Abstract
Type 2 diabetes is associated with a significantly increased risk of cardiovascular disease (CVD) morbidity and mortality. Although several clinical trials have evaluated the effects of interventions to reduce CVD risk in people with diabetes, such studies are primarily conducted to target individual risk factors such as hypertension, hyperglycemia, and dyslipidemia rather than using a multifactorial interventional approach. Existing clinical trial data suggest that intensive multifactorial interventions that target several important risk factors simultaneously result in a significantly greater risk reduction in CVD risk compared with single risk factor interventions. However, few studies have evaluated the efficacy and effectiveness of such interventions on CVD hard end points. A multidisciplinary team management of diabetes should focus on weight control, diet, physical activity, diabetes education, and adherence to pharmacotherapy. An individually tailored aggressive management program to reduce multiple CVD risk factors simultaneously has great potential to prevent CVD morbidity and mortality among patients with type 2 diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
- ACCORD:
-
Action to Control Cardiovascular Disease in Diabetes
- ADDITION:
-
Anglo-Danish-Dutch Study of Intensive Treatment in People with Screen-Detected Diabetes
- ADVANCE:
-
Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation
- NHANES:
-
National Health and Nutrition Examination Survey
- UKPDS:
-
United Kingdom Prospective Diabetes Study
- VADT:
-
Veterans Affairs Diabetes Trial
Introduction
The prevalence of type 2 diabetes mellitus in the United States has dramatically increased over the past few decades, mainly due to the rapid rise in the prevalence of overweight and obesity [1]. The metabolic dysregulation associated with diabetes causes secondary pathophysiologic changes in multiple organ systems that impose a tremendous burden of morbidity and mortality on the individual patient and on the health care system [2]. For example, diabetes is a leading cause of end-stage renal disease, nontraumatic lower extremity amputations, and adult blindness. Furthermore, individuals with diabetes are at a substantially elevated risk of cardiovascular disease (CVD), which is the leading cause of death in this population [3]. The connection between diabetes and macrovascular disease is so strong that the current National Cholesterol Education Program guidelines have elevated diabetes to the level of a “cardiac risk equivalent” [4]. Several studies have shown that the risk of death from CVD among individuals with diabetes is comparable to that among people with a previous history of myocardial infarction [5, 6]. The high burden of CVD in diabetes not only contributes to enormous direct health care costs but also to the indirect costs due to loss of productivity and decreased quality of life [7].
The major modifiable risk factors for CVD in the diabetic population include hypertension, hyperglycemia, dyslipidemia, obesity, smoking, physical inactivity, and unhealthy diet. Pharmacotherapy and lifestyle changes such as weight management, dietary modification, and physical activity are the mainstay for primary prevention of CVD in diabetes. Although several clinical trials have evaluated the effects of interventions to reduce CVD risk in people with diabetes, most of these studies have primarily targeted a single risk factor rather than using an intensive multifactorial approach. In this article, we first discuss individual risk factors for CVD in diabetes and then summarize the existing evidence for the effects of intensive multifactorial interventions targeting multiple risk factors for CVD prevention in patients with diabetes.
CVD Risk Factors in Diabetes
The UKPDS has identified hypertension, smoking, hyperglycemia, and blood lipids as the most important factors for CVD risk in people with diabetes [8]. Meanwhile, other epidemiologic studies have revealed physical inactivity, dietary factors, and body weight as additional modifiable risk factors for the development of CVD in diabetes. Table 1 shows the current clinical recommendations targeting these multiple risk factors [9••].
Hyperglycemia
Several observational studies have shown an association between levels of glycemia and macrovascular events [10], as is the case with microvascular diabetic sequelae, including retinopathy, nephropathy, and neuropathy. The hemoglobin A1c (HbA1c) goal for nonpregnant adults for microvascular disease prevention is less than 7% [9••]. However, less stringent HbA1c goals may be more appropriate for patients with a history of severe hypoglycemia, limited life expectancy, and advanced microvascular or macrovascular complications. Early data from the UKPDS suggested a protective effect of improved glucose control on CVD incidence and mortality [11]. Within the past year, however, three large randomized controlled trials reported conflicting results [12• –14•]. Although the ADVANCE study [13•] and the VADT trial [14•] found no effect of intensive glucose control on major CVD events, the ACCORD trial [12•] suggested an increased risk for CVD death and total mortality among those patients with more intensive glucose control (HbA1c goal of <6.0%). A recent meta-analysis of five trials found that intensive glucose control reduced the risk for nonfatal myocardial infarction, did not reduce or increase the risk for cardiovascular death or all-cause mortality, but increased the risk for severe hypoglycemia in diabetic patients [15•]. Clearly, the benefits and risks of tight glycemic control in diabetes warrant further investigations.
Hypertension
The UKPDS demonstrated that tight blood pressure control (systolic blood pressure > 150 and diastolic blood pressure > 85 mm Hg ) in patients with type 2 diabetes resulted in a clinically important reduction in the risk of deaths related to diabetes, complications related to diabetes, progression of diabetic retinopathy, and deterioration in visual acuity [16]. Although in this study tight control was associated with a nonsignificant reduction in risk of myocardial infarction, several other studies found a significant and substantial reduction in cardiovascular incidence and mortality with tight blood pressure control [17, 18]. The American Diabetes Association guidelines recommend that patients with diabetes should be treated to a target systolic blood pressure of less than 130 mm Hg and diastolic blood pressure of less than 80 mm Hg [9••]. The choice of antihypertensive agents is not necessarily relevant because most patients with diabetes generally require multiple drugs with different mechanisms to achieve blood pressure targets [9••]. The American Diabetes Association recommends that an angiotensin-converting enzyme inhibitor or an angiotensin receptor blocker should be commonly included [9••].
Dyslipidemia
Increased triglycerides and decreased high-density lipoprotein (HDL) cholesterol levels are the hallmark of diabetic dyslipidemia, and both have been associated with increased risk of coronary heart disease (CHD) among diabetic patients. In the UKPDS, increased low-density lipoprotein (LDL) cholesterol and decreased concentrations of HDL cholesterol predict CVD risk [8]. The estimated hazard ratios for the upper third relative to the lower third were 2.26 (95% CI, 1.70–3.00) for LDL and 0.55 (95% CI, 0.41–0.73) for HDL. In terms of the treatment of dyslipidemia, the primary goal is to maintain an LDL cholesterol less than 100 mg/dL in individuals without overt CVD and less than 70 mg/dL in individuals with overt CVD [9••]. However, statin therapy should be recommended regardless of baseline lipid levels for diabetic patients 1) with overt CVD or 2) without CVD who are over the age of 40 years and have one or more CVD risk factors (hypertension, family history, dyslipidemia, microalbuminuria, cardiac autonomic neuropathy, or smoking) [9••]. Triglyceride levels less than 150 mg/dL and HDL cholesterol greater than 40 mg/dL in men and greater than 50 mg/dL in women are considered desirable. Generally, LDL cholesterol-targeted statin therapy is the preferred strategy in the management of diabetic dyslipidemia as recommended by the American Diabetes Association [9••].
Smoking
Cigarette smoking represents one of the most important risk factors for CVD and other chronic diseases worldwide. Smoking contributes to a substantially increased risk of CVD among diabetic patients by a combination of short-term effects (coronary artery spasm, arrhythmias, and increased platelet aggregability) and long-term effects (increased triglycerides, decreased HDL levels, and other metabolic effects that lead to atherogenesis) on the cardiovascular system [19, 20]. Smoking also increases insulin resistance and aggravates metabolic disturbances among diabetic patients [21]. In the Nurses’ Health Study, cigarette smoking markedly augmented the risk of CHD in diabetic women [22]. Compared with never smokers, the relative risks (RRs) for CHD across categories of smoking were 1.21 (95% CI, 0.97–1.51) for past smokers, 1.66 (95% CI, 1.10–2.52) for current smokers of 1 to 14 cigarettes per day, and 2.68 (95% CI, 2.07–3.48) for current smokers of 15 or more cigarettes per day in multivariate analyses (P for trend < 0.0001). The multivariate RR of CHD among diabetic women who had stopped smoking for more than 10 years was similar to that among diabetic women who were never smokers (RR, 1.01 [95% CI, 0.73–1.38]). Results were also similar in the UKPDS; the estimated hazard ratio for CVD comparing smokers with nonsmokers was 1.41 (1.06–1.88) [8].
The results from the Nurses’ Health Study indicate that the risk of CHD attributable to smoking among diabetic women was 19%. Thus, smoking cessation can have an important effect on CHD risk reduction among diabetic patients at least as great as those of standard interventions including cholesterol lowering, high blood pressure lowering, and glycemic control. Given that cigarette smoking is such a strong, yet modifiable risk factor for CHD among diabetic individuals, special emphasis should be given by physicians to discourage their diabetic patients from smoking.
Body Weight
In patients with type 2 diabetes, weight loss improves insulin resistance and glycemic control [23]. In a review of 33 studies of obese patients with type 2 diabetes, hypertension, or hypercholesterolemia, moderate weight loss (< 10% of initial body weight) improved the cardiovascular risk factor profile, including glycemic control, in nondiabetic and diabetic individuals [24]. Despite favorable data on weight loss in short-term studies, the results on the relationship of obesity and weight loss among diabetic individuals from long-term prospective studies have been inconsistent [25, 26]. The Nurses’ Health Study reported that obesity and weight gain before diagnosis of diabetes were associated with future risk of CHD among women with type 2 diabetes, although obesity after diagnosis of diabetes was less predictive [27].
One major problem with observational studies is that they often cannot distinguish voluntary from involuntary weight loss, and thus the benefit of intentional weight loss could be confounded by unintentional weight loss from severity of diabetes. Nonetheless, the available evidence suggests that aiming for modest or moderate weight loss among diabetic patients with obesity is warranted when larger reductions in body weight are difficult to achieve and/or maintain.
Dietary Factors
Dietary macronutrient composition is an important consideration for medical nutrition therapy in diabetes. In epidemiologic studies, higher intakes of saturated and trans fats are associated with increased risk, whereas higher intakes of monosaturated and polyunsaturated fats are associated with decreased risk. The Nurses’ Health Study [28] estimated that replacement of 5% of energy from saturated fat by unsaturated fats would reduce coronary risk by 42% (23 to 56; P < 0.001), and replacement of 2% of energy from trans fat by unhydrogenated unsaturated fats would reduce risk by 53% (34 to 67; P < 0.001). In contrast, substituting carbohydrates for saturated fat was associated with a nonsignificant 14% reduction in CHD risk.
The optimal amount of polyunsaturated fat in the diet is still a matter of debate. It is commonly recommended that intake of polyunsaturated fat should not exceed 10% of energy, although no scientific evidence exists to support such an upper limit. Evidence is equally sparse regarding benefits of very high polyunsaturated fat intake, but earlier intervention trials using high polyunsaturated fat diets (up to 20% energy) significantly reduced CHD incidence and mortality in largely nondiabetic populations [29].
Regular consumption of fish (eg, 1-2 servings/wk), especially species higher in the omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid, reduced risk of coronary death and total mortality in epidemiologic studies and randomized clinical trials [30]. The protective effects of fish omega-3 fatty acids are probably from multiple mechanisms, including reducing triglyceride levels, reducing platelet aggregation, anti-inflammatory effects, and antiarrhythmic effects. There is some epidemiologic evidence that higher consumption of fish omega-3 fatty acids reduces risk of CVD mortality in patients with diabetes [31].
Recent studies conveyed the importance of consuming minimally processed foods with low glycemic index and glycemic load (GL) values in the prevention and management of diabetes [32, 33]. Several large cohort studies found a strong positive association between dietary GL and incidence of type 2 diabetes [33, 34] and CHD [35]. The increased risk was more pronounced among overweight and obese women, suggesting that the adverse effects of a high GL diet are probably aggravated by underlying insulin resistance. Whole grain products such as whole wheat breads, brown rice, oats, and barley tend to produce lower glycemic and insulinemic responses than highly processed refined grains. Minimally processed whole grains are also rich in fiber, antioxidant vitamins, magnesium, and phytochemicals. Several large prospective cohort studies found an inverse association between whole grain consumption and risk of diabetes [36, 37] and CHD [38, 39].
The inverse association between moderate alcohol consumption (eg, 1-2 drinks or 10–20 g of alcohol per day) and CHD in the general population is well known [40]. Similar findings have been observed among people with diabetes [41]. The mechanisms responsible for the beneficial effects of alcohol are likely to be increased HDL cholesterol, decreased coagulation (decreased platelet aggregation, decreased fibrinogen, increased tissue plasminogen activator, decreased plasminogen activator inhibitor type 1), and enhanced insulin sensitivity [42]. A major concern with alcohol consumption among individuals with diabetes is the potential danger of hypoglycemia, especially among those who use sulfonylureas. However, several clinical studies have shown no appreciable alteration of glucose homeostasis in diabetic patients when moderate alcohol is consumed with meals [43]. For diabetic patients who choose to drink, light to moderate drinking (eg, 1-2 glasses of wine per day) with a meal should not be discouraged.
Physical Activity
Several studies have indicated that higher leisure-time physical activity is associated with reduced total and CVD mortality among patients with diabetes or impaired glucose tolerance [44–46]. Many mechanisms are thought to mediate this association, including effects on insulin sensitivity, lipoprotein metabolism, blood pressure, fibrinolytic activity, and hemostatic function [47]. Exercise levels that are safe for the diabetic patient and are easily attainable may be sufficient to achieve clinically important risk reductions in diabetes. Some diabetic complications limit activity levels or prohibit certain types of activity. For example, weightlifting or high-impact aerobics are contraindicated in retinopathy [48]. Thus, early initiation of a moderate exercise program may be the best strategy for reducing risk of later macrovascular complications.
Trials of Intensive Multifactorial Intervention in Diabetes
As mentioned earlier, only a few trials have evaluated the effect of intensive interventions simultaneously targeting multiple CVD risk factors in people with diabetes. Here we review intervention strategies and main results from three such trials.
The Steno-2 Study
The Danish Steno-2 study was the first long-term trial among people with type 2 diabetes to evaluate the impact of an intensified, multitargeted intervention compared with conventional multifactorial treatment on CVD and its risk factors [49]. In this trial, investigators recruited 80 patients with type 2 diabetes and microalbuminuria to receive conventional treatment in accordance with national guidelines, whereas another group of 80 patients were assigned to an intensified, integrated treatment targeting a series of modifiable risk factors. Patients randomized to intensive therapy were followed up by a diabetes team consisting of a nurse, a clinical dietician, and a physician. The intensive intervention involved a stepwise introduction of lifestyle and pharmacologic interventions aimed at maintaining HbA1c less than 6.5%, blood pressure less than 130/80 mm Hg, total fasting serum cholesterol less than 175 mg/dL, and fasting serum triglycerides less than 150 mg/dL. At each 3-month consultation, measurements of clinical (blood pressure, body mass index, waist and hip circumference, smoking status) and biochemical variables (HbA1c, fasting serum cholesterol, HDL, triglycerides, and urinary albumin excretion rate) were performed and the treatment was adjusted accordingly.
To sustain the long-term motivation for this integrated and aggressive approach, the patients were educated about the rationale for the prescribed polypharmacy and the behavioral modification at each consultation. Dietary intervention was concentrated on qualitative changes in diet including reduced intake of animal fat, increased omega-3 fatty acid-rich food items, and increased daily intake of fruit and vegetables. At each consultation, patients were encouraged to give up smoking; structured antismoking courses for smokers in the intensive therapy group and their spouses were held throughout the follow-up period. The patients were continuously motivated to increase their physical leisure-time activity. Generally, treatment goals for smoking and exercise were similar in the two treatment arms.
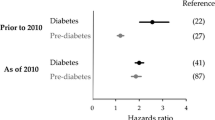
The primary composite end point of this study was death from CVD, nonfatal myocardial infarction, nonfatal stroke, coronary artery bypass grafting, revascularization, and amputation. At a mean follow-up of 7.8 years, patients receiving the intensive therapy showed a 53% (95% CI, 27–76) reduction in risk of CVD (Fig. 1). In addition, there was also a risk reduction for diabetic complications, including 61% for nephropathy (95% CI, 13–83), 58% for retinopathy (95% CI, 14–79), and 63% for autonomic neuropathy (95% CI, 21–82). Risk reductions in the primary cardiovascular end point were observed in all of the different components except mortality, possibly because of lack of statistical power. However, subsequent additional observational follow-up (mean, 5.5 years) of these study participants suggested that intensive therapy was associated with a 46% risk reduction in risk of total mortality (95% CI, 11–68), suggesting a sustained beneficial effect of intensive multifactorial therapy [50••]. The number needed to treat in the Steno-2 study was 5, (ie, one CVD event will be prevented in every five patients treated intensively for 7.8 years). The absolute risk reduction in the Steno-2 trial was considerably higher compared with that observed in trials targeting single risk factors [11, 16, 51].
Results of the Steno-2 study. Kaplan-Meier estimates of the composite end point of death from cardiovascular causes, nonfatal myocardial infarction, coronary artery bypass grafting, percutaneous coronary intervention, nonfatal stroke, amputation, or surgery for peripheral atherosclerotic artery disease in the conventional therapy group and the intensive therapy group. No.—number. (From Gaede et al. [50••]; with permission.)
The ADDITION Study
The ADDITION study is an ongoing international trial [52], with a treatment concept and end points similar to the Steno-2 protocol. The overall aim of the ADDITION study is to evaluate screening methods for prevalent undiagnosed type 2 diabetes, and to develop and evaluate optimized intensive treatment of diabetes and associated risk factors among people 40 to 69 years of age. The ADDITION investigators recently evaluated changes in CVD risk factor profile at the end of 1 year of follow-up among 79 general practices in the southwestern region of the Netherlands [53••]. The analysis was performed among 243 participants on conventional treatment according to current national guidelines and 255 participants on intensive multifactorial treatment. The intensive treatment consisted of pharmacologic treatment combined with lifestyle education to achieve HbA1c less than 7.0%, blood pressure less than 135/85 mm Hg, and total cholesterol less than 190 mg/dL (175.0 mg/dL in the presence of CVD). Changes in body mass index were 0.2 (routine care) versus -1.4 kg/m2 (intensified treatment) (P < 0.001); systolic blood pressure: −19 versus −33 mm Hg (P < 0.001); diastolic blood pressure: -7 versus -12 mm Hg (P < 0.001); HbA1c: -0.9% versus -1.1% (P = 0.03); cholesterol: -19.3 versus -46.4 mg/dL (P < 0.001); HDL cholesterol: 3.9 versus 0.1 mg/dL (P = 0.26); LDL cholesterol: -0.5 versus -1.0 mg/dL (P < 0.001); and triglycerides: -0.3 versus -0.4 mg/dL (P = 0.71). However, there was no difference in health-related quality of life between the two groups at the end of the first year. Overall, the 1-year data indicated that the intensive multilevel intervention resulted in a significant reduction in CVD risk factors without worsening health-related quality of life at the end of first year of follow-up [53••]. The data on incident CVD and mortality from this trial are not yet available.
The Look AHEAD Study
The Look AHEAD trial is a multicenter, randomized clinical trial that evaluates the effectiveness of intentional weight loss in reducing CVD events among patients with type 2 diabetes. The participants include 5145 individuals with type 2 diabetes, 45 to 74 years of age, with BMI greater than 25 kg/m2 (> 27 kg/m2 if taking insulin). An intensive lifestyle intervention (ILI) involving group and individual meetings to achieve and maintain weight loss through decreased caloric intake and increased physical activity was compared with a diabetes support and education (DSE) program. Although the study is focused on weight loss, its findings are relevant for multilevel intervention effects on CVD risk factors in diabetes. Similar to the ADDITION study, the Look AHEAD investigators conducted an interim analysis to evaluate changes in risk profile at the end of 1 year [54••]. Participants assigned to the ILI lost an average 8.6% of their initial weight versus 0.7% in the DSE group (P < 0.001). A greater proportion of ILI participants had reductions in glycemia, hypertension, and lipids, which resulted in decreased requirement of pharmacologic therapy. The mean HbA1c dropped from 7.3% to 6.6% in the ILI versus from 7.3% to 7.2% in the DSE group (P < 0.001). Systolic and diastolic pressure, triglycerides, HDL cholesterol, and urine albumin-to-creatinine ratio improved significantly more in ILI than DSE participants (all P < 0.01).
In summary, the above three trials suggest a benefit of an intensive multifactorial approach for CVD prevention in diabetes. The Steno-2 study showed benefit on CVD incidence and mortality, and such results from ADDITION and Look AHEAD are still awaited. Both these latter studies, however, provide evidence that an intensive multifactorial approach helps better control CVD risk factors. The effect of multifactorial intervention in diabetes may be dependent on the time point in the natural history of diabetes when the interventions are initiated. The Steno-2 trial was conducted in patients with existing diabetes, whereas the ADDITION study is being conducted among those with newly detected diabetes through screening procedures.
Clinical and Public Health Relevance
The current emphasis on early diagnosis, diabetes education, technological advances in glucose monitoring, and the availability of a wide range of therapeutic regimens with better adverse risk profile make it easier to achieve optimal glycemic control and control of CVD risk factors among diabetic patients. However, the level of aggressiveness of therapy should be tailored to the patient situation. The benefits of intensive control of risk factors need to consider issues related to cost and the availability of resources. In addition, the risk of hypoglycemia and other adverse effects need to be taken into account, especially in light of the results from the ACCORD and ADVANCE trials. Because some of the treatment modalities in the intensive multifactorial approach are preventive strategies involving diet and lifestyle, they can have a broader beneficial impact on health outcomes and quality of life [55]. Finally, the cost-effectiveness of a multifactorial approach deserves a great deal of attention. In the Steno-2 study, the discounted quality-adjusted life expectancy was 1.66 quality-adjusted life years (QALY) higher for intensive compared with conventional treatment, resulting in an incremental cost-effectiveness of €2538 per QALY gained [56].
An important aim of the multifactorial intervention approach is to provide patients with the knowledge and skills of self-care and to motivate the patient to become a partner in diabetes management. Therefore, diabetes educators and dieticians or nutritionists play an integral role in the management team. Recommending an overall pattern of dietary intake focusing on appropriate food choices might be easy for the patients to interpret or translate medical nutrition therapy guidelines into practical diets. In addition, smoking cessation and regular physical activity should be emphasized in the management protocols.
Recent analysis of the NHANES examined whether HbA1c, blood pressure, and cholesterol values changed for US adults with diagnosed diabetes between 1988 to 1994 and 2005 to 2006 [57]. Results indicated that HbA1c fell by 0.68% among US adults with diagnosed diabetes. Among those with diabetes and hypertension, systolic and diastolic blood pressure fell by 5.7 and 8.2 mm Hg, respectively. Among those with diabetes and high cholesterol, total cholesterol decreased by 36.4 mg/dL. These improvements would increase life expectancy for persons with newly diagnosed diabetes by 1 year due to better prognosis compared with individuals more than a decade ago. These estimations are consistent with a recent study conducted in the United Kingdom [58]. The possible explanations for this change include improved multifactorial diabetes management by following more specific clinical guidelines, better health care delivery, enhanced public health education, and the availability of more efficacious pharmacotherapeutic agents. These data indicate that an intensive multifactorial approach could further result in reduction in risk of developing complications among people with diabetes.
Conclusions
Current evidence supports potential benefits of an intensive multifactorial management on CVD risk reduction in individuals with diabetes. However, few studies have evaluated the efficacy and effectiveness of such interventions on CVD hard end points. Both pharmacologic agents and lifestyle changes are important to achieve the target levels of risk factors, while also considering potential detrimental effects of stringent management goals, especially those related to tight glycemic control. A multidisciplinary team management of diabetes should focus on weight control, diet, physical activity, diabetes education, and adherence to pharmacotherapy for the reduction of CVD risk.
References
Papers of particular interest, published recently, have been highlighted as follows: • Of importance •• Of major importance
Gregg EW, Cheng YJ, Narayan KM, et al.: The relative contributions of different levels of overweight and obesity to the increased prevalence of diabetes in the United States: 1976–2004. Prev Med 2007, 45:348–52.
Pickup J, Williams G, eds: Textbook of Diabetes, edn 3. Malden, MA: Blackwell Science; 2003.
National Institutes of Health: Diabetes in America, edn 2. Washington, DC: National Institutes of Health; 1995. NIH Publication No. 95–1468.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults: Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001, 285:2486–2497.
Cho E, Rimm EB, Stampfer MJ, et al.: The impact of diabetes mellitus and prior myocardial infarction on mortality from all causes and from coronary heart disease in men. J Am Coll Cardiol 2002, 40:954–960.
Haffner SM, Lehto S, Ronnemaa T, et al.: Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 1998, 339:229–234.
Rubin RJ, Altman WM, Mendelson DN: Health care expenditures for people with diabetes mellitus, 1992. J Clin Endocrinol Metab 1994, 78:809A–809F.
Turner RC, Millns H, Neil HA, et al.: Risk factors for coronary artery disease in non-insulin dependent diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS: 23). BMJ 1998, 316:823–828.
•• American Diabetes Association: Standards of medical care in diabetes–2009. Diabetes Care 2009, 32(Suppl 1):S13–S61. This paper provides the current recommendations of the American Diabetes Association for the management of CVD in diabetes.
Wild SH, Dunn CJ, McKeigue PM, Comte S: Glycemic control and cardiovascular disease in type 2 diabetes: a review. Diabetes Metab Res Rev 1999, 15:197–204.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998, 352:837–853.
• Gerstein HC, Miller ME, Byington RP, et al.: Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008, 358:2545–2559. This paper provides results from the ACCORD trial that evaluated the effects of intensive glycemic control on cardiovascular risk in diabetes.
• Patel A, MacMahon S, Chalmers J, et al.: Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008, 358:2560–2572. This paper provides results from the ADVANCE trial that evaluated the effects of intensive glycemic control on cardiovascular risk in diabetes.
• Duckworth W, Abraira C, Moritz T, et al.: Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009, 360:129–139. This paper provides results from the VADT trial that evaluated the effects of intensive glycemic control on cardiovascular risk in diabetes.
• Kelly TN, Bazzano LA, Fonseca VA, et al.: Systematic review: glucose control and cardiovascular disease in type 2 diabetes. Ann Intern Med 2009, 151:394–403. This meta-analysis summarized results from five clinical trials that evaluated the effects of tight glucose control on CVD morbidity and mortality in diabetes.
Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group [no authors listed]. BMJ 1998, 317:703–713.
Hansson L, Lindholm LH, Niskanen L, et al.: Effect of angiotensin-converting-enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension: the Captopril Prevention Project (CAPPP) randomised trial. Lancet 1999, 353:611–616.
Curb JD, Pressel SL, Cutler JA, et al.: Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. Systolic Hypertension in the Elderly Program Cooperative Research Group. JAMA 1996, 276:1886–1892.
Dean JD, Matthews SB, Dolben J, et al.: Cholesterol rich apo B containing lipoproteins and smoking are independently associated with macrovascular disease in normotensive NIDDM patients. Diabet Med 1994, 11:740–747.
Jonas MA, Oates JA, Ockene JK, Hennekens CH: Statement on smoking and cardiovascular disease for health care professionals. American Heart Association. Circulation 1992, 86:1664–1669.
Haire-Joshu D, Glasgow RE, Tibbs TL: Smoking and diabetes. Diabetes Care 2004, 27(Suppl 1):S74–S75.
Al-Delaimy WK, Manson JE, Solomon CG, et al.: Smoking and risk of coronary heart disease among women with type 2 diabetes mellitus. Arch Intern Med 2002, 162:273–279.
Torjesen PA, Birkeland KI, Anderssen SA, et al.: Lifestyle changes may reverse development of the insulin resistance syndrome. The Oslo Diet and Exercise Study: a randomized trial. Diabetes Care 1997, 20:26–31.
Goldstein DJ: Beneficial health effects of modest weight loss. Int J Obes Relat Metab Disord 1992, 16:397–415.
Chaturvedi N, Fuller JH: Mortality risk by body weight and weight change in people with NIDDM. The WHO Multinational Study of Vascular Disease in Diabetes. Diabetes Care 1995, 18:766–774.
Lean ME, Powrie JK, Anderson AS, Garthwaite PH: Obesity, weight loss and prognosis in type 2 diabetes. Diabet Med 1990, 7:228–233.
Cho EY, Manson JE, Stampfer MJ, et al.: A prospective study of obesity and risk of coronary heart disease among diabetic women. Diabetes Care 2002, 25:1142–1148.
Hu FB, Stampfer MJ, Manson JE, et al.: Dietary fat intake and the risk of coronary heart disease in women. N Engl J Med 1997, 337:1491–1499.
Hu FB, Manson JE, Willett WC: Types of dietary fat and risk of coronary heart disease: a critical review. J Am Coll Nutr 2001, 20:5–19.
Mozaffarian D, Rimm EB: Fish intake, contaminants, and human health: evaluating the risks and the benefits. JAMA 2006, 296:1885–1899.
Hu FB, Cho E, Rexrode KM, et al.: Fish and long-chain omega-3 fatty acid intake and risk of coronary heart disease and total mortality in diabetic women. Circulation 2003, 107:1852–1857.
Wolever TMS, Nuttall FQ, Lee R, et al.: Prediction of the relative blood-glucose response of mixed meals using the white bread glycemic index. Diabetes Care 1985, 8:418–428.
Salmeron J, Manson JE, Stampfer MJ, et al.: Dietary fiber, glycemic load, and risk of non-insulin-dependent diabetes mellitus in women. JAMA 1997, 277:472–477.
Salmeron J, Ascherio A, Rimm EB, et al.: Dietary fiber, glycemic load, and risk of NIDDM in men. Diabetes Care 1997, 20:545–550.
Liu S, Willett WC, Stampfer MJ, et al.: A prospective study of dietary glycemic load, carbohydrate intake, and risk of coronary heart disease in US women. Am J Clin Nutr 2000, 71:1455–1461.
Liu S, Manson JE, Stampfer MJ, et al.: A prospective study of whole-grain intake and risk of type 2 diabetes mellitus in US women. Am J Public Health 2000, 90:1409–1415.
Meyer KA, Kushi LH, Jacobs DR Jr, et al.: Carbohydrates, dietary fiber, and incident type 2 diabetes in older women. Am J Clin Nutr 2000, 71:921–930.
Jacobs DR Jr, Meyer KA, Kushi LH, Folsom AR: Whole-grain intake may reduce the risk of ischemic heart disease death in postmenopausal women: the Iowa Women’s Health Study. Am J Clin Nutr 1998, 68:248–257.
Liu S, Stampfer MJ, Hu FB, et al.: Whole-grain consumption and risk of coronary heart disease: results from the Nurses' Health Study. Am J Clin Nutr 1999, 70:412–419.
Rimm EB, Williams P, Fosher K, et al.: Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors. BMJ 1999, 319:1523–1528.
Rajpathak SN, Freiberg MS, Wang C, et al.: Alcohol consumption and the risk of coronary heart disease in postmenopausal women with diabetes: Women's Health Initiative Observational Study. Eur J Nutr 2009 Oct 13 (Epub ahead of print).
Rimm EB, Klatsky A, Grobbee D, Stampfer MJ: Review of moderate alcohol consumption and reduced risk of coronary heart disease: is the effect due to beer, wine, or spirits? BMJ 1996, 312:731–736.
Koivisto VA, Tulokas S, Toivonen M, et al.: Alcohol with a meal has no adverse effects on postprandial glucose homeostasis in diabetic patients. Diabetes Care 1993, 16:1612-1614.
Hu FB, Stampfer MJ, Solomon C, et al.: Physical activity and risk for cardiovascular events in diabetic women. Ann Intern Med 2001, 134:96–105.
Gregg EW, Gerzoff RB, Caspersen CJ, et al.: Relationship of walking to mortality among US adults with diabetes. Arch Intern Med 2003, 163:1440–1447.
Tanasescu M, Leitzmann MF, Rimm EB, Hu FB: Physical activity in relation to cardiovascular disease and total mortality among men with type 2 diabetes. Circulation 2003, 107:2435–2439.
Hardman A: Physical activity and cardiovascular risk. J Cardiovasc Risk 1995, 2:285–288.
Aiello LP, Cahill MT, Wong JS: Systemic considerations in the management of diabetic retinopathy. Am J Ophthalmol 2001, 132:760–776.
Gaede P, Vedel P, Larsen N, et al.: Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med 2003, 348:383–393.
•• Gaede P, Lund-Andersen H, Parving HH, Pedersen O: Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 2008, 358:580–591. This paper presented the results from the Steno-2 study on mortality. The Steno-2 study was the first randomized trial to evaluate the effect of intensified multifactorial intervention on risk of CVD in patients with diabetes. The data indicated that this approach resulted in better management of CVD risk factors and a significant reduction in CVD mortality compared with the conventional treatment.
Heart Protection Study Collaborative Group: MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002, 360:7–22.
Lauritzen T, Griffin S, Borch-Johnsen K, et al.: The ADDITION study: proposed trial of the cost-effectiveness of an intensive multifactorial intervention on morbidity and mortality among people with type 2 diabetes detected by screening. Int J Obes Relat Metab Disord 2000, 24(Suppl 3):S6–S11.
•• Janssen PG, Gorter KJ, Stolk RP, Rutten GE: Randomised controlled trial of intensive multifactorial treatment for cardiovascular risk in patients with screen-detected type 2 diabetes: 1-year data from the ADDITION Netherlands study. Br J Gen Pract 2009, 59:43–48. This article provides results from the ADDITION study showing that intensive multifactorial intervention results in the improvement in levels of traditional CVD risk factors among newly diagnosed patients with diabetes.
•• Pi-Sunyer X, Blackburn G, Brancati FL, et al.: Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care 2007, 30:1374–1383. The article provides results from the Look AHEAD study on cardiovascular risk profile changes at 1 year. It demonstrated that the intensive multifactorial intervention led to a greater weight loss and a significant improvement in CVD risk factors compared with the control group.
Gaede P, Pedersen O: Multi-targeted and aggressive treatment of patients with type 2 diabetes at high risk: what are we waiting for? Horm Metab Res 2005, 37(Suppl 1):76–82.
Gaede P, Valentine WJ, Palmer AJ, et al.: Cost-effectiveness of intensified versus conventional multifactorial intervention in type 2 diabetes: results and projections from the Steno-2 study. Diabetes Care 2008, 31:1510–1515.
Hoerger TJ, Zhang P, Segel JE, et al.: Improvements in risk factor control among persons with diabetes in the United States: evidence and implications for remaining life expectancy. Diabetes Res Clin Pract 2009, 86:225–232.
Leal J, Gray AM, Clarke PM: Development of life-expectancy tables for people with type 2 diabetes. Eur Heart J 2009, 30:834–839.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rajpathak, S.N., Aggarwal, V. & Hu, F.B. Multifactorial Intervention to Reduce Cardiovascular Events in Type 2 Diabetes. Curr Diab Rep 10, 16–23 (2010). https://doi.org/10.1007/s11892-009-0084-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11892-009-0084-8