Abstract
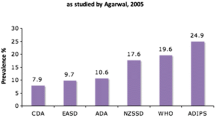
Gestational diabetes mellitus (GDM) is defined as any degree of glucose intolerance with onset or first recognition during pregnancy. The definition of GDM does not preclude the possibility that unrecognized glucose intolerance may have existed before the pregnancy, and the definition applies whether insulin, oral antidiabetic agents, or dietary modification is used for treatment. Approximately 7% of all pregnancies in the United States are complicated by gestational diabetes resulting in more than 200,000 cases annually, but the prevalence ranges from 1% to 14% of all pregnancies depending on the population studied and the diagnostic tests used. Despite the better detection of GDM and recognition of its adverse consequences for mother and baby in many countries, there is still no consensus regarding GDM pathophysiology; as a result, diagnosis and treatment of GDM remain controversial. A better understanding of obesity along with new studies in GDM has identified the intra-abdominal metabolically active adipose tissue as a major factor in the pathophysiology of GDM. This review examines recent research regarding the link between obesity and glucose intolerance and highlights studies in the areas of genetics, glucose transport, and adipokines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gestational diabetes mellitus (GDM) is a relatively common medical condition, complicating approximately 7% of pregnancies in the United States. Despite the high prevalence of GDM and the long time since its identification, its exact pathophysiology is still unclear. This review discusses some new aspects of recent advances regarding GDM pathophysiology. Future understanding of GDM pathophysiology will hopefully lead to worldwide agreement regarding diagnosis and treatment options.
Obstetrical Management of the Pregnancy Complicated by Diabetes
For over 30 years, GDM has been defined as “carbohydrate intolerance of varying degrees of severity with onset or first recognition during pregnancy” [1]. The prevalence of GDM ranges from 1% to 14% of pregnancies depending on the studied population. For example, in the United States, GDM affects 4% of pregnancies, resulting in 135,000 cases each year. Of all pregnancies complicated by diabetes mellitus, GDM represents 90% of the cases [2]. GDM is not “simply impaired glucose tolerance temporarily associated with pregnancy,” as once thought, [3] but a medical condition associated with maternal and fetal morbidity. Excessive fetal growth and its consequences are the main concerns of GDM [4]. Consequences of excessive fetal growth include birth trauma, maternal morbidity from operative delivery, and possible lifelong increased risks of glucose intolerance and obesity in the offspring. The cesarean delivery rate is increased in patients with GDM, in part to avoid birth trauma and to avoid another potential morbidity of shoulder dystocia and newborn asphyxia, both associated with large-for-gestational-age newborns [5, 6]. Other neonatal morbidities that potentially occur more frequently in infants of women with GDM include hypoglycemia, hyperbilirubinemia, hypocalcemia, erythremia, and poor feeding [4]. Although GDM is a very common problem, its exact pathophysiology remains unclear, causing controversies regarding diagnosis and treatment.
GDM Pathophysiology
Insulin resistance is an impaired response to insulin that characterizes normal pregnancy. The physiologic result of insulin resistance is an increase of insulin secretion by the pancreatic β cells. The same metabolic changes characterize obesity, a well-known factor on the path of the metabolic syndrome to the end point of type 2 diabetes mellitus. Women with GDM are unable to increase insulin production to compensate for the increased insulin resistance [7].
Insulin resistance and the relative insulin deficiency due to the pancreatic β-cell deterioration are the primary metabolic changes in GDM, and same process occurs in prediabetes stages of type 2 diabetes mellitus. As β-cell function further declines, hyperglycemia becomes more severe. A total of 40% of β-cell mass may be lost in individuals who have glucose intolerance, and approximately 60% may be lost when clinical type 2 diabetes develops. Moreover, these changes do not affect the pancreas alone. Gluconeogenesis is increased as a result of hepatic insulin resistance and relative insulin deficiency. As a consequence, hyperglycemia is worsened. Understanding the path of the metabolic changes mentioned leads to the conclusion that prediabetes may include patients with metabolic syndrome, GDM, and impaired glucose tolerance—all represent “stations” on the road to type 2 diabetes [8••]. Support for the association between GDM and insulin resistance was recently published [9]. In a large population-based study, we examined lipid profile changes during gestation in pregnancies with and without preeclampsia and/or gestational diabetes (Fig. 1). One of the major findings was that elevated levels of triglycerides during pregnancy are associated with an increased risk for preeclampsia, GDM, and greater birth weight. The metabolic syndrome and insulin resistance as a part of it might explain the findings.
GDM Genetics and Glucose Transport Activity
Several investigators studied the genetics of GDM [10–12] and the genetic relationship with type 2 diabetes mellitus [13]. In a recently published study by Enquobahrie et al. [14], 66 genes were found to participate in cell functions involving cell activation, immune response, organ development, and regulation of cell death, which were differentially expressed in GDM placentas. These studies revealed the association between the abnormal glucose tolerance in GDM and in type 2 diabetes, but reflected the end point of the pathologic process and not the underlying cause of the abnormality.
To understand the pathophysiology, Friedman et al. [15] examined impaired glucose transport and insulin receptor tyrosine phosphorylation in skeletal muscle from obese women with gestational diabetes. Glucose transport activity and the expression and phosphorylation of the insulin receptor and insulin receptor substrate (IRS)-1 in human skeletal muscle fiber strips obtained during cesarean delivery were compared in pregnant women with normal glucose tolerance, women with diagnosed GDM, and nonpregnant women. Compared with nonpregnant control subjects, maximal insulin-stimulated IRS-1 tyrosine phosphorylation was significantly lower in normal pregnancies; in GDM subjects, the IRS-1 tyrosine phosphorylation was the lowest, as reflected by a 23% (P < 0.05) and 44% (P < 0.002) reduction in IRS-1 protein levels in muscle from pregnant control and GDM subjects, respectively. Tyrosine phosphorylation of the insulin receptor was 37% lower (P < 0.05) in GDM subjects than in pregnant control subjects and was not related to changes in the abundance of the insulin receptor. The authors concluded that insulin resistance to glucose transport during pregnancy is uniquely associated with a decrease in IRS-1 tyrosine phosphorylation, primarily due to decreased expression of IRS-1 protein. Nevertheless, in GDM subjects, a decrease in tyrosine phosphorylation of the insulin receptor β subunit is associated with further decreases in glucose transport activity.
Adipokines
The association between obesity and glucose intolerance has been widely studied in recent years. Interest has been focused on a number of adipose tissue-related mediators implicated in the pathogenesis of insulin resistance, such as leptin, adiponectin, and resistin. Adiponectin is an adipocytokine that has been shown to have antiatherogenic, anti-inflammatory, and antidiabetic roles [16]. Chen et al. [17] found that the expression of adiponectin and its receptors is altered in women with GDM and suggested that adiponectin may play a role in adapting energy metabolism at the maternofetal interface. The involvement of adiponectin in insulin resistance during gestation was established by Cortelazzi et al. [18] who measured serum adiponectin and resistin in 30 healthy nonpregnant women, 73 pregnant women including normal pregnancies, pregnancies complicated with GDM, gestational hypertension, preeclampsia, and chronic hypertension. Samples were taken from 40 fetuses as well. In women with GDM, adiponectin levels were significantly lower than those found in nondiabetic women at the same gestational age. No correlation was found between maternal weight and adiponectin or resistin concentration and between maternal resistin and adiponectin concentration. Fetuses of diabetic mothers exhibited significantly lower adiponectin levels compared with normal fetuses of the same gestational age. Regarding adiponectin, the authors concluded that the secretion pattern of adiponectin in normal and complicated pregnancies strongly suggests an involvement of adiponectin in insulin resistance during gestation. The low adiponectin levels in fetuses of diabetic mothers further supports the impact of adiponectin on energy metabolism during gestation.
Resistin, a circulating cytokine, is produced in adipocytes and expressed abundantly in monocytes and macrophages. In animal experiments, resistin induces insulin resistance. The human physiologic effect of the cytokine is less pronounced. Increased serum resistin levels were found in obesity, but controversy exists concerning its role in type 2 diabetes, insulin resistance, and hypertension in humans [19]. Zhou et al. [20] found that resistin was closely related to central obesity, leading to insulin resistance, obesity, and type 2 diabetes mellitus. The relationship between circulating resistin levels and insulin sensitivity in GDM was assessed by Megia et al. [21]. Serum resistin and insulin sensitivity were examined in GDM during and after pregnancy in a total of 58 women undergoing an oral glucose tolerance test. Lower serum resistin levels were observed in GDM compared with normal pregnancies and decreased after parturition, suggesting a role for resistin in the development of this disease. Nevertheless, an independent relationship between resistin levels and insulin sensitivity during pregnancy could not be established, signifying differences in the regulation of resistin levels in pregnancies complicated by diabetes. A recently published study measured maternal serum resistin and insulin levels in 30 patients with GDM compared with 30 normal parturients [22]. In addition, at the time of delivery, umbilical levels of resistin and insulin were measured. No significant difference in maternal serum resistin levels nor in umbilical resistin levels was found. There was no correlation between infant weight and maternal resistin at 24–26 weeks or umbilical resistin levels. These findings correlate well with the previous publication by Cortelazzi et al. [18]. According to these recent studies, resistin seems to play a rather minor role in the pathophysiology of GDM and the energy metabolism during fetal life.
Adipose Tissue Pathogenicity
Obesity has been proposed to impose a variety of stresses on adipose tissue, including inflammatory, metabolic, oxidative, and endoplasmic reticulum stress (Fig. 2) [23•]. It is well established that adipose tissue is a metabolically active tissue. Intra-abdominal fat contributes uniquely to the comorbidity of obesity compared with subcutaneous (SC) fat. Stress signaling pathways constitute phosphorylation-based activation of kinases in response to various intracellular and extracellular stimuli. The activation of the kinases phosphorylates different protein substrates on Ser/Thr residues, thereby altering their function [24]. In addition to the activation of the kinases in the fat tissue, macrophage infiltration into the intra-abdominal omental (OM) fat was observed in different studies. This inflammatory response of OM fat, but not SC fat, correlated with comorbid states of obesity [25, 26]. In a recently published study, Bluher et al. [27••] provided evidence of the ASK1-MKK4-p38 MAPK/JNK stress-sensing pathway in OM fat of obese patients that strongly associates with clinical markers of morbidity and predicts whole-body insulin sensitivity. They suggested a sequence of events in which obesity induces adipose tissue inflammation, which activates apoptosis signal-regulating kinase (ASK1)–mediated signaling in adipose tissue.
Stress signaling in fat tissue by different stress sources. ASK—apoptosis signal-regulating kinase; JNK—c-Jun N-terminal kinase; MAP—mitogen-activated protein; MAPK—mitogen-activated protein kinase; MAPKAP2—mitogen-activated protein kinase-activated protein-2; MKK—mitogen-activated protein kinase kinase; MLK—mixed lineage kinase; TAK—transforming growth factor β-activated kinase
Trying to investigate the stress-sensing pathway in OM fat of pregnant women, at the 29th Society for Maternal-Fetal Medicine annual meeting [28], we presented the results of a study in which we prospectively collected OM and abdominal SC fat samples from 20 women with normal pregnancies and nine GDM pregnancies during cesarean delivery. Tissue lysates were prepared and subjected to quantitative Western blot analyses using p38 mitogen-activated protein (MAP) kinase, phospho-Thr/Tyr (active) p38 MAP kinase, MAP kinase kinase (MKK)4, pMKK4, and anti-adiponectin antibodies, followed by quantification densitometry analysis. Similar to obesity in nonpregnant women, the total expression of p38 MAP kinase was increased nearly twofold in OM compared with SC fat in normal (2.01 ± 0.18 vs 1.16 ± 0.1, P < 0.001, respectively) and GDM (1.25 ± 0.22 vs 1.94 ± 0.38, P = 0.038, respectively) pregnancies, without significant differences between the two groups. However, no differences in the expression of phosphorylated p-p38MAP kinase, or in the expression and phosphorylation of MKK4 (a p38 MAP kinase and JNK kinase), were noted between OM and SC fat, either in normal or in GDM pregnancies. Likewise, GDM pregnancies were not associated with increased adipose tissue p-p38MAP kinase. The known elevated adiponectin expression in OM versus SC fat was not detected in adipose tissue from pregnant women, and GDM was not associated with lower adiponectin expression compared with normal pregnancy. Much to our surprise, we concluded that normal pregnancy, unlike obesity, is not associated with an increased phosphorylation of the stress-responsive signaling pathway involving p38 MAP kinase in OM fat. However, increased expression of the total protein was noted. GDM does not impose increased intra-abdominal fat stress compared with normal pregnancy.
Macrophage Infiltration to the Adipose Tissue
In human obesity, infiltration of fat by macrophages has been reported [29, 30]. However, the contribution of fat tissue macrophages to the pathophysiology of human obesity and its related morbidities is still largely unknown.
An intriguing question is whether macrophage infiltration can be linked to the increased “pathogenicity” of intra-abdominal compared with SC fat. Several indirect lines of evidence exist for increased macrophage infiltration into OM fat [31]. Recently, macrophage infiltration into OM, but not SC, fat was shown to be associated with clinical parameters of obesity comorbidity, as well as with the severity of histologic changes in liver biopsies [32]. Harman-Boehm et al. [25] found that preferential macrophage infiltration into OM fat is a general phenomenon exaggerated by central obesity, potentially linking central adiposity with increased risk of diabetes and coronary heart disease. The association between the macrophage infiltration to the OM adipose tissue and the stress signaling pathway was recently established [27••]. In a study confirming the activated ASK1-MKK4-p38 MAPK/JNK stress signaling pathway, Bluher et al. [27••] reported that the stress signaling pathway in human OM fat tissue may link increased intra-abdominal fat mass and OM macrophage infiltration to impaired whole-body insulin sensitivity. Still, there are no data regarding macrophage infiltration into fat tissue, as well as the expression of proteins and cytokines in OM versus SC fat of pregnant women.
Conclusions
GDM is a significant and growing problem worldwide. Although traditionally deemed not as dangerous for the developing fetus as pregestational diabetes, we now know that GDM has serious, long-term consequences for both baby and mother.
The recent advances in understanding GDM pathophysiology involve the detection of the major role the adipose tissue plays, especially the intra-abdominal OM fat. Obesity imposes stress on this metabolically active tissue, altering its function, and the end point is glucose intolerance, GDM, and type 2 diabetes mellitus. The vast advance in our understanding obesity pathophysiology cannot be directly extrapolated to insulin resistance during pregnancy or GDM because the pathophysiology of the two is not necessarily identical. Therefore, further investigation of the GDM pathophysiology is warranted, parallel to the studies of insulin resistance occurring outside of pregnancy.
The glucose intolerance continuum is a central concept in the diagnosis and treatment of GDM. Our limited understanding of GDM pathophysiology contributes to the controversies regarding GDM diagnosis and treatment.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. National Diabetes Data Group [no authors listed]. Diabetes 1979, 28:1039–1057.
American Diabetes Association: Diagnosis and classification of diabetes mellitus. Diabetes Care 2006, 29(Suppl 1):S43–S48.
Jarrett RJ: Gestational diabetes: a non-entity? BMJ 1993, 306:37–38.
Metzger BE, Buchanan TA, Coustan DR, et al.: Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care 2007, 30(Suppl 2):S251–S260.
Gottlieb AG, Galan HL: Shoulder dystocia: an update. Obstet Gynecol Clin North Am 2007, 34:501–531, xii.
Henriksen T: The macrosomic fetus: a challenge in current obstetrics. Acta Obstet Gynecol Scand 2008, 87:134–145.
Reece EA, Leguizamon G, Wiznitzer A: Gestational diabetes: the need for a common ground. Lancet 2009, 373:1789–1797.
•• Langer O: From educated guess to accepted practice: the use of oral antidiabetic agents in pregnancy. Clin Obstet Gynecol 2007, 50:959–971. This is a review summarizing the current data regarding all oral antidiabetic agents groups for treating GDM, supporting the randomized controlled trial published in 2000 by Langer et al.
Wiznitzer A, Mayer A, Novack V, et al.: Association of lipid levels during gestation with preeclampsia and gestational diabetes mellitus: a population-based study. Am J Obstet Gynecol 2009, 201:482.e1–482.e8.
Shaat N, Groop L: Genetics of gestational diabetes mellitus. Curr Med Chem 2007, 14:569–583.
Shaat N, Karlsson E, Lernmark A, et al.: Common variants in MODY genes increase the risk of gestational diabetes mellitus. Diabetologia 2006, 49:1545–1551.
Shaat N, Lernmark A, Karlsson E, et al.: A variant in the transcription factor 7-like 2 (TCF7L2) gene is associated with an increased risk of gestational diabetes mellitus. Diabetologia 2007, 50:972–979.
Robitaille J, Grant AM: The genetics of gestational diabetes mellitus: evidence for relationship with type 2 diabetes mellitus. Genet Med 2008, 10:240–250.
Enquobahrie DA, Williams MA, Qiu C, et al.: Global placental gene expression in gestational diabetes mellitus. Am J Obstet Gynecol 2009, 200:206.e1–206.e13.
Friedman JE, Ishizuka T, Shao J, et al.: Impaired glucose transport and insulin receptor tyrosine phosphorylation in skeletal muscle from obese women with gestational diabetes. Diabetes 1999, 48:1807–1814.
Pajvani UB, Du X, Combs TP, et al.: Structure-function studies of the adipocyte-secreted hormone Acrp30/adiponectin. Implications fpr metabolic regulation and bioactivity. J Biol Chem 2003, 278:9073–9085.
Chen J, Tan B, Karteris E, et al.: Secretion of adiponectin by human placenta: differential modulation of adiponectin and its receptors by cytokines. Diabetologia 2006, 49:1292–1302.
Cortelazzi D, Corbetta S, Ronzoni S, et al.: Maternal and foetal resistin and adiponectin concentrations in normal and complicated pregnancies. Clin Endocrinol (Oxf) 2007, 66:447–453.
Palik E, Baranyi E, Melczer Z, et al.: Elevated serum acylated (biologically active) ghrelin and resistin levels associate with pregnancy-induced weight gain and insulin resistance. Diabetes Res Clin Pract 2007, 76:351–357.
Zhou Y, Zhang M, Guo W, et al.: Expression of resistin protein in normal human subcutaneous adipose tissue and pregnant women subcutaneous adipose tissue and placenta. J Huazhong Univ Sci Technolog Med Sci 2006, 26:288–291.
Megia A, Vendrell J, Gutierrez C, et al.: Insulin sensitivity and resistin levels in gestational diabetes mellitus and after parturition. Eur J Endocrinol 2008, 158:173–178.
Vitoratos N, Vlahos NF, Gregoriou O, et al.: Maternal and umbilical resistin levels do not correlate with infant birth weight either in normal pregnancies and or in pregnancies complicated with gestational diabetes. J Matern Fetal Neonatal Med 2010 Jan 19 [Epub ahead of print].
• Rudich A, Kanety H, Bashan N: Adipose stress-sensing kinases: linking obesity to malfunction. Trends Endocrinol Metab 2007, 18:291–299. This is a study reviewing the concept of stress signaling in obesity, directing future investigation of different OM tissue stress.
Bashan N, Dorfman K, Tarnovscki T, et al.: Mitogen-activated protein kinases, inhibitory-kappaB kinase, and insulin signaling in human omental versus subcutaneous adipose tissue in obesity. Endocrinology 2007, 148:2955–2962.
Harman-Boehm I, Bluher M, Redel H, et al.: Macrophage infiltration into omental versus subcutaneous fat across different populations: effect of regional adiposity and the comorbidities of obesity. J Clin Endocrinol Metab 2007, 92:2240–2247.
Cancello R, Tordjman J, Poitou C, et al.: Increased infiltration of macrophages in omental adipose tissue is associated with marked hepatic lesions in morbid human obesity. Diabetes 2006, 55:1554–1561.
•• Bluher M, Bashan N, Shai I, et al.: Activated Ask1-MKK4-p38MAPK/JNK stress signaling pathway in human omental fat tissue may link macrophage infiltration to whole-body insulin sensitivity. J Clin Endocrinol Metab 2009, 94:2507–2515. This is an important study establishing the association between stress signaling pathway in human OM fat to obesity and a possible connection to macrophage infiltration.
Harlev A, Rudich A, Bashan N, et al.: Stress-signaling in subcutaneous versus omental adipose tissue in normal and GDM pregnancies: comparison to obesity-associated adipose tissue alterations. Presented at the Society for Maternal-Fetal Medicine 29th Annual Meeting. San Diego, CA; January 26–31, 2009.
Weisberg SP, McCann D, Desai M, et al.: Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 2003, 112:1796–1808.
Cinti S, Mitchell G, Barbatelli G, et al.: Adipocyte death defines macrophage localization and function in adipose tissue of obese mice and humans. J Lipid Res 2005, 46:2347–2355.
Curat CA, Miranville A, Sengenes C, et al.: From blood monocytes to adipose tissue-resident macrophages: induction of diapedesis by human mature adipocytes. Diabetes 2004, 53:1285–1292.
Cancello R, Tordjman J, Poitou C, et al.: Increased infiltration of macrophages in omental adipose tissue is associated with marked hepatic lesions in morbid human obesity. Diabetes 2006, 55:1554–1561.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Harlev, A., Wiznitzer, A. New Insights on Glucose Pathophysiology in Gestational Diabetes and Insulin Resistance. Curr Diab Rep 10, 242–247 (2010). https://doi.org/10.1007/s11892-010-0113-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11892-010-0113-7