Abstract
Gestational diabetes is associated with adverse pregnancy outcomes, increased costs, and long-term risk of type 2 diabetes mellitus (T2DM) in the mother. Observational data have shown an association between reduced weight gain, healthy eating, and physical activity and reduced rates of gestational diabetes mellitus (GDM). Despite this, most randomized controlled trials of lifestyle interventions to prevent GDM have been negative. Dietary approaches appear to be more successful than exercise or a combination of diet and exercise at decreasing GDM. Reasons for negative studies may include lack of power, lack of intervention uptake, and severity of placenta mediated insulin resistance. Future studies should be powered for a reduction in GDM, monitor lifestyle changes closely, and include a psychological component in the intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
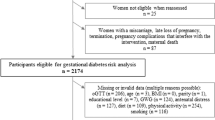
Gestational diabetes mellitus (GDM) refers to the recognition of hyperglycemia for the first time during pregnancy. The reported prevalence has ranged from 8 %–16 % of pregnancies depending on the population studied and the use of different diagnostic criteria [1]. There is a continuous relationship between hyperglycemia and adverse pregnancy outcomes including birth weight over the 90th percentile, primary caesarean section, neonatal hypoglycaemia, premature delivery (before 37 weeks), shoulder dystocia or birth injury, hyperbilirubinemia, and pre-eclampsia [2]. Treatment of hyperglycemia in pregnancy in women with GDM results in a significant reduction in macrosomia and shoulder dystocia [3]. The diagnosis of GDM also has significant long-term implications for women’s health, with 20 % of women developing type 2 diabetes (T2DM) by 10 years postpartum [4]. There also appears to be an increased risk for childhood obesity and subsequent development of T2DM in offspring of women with GDM [5]. In addition, treatment costs are not insignificant. The cost of treating 1 case of GDM is estimated to be \$817/patient for diet-treated patients and up \$3000 for women treated with insulin [6, 7]. This does not take into account the costs of GDM complications such as cesarean section and neonatal intensive care admission, which in Ontario, Canada cost on average \$4000 and \$7000, respectively [8, 9].
Prepregnancy overweight, and obesity and excessive gestational weight gain are 2 modifiable risk factors for gestational diabetes and other adverse pregnancy outcomes [10, 11]. Pregnancy represents an opportunity for prevention for women at risk for GDM and subsequent T2DM because women may be more likely to prioritize their own health when it can affect their unborn child. Prevention of GDM with lifestyle modification is attractive as the benefits may extend beyond the pregnancy to help reduce the risk of T2DM and cardiovascular disease in the long term. In this review, we will first examine the epidemiologic data linking healthy lifestyle choices to reduced risk of GDM and then compare this with the interventional trials of diet and exercise to prevent GDM. We will offer explanations for the discordant results of observational and interventional data and make recommendations for future study.
The Link between Weight, Diet, Exercise, and GDM: Observational Studies
The presence of overweight or obesity is a well-accepted risk factor for insulin resistance and dysglycemia. A case control study examined the effects of prepregnancy body mass index (BMI) on incident GDM and found that for each 1 kg/m2 increase of BMI the odds ratio (OR) of developing GDM was 1.08 (95 % confidence interval [CI] 1.08–1.09) and for each 5 kg/m2 increase, the OR was 1.48 (95 % CI 1.45–1.51) [12]. In examining the risk of repeat GDM in a second pregnancy in women who were overweight or obese in their first pregnancy, the loss of more than 2 BMI points (approximately 6 pounds for the average height of 5 foot 4) decreased subsequent GDM risk by 74 % (OR 0.26 95 % CI 0.14–0.47); and increases in the BMI by 2 units resulted in a doubling of the risk of GDM (OR 2.11 95 % CI 2.11–2.84) [13]. A study from Korea retrospectively examined weight gain in women with GDM according to the institute of medicine gestational weight gain guidelines. In those with inadequate weight gain based on the guidelines (average 2.4 kg), there was significantly fewer women needing insulin treatment (P = 0.032) and lower rates of macrosomia (P = 0.005) compared with those who had excessive weight gain (average 13.8 kg) [14].
Using data from the Nurses Health Study II cohort (1991–2001), researchers have shown that higher prepregnancy intakes of animal fat and cholesterol were associated with elevated GDM risk (RR 1.88 95 % CI 1.36, 2.60) [15]. Healthy eating patterns including the alternate Mediterranean Diet (aMED), Dietary Approaches to Stop Hypertension (DASH), and alternate Healthy Eating Index (aHEI), have been inversely associated with type 2 diabetes risk among nonpregnant individuals. Using the same Nurses Health Study cohort, these healthy eating patterns were shown to be protective for GDM (aMED RR: 0.76; 95 % CI 0.60, 0.95, DASH RR: 0.66; 95 % CI 0.53, 0.82, and aHEI RR: 0.54; 95 % CI 0.43, 0.68) [16]. In these studies, the relative risk was adjusted for pre-pregnancy BMI.
In a systematic review and meta-analysis of observational studies prepregnancy physical activity was associated with a lower risk of GDM; OR of 0.45 (95 % CI 0.28–0.75) when the highest vs lowest levels of activity were compared. Exercise in early pregnancy was also associated with a lower risk of GDM, and was also significantly protective (OR 0.76 [95 % CI 0.70–0.83]) [17]. There was significant heterogeneity with-in the pooled studies (Cochrane Q = 32.6, P < 0.001). Exercise was based on self-report, and there was no adjustment for BMI as a possible confounder, limiting the validity of these results.
Lifestyle Based Interventions for the Prevention of GDM
Exercise in Pregnancy
A 2012 Cochrane meta-analysis of 5 randomized controlled trials with a total of 1115 women assessed the impact of exercise during pregnancy on insulin resistance and GDM [18•]. All 5 trials were deemed to be at moderate risk of bias. When comparing women receiving exercise interventions with those having routine antenatal care, there was no significant difference in GDM incidence (3 trials, 826 women, risk ratio (RR) 1.10, 95 CI 0.66 to 1.84). Of note the types of exercise programs, adherence, and baseline BMIs were quite variable across the studies (Table 1). Four of the studies looked at various measures of insulin resistance [19–22], and none showed a significant improvement in those exposed to exercise in pregnancy.
Nutritional Interventions in Pregnancy
There have been many recent meta-analyses of RCTs assessing the impact of lifestyle interventions in pregnancy on gestational weight gain (GWG) and obstetrical outcomes [23•, 24•, 25•, 26•]. We included meta-analyses of excess GWG as it has been linked to GDM in observational studies; it was hypothesized that studies aimed at decreasing GWG may show an impact on GDM incidence. The sample sizes, baseline BMIs, types of interventions, definitions of GDM, and reporting of GDM varied significantly across the primary studies. Table 2 outlines the 13 studies of diet and physical activity in pregnancy used in the 4 systematic reviews. Three studies were included in all 4 meta-analyses [27–29]; 2 studies were included in 3 of the meta-analyses [30, 31]; and1 study was included twice [32••]. The variation in included studies is because the systematic reviews had different inclusion criteria and were published over a few years; only 1 of the 5 meta-analyses had GDM as its primary outcome [26•].
Thangaratinam et al. [24•] performed a meta-analysis of 44 RCTs assessed the impact of lifestyle interventions in pregnancy on maternal weight gain and an array of obstetric outcomes. The authors classified the interventions as being diet alone; physical activity alone, or mixed. Three eligible studies [28, 29, 32••] of diet alone reported on GDM. For 409 overweight or obese pregnant women, a dietary intervention resulted in a pooled OR of 0.39 (95 % CI 0.23–069, P = 0.001) for developing GDM. Six studies of multicomponent diet and physical activity based interventions were pooled for a total of 1233 women of various weight categories. The pooled OR for GDM was 1.18 (95 % CI 0.78–1.77). In these studies adherence with the intervention was not explicitly stated; however, in 4 of the studies [27, 30, 31, 33] GWG was not significantly reduced in the intervention groups indicating poor fidelity of the intervention.
Tanentsapf et al. [23•] pooled 13 randomized controlled trials of nutritional interventions to prevent excessive GWG to normal, overweight, and obese pregnant women. The interventions themselves were heterogeneous with some including both nutritional counseling and physical activity; some including a motivational component and others focusing only on total calories consumed. Overall, there was a significant decrease in GWG (n = 1434; WMD = −1.92 kg; 95 % CI −3.65/-0.19; P = 0.03); however, in the 6 studies that assessed the incidence of GDM, there was no significant reduction (n = 886; WMD = 0.74 95 % CI 0.52–1.06).
The meta-analysis conducted by Oteng-Ntim et al. [25•] included only studies in overweight and obese women; it concluded that antenatal dietary and lifestyle intervention reduced maternal pregnancy weight gain (10 RCTs, n = 1228; -2.21 kg (95 % CI −2.86 kg to −1.59 kg)) and showed a trend toward a reduction in the prevalence of gestational diabetes (6 RCTs; n = 1011; odds ratio 0.80 (95 % CI 0.58–1.10)) [25•].
Oostdam et al. [26•] designed a meta-analysis to look at all interventions (diet, metformin, and exercise) for preventing GDM. Seven pooled studies showed that dietary counseling is more effective than usual care in reducing the risk of GDM (n = 813, risk difference −0.05, 95 % CI −0.1 to 0.01). However, the authors cautioned that the evidence was of low quality and none of the studies independently showed a significant reduction of GDM. In this study, metformin and exercise showed no significant reduction in GDM incidence.
The meta-analyses by Thangaratinam and Oteng-Ntim [24•, 25•], both included the only RCT to show a significant reduction in GDM incidence. Women attended a study- specific antenatal clinic providing continuity of care, weight on arrival, brief dietary intervention by food technologist, and psychological assessment and intervention if indicated. This study of 132 women showed a 50 % reduction in GWG in the intervention group (7.0 vs 13.8 kg (P < 0.0001) and statistically significant reduction in GDM incidence (6 % vs 29 %, OR 0.17 (95 % CI 0.03–0.95, P = 0.04) [32••].
Explanation for Poor Results of RCTs to Prevent GDM
The observational literature supports a positive relationship between prepregnancy BMI, excess gestational weight gain, and GDM [12–14]; however, the RCTs that aimed to decrease GWG had conflicting results. Even in those that managed to have a significant impact on GWG, only1 showed a significant decrease in incident GDM [34]. The meta-analysis of physical exercise RCTs failed to show an association between physical activity and GDM [18•]. The meta-analysis of dietary interventions showed a small improvement in GDM incidence [24•, 26•]; however, those of mixed diet and exercise interventions did not show a significant improvement in GDM incidence [23•, 24•, 25•]. There are a few possible explanations for the conflicting results of observational data, individual RCTs, and meta-analyses.
The first possible explanation for the negative trials is that there is a confounding factor in the observational literature that is accounted for by randomization. The most likely confounding factor in studies of weight gain and exercise in pregnancy is that of BMI. That is, women who exercise less and gain more weight in pregnancy are more likely to be overweight to begin with and, thus, have an increased risk of GDM. Through randomization and stratification the prevalence of overweight and obesity is split evenly in the control and intervention group, thereby accounting for this confounding variable.
The second possible explanation is that the studies were underpowered to detect changes in GDM. The majority of these studies had sample sizes of 50–100 and if a sample size calculation was done at all, it was done for the primary outcome of GWG. The meta-analysis by Oostdam was able to overcome the sample size limitation by pooling 7 small studies of dietary intervention and show a significant, although clinically small, risk reduction in GDM [26•].
A third possible explanation is poor adherence with the intervention. Uptake of lifestyle interventions is usually low, as behavioral modification is much more difficult than merely taking a pill. In pregnancy, women face additional barriers to physical activity and healthy eating including physical discomfort from nausea, fatigue, shortness of breath, heartburn, leg cramps, and body soreness. Another commonly reported prenatal barrier to behavioural modification is a perceived lack of time, especially due to childcare commitments [34]. In the studies focused on physical activity, adherence with the intervention was on average 76 % (range 55 %–94 %); however, exercise alone is not likely enough to alter the profound insulin resistance of pregnancy. In fact, the sub-division of studies based on exercise, diet, or mixed intervention showed that diet alone was most effective at limiting GWG and preventing obstetrical complications [24•, 26•].
The studies that reported on diet and activity based interventions did not explicitly report adherence with the intervention, likely because they were not able to accurately track women’s compliance with dietary advice. In these studies, however, GWG was almost always reported and this is a good surrogate for uptake of the intervention. Many of the studies were not able to limit GWG and in some, there was even a paradoxical excessive weight gain in the overweight and obese groups [27, 30]. In the studies that did limit GWG [28, 29, 34, 37–39] the differences in GDM between intervention and control groups ranged from −1 %–25 %. The Oostdam meta-analysis that showed a significant decreased in GDM incidence and included diet only interventions included some studies that showed a decreases in GWG [28, 29, 31]; some that did not show an improvement in GWG [27, 35]; and some that did not report GWG [36, 37]. Thus, the evidence to date challenges the notion that limiting GWG will reliably decrease incident GDM.
The fourth possible explanation for poor outcomes with lifestyle interventions is that placenta mediated insulin resistance is too severe to overcome with lifestyle interventions alone. Most of the physical activity intervention trials have looked at impact of exercise on insulin resistance using various techniques (HOMA-IR, IV Glucose Tolerance Test, 75gOGTT with area under the curve (AUC) for glucose and insulin). Regardless of the type of technique used none of the studies showed a significant difference in insulin resistance in those exposed to an exercise intervention [19–22]. It is likely that diet is more effective than physical activity at managing the insulin resistance of pregnancy as 2 meta-analysis of dietary interventions did show a reduction in GDM [24•, 26•], but across all the studies the effect of limiting GWG on incident GDM was inconsistent.
Suggestions for Future Research
Despite well-described interventions, it is difficult to tease out what the “active” ingredients of a successful lifestyle program in pregnancy should include. Some, but not all, of the previous research has shown that lifestyle interventions can minimize gestational weight gain. A search of clinicaltrials.gov revealed 14 studies of lifestyle interventions in pregnancies that are currently recruiting. In all 14 studies, the primary outcome is GWG; none have been powered to detect incidence of GDM. It is likely the results of these studies will be similar to those already published, providing little additional knowledge on how best to prevent GDM.
Future research should be directed at replicating the intervention in Quinliavan et al. [32••] that included a specific antenatal clinic for women who were overweight and obese with dietician and psychology support. The study should be large enough to have the power to show a difference in the incidence of GDM. In addition, more attention should be paid to monitoring adherence with the intervention. If this intervention is successful in different environments and different populations of patients then guideline developers and policy makers could make evidence based recommendations in support of specialized clinics for the management of obesity in pregnancy.
Conclusions
Obesity is a rising concern in women of reproductive age. Lifestyle interventions introduced in pregnancy have the potential to prevent the development of GDM and other complications. The observational literature supports a link between unhealthy lifestyle habits, obesity, and GDM. Thus far, most trials of lifestyle interventions to prevent GDM have been negative. However, these trials were not powered to detect difference in GDM. Physicians should continue to recommend against excessive weight gain in pregnancy as it has been associated with large for gestational age neonates, nonelective Cesarean section, and post-partum weight retention [38, 39]. At this time, however, there is insufficient evidence to recommend for a specific lifestyle program to prevent GDM.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
International Association of Diabetes and Pregnancy study groups’ recommendations on the diagnosis and classification of hyperglycemia in pregnancy 2010–03. 2013;33:676+.
HAPO Study Cooperative Research Group. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;35:e1991–2002.
Horvath K, Koch K, Jeitler K, Matyas E, Bender R, Bastian H, et al. Effects of treatment in women with gestational diabetes mellitus: systematic review and meta-analysis. BMJ. 2010;340:1395.
Feig DS, Zinman B, Wang X, Hux JE. Risk of development of diabetes mellitus after diagnosis of gestational diabetes. CMAJ. 2008;179:229–34.
Dabelea D, Knowler WC, Pettitt DJ. Effect of diabetes in pregnancy on offspring: follow-up research in the Pima Indians. J Matern Fetal. 2000;9:83–8.
Kitzmiller JL. Cost analysis of diagnosis and treatment of gestational diabetes mellitus. Clin Obstet Gynecol. 2000;43:140–53.
Moss JR, Crowther CA, Hiller JE, Willson KJ, Robinson JS. Australian Carbohydrate Intolerance Study in Pregnant Women Group. Costs and consequences of treatment for mild gestational diabetes mellitus - evaluation from the ACHOIS randomized trial. BMC Pregnancy Childbirth. 2007;7:27.
Fallah S, Chen X-K, Lefebrve D. Babies admitted to NICU/ICU: province of birth and mode of delivery matter. Healthc Q. 2011;14:16–20.
Canadian Institute for Health Information. The costs of giving birth in Canada. Canadian Institute for Health Information. Available at: http://publicationsgc.ca/collections/Collection/H118-38-2006E pdf. Accessed 15 May 2013.
Chung JH, Melsop KA, Gilbert WM, Caughey AB, Walker CK, Main EK. Increasing pre-pregnancy body mass index is predictive of a progressive escalation in adverse pregnancy outcomes. J Matern Fetal Neonatal Med. 2012;25:1635–9.
Mamun AA, Callaway LK, O’Callaghan MJ, Williams GM, Najman JM, Alati R, et al. Associations of maternal pre-pregnancy obesity and excess pregnancy weight gains with adverse pregnancy outcomes and length of hospital stay. BMC Pregnancy Childbirth. 2011;11:62.
Singh J, Huang CC, Driggers RW, Timofeev J, Amini D, Landy HJ, et al. The impact of pre-pregnancy body mass index on the risk of gestational diabetes. J Matern Fetal Neonatal Med. 2012;25:5–10.
Ehrlich SF, Hedderson MM, Feng J, Davenport ER, Gunderson EP, Ferrara A. Change in body mass index between pregnancies and the risk of gestational diabetes in a second pregnancy. Obstet Gynecol. 2011;117:1323–30.
Park JE, Park S, Daily JW, Kim SH. Low gestational weight gain improves infant and maternal pregnancy outcomes in overweight and obese Korean women with gestational diabetes mellitus. Gynecol Endocrinol. 2011;27:775–81.
Bowers K, Tobias DK, Yeung E, Hu FB, Zhang C. A prospective study of prepregnancy dietary fat intake and risk of gestational diabetes. Am J Clin Nutr. 2012;95:446–53.
Tobias DK, Zhang C, Chavarro J, Bowers K, Rich-Edwards J, Rosner B, et al. Prepregnancy adherence to dietary patterns and lower risk of gestational diabetes mellitus. Am J Clin Nutr. 2012;96:289–95.
Tobias DK, Zhang C, van Dam RM, Bowers K, Hu FB. Physical activity before and during pregnancy and risk of gestational diabetes mellitus: a meta-analysis. Diabetes Care. 2011;34:223–9.
• Han S, Middleton P, Crowther CA. Exercise for pregnant women for preventing gestational diabetes mellitus. Cochrane Database Syst Rev. 2012;7:009021. A well done meta-analysis of exercise for the prevention of gestational diabetes. Exercise in addition to standard prenatal care did not reduce weight gain, GDM, Cesarean Section, or operative vaginal birth.
Callaway LK, Colditz PB, Byrne NM, Lingwood BE, Rowlands IJ, Foxcroft K, et al. Prevention of gestational diabetes: feasibility issues for an exercise intervention in obese pregnant women. Diabetes Care. 2010;33:1457–9.
Ong MJ, Guelfi KJ, Hunter T, Wallman KE, Fournier PA, Newnham JP. Supervised home-based exercise may attenuate the decline of glucose tolerance in obese pregnant women. Diabetes Metab. 2009;35:418–21.
Hopkins SA, Baldi JC, Cutfield WS, McCowan L, Hofman PL. Exercise training in pregnancy reduces offspring size without changes in maternal insulin sensitivity. J Clin Endocrinol Metabol. 2010;95:2080–8.
Stafne SN, Salvesen KA, Romundstad PR, Eggebo TM, Carlsen SM, Morkved S. Regular exercise during pregnancy to prevent gestational diabetes: a randomized controlled trial. Obstet Gynecol. 2012;119:29–36.
• Tanentsapf I, Heitmann BL, Adegboye AR. Systematic review of clinical trials on dietary interventions to prevent excessive weight gain during pregnancy among normal weight, overweight and obese women. BMC Pregnancy Childbirth. 2011;11:81. The primary outcome of this meta-analysis was gestational weight gain and the results were significant (1.92 kg less weight gain in the lifestyle group). Five studies were pooled for the outcome of GDM, and there was no significant effect.
• Thangaratinam S, Rogozinska E, Jolly K, Glinkowski S, Duda W, Borowiack E, et al. Interventions to reduce or prevent obesity in pregnant women: a systematic review. Health Technol Assess. 2012;16(31):iii-iv, 1–191. doi:10.3310/hta16310. Three studies of diet alone were pooled and showed a RR of 0.39 for GDM. Six studies of diet and exercise did not have a significant effect on GDM.
• Oteng-Ntim E, Varma R, Croker H, Poston L, Doyle P. Lifestyle interventions for overweight and obese pregnant women to improve pregnancy outcome: systematic review and meta-analysis. BMC Med. 2012;10:47. Focused only on studies of overweight and obese women. Lifestyle interventions reduced gestational weight gain but did not significantly reduce GDM.
• Oostdam N, van Poppel MN, Wouters MG, van Mechelen W. Interventions for preventing gestational diabetes mellitus: a systematic review and meta-analysis. J Womens Health. 2011;20:1551–63. Seven studies of diet alone when pooled showed a significant decrease in GDM. Authors cautioned the studies were all of poor quality.
Polley BA, Wing RR, Sims CJ. Randomized controlled trial to prevent excessive weight gain in pregnant women. Int J Obes Relat Metab Disord. 2002;26:1494–502.
Wolff S, Legarth J, Vangsgaard K, Toubro S, Astrup A. A randomized trial of the effects of dietary counseling on gestational weight gain and glucose metabolism in obese pregnant women. Int J Obes. 2008;32:495–501.
Thornton YS, Smarkola C, Kopacz SM, Ishoof SB. Perinatal outcomes in nutritionally monitored obese pregnant women: a randomized clinical trial. J Natl Med Assoc. 2009;101:569–77.
Phelan S, Phipps MG, Abrams B, Darroch F, Schaffner A, Wing RR. Randomized trial of a behavioral intervention to prevent excessive gestational weight gain: the fit for delivery study. Am J Clin Nutr. 2011;93:772–9.
Hui AL, Ludwig SM, Gardiner P, Sevenhuysen G, Murray R, Morris M, et al. Community-based excercise and dietary intervention during<br />pregnancy: a pilot study. Can J Diabetes. 2006;30:169–75.
•• Quinlivan JA, Lam LT, Fisher J. A randomized trial of a 4-step multidisciplinary approach to the antenatal care of obese pregnant women. Aust N Z J Obstet Gynaecol. 2011;51:141–6. Only RCT to show a significant effect on GDM. Was specifically powered for GDM and included a psychological component to the intervention. Future research should focus on replicating this intervention in other environments.
Jeffries K, Shub A, Walker SP, Hiscock R, Permezel M. Reducing excessive weight gain in pregnancy: a randomized controlled trial. Med J Aust. 2009;191:429–33.
Downs DS, Chasan-Taber L, Evenson KR, Leiferman J, Yeo S. Physical activity and pregnancy: past and present evidence and future recommendations. Res Q Exerc Sport. 2012;83:485–502.
Guelinckx I, Devlieger R, Mullie P, Vansant G. Effect of lifestyle intervention on dietary habits, physical activity, and gestational weight gain in obese pregnant women: a randomized controlled trial. Am J Clin Nutr. 2010;91:373–80.
Fraser RB, Ford FA, Milner RD. A controlled trial of a high dietary fibre intake in pregnancy—effects on plasma glucose and insulin levels. Diabetologia. 1983;25:238–41.
Laitinen K, Poussa T, Isolauri E. Nutrition, Allergy,Mucosal Immunology and Intestinal Microbiota Group. Probiotics and dietary counseling contribute to glucose regulation during and after pregnancy: a randomized controlled trial. Br J Nutr. 2009;101:1679–87.
Siega-Riz AM, Viswanathan M, Moos MK, Deierlein A, Mumford S, Knaack J, et al. A systematic review of outcomes of maternal weight gain according to the institute of medicine recommendations: birthweight, fetal growth, and postpartum weight retention. Am J Obstet Gynecol. 2009;201:339.e1–14.
Viswanathan M, Siega-Riz AM, Moos MK, Deierlein A, Mumford S, Knaack J, et al. Outcomes of maternal weight gain. Evid Rep Technol Assess. 2008;168:1–223.
Barakat R, Cordero Y, Coteron J, Luaces M, Montejo R. Exercise during pregnancy improves maternal glucose screen at 24–28 weeks: a randomized controlled trial. Br J Sports Med. 2012;46:656–61.
Hui A, Back L, Ludwig S, Gardiner P, Sevenhuysen G, Dean H, et al. Lifestyle intervention on diet and exercise reduced excessive gestational weight gain in pregnant women under a randomized controlled trial. BJOG. 2012;119:70–7.
Vinter CA, Jensen DM, Ovesen P, Beck-Nielsen H, Jorgensen JS. The LiP (lifestyle in pregnancy) study: a randomized controlled trial of lifestyle intervention in 360 obese pregnant women. Diabetes Care. 2011;34:2502–7.
Compliance with Ethics Guidelines
Conflict of Interest
Ilana J. Halperin declares that she has no conflict of interest. Denice S. Feig declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Diabetes and Pregnancy
Rights and permissions
About this article
Cite this article
Halperin, I.J., Feig, D.S. The Role of Lifestyle Interventions in the Prevention of Gestational Diabetes. Curr Diab Rep 14, 452 (2014). https://doi.org/10.1007/s11892-013-0452-2
Published:
DOI: https://doi.org/10.1007/s11892-013-0452-2