Abstract
Approximately 8.3% of the US population has diabetes and estimates indicate that 79 million adults have prediabetes and 33.8% are obese, increasing their risk of diabetes. The national Diabetes Prevention Program (DPP) and subsequent translation studies have demonstrated the efficacy of the DPP lifestyle intervention (DPPLI) on lowering weight and reducing risk of type 2 diabetes over 10 years. Innovative strategies are needed to translate the DPPLI to reach people at risk of diabetes. Community health workers represent a group of individuals poised to play a role in supporting the translation of the DPPLI, especially in underserved populations. This article aims to 1) describe community health workers in general; 2) describe their role and impact on diabetes care in general; and 3) provide a detailed overview of studies involving community health workers in the translation of the DPPLI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction: Background on Diabetes, Prediabetes, and Obesity
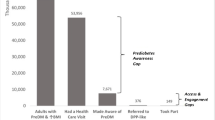
Diabetes mellitus is one of the most common chronic diseases throughout the world. The number of those affected is increasing rapidly as economic development and urbanization lead to sedentary lifestyles and increased obesity [1]. Approximately 25.8 million in the United States (8.3%) have diabetes, including 18.8 million who are diagnosed and 7.0 million undiagnosed [2]. Estimates indicate that 33.8% of US adults are obese [3] and 79 million have prediabetes [2]. There has been a dramatic increase in obesity in the United States over the past two decades. In 2010, there was no state with an obesity prevalence of less than 20% [3] and 12 states had reached a prevalence of 30% or greater [4]. Reducing obesity, by improving eating and physical activity habits, represents an important path to reducing the risk of diabetes [5].
Obesity [6] and diabetes disproportionately affect minority populations [2]. Non-Hispanic blacks have the highest rates of obesity (44.1%) compared to Mexican Americans (39.3%), all Hispanics (37.9%), and non-Hispanic whites (32.6%) [4]. Furthermore, 8.4% of Asian Americans, 11.8% of Hispanics/Latinos, and 12.6% of non-Hispanic blacks have diagnosed diabetes, compared with 7.1% of non-Hispanic whites [2]. In addition, an estimated 16.1% of the total adult population served by the Indian Health Service has diagnosed diabetes [2]. Other underserved populations at higher risk of diabetes include older adults and lower income groups [7]. Widening health disparities [8] and the aging of the US population [9] will continue to expand the number of people with diabetes if effective prevention interventions are not translated to reach these groups, among others at risk.
The growing epidemic of obesity and diabetes requires urgent, diverse, and broad efforts to have a major impact in these public health challenges. The national Diabetes Prevention Program (DPP) [10, 11] and subsequent translation studies have demonstrated the efficacy of the DPP lifestyle intervention (DPPLI) on lowering weight [12•, 13–17, 18••, 19, 20, 21••, 22•, 23] and reducing risk of type 2 diabetes over 10 years [11]. Innovative strategies are needed to translate the efficacious DPPLI to reach the estimated 79 million people with prediabetes [2] and the even greater number of obese adults at risk for diabetes [4]. Efforts are especially needed to reach underserved and/or populations who are at higher risk of obesity and diabetes.
Shortage of Health Professionals: A Role for Community Health Workers
The shortage of health professionals has been recognized as a global issue, and efforts have been initiated to identify ways to extend our health care workforce [24]. One group, community health workers (CHWs), may offer hope in providing additional help, particularly for underserved populations. CHWs have been serving an important role in supporting the health needs of their communities across the globe for many years. Recently, the World Health Organization’s Global Health Workforce Alliance conducted a systematic review of the literature on the global experience of CHWs. The executive summary of the final document noted that “Participation of community health workers (CHWs) in the provision of primary health care has been experienced all over the world for several decades, and there is an amount of evidence showing that they can add significantly to the efforts of improving the health of the population, particularly in those settings with the highest shortage of motivated and capable health professionals” (p. 11) [25]. In addition, [25] stated:
The World Health Report 2006 argued that community health workers (CHWs) have the potential to be part of the solution to the human resource crisis affecting many countries. CHWs provide a variety of functions, including outreach, counseling and patient home care and represent a resource to reach and serve disadvantaged populations. There has been mounting evidence to demonstrate the positive potential of community health workers in improving equitable access to care and health outcomes.
Therefore, the overall goal of this paper is to describe the role of CHWs in the translation of the DPPLI. Secondary objectives are to 1) describe CHWs in general; 2) describe their role and impact on diabetes care in general; and 3) provide a detailed overview of studies involving CHWs in the translation of the DPPLI.
General Definition of CHW
The US Department of Health and Human Services (USDHHS) Health Resources and Services Administration Bureau of Health Professions conducted a Community Health Worker National Workforce Study [26]. In the report on this study, the USDHHS defined CHWs as:
…lay members of communities who work either for pay or as volunteers in association with the local health care system in both urban and rural environments and usually share ethnicity, language, socioeconomic status, and life experiences with the community members they serve. They have been identified by many titles such as community health advisors, lay health advocates, “promotores(as),” outreach educators, community health representatives, peer health promoters, and peer health educators. CHWs offer interpretation and translation services, provide culturally appropriate health education and information, assist people in receiving the care they need, give informal counseling and guidance on health behaviors, advocate for individual and community health needs, and provide some direct services such as first aid and blood pressure screening. (p. 3–4 executive summary).
Diabetes-Specific Definition of CHWs
The potential role of CHWs in diabetes has recently been identified by the American Association of Diabetes Educators (AADE), and CHWs have been included within Level 1 of the 5 levels of diabetes educators [27, 28]. The AADE [29] stated:
Community health workers (Level 1 providers) are non-diabetes educators uniquely positioned to collaborate with diabetes educators and other providers to improve the quality of diabetes education, care, and prevention in communities. CHWs dedicated to diabetes prevention and care are likely to have completed specialized training. They can serve as bridges between their ethnic, cultural, or geographic communities and health care providers, and they engage their community to prevent diabetes and its complications through education, lifestyle change, self-management, and social support. CHWs also play a vital role in data gathering and data entry. (p. 3).
In a 2009 position statement, the AADE [30] defined a CHW as a: Frontline public health worker who is a trusted member of and/or has an unusually close understanding of the community served. This trusting relationship enables the CHW to serve as a liaison/link/intermediary between health/social services and the community to facilitate access to services and improve the quality and cultural competence of service delivery. A CHW also builds individual and community capacity by increasing health knowledge and self-sufficiency through a range of activities such as outreach, community education, informal counseling, social support, and advocacy. (p. 49S).
The AADE [30] also described the following positions regarding inclusion of CHWs:
-
1.
Diabetes educators and other health care professionals should support:
-
a.
the role of CHWs in serving as bridges between the health care system and people with and at risk for diabetes;
-
b.
the role of CHWs in primary and secondary prevention;
-
c.
continued research that evaluates the roles, contributions, and effectiveness of CHWs.
-
a.
-
2.
“CHWs should receive effective training in core diabetes skills and competencies”; and
-
3.
“There should be reciprocal exchange of information and support between CHWs and the health care team to facilitate the best outcomes for people with and at risk for diabetes.” (p. 48–49S).
Evidence Supporting Benefits of CHWs in Diabetes: Community-Based Screening, Awareness, and Support
Several studies reported beneficial outcomes for the use of CHWs in community screening, diabetes awareness, and support. A systematic review of 18 studies (including 8 randomized clinical trials [RCTs]) by Norris et al. [31] evaluated evidence of the roles of CHWs and the impact on measurable diabetes outcomes. CHWs were engaged in patient care and support, outreach, patient education, instrumental support to other health care professionals in delivery of care and educational programs, and liaisons with the health care system. Interventions using CHWs as team members reported significant improvements in knowledge of diabetes and self-care practices, particularly glucose self-monitoring, diet, and physical activity. Physiologic variables such as hemoglobin A1c (HbA1c), blood pressure, and lipid levels also reportedly showed improvement; and health care utilization measured by number of emergency visits and hospital admissions was significantly reduced.
A recent study by Castillo et al. [32] examined a community diabetes education and support intervention led by CHWs. In this study, CHWs received 20 hours of intensive training in the Diabetes Empowerment Education Program (DEEP) [32] followed by coaching, supervision, and support from experienced CHWs and research staff. Trained CHWs then provided diabetes education and support to 70 community residents following the standardized DEEP curriculum. At the end of the 3-month intervention, results showed significant improvements in diabetes knowledge, self-care behaviors, and clinical measures, including HbA1c, blood pressure, and depression [32]. In addition, a subsample was assessed on self-efficacy and showed a trend toward significant improvement.
An RCT by Lorig et al. [33] examined the effectiveness of a 6-week community-based diabetes self-management program compared to usual care on health status, self-management behaviors, and self-efficacy. Three hundred forty-five community residents with type 2 diabetes were assessed at 6 and 12 months post-intervention. CHWs received intensive training in the delivery of the Diabetes Self-Management Program [33], and further coaching in class management, teaching strategies, and program logistics. The study showed significant improvements at 6 months in hypoglycemia; depression scores; communication with physician; self-care behaviors, including exercise, glucose monitoring, healthy eating, and reading food labels; self-efficacy scores; and patient activation. The 12-month follow-up showed maintenance of improvements in depression, healthy eating, provider communication, patient activation, and self-efficacy.
A qualitative evaluation by Davis et al. [34] described CHWs engaged in providing assistance, teaching skills, distributing information, recruiting, and monitoring progress. The skills most often taught by CHWs were related to blood glucose monitoring, healthy eating, and physical activity. They provided assistance in goal setting, problem solving, emotional support, encouragement/motivation, and instrumental support for the patient with diabetes. Patients’ reports consistently expressed their appreciation for the CHWs’ encouragement, assistance with personal needs and motivation, and the accessibility, attentiveness, and openness in their interactions. In summary, CHWs make meaningful contributions to outreach, screening, patient education, and support, and do so in a manner that is culturally sensitive and focused on eliminating patient barriers to optimal self-care.
Evidence Supporting Benefits of CHWs in Diabetes: Role on Multidisciplinary Health Care Team
To date, only a small number of published papers report on the inclusion of CHWs as members of the health care team. One of the few examples included an evaluation of a service project for patients in Medicaid using a nurse care management/peer education team approach [35]. In this project, CHWs received additional training to serve as diabetes peer educators and delivered diabetes education curriculum to low-income, low-literacy patients. The team collaboration proved effective in significantly improving health outcomes, including glycemic control, total cholesterol, low-density lipoprotein (LDL), triglycerides, and diastolic blood pressure; diabetes knowledge; treatment satisfaction; and health beliefs. Another study, an RCT by Babamoto et al. [36], compared a CHW approach to nurse case management and to standard provider care for newly diagnosed patients with type 2 diabetes in an inner city population. CHWs were considered paid clinical staff and met the organization’s requirements of having a high school degree or general equivalency degree (GED). After receiving formal program training, CHWs conducted educational sessions based on American Diabetes Association standards that were tailored to the participant’s needs and followed a format that offered accessibility and flexibility to the participant. Even though all three groups significantly reduced HbA1c, the CHW intervention had the greatest impact on modifiable risk factors (exercise, fruit and vegetable intake, body mass index [BMI]), medication-taking behavior, diabetes knowledge, reduction in emergency department admissions, and patients’ self-reported health status. Another example of integration of CHWs in the health care team is a model that used a pharmacist-CHW team to improve self-care and reduce barriers in medication adherence among Latinos with type 2 diabetes [37]. Gerber et al. [37] detailed procedures of the CHW interaction with the pharmacist and the patient and highlighted the intensity of the effort required to achieve adequate medication adherence. The role of the CHW was to facilitate communicating, interpreting, and reinforcing the provider’s instructions, while maintaining a personal connection with the patient.
A study by Thompson et al. [38] reported on the effectiveness of CHWs trained in the Transtheoretical Model of Change (TTM) to provide diabetes management education and support to a cohort of 142 patients in an inner city clinic. The intervention included the addition of two components to the usual care provided by the clinic: CHWs worked one on one with patients at least weekly for the first 6 months and monthly thereafter; and CHWs provided patient-centered counseling using the TTM. This clinic integrated CHWs into the health care team, with providers and CHWs sharing patient information and collaborating in patient care. CHWs received training in popular education, group facilitation, communication, presentation, and analysis. They also received intensive training in diabetes education and the TTM, and ongoing instruction and support for the duration of the project. Providers also received training in the TTM. This pre-/post-test study observed significant improvements in HbA1c at the 6- and 12-month follow-ups. Other measures (cholesterol, blood pressure, BMI) showed improvement but did not reach statistical significance. Changes in HbA1c correlated with the frequency of weekly CHW contacts, so that patients with the greatest number of contacts with CHWs showed the greatest change in HbA1c levels. Besides one-on-one counseling, CHWs provided community outreach, led walking clubs and diabetes self-management classes, and facilitated cognitive-behavioral group therapy led by a mental health professional. Finally, a study by Otero-Sabogal et al. [39] reported the successful partnership of physicians with CHWs in implementing a team model of diabetes care. CHWs worked closely with physicians, a Certified Diabetes Educator and a social worker in developing and following up on action plans for the patient’s management. This pre-/post-test prospective pilot study assessed changes in clinical and patient activation measures in a cohort of 114 patients enrolled in the clinic. Over the course of 2 years, patients received interventions by the primary care provider complemented by the CHW’s interventions that included diabetes education, medication adherence, self-management support, group support, navigation, and follow-up phone support. The study also reviewed patient satisfaction and providers’ satisfaction with the CHW roles. Statistically significant improvements were reported on glycemic levels, LDL, total cholesterol, and patient activation. Patients reported a high level of satisfaction with the provider-CHW relationship and how it facilitated patient-provider communication. Providers gave a very positive evaluation of the work of the CHWs, and their patients were better educated, had improved self-management, and reduced the number of unnecessary visits and hospitalizations.
The studies examining models of including CHWs as part of a multidisciplinary diabetes care team have shown promising results. Because few studies have been conducted and only one was an RCT, more research is needed to further investigate the role of CHWs on the diabetes care team.
Evidence Supporting the Benefits of CHWs in Prevention: DPPLI Translation Efforts
To date, six studies that focused on the translation of the DPPLI have incorporated CHWs into their work in some manner (Tables 1 and 2). These include two primary CHW models: 1) serving as the primary interventionists delivering the DPPLI in various community settings; and 2) participating as a team member and serving a supportive role for health professional delivery of the DPPLI. An overview of each of these DPPLI translation studies will be provided with a focus on the weight-related outcomes. Only studies which specifically focused on translation of the DPPLI program were included in this review.
The DEPLOY Model
In the DEPLOY (Diabetes Education & Prevention with a Lifestyle Intervention Offered at the YMCA) study, a YMCA model [12•] was used to translate the DPPLI. This pilot cluster-randomized trial compared a group-based DPPLI delivered at a YMCA to brief counseling alone. A total of 92 participants enrolled in the study, with a mean age of 56.5 years in the DPP group and 60.1 years in the standard advice group, 55.4% female, and 81.5% white. Although differences in age and weight between the control and intervention groups were not significant, it is notable that the control group was more likely to be female and non-white. Participants were recruited from health screenings conducted at two YMCAs. The eligibility criteria included BMI ≥24 kg/m2, two or more diabetes risk factors based on ADA risk assessment, and a random capillary blood glucose of 110 to 199 mg/dL. The DPPLI core program, modified for sustainability in the YMCA, was delivered in small groups over 16 to 20 weeks by trained YMCA staff (CHWs). Monthly maintenance large group sessions were held after the core program. Assessments of weight and clinical measures (eg, HbA1c, total cholesterol) were collected at baseline and at 4 to 6 and 12 to 14 months after study enrollment. The results of this study demonstrated a significant decrease in weight post-intervention, with an average weight loss of 6% in the DPPLI group compared with 2% in the control group. In addition, the weight losses were sustained at 12 months. Statistical adjustments for baseline differences in ethnicity and gender did not change the findings. These findings support the YMCA model as another promising translation model suitable for wide dissemination.
The HELP PD Project
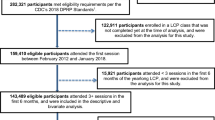
The HELP PD (Healthy Living Partnerships to Prevent Diabetes) project was a community-based DPPLI translation study [18••]. In this study, the DPPLI was delivered by CHWs who received 36 hours of intensive training and were supervised by dietitians. To examine the impact of this DPPLI translation, a sample of 301 overweight/obese individuals with fasting blood glucose (FBG) of between 95 and 125 mg/dL were randomized to receive either DPPLI or usual care. The primary inclusion criteria for this group were adults over 21 years old, high risk for developing diabetes, no medical contraindications to participate in a lifestyle intervention including unsupervised physical activity and weight loss, BMI ≥25 kg/m2 and BMI ≤39.9 kg/m2, and FBG between 95 and 125 mg/dL following at least an 8-hour fast. The characteristics of the sample were mean age of 57.9 years, 42.5% male, 26% race/ethnicity other than white, and 80% with an education level beyond high school. The enhanced usual care group had two visits with a registered dietitian and was provided with a quarterly newsletter with tips for lifestyle changes. The DPPLI was a 2-year, 24-session, group-based intervention administered through a diabetes education program and delivered by CHWs in community settings (eg, recreation centers, libraries, schools, or churches). All participants in the intervention group received three personalized consultations with a registered dietitian at months 1, 3, and 6. Measurements of fasting glucose, insulin resistance, and adiposity were taken at baseline and every 6 months up to 2 years. The 1-year results indicated that the CHW DPPLI groups achieved and maintained significantly better weight-related outcomes, including weight/BMI and waist circumference, and significantly better improvements in clinical outcomes, including fasting glucose and insulin resistance. The results of this randomized controlled study support a DPPLI translation model with CHWs delivering the lifestyle intervention in groups in community settings through a diabetes education program and under the supervision of dietitians.
The POLI Study
One community-based participatory research (CBPR) study examined a DPPLI translation in a population of Native Hawaiians and Other Pacific Islanders (NHOPI) [40••]. The DPPLI was culturally adapted for NHOPI communities and named the POLI (Pili ’Ohana Lifestyle Intervention). The primary inclusion criteria for this study were self-identified Native Hawaiian, Filipino or Other Pacific Islander, 18 years or older, overweight or obese (BMI ≥25 kg/m2 for NHOPIs or ≥23 kg/m2 for Filipinos), and able to follow a behavioral weight loss program that involved 150 min of brisk walking per week and a dietary regimen to achieve weight loss of 1 to 2 lb per week. A total of 239 participants enrolled in POLI and had the following characteristics: mean age of 49 years, 83% female, 52% Native Hawaiian, 27% Chuukese, and 12% Samoan. The intervention was delivered in groups in community settings by trained community peer educators (CHWs). The POLI program included four sessions delivered weekly followed by four sessions delivered every 2 weeks for 2 months for a total of 12 weeks. Assessments were conducted at baseline and within 2 weeks of completing the 12-week program. Significant improvement was found for all clinical measures. The mean weight loss was 1.5 kg, with 11% of participants losing at least 5% of baseline weight. Greater adherence was associated with greater weight loss. This CBPR translation delivered by CHWs with an underserved population showed promise and warrants further study using a controlled design.
The MTC Study
The MTC (Making the Connection) (¡Conéctate!) study examined a community-based participatory translation of the DPPLI in a Latino community [21••]. The researchers in this study partnered with the community to tailor, implement, and evaluate a community-based version of the 24-session DPPLI delivered in groups by a CHW. The CHWs participated in a 20-hour DEEP [32] training of trainers and received intensive and experiential training from a multidisciplinary team in the curriculum, leadership skills, behavior change and motivational strategies, and compliance with a research protocol. The CHWs delivered a 1-year DPPLI Vanguard group and received observation, supervision, and skill refinement before leading the translation study lifestyle groups. Participants were recruited from community-based health screenings. A total of 69 participants were enrolled based on the following eligibility criteria: low physical activity level, screening glucose value in the normal to prediabetes range with no current diagnosis of diabetes, overweight/obese (BMI >24.9 kg/m2 and <40 kg/m2), not pregnant nor planning to become pregnant during study period, aged 18 to 65 years, Latino, living in the study target communities, and no reported medical restrictions related to the program goals. This was a nonrandomized prospective study using a single-group completely within-subject design. Assessments were conducted at baseline, 6 months, and 12 months, and included three anthropometric measures (ie, weight/BMI, waist circumference, and body fat). The characteristics of the sample were mean age of 37.86 years, 92.8% female, 100% Hispanic, 40.5% with at least high school diploma, 24.6% employed, and 40.6% with health insurance. The MTC DPPLI was a 1-year program modeled after the DPPLI including a “core” program with weekly sessions that shifted to biweekly and then monthly sessions for the “aftercore” program. The MTC DPPLI intervention was delivered in Spanish in small groups in community settings, such as schools, community hospitals, a cultural center, and a social service facility. The results of this translation study indicated statistically significant improvements across time for all three anthropometric measures (ie, weight/BMI, waist circumference, body fat), particularly at 6 months. The proportion of participants that achieved 5% weight loss and 7% weight loss was 29% and 20%, respectively, at 6 months, and 30% and 16%, respectively, at 12 months. The results of this study support this CBPR CHW translation model as another promising approach to delivering the DPPLI, particularly in a high-risk underserved population. Randomized controlled studies are needed to further examine this CHW model of DPPLI translation.
Pittsburgh Community-Based Model
A DPPLI translation was conducted in a community hospital in an urban medically underserved community in Pittsburgh [22•]. This nonrandomized prospective intervention study used a single-group repeated measures design to test the effectiveness of a community-based DPPLI program. Participants were recruited from community-based screenings in 11 urban medically underserved neighborhoods, representing the primary service area for a community hospital. Eligibility criteria included BMI ≥25 kg/m2, physician consent to exercise, and at least 3 of 5 components of metabolic syndrome. A total of 88 participants enrolled in the DPPLI program, and their characteristics included mean age of 54 years, 84.1% female, 72.7% non-Hispanic white, 59.7% had an annual household income ≤200% below the poverty level, and 77.4% had at least a high school education. Assessments were conducted at baseline, 3 months, and 6 months, and the primary weight measures included anthropometrics (weight/BMI, waist circumference) and laboratory data (eg, glucose). The DPPLI program included 12 weekly group sessions over 12 to 14 weeks and was delivered in a community hospital by a registered dietitian and an exercise specialist with support from two “lay health coaches” (CHWs). The CHWs were trained, along with the team, in delivery of the program. The CHWs were supervised by the professional staff, and their role included communicating with participants and physician offices, sharing relevant experiences to initiate class discussions, identifying barriers and solutions to promote program engagement and retention, and assisting in study logistics. Improvements were found in weight across time. The percentages who lost at least 5% and 7%, respectively, were 46.4% and 26.1% at 3 months, and the majority sustained their losses at 6 months. When improvement in metabolic syndrome components was examined, similar patterns were observed. This translation study supports a hospital-based translation model that uses a team approach with health professionals leading the groups and CHWs playing a supportive role. Randomized controlled research is also needed to examine this promising model.
Senior Center Model
In another study, the DPPLI was delivered by lay health educators (CHWs) in senior centers with obese older adults [41]. This study used a cluster-randomized control trial design with 228 obese older adults nested within 15 senior centers. The inclusion criteria were obese (BMI ≥30 kg/m2), older adults (≥60 years), able to engage in moderate exercise, and free of serious memory problems. The total participant characteristics were mean age 71.2 years, 84% female, 92% white, 89% completed high school, 12.7% employed, 80.3% retired or disabled, and mean BMI of 36.1 kg/m2. The attention control group received “cognitive training,” which included basic information about how the brain functions: memory processes and how aging and other factors affect these processes, and cognitive strategies to enhance memory functioning. The CHWs received a total of 32 hour of face-to-face training from research staff and participated in weekly telephone supervision sessions. The DPPLI was a 12-session group program led by CHWs in the senior centers. Weight-related measurements were taken at baseline and 4 months after the 12-week program. For the seniors at centers randomized to receive the CHW-led DPPLI groups, the results indicated significantly greater weight loss, and a significantly greater proportion reached either a 5% or 7% weight loss goal (38% and 24%, respectively) compared with those at the control centers (5% and 3%, respectively). Results from this study support this as another promising model of translation with an underserved population.
Conclusions
The important role that CHWs may play in supporting the health of community members has been recognized by national and international groups, such as the World Health Organization [24] and the Centers for Disease Control and Prevention [42]. In addition, the role they may play in supporting diabetes education, especially in underserved community populations, has been recognized by the AADE [30]. Evidence has been mounting demonstrating their role in community-based outreach, awareness, and support for people with diabetes. Some recent evidence has also emerged demonstrating their promise as members of a multidisciplinary diabetes care team.
As noted in the introduction, the growing epidemic of obesity and diabetes requires urgent, diverse, and broad efforts to have a major impact in these public health challenges. The DPPLI is one efficacious approach to tackling this challenge through weight reduction to help control the risk of type 2 diabetes. Innovative strategies are needed to translate the DPPLI to reach people at risk of diabetes. CHWs represent a motivated group of individuals poised to play a role in supporting the translation of the DPPLI, especially in underserved populations. Six studies were identified in the literature that included CHWs in efforts to translate the DPPLI. These studies and a recent meta-analysis support the promising role that CHWs may play in delivering the DPPLI in community settings and/or working with multidisciplinary health care teams [43]. The DPPLI has been adapted in different ways, but the program goals have remained consistent with the original DPPLI. These DPPLIs have demonstrated promise across a variety of high-risk and underserved populations and diverse medical and community settings.
Although the results to date examining the role of CHWs in DPPLI translation are promising, few have been RCTs. Therefore, further research is needed to examine these promising models using large-scale RCTs. In addition, consistency in outcome measures and assessment points would greatly enhance our interpretation of the findings and promote clearer comparison across studies.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Whiting D, Guariguata L, Weil C, et al. IDF Diabetes Atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–21.
Centers for Disease Control and Prevention: National diabetes fact sheet, 2011. Available at http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed December 2011.
Centers for Disease Control and Prevention, Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion: U.S. Obesity Trends. Available at http://www.cdc.gov/obesity/data/trends.html. Accessed December 2011.
Centers for Disease Control and Prevention, Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion: Adult Obesity. Available at http://www.cdc.gov/obesity/data/adult.html. Accessed December 2011.
National Diabetes Information Clearinghouse: Diabetes Prevention Program. Available at http://diabetes.niddk.nih.gov/dm/pubs/preventionprogram/#results. Accessed December 2011.
Centers for Disease Control and Prevention: Obesity: halting the epidemic by making health easier. Available at http://cdc.gov/chronicdisease/resources/publications/aag/obesity.htm. Accessed November 2011.
Centers for Disease Control and Prevention. MMWR Weekly Report: Diabetes – United States, 2004 and 2008. Available at http://www.cdc.gov/mmwr/preview/mmwrhtml/su6001a20.htm?s_cid=su6001a20_w. Accessed November 2011.
Centers for Disease Control and Prevention: CDC Health Disparities & Inequalities Report (CHDIR). Available at http://www.cdc.gov/minorityhealth/CHDIReport.html. Accessed December 2011.
Administration on Aging: A profile of older Americans: 2010. Available at http://aoa.gov/AoAroot/Aging_Statistics/Profile/2010/3.aspx. Accessed December 2011.
Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the diabetes prevention program outcomes study. Lancet. 2009;374:1677–86.
• Ackermann RT, Finch EA, Brizendine E, et al. Translating the diabetes prevention program into the community. The DEPLOY pilot study. Am J Prev Med. 2008;35:357–363. This is a cluster randomized study conducted in the community that compared the effects of DPPLI versus brief counseling in adults at risk of diabetes on HbA 1c , blood pressure, cholesterol and weight at 6 and 12 months.
Amundson HA, Butcher MK, Gohdes D, et al. Translating the diabetes prevention program into practice in the general community: findings from the Montana cardiovascular disease and diabetes prevention program. Diabetes Educ. 2009;35:209–10.
Boltri JM, Davis-Smith YM, Seale JP, et al. Diabetes prevention in a faith-based setting: results of translational research. J Publ Health Manag Pract. 2008;14:29–32.
Davis-Smith YM, Boltri JM, Seale JP, et al. Implementing a diabetes prevention program in a rural African-American church. J Natl Med Assoc. 2007;99:440–6.
Dodani S, Kramer MK, Williams L, et al. Fit body and soul: a church-based behavioral lifestyle program for diabetes prevention in African Americans. Ethn Dis. 2009;19:135–41.
Jackson L. Translating the diabetes prevention program into practice: a review of community interventions. Diabetes Educ. 2009;35:309–20.
•• Katula JA, Vitolins MZ, Rosenberger EL, et al. One-year results of a community-based translation of the diabetes prevention program: healthy-living partnerships to prevent diabetes (HELP PD) project. Diabetes Care. 2011;34:1451–1457. This is a randomized controlled trial implementing the DPPLI in community settings, led by CHWs, and evaluating the effect on fasting glucose, insulin, insulin resistance, weight, and waist circumference at 6 and 12 months.
Kramer MK, McWilliams JR, Chen HY, et al. A community-based diabetes prevention program: evaluation of the group lifestyle balance program delivered by diabetes educators. Diabetes Educ. 2011;37:659–68.
McTigue KM, Conroy MB, Hess R, et al. Using the internet to translate an evidence-based lifestyle intervention into practice. Telemed J E Health. 2009;15:851–8.
•• Ruggiero L, Oros S, Choi YK. Community-based translation of the diabetes prevention program’s lifestyle intervention in an underserved Latino population. Diabetes Educ. 2011;37:564–572. This is a nonrandomized prospective single-group study applying CBPR approaches to translate DPPLI into the Latino community to assess changes in measures of obesity, physical activity, and eating habits.
• Seidel MC, Powell RO, Zgibor JC, et al. Translating the diabetes prevention program into an urban medically underserved community: a nonrandomized prospective intervention study. Diabetes Care. 2008;31:684–689. This is a nonrandomized single group study evaluating the translation of a 12-week DPPLI for obese patients from an urban underserved community.
Vadheim LM, McPherson C, Kassner DR, et al. Adapted diabetes prevention program lifestyle intervention can be effectively delivered through telehealth. Diabetes Educ. 2010;36:651–6.
World Health Organization: The World Health Report 2006 - working together for health. Available at http://www.who.int/whr/2006/en/. Accessed November 2011.
Global Health Workforce Alliance, World Health Organization: Global experience of community health workers for delivery of health related millennium development goals: a systematic review, country case studies, and recommendations for integration into national health systems. Available at http://www.who.int/workforcealliance/knowledge/publications/CHW_FullReport_2010.pdf Accessed December 2011.. Accessed December 2011.
U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions: Community health worker national workforce study, March 2007. Available at http://bhpr.hrsa.gov/healthworkforce/reports/chwstudy2007.pdf. Accessed March 2009.
American Association of Diabetes Educators: Guidelines for the practice of diabetes education. Available at http://www.diabeteseducator.org/DiabetesEducation/position/Practice_Guidelines.html. Accessed December 2011.
American Association of Diabetes Educators: Competencies for diabetes educators. Available at http://www.diabeteseducator.org/DiabetesEducation/position/competencies.html. Accessed December 2011.
American Association of Diabetes Educators: A sustainable model of diabetes self-management education/training involves a multi-level team that can include community health workers. Available at: http://www.diabeteseducator.org/export/sites/aade/_resources/pdf/research/Community_Health_Workers_White_Paper.pdf. Accessed November 2011.
American Association of Diabetes Educators. AADE position statement: community health workers in diabetes management and prevention. Diabetes Educ. 2009;35:48S–52S.
Norris SL, Chowdhury FM, Van Le K, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabet Med. 2006;23:544–56.
Castillo A, Giachello A, Bates R, et al. Community-based diabetes education for Latinos: the Diabetes Empowerment Education Program. Diabetes Educ. 2010;36:586–94.
Lorig K, Ritte PL, Villa FJ, et al. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ. 2009;35:641–51.
Davis KL, O’Toole ML, Brownson CA, et al. Teaching how, not what: the contributions of community health workers to diabetes self-management. Diabetes Educ. 2007;33:208S–15S.
Philis-Tsimikas A, Walker C, Rivard L, et al. Improvement in diabetes care of underinsured patients enrolled in project dulce: a community-based, culturally appropriate, nurse case management and peer education diabetes care model. Diabetes Care. 2004;27:110–5.
Babamoto KS, Sey KA, Camilleri AJ, et al. Improving diabetes care and health measures among Hispanics using community health workers: results from a randomized controlled trial. Health Educ Behav. 2009;36:113–26.
Gerber BS, Cano AI, Caceres ML, et al. A pharmacist and health promoter team to improve medication adherence among Latinos with diabetes. Ann Pharmacother. 2010;44:70–9.
Thompson JR, Horton C, Flores C. Advancing diabetes self-management in the Mexican American population: a community health worker model in a primary care setting. Diabetes Educ. 2007;33:159S–65S.
Otero-Sabogal R, Arretz D, Siebold S, et al. Physician-community health worker partnering to support diabetes self-management in primary care. Qual Prim Care. 2010;18:363–72.
•• Mau MK, Keawe’aimoku Kaholokula J, West MR, et al. Translating diabetes prevention into Native Hawaiian and Pacific Islander communities: the PILI ’ohana pilot project. Progress in Community Health Partnerships. 2010;4:7–16. This study reports the translation of DPPLI to Native Hawaiian and Pacific Islander communities applying CBPR in the design, implementation, and evaluation of a pilot study assessing changes in weight, blood pressure, and lifestyle behaviors.
West DS, Bursac Z, Cornell CE, et al. Lay health educators translate a weight-loss intervention in senior centers: a randomized controlled trial. Am J Prev Med. 2011;41:385–91. This is a cluster-randomized controlled trial that compares an adaptation of DPPLI for obese older adults conducted by lay health educators versus a cognitive training control group and measuring weight loss at 4 months post-intervention.
Centers for Disease Control, Division of Diabetes Translation: Community health workers/promotores de salud: critical connections in communities. Available at http://www.cdc.gov/diabetes/projects/pdfs/comm.pdf. Accessed March 2010.
Ali MK, Echouffo-Tcheugui JB, Williamson DF. How Effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health Affair. 2012;31:67–75.
Acknowledgments
The authors would like to thank Kevin Grandfield for his editorial review of this manuscript. Also, L. Ruggiero’s research described in this paper was supported by Cooperative Agreement #1-U48-DP-000048 from the US Centers for Disease Control and Prevention (CDC), including support from the Division of Diabetes Translation. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the CDC.
Disclosure
Conflicts of interest: L. Ruggiero: has received payment for lectures including service on speakers bureaus and for development of educational presentations for Johnson and Johnson Diabetes Institute; and has received grant support from the National Institutes of Health; A. Castillo: has been a consultant for the American Diabetes Association; has received grant support from the National Institutes of Diabetes, Digestive and Kidney Diseases; National Institute on Aging; Centers for Disease Control and Prevention; and has received payment for lectures including service on speakers bureaus for the National Speakers Network L. Quinn: none; M. Hochwert: none.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ruggiero, L., Castillo, A., Quinn, L. et al. Translation of the Diabetes Prevention Program’s Lifestyle Intervention: Role of Community Health Workers. Curr Diab Rep 12, 127–137 (2012). https://doi.org/10.1007/s11892-012-0254-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11892-012-0254-y