Abstract
Purpose of Review
Stroke prevention is the cornerstone of atrial fibrillation (AF) management and the anticoagulation decision is currently based on CHA2DS2-VASc risk score. We discuss several novel risk factors besides those included in CHA2DS2-VASc score and alternative models for stroke prediction.
Recent Findings
Several clinical markers including obstructive sleep apnea and renal failure, laboratory markers like brain natriuretic peptide, imaging criteria including left atrial appendage morphology, spontaneous echo contrast, and coronary artery calcium score may predict stroke in AF patients. Addition of African American ethnicity to CHA2DS2-VASc score also improves stroke prediction in AF. Finally, novel models including TIMI-AF score, ATRIA score, and GARFIELD-AF scores have potential roles in risk stratification for stroke.
Summary
While CHA2DS2-VASc score is the currently recommended risk stratification model for stroke prediction in AF, use of additional clinical, laboratory, imaging markers, ethnicity, and novel stroke prediction models may further assist in decision to anticoagulate the AF patient for stroke prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction: Stroke and Atrial Fibrillation
Stroke affects 795,000 individuals annually in the USA alone, of which 610,000 are first episodes [1]. It is responsible for about “1 of every 19 deaths in the USA” and marks the fifth most common cause of death [1]. Among stroke subtypes, 87% are ischemic, with increasing prevalence in recent decades, and this burden is borne by low- and middle-income countries [1, 2].
The most noteworthy risk factor for stroke, especially for cardioembolic stroke, is atrial fibrillation (AF) [1, 3, 4]. AF affects between 2.7 and 6.1 million individuals in the USA (2010 data) and up to 46.3 million individuals worldwide (2016 data, including atrial flutter) [1]. The prevalence of AF in the USA is projected to more than double in the coming decades [3,4,5], reaching 12.1 million by 2030 [1]. It has a lifetime incidence of 25% for patients over age 40 [1, 6], with approximately 1 in 3 individuals of European ancestry and 1 in 5 black individuals having a lifetime risk of AF [1].
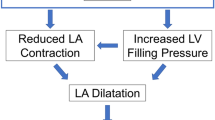
AF predicts ischemic stroke severity, recurrence, and mortality [1], and it confers a threefold to fivefold increased risk of stroke at all ages after adjustment for risk factors [1, 4, 6, 7]. In fact, an increasing percentage of strokes are attributable to AF per decade one ages [1, 5]. AF independently accounts for 15–20% of all strokes in the USA [7, 8], and mortality rates are higher among patients with AF-related stroke (50%) than those with non-AF-related stroke (27%) [4]. The pathophysiology of cardioembolic stroke in AF is primarily due to stasis in the left atrium (LA) and left atrial appendage (LAA). In fact, the LAA is the most common location for thrombus formation, accounting for 90% of LA thrombi [9]. When combined with hypercoagulability and endothelial dysfunction, all parts of Virchow’s triad are affected, which further promotes thrombus formation [9,10,11]. Despite numerous mechanisms, stroke in AF is preventable with anticoagulation and alternatively with the use of left atrial appendage closure (LAAC) devices in patients who are not candidates for long-term anticoagulation [12]. Thus, it is crucial to risk stratify patients who have AF to reduce the incidence of cardioembolic stroke.
Risk Stratification with CHADS2 and CHA2DS2-VASc
CHADS2 Score
The CHADS2 score, developed in 2001 [13], gave one point to each of congestive heart failure (CHF), hypertension, age 75 years or older, and diabetes mellitus (DM) and two points to patients with a previous stroke or transient ischemic attack (TIA) (Table 1) [13]. However, CHADS2 had major limitations including the underestimation of true stroke risk in patients with a low score [14, 15]. In a study of 541 patients who had AF for > 48 h, 10% of patients having a CHADS2 score of 0 had a left atrial appendage (LAA) thrombus on transesophageal echocardiogram (TEE) [16]. Furthermore, not all risk factors contributing to a CHADS2 score of 1 were truly equivalent. For example, age ≥ 75 had a higher stroke risk than age 65–74 years [14]. Thus, the CHADS2 score fell out of favor as the CHA2DS2-VASc score became the evidence-based risk-stratification model for stroke prediction in AF patients.
CHA2DS2-VASc Score
Initially proposed in 2010, the CHA2DS2-VASc score gives one point for age 65 to 74, and two points for age 75 or more—in addition to the risk factors defined by CHADS2. It also adds one point each for vascular disease and female sex (Table 1). It was initially validated in the Swedish Atrial Fibrillation cohort study [17]. The study compared CHA2DS2-VASc score with CHADS2 score in 90,490 patients with non-valvular AF who never received anticoagulation. Over an average follow-up of 1.5 years, CHA2DS2-VASc performed marginally better than CHADS2 at predicting the composite of thromboembolism (ischemic stroke and a composite of “ischemic stroke, unspecified stroke, TIA, and systemic embolism” [17]. The c-statistics for the CHADS2 and CHA2DS2-VASc schemes were 0.66 (0.65–0.66) and 0.67 (0.67–0.68), respectively. More importantly, CHA2DS2-VASc was better than CHADS2 score at identifying truly low-risk patients for stroke.
Another study of 7384 patients with non-valvular AF from the Japanese J-RHYTHM Registry found a similar frequency of thromboembolic events in patients with a CHA2DS2-VASc score of 0 in the warfarin and non-warfarin groups [18]; this suggests that these patients are truly low-risk and may not benefit from anticoagulation.
Guideline-Directed Anticoagulation
The CHA2DS2-VASc score first became part of guideline-directed medical therapy as part of the 2012 European Society of Cardiology (ESC) updated guidelines [19] for the management of AF as well as the 2014 American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) Guideline for the Management of Patients with AF [12]. Current recommendations are based on the 2016 ESC Guidelines and the 2019 AHA/ACC/HRS focused update for AF management [12]. Both the European and US guidelines specifically recommend risk stratification with the CHA2DS2-VASc score, further specifying that a score of ≥ 2 in males and ≥ 3 in females warrants oral anticoagulation (AC), barring contraindications [12, 20]. Both delineate that AC may be considered for males with a score of 1 and females with a score of 2 [12, 20].
Limitations of the CHA2DS2-VASc Score
Despite evidence in its favor, there are many limitations of CHA2DS2-VASc score. First, it does not distinguish between the types of AF. Studies have demonstrated that patients have higher rates of stroke or TIA with persistent AF compared with paroxysmal-type AF [21,22,23]. Another study demonstrated that anticoagulation may not benefit populations with secondary causes of AF [24], but the CHA2DS2-VASc score treats all types of AF the same.
Second, CHA2DS2-VASc does not consider many physiological contributors to AF and stroke risk. It fails to consider not only the size of the LA and shape of the LAA [9, 25] but also—despite being the major physiological mechanism for stroke in AF—ignores thrombus presence in the LA altogether [26].
The score additionally does not accurately risk-stratify patients in some subpopulations. For example, females are given one point regardless of age even though stroke risk is age-dependent [12]. Hence, the recent guidelines do not recommend anticoagulation in females with a CHA2DS2-VASc score of 1 [12]. Also, the score has not been validated in an ethnically diverse population, so African-Americans and Hispanics are treated the same as those of European descent despite differing levels of risk [8, 27,28,29].
While CHA2DS2-VASc may be better at identifying truly low-risk patients, its scoring capacity is not discriminatory enough for truly high-risk, elderly patients. Thus, it should be considered in the context of its limitations.
Stroke Risk in AF: Beyond the CHA2DS2-VASc Score
Clinical Risk Factors
Obstructive Sleep Apnea
There is a strong, independent association between stroke and OSA [30,31,32,33,34] as well as between OSA and AF [34,35,36,37]. Up to 70% of stroke patients have concurrent OSA, while only about 4% of the general population has OSA [30, 31]. There is also a dose-response relationship between OSA and stroke, such that moderate-to-severe disease is associated with an increased risk of stroke [32, 34]. A study of 53 patients found that cardioembolic stroke was higher among patients with OSA than in controls (p = 0.01) [35].
Among AF patients, those with OSA have a higher risk of hospitalization and worse prognosis post-stroke but similar rates of major adverse cardiovascular events, comprising a composite of death from cardiovascular causes, myocardial infarction (MI), and stroke/transient ischemic attack (TIA) [34, 38, 39••]. After adjustment for other risk factors including AF, hypertension, and DM, patients with OSA have higher overall rates of stroke and all-cause death [30, 34]. Whether obstructive sleep apnea confers additional risk of stroke in AF patients independent of CHA2DS2-VASc score needs to be studied further in clinical studies.
Renal Failure
In a study of 90,490 patients with non-valvular AF who were not on anticoagulation, renal failure showed a significant association with the composite thromboembolism endpoint of stroke, TIA, or systemic embolism but not with ischemic stroke alone [17]. Renal dysfunction—whether recognized or unrecognized—is associated with higher rates of in-hospital mortality and severe disability at hospital discharge in stroke patients [40]. In a study of 3080 AF patients as subdivided by creatinine clearance (CrCl) categories, patients with CrCl < 30, 39–49, and ≥ 50 had statistically significant differences in the incidence of stroke/systemic embolism with more events among patients with worse renal function (p = 0.0002) [41]. Comparing patients with a CrCl < 30 with those ≥ 50, and after adjusting for risk factors, the risk of stroke/systemic embolism was statistically higher in the group with increased dysfunction (HR 1.68; 95% CI 1.04 to 2.65; p = 0.04) [41].
Given these factors, adding renal failure to current models may improve their ability to risk-stratify patients [17, 41,42,43]. A novel R2-CHADS2 index, which adds two points for CrCl below 60 mL/min to the CHADS2 score, was developed in ROCKET-AF (Rivaroxaban Once-daily, oral, direct factor Xa inhibition Compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation) patient cohort. This score improved net stroke risk reclassification by 8.2% as compared with the CHADS2 score and by 6.2% over the CHA2DS2VASc score. This novel index was validated in 13,559 patients in the ATRIA (AnTicoagulation and Risk factors In Atrial fibrillation) cohort where it conferred a 17.4% improvement in net stroke risk reclassification compared with the CHADS2 score [42].
In a study of 219 patients with AF, Fu et al. observed that adding either creatinine clearance (CrCl) or glomerular filtrate rate (GFR) to both CHADS2 and CHA2DS2VASc schemes improved mortality prediction in older Chinese patients with AF and renal dysfunction [43]. The GFR-containing models demonstrated a more robust improvement on current models than those with CrCl; however, the study did not assess the impact on the novel model on stroke risk stratification [43]. Further studies are, therefore, needed to validate whether the addition of renal insufficiency improves stroke prediction in AF patients.
Laboratory Predictors of Stroke in AF
Brain Natriuretic Peptide
Brain natriuretic peptide (BNP) is a known correlate of stroke and heart failure [44,45,46,47]. It is a chemical synthesized by cardiac muscle cells in response to stress, rising significantly with elevated blood pressure or with circulatory overload from salt and water retention [44, 46, 47]. It is also secreted by the hypothalamus in response to cerebral ischemia [44, 46, 47].
In a study of 40 stroke patients, Sayan et al. found that BNP rose acutely in the first 24–72 h post-stroke [44]. Elevated BNP is an indicator of poor prognosis and death but does not accurately predict infarct volume [44]. Even at lower levels, BNP is a good predictor of stroke, with prognostic differences for individuals with a BNP < 13 pg/mL versus those with levels below 34 pg/mL [47].
Based on study data from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort of 30,239 individuals aged 45 and above, Cushman et al. found that N-terminal pro-BNP (NT-proBNP) tended to be higher in older individuals as well as those with heart and renal disease, AF, and elevated low-density lipoprotein cholesterol [45]. Of the 576 participants with first-time ischemic stroke, NT-proBNP was a marker for cardioembolic stroke, in particular. The hazard ratio of incident stroke increased with each increasing quartile of baseline NT-proBNP [45].
Hayashi et al. studied the impact of BNP using the Japanese Hokuriku-Plus AF Registry [46]. Of the 1013 AF patients aged 30 to 94, thromboembolic events occurred more significantly among patients with BNP levels at or above 170 pg/mL, while patients with levels at or above 147 pg/mL were more likely to have a composite of thromboembolic events and cardiovascular death [46]. Based on these results, there is potential role of BNP/NT-proBNP in prediction of stroke and thromboembolism in AF patients as well as to determine prognosis.
Imaging Predictors of Stroke in Atrial Fibrillation
Left Atrial/Left Atrial Appendage (LAA) Thrombus and LAA Morphology
Thrombus formation in the left atrium, specifically left atrial appendage (LAA), is associated with thromboembolic events including embolic stroke—in patients with AF. Studies have demonstrated a 10–33% increased risk of stroke, systemic embolism, and death over 1 to 3 years of observation among patients with AF and LA/LAA thrombus [26]. Risk factors for LAA thrombus include a larger LA as well as a higher LAA position, reduced left ventricular ejection fraction (LVEF), increased left ventricular end-diastolic volume, degree of spontaneous echocardiographic contrast (SEC), increased LAA volume, and LAA morphology [9]. LAA morphology has been subdivided into four types—cactus, chicken wing, windsock, and cauliflower [25]. After adjusting for presence of comorbidities and stroke risk based on the CHADS2 score, patients with the chicken wing LAA morphology were found to have fewer embolic events than the others [25]. Looking not just for the presence of an LA/LAA thrombus but also for the LAA morphology can perhaps improve echocardiographic prediction of stroke in AF patients.
Spontaneous Echo Contrast
Spontaneous echo contrast (SEC), colloquially known as smoke, is defined as the echogenicity of blood in the absence of injected contrast agents [11]. It occurs when RBC aggregates scatter the ultrasound signal [26], creating dynamic smoke-like echoes within the LA cavity or appendage and appears distinct from artifacts due to noise or injected bubbles [11]. It may be noted on transthoracic echocardiogram (TTE) but is more commonly identified on transesophageal echocardiogram (TEE). Among patients with non-valvular AF, it is considered predictive of future embolic events and death [11]. In a prospective cohort study of 206 patients with non-valvular AF, TEE was performed at baseline to assess for left atrial appendage thrombus. In addition, left atrial thrombus (LAT), the five-grades of left atrial spontaneous echo contrast (LASEC) and video intensity (VI) value of LASEC were measured. Over 2 years of follow-up, 20 patients (9.7%) had stroke. The authors noted that the VI value of LASEC in patients with stroke was higher than the patients without stroke (25.30 ± 3.61 vs. 8.65 ± 0.81, p < 0.001). They also observed that LAT, qualitative LASEC, graded LASEC, VI value of LASEC, and CHADS2 and CHA2DS2-Vasc score were independent predictors of stroke on logistic regression analysis, of which VI value of LASEC had the highest area under the curve of receiver operating characteristic (ROC) in predicting stroke (p < 0.05). Based on these results, quantification of LASEC by VI value is a strong predictor of stroke in patients with NVAF.
Coronary Artery Calcium Score
Prior studies have shown that coronary artery calcium score is an independent risk factor for stroke in general population [48]. In a study of 401 patients with non-valvular AF who were admitted for ischemic stroke, coronary CT angiogram was performed to assess for coronary artery disease and coronary artery calcium score (CACS) [49]. CACS was noted to have an additive value in predicting non-cardioembolic risk factors of stroke—such as complex aortic plaque, significant carotid, or intracranial arterial stenosis—in addition to those defined in the CHA2DS2-VASc score. Based on these results, CACS provides additional information for risk of stroke in AF patients beyond the current determinants of CHA2DS2-VASc scores.
Ethnicity and Stroke Prediction in AF
Despite lower rates of AF, African-American patients are at a disproportionately increased risk of fatal stroke when compared with whites [27]. They have a higher overall incidence of stroke, and their age-adjusted mortality from stroke is 2–4 times higher than that for whites [27, 28]. This has been attributed to several risk factors including hypertension, diabetes mellitus, and lower socioeconomic status. In the REGARDS (Reasons for Geographic and Racial Differences in Stroke) cohort, only half of the excess stroke incidence in African-Americans was attributable to traditional risk factors and socioeconomic status, while the other half was attributed to other unknown factors and pathways [50]. The incidence of stroke is also higher in African-American patients with AF compared with white counterparts. A study of 517,941 Medicare patients aged > 65 years with newly diagnosed AF looked at the racial differences in outcomes of stroke and mortality [29]. Of these, 452,986 patients (87%) were non-Hispanic white, 36,425 (7%) were black, and 28,530 (6%) were Hispanic. Over a median follow-up of 20.3 months, blacks had a significantly higher hazard of stroke compared with the whites (HR = 1.66; 95% CI 1.57 to 1.75; p < 0.001), which persisted even after controlling for pre-existing comorbidities (HR = 1.46; 95% CI 1.38 to 1.55; p < 0.001).
A follow-up study hypothesized that adding an additional point for African-American ethnicity to CHA2DS2-VASc score would improve stroke prediction [8]. This novel CHA2DS2-VASc-R score was compared with CHA2DS2-VASc score in 460,417 patients aged 65 and above with newly diagnosed AF. The population comprised of 390,590 (85%) non-Hispanic whites and 31,702 (7%) non-Hispanic African Americans. Compared with CHA2DS2-VASc score, CHA2DS2-VASc-R improved the model-fit significantly—as measured by the log likelihood ratio statistic (p < 0.001). CHA2DS2-VASc had a c-statistic of 0.60 (95% CI, 0.59–0.61), while CHA2DS2-VASc-R demonstrated an improvement with a c-statistic of 0.61 (95% CI, 0.60–0.62). Of all the risk factors in the CHA2DS2-VASc-R score, only prior history of stroke, age 75 years, and female sex were more important than African-American ethnicity in prediction of stroke in this population [8]. Coefficients associated with other races (Hispanics, Native Americans, Asians/Pacific Island descent) were either small or non-significant, so additional points for these races were not warranted in CHA2DS2-VASc-R score. Based on these results, there is a good evidence of considering ethnicity in addition to CHA2DS2-VASc score for stroke prediction in AF patients.
Alternative Stroke Prediction Models for Atrial Fibrillation
TIMI-AF
The Thrombolysis in Myocardial Infarction-Atrial Fibrillation (TIMI-AF) score was established to predict net clinical outcome consisting of disabling stroke, life-threatening bleeding, or all-cause mortality in patients receiving warfarin therapy while also advising on use of a NOAC versus warfarin in anticoagulant-naïve patients [51]. It is based on the ENGAGE AF-TIMI 48 randomized clinical trial comparing edoxaban with warfarin for patients with AF [51•]. This score gives 3 points for age > 75 years and LVEF < 30% and two points for age 66 to 74, LVEF 30–49%, hemoglobin below 13 g/dL, and non-white race. One point is given for each of the following: unknown LVEF, baseline AF or atrial flutter, prior ischemic stroke, creatinine ≥ 110 μmmol/L, male sex, diabetes mellitus, carotid disease history, and prior myocardial infarction [52]. An individual can receive a maximum of 17 points (Table 1) [51•]. TIMI-AF score predicted a net clinical outcome in warfarin-naïve patients with AF who were started on warfarin or edoxaban for stroke prevention [51•]. Edoxaban and warfarin were equivalent in low-score patients, but edoxaban outperformed warfarin in patients with intermediate and high scores [51•]. In a single center retrospective study of 426 patients with non-valvular AF, the TIMI-AF score was better than CHA2DS2-VASc, SAMeTT2R2, and HAS-BLED at identifying patients at higher risk of cardiovascular events as well as those with a “poor net clinical outcome” of life-threatening bleeding, disabling stroke, or all-cause mortality [52]. These findings need to be confirmed in larger prospective studies.
The ATRIA Score
The ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) score, based on the self-titled cohort, was created to better identify those patients at highest risk for stroke while also considering bleeding risk [53]. The risk score incorporates renal dysfunction into CHADS2 and strongly considers age categories. It also weighs the interaction of age and prior stroke, reflecting a higher risk of stroke in patients with a prior history of stroke irrespective of age. This model assigns a maximum of fifteen points to patients based on previous stroke and age (< 65, 65–74, 75–84, and 85+) with each of female sex, DM, CHF, hypertension, urine dipstick proteinuria, and either eGFR < 45 or end-stage renal disease receiving one point (Table 1). The score was validated in ATRIA–Cardiovascular Research Network (CVRN) cohort comprising of 33,247 patients with AF, in which it outperformed CHADS2 and CHA2DS2VASc in terms of c-index and net reclassification improvement (NRI) for prediction of stroke and thromboembolism. These scores were also compared in 60,594 AF patients in the UK Clinical Practice Research Datalink cohort, who were untreated with warfarin. The ATRIA score was better at identifying low-risk AF patients who had been classified as high risk by CHA2DS2VASc score [54]. Based on these studies, the ATRIA score may aid the risk-stratification of very low to low stroke-risk AF patients (CHA2DS2-VASc score of 0 or 1 [men] and 1 or 2 [women]) [55].
The GARFIELD-AF Risk Tool
The GARFIELD-AF risk tool is a novel computer-generated machine learning risk model that predicts all-cause mortality, ischemic stroke/systemic embolism (SE), and hemorrhagic stroke/major bleeding in AF patients. It is based on data from the Global Anticoagulant Registry in the FIELD-Atrial Fibrillation (GARFIELD-AF Registry) with data from 35 countries on adults with newly diagnosed AF and at least one additional risk factor for stroke and validated externally by data from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) database [56]. GARFIELD-AF risk tool showed improved prediction of ischemic stroke risk and all-cause mortality compared with CHA2DS2-VASc, and it out-performed HAS-BLED in prediction of major bleeding for both the cumulative population and of low-risk patients. This risk model may have a place integrated into electronic health records to simultaneously risk-stratify patients for ischemic stroke, all-cause mortality, and major bleeding [57•].
Conclusions
Overall, the close relationship between AF and stroke warrants models and mechanisms to stratify patients for risk of cardioembolic phenomena. CHA2DS2-VASc score seeks to explicate this stroke risk by identifying low-risk population and has been endorsed by American and European guidelines. However, recent studies have demonstrated several clinical, laboratory, imaging parameters, which may improve stroke prediction in AF patient’s, independent of CHA2DS2-VASc score. Addition of African-American ethnicity to CHA2DS2-VASc score also resulted in better stroke prediction. In order to have a widespread acceptance and use in clinical practice, it is important for the novel stroke prediction models to be user friendly and easy to calculate. The potential for computer-generated risk models using artificial intelligence is very promising for the future. Ultimately, stroke risk in atrial fibrillation extends far beyond the CHA2DS2-VASc score, with much left to learn and refine on the topic.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–528 Available from: http://www.ncbi.nlm.nih.gov/pubmed/30700139.
Krishnamurthi RV, Feigin VL, Forouzanfar MH, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health. 2013;1:e259–81 Available from: http://www.ncbi.nlm.nih.gov/pubmed/25104492.
Kamel H, Healey JS. Cardioembolic stroke. Circ Res. 2017;120:514–26 Available from: http://www.ncbi.nlm.nih.gov/pubmed/28154101.
Pistoia F, Sacco S, Tiseo C, Degan D, Ornello R, Carolei A. The epidemiology of atrial fibrillation and stroke. Cardiol Clin. 2016;34:255–68 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27150174.
Wasmer K, Eckardt L, Breithardt G. Predisposing factors for atrial fibrillation in the elderly. J Geriatr Cardiol. 2017;14:179–84 Available from: http://www.ncbi.nlm.nih.gov/pubmed/28592961.
McIntyre WF, Healey J. Stroke prevention for patients with atrial fibrillation: beyond the guidelines. J Atr fibrillation. 9:1475 Available from: http://www.ncbi.nlm.nih.gov/pubmed/29250283.
Ugowe FE, Jackson LR, Thomas KL. Racial and ethnic differences in the prevalence, management, and outcomes in patients with atrial fibrillation: a systematic review. Hear Rhythm. 2018;15:1337–45 Available from: http://www.ncbi.nlm.nih.gov/pubmed/29803022.
Kabra R, Girotra S, Vaughan SM. Refining stroke prediction in atrial fibrillation patients by addition of African-American ethnicity to CHA2DS2-VASc score. J Am Coll Cardiol. 2016;68:461–70 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27470453.
Marsico F, Cecere M, Parente A, Paolillo S, de Martino F, Dellegrottaglie S, et al. Effects of novel oral anticoagulants on left atrial and left atrial appendage thrombi: an appraisal. J Thromb Thrombolysis. 2017;43:139–48 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27614756.
D’Souza A, Butcher KS, Buck BH. The multiple causes of stroke in atrial fibrillation: thinking broadly. Can J Cardiol. 2018;34:1503–11 Available from: http://www.ncbi.nlm.nih.gov/pubmed/30404753.
Black IW. Spontaneous echo contrast: where there’s smoke there’s fire. Echocardiography. 2000;17:373–82 Available from: http://www.ncbi.nlm.nih.gov/pubmed/10979010.
January CT, Wann LS, Calkins H, Field ME, Chen LY, Furie KL, et al. AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the Heart R. Hear Rhythm. 2019; Available from: http://www.ncbi.nlm.nih.gov/pubmed/30703530.
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285:2864–70 Available from: http://www.ncbi.nlm.nih.gov/pubmed/11401607.
Olesen JB, Lip GYH, Hansen ML, Hansen PR, Tolstrup JS, Lindhardsen J, et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;342:d124 Available from: http://www.ncbi.nlm.nih.gov/pubmed/21282258.
Olesen JB, Torp-Pedersen C, Hansen ML, Lip GYH. The value of the CHA2DS2-VASc score for refining stroke risk stratification in patients with atrial fibrillation with a CHADS2 score 0-1: a nationwide cohort study. Thromb Haemost. 2012;107:1172–9 Available from: http://www.ncbi.nlm.nih.gov/pubmed/22473219.
Yarmohammadi H, Varr BC, Puwanant S, Lieber E, Williams SJ, Klostermann T, et al. Role of CHADS2 score in evaluation of thromboembolic risk and mortality in patients with atrial fibrillation undergoing direct current cardioversion (from the ACUTE trial substudy). Am J Cardiol. 2012;110:222–6 Available from: http://www.ncbi.nlm.nih.gov/pubmed/22503581.
Friberg L, Rosenqvist M, Lip GYH. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012;33:1500–10 Available from: http://www.ncbi.nlm.nih.gov/pubmed/22246443.
Okumura K, Inoue H, Atarashi H, Yamashita T, Tomita H, Origasa H, et al. Validation of CHA2DS2-VASc and HAS-BLED scores in Japanese patients with nonvalvular atrial fibrillation: an analysis of the J-RHYTHM Registry. Circ J. 2014;78:1593–9 Available from: http://www.ncbi.nlm.nih.gov/pubmed/24759791.
Camm AJ, Lip GYH, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al. Focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation--developed with the special contribution of the European Heart Rhythm Association. Europace. 2012;14:1385–413 Available from: http://www.ncbi.nlm.nih.gov/pubmed/22923145.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur J Cardiothorac Surg. 2016;50:e1–88 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27663299.
Koga M, Yoshimura S, Hasegawa Y, Shibuya S, Ito Y, Matsuoka H, et al. Higher risk of ischemic events in secondary prevention for patients with persistent than those with paroxysmal atrial fibrillation. Stroke. 2016;47:2582–8 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27531346.
Steinberg BA, Hellkamp AS, Lokhnygina Y, Patel MR, Breithardt G, Hankey GJ, et al. Higher risk of death and stroke in patients with persistent vs. paroxysmal atrial fibrillation: results from the ROCKET-AF trial. Eur Heart J. 2015;36:288–96 Available from: http://www.ncbi.nlm.nih.gov/pubmed/25209598.
Ganesan AN, Chew DP, Hartshorne T, Selvanayagam JB, Aylward PE, Sanders P, et al. The impact of atrial fibrillation type on the risk of thromboembolism, mortality, and bleeding: a systematic review and meta-analysis. Eur Heart J. 2016;37:1591–602 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26888184.
Quon MJ, Behlouli H, Pilote L. Anticoagulant use and risk of ischemic stroke and bleeding in patients with secondary atrial fibrillation associated with acute coronary syndromes, acute pulmonary disease, or sepsis. JACC Clin Electrophysiol. 2018;4:386–93 Available from: http://www.ncbi.nlm.nih.gov/pubmed/30089566.
Di Biase L, Santangeli P, Anselmino M, Mohanty P, Salvetti I, Gili S, et al. Does the left atrial appendage morphology correlate with the risk of stroke in patients with atrial fibrillation? Results from a multicenter study. J Am Coll Cardiol. 2012;60:531–8 Available from: http://www.ncbi.nlm.nih.gov/pubmed/22858289.
Vinereanu D, Lopes RD, Mulder H, Gersh BJ, Hanna M, de Barros E Silva PGM, et al. Echocardiographic risk factors for stroke and outcomes in patients with atrial fibrillation anticoagulated with apixaban or warfarin. Stroke. 2017;48:3266–73 Available from: http://www.ncbi.nlm.nih.gov/pubmed/29089455.
Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke. 1999;30:736–43 Available from: http://www.ncbi.nlm.nih.gov/pubmed/10187871.
Golwala H, Jackson LR, Simon DN, Piccini JP, Gersh B, Go AS, et al. Racial/ethnic differences in atrial fibrillation symptoms, treatment patterns, and outcomes: insights from Outcomes Registry for Better Informed Treatment for Atrial Fibrillation registry. Am Heart J. 2016;174:29–36 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26995367.
Kabra R, Cram P, Girotra S, Vaughan SM. Effect of race on outcomes (stroke and death) in patients >65 years with atrial fibrillation. Am J Cardiol. 2015;116:230–5 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26004053.
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41 Available from: http://www.ncbi.nlm.nih.gov/pubmed/16282178.
Lyons OD, Ryan CM. Sleep apnea and stroke. Can J Cardiol. 2015;31:918–27 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26112302.
Wang X, Ouyang Y, Wang Z, Zhao G, Liu L, Bi Y. Obstructive sleep apnea and risk of cardiovascular disease and all-cause mortality: a meta-analysis of prospective cohort studies. Int J Cardiol. 2013;169:207–14 Available from: http://www.ncbi.nlm.nih.gov/pubmed/24161531.
Dyken ME, Somers VK, Yamada T, Ren ZY, Zimmerman MB, et al. Stroke. 1996;27:401–7 Available from: http://www.ncbi.nlm.nih.gov/pubmed/8610303.
Jehan S, Farag M, Zizi F, Pandi-Perumal SR, Chung A, Truong A, et al. Obstructive sleep apnea and stroke. Sleep Med Disord Int J. 2018;2:120–5 Available from: http://www.ncbi.nlm.nih.gov/pubmed/30680373.
Lipford MC, Flemming KD, Calvin AD, Mandrekar J, Brown RD, Somers VK, et al. Associations between cardioembolic stroke and obstructive sleep apnea. Sleep. 2015;38:1699–705 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26237769.
Mansukhani MP, Calvin AD, Kolla BP, Brown RD, Lipford MC, Somers VK, et al. The association between atrial fibrillation and stroke in patients with obstructive sleep apnea: a population-based case-control study. Sleep Med. 2013;14:243–6 Available from: http://www.ncbi.nlm.nih.gov/pubmed/23340087.
Gami AS, Pressman G, Caples SM, Kanagala R, Gard JJ, Davison DE, et al. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004;110:364–7 Available from: http://www.ncbi.nlm.nih.gov/pubmed/15249509.
Holmqvist F, Guan N, Zhu Z, Kowey PR, Allen LA, Fonarow GC, et al. Impact of obstructive sleep apnea and continuous positive airway pressure therapy on outcomes in patients with atrial fibrillation-results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Am Heart J. 2015;169:647–654.e2 Available from: http://www.ncbi.nlm.nih.gov/pubmed/25965712.
•• Staerk L, Sherer JA, Ko D, Benjamin EJ, Helm RH. Atrial fibrillation: epidemiology, pathophysiology, and clinical outcomes. Circ Res. 2017;120:1501–17 Available from: http://www.ncbi.nlm.nih.gov/pubmed/28450367. This study summarizes the current knowledge on atrial fibrillation, its risk factors, and clinical outcomes.
Pereg D, Rozenbaum Z, Vorobeichik D, Shlomo N, Gilad R, Bloch S, et al. Prevalence and significance of unrecognized renal dysfunction in patients with stroke. Am J Med. 2016;129:1074–81 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27215905.
Abe M, Ogawa H, Ishii M, Masunaga N, Esato M, Chun Y-H, et al. Relation of stroke and major bleeding to creatinine clearance in patients with atrial fibrillation (from the Fushimi AF registry). Am J Cardiol. 2017;119:1229–37 Available from: http://www.ncbi.nlm.nih.gov/pubmed/28219663.
Piccini JP, Stevens SR, Chang Y, Singer DE, Lokhnygina Y, Go AS, et al. Renal dysfunction as a predictor of stroke and systemic embolism in patients with nonvalvular atrial fibrillation: validation of the R(2)CHADS(2) index in the ROCKET AF (Rivaroxaban Once-daily, oral, direct factor Xa inhibition Compared with vitamin K ant). Circulation. 2013;127:224–32 Available from: http://www.ncbi.nlm.nih.gov/pubmed/23212720.
Fu S, Zhou S, Luo L, Ye P. R2(GFR)CHADS2 and R2(GFR)CHA2DS2VASc schemes improved the performance of CHADS2 and CHA2DS2VASc scores in death risk stratification of Chinese older patients with atrial fibrillation. Clin Interv Aging. 2017;12:1233–8 Available from: http://www.ncbi.nlm.nih.gov/pubmed/28848331.
Sayan S, Kotan D. Levels of brain natriuretic peptide as a marker for the diagnosis and prognosis of acute ischemic stroke. Arch Med Sci Atheroscler Dis. 2016;1:e16–22 Available from: http://www.ncbi.nlm.nih.gov/pubmed/28905014.
Cushman M, Judd SE, Howard VJ, Kissela B, Gutiérrez OM, Jenny NS, et al. N-terminal pro-B-type natriuretic peptide and stroke risk: the reasons for geographic and racial differences in stroke cohort. Stroke. 2014;45:1646–50 Available from: http://www.ncbi.nlm.nih.gov/pubmed/24757103.
Hayashi K, Tsuda T, Nomura A, Fujino N, Nohara A, Sakata K, et al. Impact of B-type natriuretic peptide level on risk stratification of thromboembolism and death in patients with nonvalvular atrial fibrillation - the Hokuriku-Plus AF Registry. Circ J. 2018;82:1271–8 Available from: http://www.ncbi.nlm.nih.gov/pubmed/29491320.
Sughrue T, Swiernik MA, Huang Y, Brody JP. Laboratory tests as short-term correlates of stroke. BMC Neurol. 2016;16:–112 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27439507.
Hermann DM, Gronewold J, Lehmann N, Moebus S, Jöckel K-H, Bauer M, et al. Coronary artery calcification is an independent stroke predictor in the general population. Stroke. 2013;44:1008–13 Available from: http://www.ncbi.nlm.nih.gov/pubmed/23449263.
Yang P-S, Pak H-N, Park D-H, Yoo J, Kim T-H, Uhm J-S, et al. Non-cardioembolic risk factors in atrial fibrillation-associated ischemic stroke. PLoS One. 2018;13:e0201062 Available from: http://www.ncbi.nlm.nih.gov/pubmed/30028885.
Howard G, Cushman M, Kissela BM, Kleindorfer DO, McClure LA, Safford MM, et al. Traditional risk factors as the underlying cause of racial disparities in stroke: lessons from the half-full (empty?) glass. Stroke. 2011;42:3369–75 Available from: http://www.ncbi.nlm.nih.gov/pubmed/21960581.
• Fanola CL, Giugliano RP, Ruff CT, Trevisan M, Nordio F, Mercuri MF, et al. A novel risk prediction score in atrial fibrillation for a net clinical outcome from the ENGAGE AF-TIMI 48 randomized clinical trial. Eur Heart J. 2017;38:888–96 Available from: http://www.ncbi.nlm.nih.gov/pubmed/28064150. The TIMI-AF score is helpful in predicting outcomes with anticoagulation and guiding the use of a direct oral anticoagulant (Edoxaban) versus warfarin for stroke prevention in vitamin K antagonist-naïve patients. Edoxaban proved superior in those with intermediate and higher risk scores, while edoxaban and warfarin were equivalent in patients with low-risk scores.
Pérez Cabeza AI, Bravo Marques R, Chinchurreta Capote PA, Ruiz Mateas F, Fanola CL, Rosas Cervantes G, et al. TIMI-AF score and cardiovascular events in vitamin K antagonists-naïve outpatients with atrial fibrillation. Clin Cardiol. 2018;41:1252–8 Available from: http://www.ncbi.nlm.nih.gov/pubmed/30062699.
Singer DE, Chang Y, Borowsky LH, Fang MC, Pomernacki NK, Udaltsova N, et al. A new risk scheme to predict ischemic stroke and other thromboembolism in atrial fibrillation: the ATRIA study stroke risk score. J Am Heart Assoc. 2013;2:e000250 Available from: http://www.ncbi.nlm.nih.gov/pubmed/23782923.
van den Ham HA, Klungel OH, Singer DE, Leufkens HGM, van Staa TP. Comparative performance of ATRIA, CHADS2, and CHA2DS2-VASc risk scores predicting stroke in patients with atrial fibrillation: results from a National Primary Care Database. J Am Coll Cardiol. 2015;66:1851–9 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26493655.
Deering TF. Incorporating stroke and bleeding risk stratification tools into atrial fibrillation management making sense of the alphabet soup. J Atr Fibrillation. 2017;9:1497 Available from: http://www.ncbi.nlm.nih.gov/pubmed/29250284.
Piccini JP, Fraulo ES, Ansell JE, Fonarow GC, Gersh BJ, Go AS, et al. Outcomes registry for better informed treatment of atrial fibrillation: rationale and design of ORBIT-AF. Am Heart J. 2011;162:606–612.e1 Available from: http://www.ncbi.nlm.nih.gov/pubmed/21982650.
• Fox KAA, Lucas JE, Pieper KS, Bassand J-P, Camm AJ, Fitzmaurice DA, et al. Improved risk stratification of patients with atrial fibrillation: an integrated GARFIELD-AF tool for the prediction of mortality, stroke and bleed in patients with and without anticoagulation. BMJ Open. 2017;7:e017157 Available from: http://www.ncbi.nlm.nih.gov/pubmed/29273652. This is the GARFIELD-AF integrated risk tool study, which showed superiority compared with CHA2DS2VASc for stroke- and mortality-risk prediction and compared with HAS-BLED for bleeding risk.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Pooja S. Jagadish and Rajesh Kabra declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Invasive Electrophysiology and Pacing
Rights and permissions
About this article
Cite this article
Jagadish, P.S., Kabra, R. Stroke Risk in Atrial Fibrillation: Beyond the CHA2DS2-VASc Score. Curr Cardiol Rep 21, 95 (2019). https://doi.org/10.1007/s11886-019-1189-6
Published:
DOI: https://doi.org/10.1007/s11886-019-1189-6