on PubMed-indexed articles published from 2009 to 2013. Authors CYO and CRL performed literature searches and independently reviewed each title and abstract for potential relevance to the research questions. Articles included by either investigator underwent full-text screening. Authors CYO and CRL independently evaluated candidate full-text articles for inclusion and resolved discrepancies through review and discussion. A third, independent reviewer, author US, assisted with reconciling discrepancies as needed.
Study Eligibility
Studies were included in the present review if they satisfied all of the following criteria: (1) included a technology-supported intervention platform with a patient interface (e.g., Internet, cell phone, mobile device); (2) tested a patient-facing diabetes self-care monitoring, support, or educational or behavioral solution; (3) employed a usability testing method; (4) were published in a peer-reviewed journal from 2009 to 2013; and (5) were published in English. Articles were excluded if they focused only on the design phase of the intervention/technology (i.e., because we consider user-centered design to be a distinct and separate entity); were based on secondary analyses; were a meta-analysis, systematic review, or editorial/commentary; targeted nonpatients (e.g., physicians or other medical staff); or tested a medical device (e.g., new insulin pen) instead of a technology-based educational, self-management solution or tool for monitoring patients’ behavior for self-care decision-making.
We initially identified 135 studies. After removing duplicate studies and conducting an initial title and abstract review to apply our inclusion and exclusion criteria outlined above, we identified 26 articles for full-text review. Additional hand review of these articles produced two more articles for consideration, for a total of 28 articles reviewed. Authors CYO and CRL excluded one of these articles because the technology-based solution was not designed specifically for people with diabetes, per se, and was therefore not tested with that user group [8]. These authors then excluded three more articles because the technology-based solution collected and transmitted patient data to providers (i.e., telemonitoring) without offering either a patient-facing component that allowed patients to track self-care or a close-looped system in which patient data was then used to educate or provide patients with self-care support [9–11]. Author US reconciled discrepancies, resulting in the removal of one additional article that tested the usability of an artificial pancreas built atop the IOS operating system that offered minimal self-care monitoring, education, or support [12]. Thus, a total of 23 articles were included in our narrative synthesis.
Narrative Synthesis
In an effort to bring together the broadest knowledge from a variety of usability testing study designs and methodologies, we analyzed studies using a narrative synthesis approach [13]. This approach is not to be confused with the narrative descriptions that accompany many reviews. Rather, a narrative synthesis is an attempt to systematize the process of analysis when a meta-analysis or a systematic review may not be appropriate because of the range of methodologies in the studies reviewed. Consistent with the narrative synthesis steps proposed by Popay et al. [13], we conducted (1) a preliminary analysis of the included studies, (2) an exploration of relationships between included studies, and (3) an assessment of the robustness of the synthesis. Due to the exploratory nature of our review, we omitted theory development from our synthesis process [13]. Preliminary synthesis consisted of extracting the descriptive characteristics of the studies in a table and producing a textual summary of the studies employing a specific usability testing design/methodology. When appropriate, a thematic analysis was used to extract themes from the cluster of studies within a given methodological domain. The subsequent narrative results represent the main areas of knowledge available about the types of usability testing methods employed with technology-based diabetes education and behavioral interventions from 2009 to 2013. We conclude with a reflection on our synthesis process and implications for technology-based intervention research in diabetes.
Results
Of the 23 articles included in the final sample (Table 1), over two thirds were published in the past 2 years (i.e., 2012 or 2013)—indicating an increase in this type of research. Eight of these articles tested web-delivered solutions, 12 tested mobile phone-delivered solutions, and 3 leveraged personal digital assistants (PDAs). Usability testing studies were largely conducted in the USA (n = 11), followed by Norway (n = 5), the Netherlands (n = 3), and Canada (n = 2). The remaining usability studies were conducted in Japan, Spain, and the UK. Thirteen studies included adult users with diabetes; six included children/adolescents with diabetes and/or their parents; two included expert reviewers/testers; and two included volunteer testers. Finally, of the studies including users with diabetes (n = 19), 10 reported patient characteristics or inclusion criteria beyond age, gender, and diabetes type, duration, and/severity (e.g., HbA1c).
The included articles covered all usability methodologies mentioned above; 16 reported results from usability questionnaires, 13 captured system usage data, 12 used qualitative methods in the form of focus groups or individual interviews, 3 used think aloud, 1 used a cognitive walkthrough, and 1 used a heuristic evaluation. These categories were not mutually exclusive as many studies used a combination of different methodological approaches.
Usability Questionnaire
Over two thirds of the studies included in our review relied on user self-report to assess the usability of a technology-based diabetes self-management solution. Survey- or questionnaire-based scoring of usability solicits users’ subjective opinion, perceived ease of use and helpfulness, and/or experiences with using a technology-based intervention or application. While studies utilizing this approach differed in terms of what they asked users, common user outcomes were an overall usability score of the system being studied, and satisfaction with and general ease of use of the system/application and/or its feature(s). Most of the 16 usability studies that included surveys relied on homegrown items that mapped onto the solution being tested (n = 12) rather than reliable and validate instruments of usability (n = 4). Many studies provided only a general discussion of their usability scoring, such as the specific questions asked with the sample mean score for each question. While several studies assessed usability only as users’ experience (such as satisfaction or willingness to recommend the technology to someone else), others scored a wider variety of concepts related to functionality and users’ acceptability of the system. For example, Britto et al. [14] reported that a patient portal with a diabetes chronic condition-specific page was rated highest for interface pleasantness and likeability, but rated lowest for error messages and clarity of information.
Qualitative Assessment
A qualitative assessment of usability identifies barriers to using a technology-based solution and reasons for nonuse or discontinued use more comprehensively than usability questionnaires. A qualitative assessment can detect unanticipated usability challenges that may not be included in a quantitative usability measure. Nearly half (12 of 23, 52 %) of the included studies used qualitative methods, specifically focus groups and/or individual interviews. Data gathered pertained to users’ perceptions of and/or personal experiences with an application’s ease of use and accessibility, and their ideas for how it might be improved. For instance, Urowitz et al. [15] conducted a qualitative usability evaluation of a web-based diabetes portal. Major themes included users’ suggested improvements by differentiating between the most used and well-liked features (e.g., the graphical display of the patient self-monitoring data and the ability to email with providers) and the least used features (e.g., the online library). Moreover, users generated new ideas about additions to the portal, such as an online tutorial to help future users become oriented with the portal’s available features and how to use them.
System Usage Data
Usability data captured from an application or what is often referred to as system usage data can complement users’ subjective quantitative or qualitative self-reports. By design, applications gather objective data on how often users log in, upload information (e.g., blood glucose values or dietary information), use/view specific features, or are responsive (e.g., replying to a text message). For example, Dick et al. [16] leveraged system-captured usability data to understand how low-income patients with diabetes used a text messaging program. Usability outcomes included the average length of time it took users to respond to each system-generated message, the average number of text messages users sent over the course of the study, and the content of those messages (e.g., medication adherence vs. blood glucose monitoring). The authors also provided a detailed account of who was approached to participate in the study (i.e., characteristics of potential participants, including their prior use of text messaging) and who ultimately participated in the study, allowing for inferences to be made about the generalizability of findings to other, comparable patient populations. To our knowledge, no studies cited agreed-upon standards for reporting system usage data.
Think Aloud (Cognitive Task Analysis)
A much smaller proportion of included studies (n = 3) used the think aloud method to assess system/application usability. In a think aloud usability test, participants are asked to use a system/application while continuously thinking out loud—that is, simply verbalizing their thoughts as they move through the user interface at will, or when asked to complete a specific task [17]. This method facilitates understanding how users perceive each feature by observing how and in what order they interact with a system/application. For example, Simon et al. [18] used a think aloud approach to identify patients’ barriers to using a web-based patient-guided insulin titration application. They observed patients interacting with the website in a clinic setting or in a more “experimental” location as well as in patients’ homes and in doing so identified 17 unique usability concerns that needed to be addressed prior to evaluating the application’s effect on patient outcomes.
Cognitive Walkthrough and Heuristic Evaluation
The final two usability testing methods typically involve expert-based as opposed to user-based system/application inspections [7]. A cognitive walkthrough involves evaluating first-time use (without formal training) of the system/application, in which an expert (1) sets a goal to be accomplished, (2) searches for available actions, (3) selects an action or task that seems most relevant, and (4) performs the action and evaluates the entire system/application for making progress toward the original goal [19]. Alternatively, a heuristic evaluation is a more task-free method in which pre-established “rules of thumb” are applied to using a system/application to uncover general issues unrelated to completing a specific action or task [20]. Examples of such heuristics include, but are not limited to, communicating in user’s language, minimizing user memory load, consistency, providing user feedback, clearly marked exits and shortcuts, relevant error messages, and achieving expected criteria [21]. A specific example of the latter is from Demidowich et al. [22] who had two experts review 42 diabetes self-management mobile applications (apps) publicly available on the Android platform as of April 2011. Reviewers graded every app on whether it supported self-monitoring of blood glucose, diabetes medication tracking, prandial insulin calculation, data graphing, data sharing and other data tracking, and the usability of each of these features and found that less than 10 % of Android apps comprehensively supported diabetes self-management [22].
Combining Methodologies
Several included studies combined different usability testing methods to inform fixes and enhancements to the technology-based solution. They are highlighted here to gain a deeper understanding of how usability testing can provide insight into why and how patients choose to engage with a technology-delivered support system/application as part of their everyday lives.
The first example is from Nijland et al. [23••] who conducted a comprehensive usability testing study of their web-based application for diabetes management in the Netherlands. First, this study outlined the recruitment process for their application very clearly, including the number of patients who refused to participate (and their reasons for nonparticipation) as well as detailed information about the final sample who agreed to pilot the application (such as the sample’s self-reported health status and level of education). When assessing participants’ usage of the application over 2 years, the authors also provided specifics about user engagement, identifying subgroups of continuous users (with both high and low levels of activity) vs. those who discontinued use and specifying the use of each application feature (e.g., glucose uploads, emailing with providers) over time. Finally, the authors assessed qualitative data to understand barriers to both initial adoption and sustained use, such as the lack of interest in engaging with diabetes self-management and the desire for more interactivity within the application.
In a similar way, Froisland et al. [24•] combined methodologies to provide a more comprehensive view of the usability of their diabetes mobile phone application for adolescents with diabetes. For their qualitative assessments, they conducted in-depth interviews with participants about their experiences using the application. These interviews uncovered important themes about the graphical displays of personalized health information, the sense of increased access to providers, and technical glitches with the software. To complement these findings, they also collected and reported quantitative data on system usability. They used the system usability scale (SUS), which is a validated scale of 10 statements (e.g., “I found this system easy to use” and “I feel very confident in using the system”) scored from strongly agree to strongly disagree, resulting in a total sum out of 100 [25, 26]. Froisland and colleagues reported a mean SUS of 73 out of 100 among their adolescent participants.
Finally, Ossebaard et al. [27••] combined qualitative assessments (both interviews and focus groups), think aloud, system usage data, and a usability questionnaire to gain a more complete picture of both the functionality of their technology as well as the patients’ perceptions of its usability (i.e., observing them interacting with the system followed by in-depth reflections about their experiences). The authors report detailed scenarios of how users engaged with a diabetes web portal account, such as patterns for how users completed an assigned task and how long it took users to complete it. They also specified how different tasks led to different rates of completion and what proportion of the content verbalized during the think aloud was positive, neutral, and negative across categories of navigation, content, layout, acceptance, satisfaction, and empowerment. In the follow-up interviews and focus groups, the authors were then able to dive deeper into each of these categories to similarly assess the proportion of participants’ positive and negative sentiments about using the portal.
Discussion
There is a limited, but growing, body of literature describing usability testing for technology-enabled diabetes self-management education and support. Most studies assessing usability do so with questionnaire items created for the study and to a lesser degree standardized usability instruments. While questionnaires are a potentially useful starting point for understanding users’ perceptions of ease of use and satisfaction, users’ perceptions may not provide a complete perspective of usability. Specifically, actual user behavior, as measured by system usage, and think aloud, in which users report their understanding/interpretation of each feature/step in use, may provide a more detailed account of users’ behavior and understanding, respectively, than usability or satisfaction questionnaires. Qualitative studies provided additional insights by soliciting participant ideas to improve usability and identifying unanticipated usability challenges. Notably, both qualitative and think aloud methods identified more usability problems with a system/application and user concerns than usability questionnaires alone (Table 2).
Our findings are consistent with a recent review of provider-facing usability testing studies conducted by Yen and Bakken [28], such as the call for a more systematic approach to reporting users’ experiences and the benefit of combining several complementary usability methodologies. Similarly, our findings are consistent with a broader review article by LeRouge and Wickramasinghe that found that virtually no user-centered design studies of diabetes technologies reported on methods used across the entire development spectrum, from planning/feasibility to postrelease [4]. Taken together, these suggest that an overarching framework for user engagement, from design through development to implementation and evaluation, is needed. Such a framework should include standard and validated metrics for distinct aspects of the user experience.
The research using usability questionnaires suggests a need to develop and implement standardized instruments to measure usability across a range of domains. Studies should report norms such that scores can be interpreted across different types of technology-delivered interventions. In particular, existing usability scales such as the SUS [25, 26] or Computer Usability Satisfaction Questionnaire (CUSQ) [29] may not provide sufficient context for understanding which aspects of a solution are functional and/or accessible and which are less useable. Alternatively, system usage data provides more objective feedback about usability, in that, regardless of perceptions, lack of use likely indicates poor usability. The difficulty lies in determining appropriate thresholds for what would constitute “good” or desired system usage. As an example, if a participant takes 3 days to respond to a text message, but responds to each and every message, it is unclear how to interpret usage vis-à-vis usability. Moreover, long-term usage of a technology—as opposed to a pilot trial that is only a few weeks long—provides more indication of sustained patient engagement; yet, it is difficult to conduct lengthy trials in order to report on ongoing use. Finally, expert evaluation such as cognitive walkthrough and heuristic evaluation detected errors of omission, in that experts will be actively seeking relevant features and content that are needed for diabetes self-management—which patients themselves may not be aware of. Therefore, combining these diverse techniques can leverage the strengths and weaknesses of each method and provide more nuanced insight into why and how patients use a technology-delivered intervention, as evidenced in the highlighted studies in our review.
In almost half of the studies included in this review, the authors did not report on detailed characteristics of their participant population, such as educational attainment, health literacy, or self-reported technical knowledge. This can be problematic for disseminating these solutions to larger patient populations, especially if all or most of the participants involved in usability testing had high levels of technical savviness. It is unclear whether the usability of such technologies would then be generalizable to other patient populations. Furthermore, among the studies that did report some specific information about their participants, there is room for increasing the diversity of the participants involved in usability testing. For example, there is a need to understand how those with limited health literacy or lower technical skills interact with the technology—and methods to evaluate new technologies across health literacy levels exist [30, 31]. This is essential, as there is evidence of a digital divide by health literacy [32, 33] and by socioeconomic status in the USA, particularly among older Americans who are more likely to have type 2 diabetes [34]. There is also a growing literature to suggest that diabetes patients from racial/ethnic minority groups are less likely to engage with health technology, even among those who are already existing computer and Internet users [35, 36]. This may suggest that diverse patients need to be more involved in the early design and testing of technology to ensure that the content and format are relevant to broader populations—an area in which usability testing could be particularly impactful. Purposive recruitment by health literacy level and self-reported technical skills are initial strategies to increase the diverse of usability testing participants.
While we conducted a thorough literature review, we were unable to include papers not written in English. Because methods were dissimilar, we were unable to perform a systematic review of all the included articles.
Conclusions
We conclude that each usability testing method confers a distinct advantage. While all technology-delivered interventions should investigate and report on usability, it is critical to perform a robust usability evaluation using combination of methodologies in order to achieve a comprehensive assessment, which would ideally follow an iterative user-centered design process. We believe the field of user engagement, across all phases from design through evaluation, could benefit from a standardized approach and validated metrics for prespecified and distinct aspects of the user experience. We advocate for routine inclusion of open-ended inquiry and qualitative analysis to identify unanticipated user concerns.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bu D, Pan E, Walker J, Adler-Milstein J, Kendrick D, Hook JM, et al. Benefits of information technology-enabled diabetes management. Diabetes Care. 2007;30:1137–42.
Archer E, Groessl EJ, Sui X, McClain AC, Wilcox S, Hand GA, et al. An economic analysis of traditional and technology-based approaches to weight loss. Am J Prev Med. 2012;43:176–82.
Or CK, Tao D. Does the use of consumer health information technology improve outcomes in the patient self-management of diabetes? A meta-analysis and narrative review of randomized controlled trials. Int J Med Inform 2014.
LeRouge C, Wickramasinghe N. A review of user-centered design for diabetes-related consumer health informatics technologies. J Diabetes Sci Technol. 2013;7:1039–56.
Corry MD, Frick TW, Hansen L. User-centered design and usability testing of a Web site: an illustrative case study. Etr & D-Educ Tech Res. 1997;45:65–76.
Schleyer TK, Thyvalikakath TP, Hong J. What is user-centered design? J Am Dent Assoc. 2007;138:1081–2.
Jaspers MW. A comparison of usability methods for testing interactive health technologies: methodological aspects and empirical evidence. Int J Med Inform. 2009;78:340–53.
Napolitano MA, Hayes S, Russo G, Muresu D, Giordano A, Foster GD. Using avatars to model weight loss behaviors: participant attitudes and technology development. J Diabetes Sci Technol. 2013;7:1057–65.
Bus SA, Waaijman R, Nollet F. New monitoring technology to objectively assess adherence to prescribed footwear and assistive devices during ambulatory activity. Arch Phys Med Rehabil. 2012;93:2075–9.
Hazenberg CE, Bus SA, Kottink AI, Bouwmans CA, Schonbach-Spraul AM, van Baal SG. Telemedical home-monitoring of diabetic foot disease using photographic foot imaging—a feasibility study. J Telemed Telecare. 2012;18:32–6.
Morak J, Schwarz M, Hayn D, Schreier G. Feasibility of mHealth and Near Field Communication technology based medication adherence monitoring. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:272–5.
Keith-Hynes P, Guerlain S, Mize B, Hughes-Karvetski C, Khan M, McElwee-Malloy M, et al. DiAs user interface: a patient-centric interface for mobile artificial pancreas systems. J Diabetes Sci Technol. 2013;7:1416–26.
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Britten N, Roen K, Duffy S. Guidance on the conduct of narrative synthesis in systematic reviews. A Product from the ESRC Methods Programme 2006:1–92.
Britto MT, Jimison HB, Munafo JK, Wissman J, Rogers ML, Hersh W. Usability testing finds problems for novice users of pediatric portals. J Am Med Inform Assoc. 2009;16:660–9.
Urowitz S, Wiljer D, Dupak K, Kuehner Z, Leonard K, Lovrics E, et al. Improving diabetes management with a patient portal: a qualitative study of diabetes self-management portal. J Med Internet Res. 2012;14:e158.
Dick JJ, Nundy S, Solomon MC, Bishop KN, Chin MH, Peek ME. Feasibility and usability of a text message-based program for diabetes self-management in an urban African-American population. J Diabetes Sci Technol. 2011;5:1246–54.
Boren MT, Ramey J. Thinking aloud: reconciling theory and practice. IEEE Trans Prof Commun. 2000;43:261–78.
Simon AC, Holleman F, Gude WT, Hoekstra JB, Peute LW, Jaspers MW, et al. Safety and usability evaluation of a web-based insulin self-titration system for patients with type 2 diabetes mellitus. Artif Intell Med. 2013;59:23–31.
Wharton C, Rieman J, Lewis C, Polson P. The cognitive walkthrough method: a practitioner’s guide. In: Usability Inspection Methods. New York: Wiley; 1994. p. 105–41.
Lewis C, Rieman J. Chapter 4. Evaluating the design without users. In Task-centered user interface design: a practical introduction. Online via shareware; 1993, 1994.
Nielsen J, Molich R. Heuristic evaluation of user interfaces. In Proc ACM CHI'90 Conf; April 1–5; Seattle, WA. 1990: 249–256.
Demidowich AP, Lu K, Tamler R, Bloomgarden Z. An evaluation of diabetes self-management applications for Android smartphones. J Telemed Telecare. 2012;18:235–8.
Nijland N, van Gemert-Pijnen JE, Kelders SM, Brandenburg BJ, Seydel ER. Factors influencing the use of a Web-based application for supporting the self-care of patients with type 2 diabetes: a longitudinal study. J Med Internet Res. 2011;13:e71. This study used four usability approaches and collected data on reasons for discontinued use of a website. It only took 20 users to identify 166 unique usability problems, and users attributed a suboptimal user interface and limited interactivity as reasons for discontinued use.
Froisland DH, Arsand E, Skarderud F. Improving diabetes care for young people with type 1 diabetes through visual learning on mobile phones: mixed-methods study. J Med Internet Res. 2012;14:e111. This study illustrates how to conduct a comprehensive qualitative and quantitative usability testing approach to identify technical problems, obtain users’ ideas for improvements, and, in turn, inform further development and testing.
Bangor A, Kortum PT, Miller JT. An empirical evaluation of the System Usability Scale (SUS). Int J Hum Comput Interact. 2008;24:574–94.
Brooke J. SUS: a “quick and dirty” usability scale. In: Jordan PW, Thomas B, Weerdmeester BA, McClelland AL, editors. Usability evaluation in industry. London: Taylor and Francis; 1996.
Ossebaard HC, Seydel ER, van Gemert-Pijnen L. Online usability and patients with long-term conditions: a mixed-methods approach. Int J Med Inform. 2012;81:374–87. This study employed four usability testing approaches, including software that recorded screen action during think aloud sessions. Utilization of a variety of methods uncovered negative user experiences, negative think aloud expressions, incomplete user tasks by most participants, and usability issues pertaining to navigation and non-personalized content that could be improved.
Yen PY, Bakken S. Review of health information technology usability study methodologies. J Am Med Inform Assoc. 2012;19:413–22.
Lewis JR. IBM computer usability satisfaction questionnaires: psychometric evaluation and instructions for use. In Human Factors Group. Boca Raton, FL: IBM Corporation; 1993.
Monkman H, Kushniruk A. A health literacy and usability heuristic evaluation of a mobile consumer health application. Stud Health Technol Inf. 2013;192:724–8.
Broderick J, Devine T, Langhans E, Lemerise AJ, Lier S, Harris L. Designing health literate mobile apps. Washington: Institute of Medicine; 2014.
Chakkalakal RJ, Kripalani S, Schlundt DG, Elasy TA, Osborn CY. Disparities in using technology to access health information: race versus health literacy. Diabetes Care. 2014;37:e53–4.
Sarkar U, Karter AJ, Liu JY, Adler NE, Nguyen R, Lopez A, et al. The literacy divide: health literacy and the use of an internet-based patient portal in an integrated health system—results from The Diabetes Study of Northern California (DISTANCE). J Health Commun. 2010;15 Suppl 2:183–96.
Smith A. Older adults and technology use. Washington: Pew Research Center; 2014.
Lyles CR, Harris LT, Jordan L, Grothaus L, Wehnes L, Reid RJ, et al. Patient race/ethnicity and shared medical record use among diabetes patients. Med Care. 2012;50:434–40.
Sarkar U, Karter AJ, Liu JY, Adler NE, Nguyen R, Lopez A, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc. 2011;18:318–21.
Gude WT, Simon AC, Peute LW, Holleman F, Hoekstra JB, Peek N, et al. Formative usability evaluation of a web-based insulin self-titration system: preliminary results. Stud Health Technol Inf. 2012;180:1209–11.
Jennings A, Powell J, Armstrong N, Sturt J, Dale J. A virtual clinic for diabetes self-management: pilot study. J Med Internet Res. 2009;11:e10.
Nielsen J, Mack RL, editors. Usability inspection methods. New York: Wiley; 1994.
Zayas-Caban T, Marquard JL, Radhakrishnan K, Duffey N, Evernden DL. Scenario-based user testing to guide consumer health informatics design. AMIA Annu Symp Proc. 2009;2009:719–23.
Arsand E, Tatara N, Ostengen G, Hartvigsen G. Mobile phone-based self-management tools for type 2 diabetes: the few touch application. J Diabetes Sci Technol. 2010;4:328–36.
Cafazzo JA, Casselman M, Hamming N, Katzman DK, Palmert MR. Design of an mHealth app for the self-management of adolescent type 1 diabetes: a pilot study. J Med Internet Res. 2012;14:e70.
Carroll AE, DiMeglio LA, Stein S, Marrero DG. Using a cell phone-based glucose monitoring system for adolescent diabetes management. Diabetes Educ. 2011;37:59–66.
Chomutare T, Tatara N, Arsand E, Hartvigsen G. Designing a diabetes mobile application with social network support. Stud Health Technol Inf. 2013;188:58–64.
DeShazo J, Harris L, Turner A, Pratt W. Designing and remotely testing mobile diabetes video games. J Telemed Telecare. 2010;16:378–82.
Garcia-Saez G, Hernando ME, Martinez-Sarriegui I, Rigla M, Torralba V, Brugues E, et al. Architecture of a wireless personal assistant for telemedical diabetes care. Int J Med Inform. 2009;78:391–403.
Mulvaney SA, Anders S, Smith AK, Pittel EJ, Johnson KB. A pilot test of a tailored mobile and web-based diabetes messaging system for adolescents. J Telemed Telecare. 2012;18:115–8.
Osborn CY, Mulvaney SA. Development and feasibility of a text messaging and interactive voice response intervention for low-income, diverse adults with type 2 diabetes mellitus. J Diabetes Sci Technol. 2013;7:612–22.
Padman R, Jaladi S, Kim S, Kumar S, Orbeta P, Rudolph K, et al. An evaluation framework and a pilot study of a mobile platform for diabetes self-management: insights from pediatric users. Stud Health Technol Inf. 2013;192:333–7.
Tani S, Marukami T, Matsuda A, Shindo A, Takemoto K, Inada H. Development of a health management support system for patients with diabetes mellitus at home. J Med Syst. 2010;34:223–8.
Tatara N, Arsand E, Bratteteig T, Hartvigsen G. Usage and perceptions of a mobile self-management application for people with type 2 diabetes: qualitative study of a five-month trial. Stud Health Technol Inf. 2013;192:127–31.
Vuong AM, Huber Jr JC, Bolin JN, Ory MG, Moudouni DM, Helduser J, et al. Factors affecting acceptability and usability of technological approaches to diabetes self-management: a case study. Diabetes Technol Ther. 2012;14:1178–82.
Acknowledgments
Dr. Lyles is supported by a Career Development Award from the Agency for Healthcare Research and Quality (K99 HS022408). Dr. Sarkar is also supported by the Agency for Healthcare Research and Quality (R21 HS021322). Dr. Osborn is supported by a Career Development Award from the National Institute of Diabetes and Digestive and Kidney Diseases (K01 DK087894). The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent these funding entities. We thank Lina Tieu, MPH, for her assistance in reviewing and finalizing the manuscript.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Courtney R. Lyles, Urmimala Sarkar, and Chandra Y. Osborn declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Psychosocial Aspects
Rights and permissions
About this article
Cite this article
Lyles, C.R., Sarkar, U. & Osborn, C.Y. Getting a Technology-Based Diabetes Intervention Ready for Prime Time: a Review of Usability Testing Studies. Curr Diab Rep 14, 534 (2014). https://doi.org/10.1007/s11892-014-0534-9
Published:
DOI: https://doi.org/10.1007/s11892-014-0534-9