Abstract
New proposals for the diagnosis of gestational diabetes (GDM), promulgated by the International Association of Diabetes and Pregnancy Study Groups (IADPSG), will substantially increase the number of women diagnosed with GDM. This will have an enormous impact on healthcare resources, diverting attention away from genuinely high risk diabetic pregnancies. Randomized trials in ‘mild’ GDM indicate that the main effects of treatment are a 2 %–3 % reduction in birth weight, fewer ‘big babies’, and less shoulder dystocia. However, these studies used different diagnostic criteria, and women diagnosed by the broader IADPSG criteria may not derive the same modest benefit. Modeling indicates a very high cost per QALY, unless later development of type 2 diabetes can be prevented. Far from producing consensus, the IADPSG suggestion has thrown sharply into focus the need to assess critically the risks, costs and benefits of adopting criteria that may pathologize a large number of otherwise normal pregnancies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since its first description, nearly 50 years ago, gestational diabetes (GDM) has been surrounded in controversy over its significance, how it should be diagnosed, and if it should be treated. The Hyperglycemia and Pregnancy Outcomes (HAPO) study examined the relationship between maternal glycemia and various pregnancy outcomes, aiming to provide some definitive answers to the first 2 of these questions [1•]. Two recent large randomized controlled trials of treatment of GDM have attempted to provide answers to the last [2•, 3•]. One might then imagine that controversy has now subsided and consensus reached. We will argue that this is far from the case, and that the recent research has not resolved many of the basic questions and contradictions raised 2 decades ago by Jarrett [4] and Ales and Santini [5].
In 2010, the IADPSG proposed universal screening and new diagnostic criteria that would result in nearly 1 in 5 pregnancies being classified as GDM [6•]. Although this proposal has been endorsed by the American Diabetes Association (ADA) [7•], we and others have expressed our concerns that these recommendations are not evidence-based and may cause more harm than good [8–11]. This paper provides a counterpoint to what we believe is an unjustified change of practice.
Gestational Diabetes: the Definition
GDM is currently defined as ‘any degree of glucose intolerance with onset or first recognition during pregnancy’. Excluding those with previously undiagnosed diabetes or very high blood glucose, GDM is not ‘a disease’ but a laboratory finding that reflects some disturbance in glucose metabolism. It should then be considered as a risk factor, but a risk factor for what?
The first diagnostic criteria proposed by O’Sullivan in 1964 were not based on pregnancy outcomes but on the maternal risk of developing type 2 diabetes. The many different criteria now in use are either derived from these studies or are the same as those used in non-pregnant individuals. The ensuing confusion has hampered research and evidence-based clinical care, so consensus would surely be welcome. The new recommendations from the IADPSG attempt to redefine GDM in terms of adverse pregnancy outcomes. While the aim seems sound, crucial steps must be taken before such a change can be implemented. Let us first review the evidence on which the IADPSG based their decision.
The HAPO Study
The HAPO study [1•] was an observational study designed to determine the impact of varying degrees of maternal glycemia less severe than overt diabetes on a number of pregnancy outcomes. The strengths of the study include its very large size (nearly 25,000 pregnant women took part) and its international scope (15 centers from 9 countries). All women with a fasting blood glucose ≤5.8 mmol/L and 2 h values up to 11.1 mmol/L on a 75 g oral glucose tolerance test (OGTT) performed at 24–32 weeks’ gestation (mean 28 weeks) were included. Clinicians were blinded as to the result of the OGTT.
Investigators were hoping to find an inflection point beyond which maternal and fetal risks clearly increased, in the same manner that type 2 diabetes was defined as a particular glycemic threshold above which the risk of retinopathy increases sharply. Instead, they found a continuous, independent relationship between untreated maternal blood glucose (both fasting, 1 h and 2 h post glucose load) and the 4 components of their primary endpoints (namely birth weight and cord-blood serum C-peptide level >90th percentile for gestational age, primary cesarean section, and neonatal hypoglycemia). The cord blood C-peptide level showed the strongest association with maternal blood glucose. Even though neonatal anthropometrics suggest it is related to neonatal adiposity [12], C-peptide is only a surrogate measure without proven long-term clinical significance. The association between maternal blood glucose and neonatal hypoglycemia almost disappeared when maternal characteristics such as body mass index (BMI), were taken into account. As for the need for primary cesarean section, its relationship with blood sugar was weak, and also significantly confounded by maternal obesity. Further analysis of HAPO data suggests that birth weight, cesarean section rate, and pre-eclampsia were more strongly associated with maternal BMI than with the degree of maternal glycemia [13], although there was an interaction effect [14].
Importantly, the HAPO study showed no association between perinatal mortality and higher blood glucose levels within this range. A number of other neonatal morbidities defined as secondary endpoints (shoulder dystocia, premature delivery, hyperbilirubinemia, and pre-eclampsia) also demonstrated linear, but weak, associations with higher blood glucose (the strongest being with pre-eclampsia) but such complications were infrequent. Admissions to neonatal special care facilities were also related to blood glucose levels, but there was a striking ten-fold between-center variation, suggesting that local practice largely determined this particular outcome. Previous GDM, previous macrosomia and maternal gestational weight gain were not reported in the HAPO study
Overall, the only conclusion that the authors of HAPO published in their original New England Journal of Medicine abstract was that there were ‘strong, continuous associations of maternal glucose levels below those diagnostic of diabetes with increased birth weight and increased cord-blood serum C-peptide levels’. These outcomes are not hard clinical events, but risk factors for perinatal adverse outcomes. Because of the observational nature of the HAPO study, it cannot be assumed that treatment can reverse these outcomes.
The Intervention Trials
Two high profile randomized controlled trials (RCTs) of detection and treatment of GDM have been published in recent years: the Australian Carbohydrate Intolerance Study in Pregnant Women (ACHOIS) and the Maternal Fetal Medicines Unit Network (MFMU) study [2•, 3•]. It is important to understand what these studies actually showed and how GDM was diagnosed and treated (details are given in the Table 1). Unlike HAPO, both studies excluded women with prior GDM. Both studies used a 2-step diagnostic procedure but with different diagnostic criteria. The MFMU study excluded women with fasting blood glucose (FBG) values >5.3 mmol/l so the participants were less hyperglycemic than those of the ACHOIS cohort. Accordingly, fewer women in the active treatment group were treated with insulin in the MFMU than in the ACHOIS trials (8 % vs 20 %).
Both studies used composite endpoints as their primary outcome measure (a number of different events were counted together because too great a sample size would be required to demonstrate an effect on individual components). In the MFMU trial [3•], there were no differences between the groups in the composite primary outcome score so the trial indeed produced a clear negative result. Significant results regarding secondary outcomes should then be regarded as ‘exploratory,’ because the sample size and power were calculated and the errors controlled for the primary outcomes only (except for LGA infants). In the ACHOIS study [2•], the composite primary outcome of ‘any serious perinatal complication’ was more frequent (4 % vs 1 %) in the routine-care group. The significance of this difference was critically dependent on the high number of perinatal deaths (5 deaths, or 1 %, vs 0 %) and shoulder dystocia (16 vs 7 or 3.2 % vs 1.4 %, see Table 1) in the routine-care group. However, some of the deaths could not plausibly be attributed to the non-treatment of GDM; for example, one infant had a lethal congenital anomaly, another had severe intrauterine growth retardation. The authors themselves acknowledged the lack of evidence that perinatal mortality is increased in mild GDM; and indeed there was no increase in perinatal mortality in either the HAPO study or MFMU trial [1•, 3]. The authors of the ACHOIS trial calculated a NNT (number-needed-to-treat) of 34 to prevent one ‘any serious perinatal complication’ but a NNH (number-needed-to-harm) of 11 for induction of labor or admission to neonatal nursery [2•]. Although the difference was not statistically significant, more neonates suffered hypoglycemia requiring treatment with intravenous glucose and/or respiratory distress syndrome (RDS) in the ACHOIS intervention group (62 vs 46). Neither study provided data demonstrating that the incidence of the adverse outcome composite was related to glycemic control; either at the time of diagnosis of GDM, or attained on treatment.
In both trials, maternal weight gain was less (by about 2 kg) in the intervention groups, LGA and/or macrosomic babies were reduced by half while mean birth weight was significantly lower (by 140 g in the ACHOIS trial and 100 g in the MFMU trial). About a third of this was estimated to be due to lower fat mass [3•]. In the intervention groups, the incidence both of shoulder dystocia and pregnancy-associated hypertension was lower by about 33 %. The cesarean section rate was unchanged in ACHOIS, but lower in the MFMU intervention group (27 % vs 34 %).
A recent meta-analysis of the treatment RCTs (including, and dominated by, the ACHOIS and MFMU trials) concluded that the only pregnancy outcomes affected by detection and treatment GDM are a reduction in macrosomia (OR 0.38; 95 % CI 0.30–0.49), large-for-gestational age (LGA) infants (OR 0.48; 95 % CI 0.38–0.62) and the incidence of shoulder dystocia (OR 0.40; 95 % CI 0.21–0.75) [15•].
In summary, the intervention trials in GDM confirmed that treatment makes babies 2 %–3 % lighter, leading to a lower incidence of ‘big babies’ and shoulder dystocia. An effect of treatment on pregnancy-associated hypertension was also seen, but it is not known if this can be attributed to lower glycemia or to less maternal weight gain.
The IADPSG Proposal
In 2010, the IADPSG, a group of experts that included several of the HAPO investigators, advocated 2 significant changes to the diagnostic strategy for GDM [6•]. The first is that women with significant risk factors should be screened for unrecognized type 2 diabetes in early pregnancy. Such pregnancies are at increased risk of major congenital anomalies and perinatal mortality [16, 17], so this is a sensible recommendation.
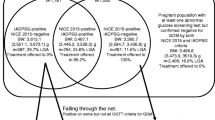
More controversial is the recommendation that all women not previously diagnosed with diabetes should undergo screening for GDM with a 75 g OGTT at 24–28 weeks. GDM is to be diagnosed if any one of the 3 blood glucose results reaches specified levels (fasting ≥5.1; 1 h ≥10.0; 2 h ≥8.5 mmol/l). By increasing the number of women tested, lowering the diagnostic thresholds, and requiring only 1 abnormal result (instead of 2) for diagnosis, this proposal would, in most countries, result in a 2- to 3-fold increase of GDM prevalence. In a cohort such as that of the HAPO study, 18 % of women would have been diagnosed with GDM according to the IADPSG criteria.
The Diagnostic Test
An important principle of any screening program is that the diagnostic test to be used should be robust, reproducible, and define a high risk group with precision. Plasma glucose levels after an OGTT vary considerably – with a CV of up to 20 %. This concern was one of the main motives in the move away from using the OGTT to diagnose diabetes outside pregnancy [18]. Pregnancy is no exception - as illustrated in studies that have looked at the results of women having two 100 g OGTTs at short intervals (with 2 elevated glucose results out of 4 required to diagnose GDM). Nearly a quarter of women changed diagnostic category on the second test–with a similar number going from abnormal to normal as the other way round [19, 20]. Reliance on a single blood glucose result in a 1-step screening test, especially using lower thresholds, will have even poorer precision. An advantage of the widely used 2-step test (non-fasting 50 g glucose challenge, followed, if positive, by a fasting OGTT) is that women have to ‘fail’ 2 tests to be diagnosed with GDM, so one can be more confident that indeed they have significant glucose intolerance. The proposed 1-step test, while administratively more convenient, loses this discriminating power. Recent data from individual centers participating in the HAPO study suggests that the IADPSG-recommended test performs quite variably, and may identify different populations. For example, only 25 % of cases in the Thailand and Hong Kong centers were diagnosed on the basis of an elevated fasting glucose level in contrast to 63 %–73 % of cases in North American centers [21].
The Diagnostic Threshold
The new diagnostic glucose thresholds suggested by the IADPSG correspond to the fifth of the seven glucose categories defined in the HAPO study [1•]. These values were arbitrarily chosen and represent the average OGTT glucose values at which odds ratios (OR) for big and hyperinsulinemic babies in HAPO were ≥1.75 vs cohort mean glucose values. Of note, this OR of 1.75 only applies to 3 surrogate outcomes, namely >90th percentile for birth weight, cord C-peptide, and percent body fat. ORs for meaningful clinical events were more modest, ranging from 0.99 to 1.57. Practically, this means that the IADPSG proposal redefines GDM as a risk factor for having a surrogate marker for adverse pregnancy outcomes (ie, GDM women are ‘at risk of being at risk’ for an event!). Having a big baby is not in itself a clinical event; macrosomia was indeed described by the US Preventive Services Task Force as ‘not an outcome of primary interest to us’ [22].
Using such a small OR of 1.75 to define GDM does not add any predictive value for a clinician to discriminate between high and low risk women, as the importance of any OR relies on the absolute risk of an adverse outcome. Furthermore the OR overestimates the RR (Risk Ratio or Relative Risk) when the prevalence of the ‘event’ is high (>10 %), as in the case of the outcomes chosen by the IADPSG to define GDM (big babies).
Long-Term Effects of Gestational Diabetes
A commonly expressed concern is that macrosomic babies born to mothers with GDM are at increased risk of obesity and type 2 diabetes in later life. Although this is very likely to be true, in utero exposure to modest degree of hyperglycemia is unlikely to be the proximate cause. Babies born to mothers with type 1 diabetes are exposed to greater degrees of hyperglycemia in utero and are frequently macrosomic at birth, but there is no epidemic of early onset type 2 diabetes in these offspring. With time, the prevalence of overweight in the children of women with type 1 diabetes falls, and by age 11 is no different to that in the general population. In contrast, the prevalence of overweight in the children of women with GDM increases with age [23•], arguing strongly that postnatal environmental factors (or genetic factors) play a critical role for these children.
Consistent with these observations, a follow-up study of the Belfast HAPO cohort showed that the relationship between the weight of the offspring and maternal glycemia in pregnancy was lost by the age of 2 [24], and the BMI of children of the ACHOIS intervention and control groups were similar at age 5–7 [25]. Although no study has ever demonstrated that reducing macrosomia at birth results in reduced long-term obesity and glucose intolerance in children of mothers with GDM, the main argument of the adoption of the IADPSG criteria by the ADA in 2011 was that ‘…changes are being made in the context of worrisome worldwide increases in obesity and diabetes rates, with the intent of optimizing gestational outcomes for women and their babies’ [7•]. This is a large leap of faith that needs to be examined critically.
What Might Be the Benefits of the IADPSG Approach?
As outlined above, evidence from the intervention trials suggests that there are benefits of treating ‘mild GDM’, but these benefits were either on surrogate markers (fewer ‘big babies’), or measures that were secondary outcomes (maternal weight gain, pregnancy-associated hypertension, and shoulder dystocia).
It is important to note that, even if we define GDM by the stricter IADSPG criteria, 78 % of large-for-gestational age babies in HAPO (defined as birth weight >90th percentile) were born to women with normal glucose tolerance [1•]. A recent study demonstrate that women delivering a LGA baby without GDM (as diagnosed by less than 2 abnormal glucose values at the 100 g OGTT using less strict NDDG criteria) do not exhibit postpartum metabolic dysfunction at 3 months. This argues against the assumption that most mothers of LGA infants have unrecognized dysglycemia [26].
As for shoulder dystocia, it is infrequent, subjective, and rarely results in birth trauma or permanent disability. The vast majority of deliveries (>97 %) complicated by shoulder dystocia do not occur in women with GDM [27], so this seems an illogical justification for diagnosing GDM in many more women. With regard to hypertension, less than a third of the women with pregnancy-associated hypertension in the MFMU trial had pre-eclampsia; the remainder had simple gestational hypertension, which has a generally benign outcome [3•].
Most importantly, there is no clinical trial data supporting the expansion of population of GDM cases to the large group of women who would be diagnosed by the new criteria. The intervention studies were conducted on populations identified by 2-step testing with higher diagnostic criteria. It cannot be assumed that the marginal benefits outlined above will also be seen in those with minimally elevated blood glucose levels in pregnancy [9].
What Might Be the Harms of the IADPSG Approach?
There is no doubt that once clinicians know that a woman has GDM, it makes them more likely to intervene. For example, in the ACHOIS study, the rate of induction of labor and NICU admission were significantly increased in the intervention group [2•]. Other prospective studies showed that a label of GDM increases the cesarean section rate, even if birth weight is normalized by treatment [28], especially for women treated with insulin and independent of conventional indications [29]. It seems unlikely that diagnosing and treating more women with GDM outside controlled research settings will lower the cesarean section rate significantly, particularly in an environment where rates are increasing in almost all countries - a change that is not being driven by concerns about GDM [30].
Lower diagnostic criteria for GDM will mean more glucose-lowering treatment given, and will likely lead also to lower target glucose values (increasing the risk of maternal hypoglycemia and poor fetal growth), more obstetrical monitoring, and more medical interventions. The prospect of aggressive diet and/or glucose-lowering treatments in pregnant women, irrespective of their BMI, and other risk factors for adverse pregnancy outcomes, is worrisome in the absence of proven benefit, given the concerns about association of low birth weight with metabolic disorder in adulthood [31]. Can we discriminate with certainty those pregnancies that would benefit from treatment from those that might be harmed?
Medicalization
Medicalization means transforming normal life events like pregnancy and childbirth into medical events and ‘pathologies’. It also means focusing the source of a problem in the individual rather than in the social environment and calling for individual medical intervention rather than more collective or social solutions [32]. This is the case for redefinition of GDM: by taking the authority to define ‘normal blood glucose’ in pregnancy, experts and medical associations will medicalize a large number of hitherto healthy pregnancies. Pregnancy is a time when women are particularly sensitive to their health and receptive to changes, but also vulnerable to stress, anxiety, and guilt. Preventive medical interventions that concern asymptomatic pregnant women must be based on the highest level of randomized evidence, not on observational data or misguided attempts to do good [33].
Cost-Effectiveness
The sustainability of escalating health care costs is a major concern [34]. Identifying a substantially increased number of women with lesser degrees of hyperglycemia as having GDM would have a large impact on health care costs and will divert attention and resources away from genuinely high risk diabetic pregnancies. A decision-tree model of the likely costs and utility of implementing the IADPSG proposal indicates that the incremental cost-effectiveness ratio (the amount we are willing to pay for each unit of improved quality of life) would be over $500,000 per QALY [35]. There are many ethical issues relating to wasteful medical care [36].
The recent analysis suggested that the IADPSG strategy would only be cost-effective if the later progression to maternal type 2 diabetes could be delayed or prevented [35], but there is no evidence that experiencing a GDM pregnancy does this. Published reports from different parts of the world showed that compliance to postpartum OGTT testing is poor, and that women who have had GDM are often from deprived sections of the community who find it difficult to access care and adhere to lifestyle recommendations [37, 38]. Enormous healthcare resources allocation would be needed to make such a diabetes prevention program effective, especially if we double GDM prevalence. Furthermore, we do not know the long-term risk of type 2 diabetes in the women who will be identified by the IADPSG criteria, but we can be reasonably sure that it will be less than in women with greater degrees of hyperglycemia. While effective lifestyle change can indeed delay the progression to type 2 diabetes, this applies not only to women. As GDM largely reflects the degree of glucose intolerance in the community [39], their male partners should in theory benefit just as much.
Toward a Redefinition of GDM and a Potential Consensus
Ryan has recently pointed out that if the GDM diagnostic values were shifted to level 6 out of 7 (corresponding to an OR of 2 for the same HAPO-defined adverse events), the number of serious adverse events that would be potentially averted—assuming interventions are successful—is still low, but the number of women diagnosed would be reduced by 40 % [8]. He proposed to keep a 2-step diagnostic approach with a 1 h–50 g glucose screen confirmed by a 75 g OGTT using an OR of 2.0 for ‘big babies’ (any elevated glucose value: FPG ≥5.3, 1 h ≥10.6, and 2 h ≥9.0 mmol/L). This proposal corresponds to a prevalence of GDM in the HAPO study of 10.5 % vs 17.8 % for the IADPSG criteria. This proposal is closer to the GDM definition used in the ACHOIS and MFMU trials, but still represents a ‘glucocentric’ approach.
If we redefine GDM as ‘maternal glycemia associated with a clinically meaningful increase in adverse pregnancy outcomes,’ we are no longer defining a ‘disease,’ but a prognostic factor. We now recognize that maternal glucose and adverse pregnancy outcomes are linearly and continuously related, without a diagnostic threshold. In this new context, the dichotomous view of GDM being present or absent can only be misleading. Clinicians do not treat OGTTs; they treat individual women with particular characteristics, such as a given BMI, blood pressure, ethnic background, past obstetrical history, and so on. As with any risk factor taken in isolation, maternal glycemia cannot predict accurately, the outcomes we are trying to prevent, because they are multifactorial.
So a more helpful redefinition should more appropriately be based on a prognostic model integrating all HAPO observations, combining the other risk factors for adverse pregnancy outcomes (such as maternal age and BMI) with maternal glycemia as a continuous variable. Only once this prognostic model is validated in a RCT, showing that the new model yields better outcomes than the present strategies, can practice guidelines be proposed [40].
Experts of the IADPSG and others should unite their efforts to plan and pursue the clinical research necessary for offering an evidence-based care of GDM. Arbitrary recommendations and their endorsement as ‘standards of care’, can only obstruct the conduct of the necessary trials by sending the message that doctors know what to do, when in fact they do not. As Epictetus emphasized: ‘A man cannot learn what he thinks he already knows.’ Pregnant women deserve better.
Conclusions
The IADPSG recommendations would lead to nearly 1 in 5 pregnancies being diagnosed with GDM. We believe that clinicians and medical associations that have endorsed the IADSPG recommendations have been tempted to act without sufficient evidence. There are risks in submitting women to invalidated care that can potentially cause more harm than good, and real risk that resources and attention will be diverted away from genuinely high-risk pregnancies in women with pre-gestational diabetes. Far from achieving the much hoped for consensus, the IADPSG proposal has raised important questions about the significance, risks, and cost of redefining GDM. The evidence suggests that the yet unproven benefits are likely to be modest and the costs high. Endorsement of these arbitrary recommendations and their application to all pregnant women is presently unjustified.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• HAPO Study Cooperative Research Group, Metzger BE, Lowe LP, Dyer AR, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002. The HAPO study that related pregnancy outcomes to maternal glycemia on a 75 g OGTT at 28 weeks gestation.
• Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352:2477–86. ACHOIS – a large randomized controlled trial of the treatment of mild GDM.
• Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM, Casey B, et al. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med. 2009;361:1339–48. MFMU study – a large randomized controlled trial of the treatment of mild GDM.
Jarrett RJ. Gestational diabetes: a non-entity? BMJ. 1993;306:37–8.
Ales KL, Santini DL. Should all pregnant women be screened for gestational glucose intolerance? Lancet. 1989;i:1187–91.
• Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, Damm P, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–82. The International Association of Diabetes and Pregnancy Study Groups (IADPSG) consensus panel recommendations.
• American Diabetes Association. Standards of medical care in diabetes–2011. Diabetes Care. 2011;24(Supp 1):s1–s61. The ADA explains its rationale for adopting the IADSPG recommendations.
Ryan EA. Diagnosing gestational diabetes. Diabetologia. 2011;54:480–6.
Long H. Diagnosing gestational diabetes: can expert opinions replace scientific evidence? Diabetologia. 2011;54:2211–3.
Cundy T. Proposed new diagnostic criteria for gestational diabetes–a pause for thought? Diabetic Medicine. 2012;29:176–80.
Moynihan R, Doust J, Henry D. Preventing overdiagnosis: how to stop harming the healthy. BMJ. 2012;344:19–23.
HAPO Study Cooperative Research group. Hyperglycemia and adverse pregnancy outcome study: associations with neonatal anthropometrics. Diabetes. 2009;58:453–59.
HAPO Study Cooperative Research group. Hyperglycemia and adverse pregnancy outcome study: associations with maternal body mass index. Br J Obstet Gynaecol. 2010;117:575–84.
Catalano PM, McIntyre HD, Crickshank JK, McCance DR, Dyer AR, Metzger BE. The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care. 2012;35:780–6.
• Horvath K, Koch K, Jeitler K, Matyas E, Bender R, Bastian H, et al. Effects of treatment in women with gestational diabetes mellitus: systemic review and meta-analysis. BMJ. 2010;340:c1395. Systematic review and meta-analysis of the RCTs on the effects of treatment in women with GDM.
Farrell T, Neale L, Cundy T. Congenital anomalies in the offspring of women with type 1, type 2 and gestational diabetes. Diabetic Med. 2002;19:322–6.
Cundy T, Gamble G, Townend K, Henley PG, MacPherson P, Roberts AB. Perinatal mortality in type 2 diabetes mellitus. Diabetic Med. 2000;17:33–9.
International Expert Committee. Report on the role of A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32:1327–34.
Harlass FE, Brady K, Read JA. Reproducibility of the oral glucose tolerance test in pregnancy. Am J Obstet Gynecol. 1991;164:564–8.
Catalano PM, Drago NM, Amini SB. Reproducibility of the oral glucose tolerance test in pregnant women. Am J Obstet Gynecol. 1993;169:874–81.
Sacks DA, Hadden DR, Maresh M, Deerochnawong C, Dyer AD, Metzger BA, et al. Frequency of gestational diabetes mellitus based on IADPSG consensus panel - recommended criteria at collaborating centers. Diabetes Care. 2012;35:526–8.
Hillier TA, Vesco KK, Pedula KL, Beil TL, Whitlock EP, Pettitt DJ. Screening for gestational diabetes mellitus: a systematic review for the U.S. Preventive Task Force. Ann Intern Med. 2008;148:766–75.
• Boershmann H, Pflüger M, Henneberger L, Ziegler AG, Hummel S. Prevalence and predictors of overweight and insulin resistance in offspring of mothers with gestational diabetes mellitus. Diabetes Care. 2010;33:1845–9. Long-term follow up of infants of mothers with GDM and mothers with type 1 diabetes.
Pettitt DJ, McKenna S, McLaughlin C, et al. Maternal glucose at 28 weeks of gestation is not associated with obesity in 2-year-old offspring: The Belfast HAPO family study. Diabetes Care. 2010;33:1219–23.
Gillman MW, Oakey H, Baghurst PA, et al. Effect of treatment of gestational diabetes mellitus on obesity in the next generation. Diabetes Care. 2010;33:964–8.
Kew S, Ye C, Sermer M, et al. Postpartum metabolic function in women delivering a macrosomic infant in the absence of gestational diabetes. Diabetes Care. 2011;34:2608–13.
Fadl HE, Östlund IKM, Magnuson AFK, Hanson USB. Maternal and neonatal outcomes and time trends of gestational diabetes mellitus in Sweden from 1991 to 2003. Diabetic Med. 2010;27:436–41.
Naylor CD, Sermer M, Chen E, Sykora K. Cesarean delivery in relation to birth weight and gestational glucose tolerance: pathophysiology or practice style? JAMA. 1996;275:1165–70.
Donovan LE, Boyle SL, McNeil DA, Pedersen SD, Dean SR, Wood S, Edwards AL. Label of gestational diabetes mellitus affects caesarean section and neonatal intensive care unit admission without conventional indications. Can J Diabetes. 2012;36:58–63.
Lumbiganon P, Laopaiboon M, Gülmezoglu AM, Souza JP, Taneepanichskul S, Ruyan P, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007–2008. Lancet. 2010;375:490–9.
Hales CN, Barker DJP, Clark PMS, Cox LJ, Fall C, Winter PD. Fetal and infant growth and impaired glucose tolerance at age 64. BMJ. 1991;303:1019–22.
Conrad P. The medicalization of society. Baltimore: The John Hopkins University Press; 2007. p. 7–8.
Sackett DL. The arrogance of preventive medicine. CMAJ. 2002;167:363–4.
Neumann PJ. What we talk about when we talk about health care costs. N Engl J Med. 2012;366:585–6.
Werner EF, Pettker CM, Zuckerwise L, Reel M, Funai EF, Henderson J, Thung SF. Screening for gestational diabetes mellitus: are the criteria proposed by the International Association of the Diabetes and Pregnancy Study Groups cost-effective? Diabetes Care. 2012;35:529–35.
Brody H. From an ethics of rationing to an ethics of waste avoidance. N Engl J Med. 2012;366:1949–51.
Kim C, Sinco B, Kieffer EA. Racial and ethnic variation in access to health care, provision of health care services, and ratings of health among women with histories of gestational diabetes mellitus. Diabetes Care. 2007;30:1459–65.
Kieffer EA, Sinco B, Kim C. Health behaviors among women of reproductive age with and without a history of gestational diabetes mellitus. Diabetes Care. 2006;29:1788–93.
Harris MI. Gestational diabetes may represent discovery of pre-existing glucose intolerance. Diabetes Care. 1988;11:402–11.
Royston P, Moons KJM, Altman DG, Vergouwe Y. Prognosis and prognostic research: developing a prognostic model. BMJ. 2009;338:B605.
Disclosure
Conflicts of interest: T. Cundy: none; H. Long: has received honoraria from Eli Lilly, Novo Nordisk, Merck, Aventis, Bristol Myers Squibb, and Roche.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Long, H., Cundy, T. Establishing Consensus in the Diagnosis of Gestational Diabetes Following HAPO: Where Do We Stand?. Curr Diab Rep 13, 43–50 (2013). https://doi.org/10.1007/s11892-012-0330-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11892-012-0330-3