Abstract
Heart failure with preserved ejection fraction (HFpEF), a highly prevalent and complex clinical syndrome with high morbidity and mortality, is often unrecognized and not optimally treated. Clinical trials for HFpEF have been plagued by low enrollment, and clinicians often approach HFpEF patients with “therapeutic nihilism” given the perceived lack of available therapies based on the disappointing results of these prior trials. Due to these challenges, we have pioneered the successful creation of dedicated, specialized HFpEF clinical programs. Here, we discuss (1) the rationale for the development of a specialized HFpEF clinical program; (2) strategies for the systematic identification of HFpEF patients; (3) a standardized diagnostic and therapeutic approach; (4) validation of the HFpEF clinical program paradigm; (5) staffing and reimbursement considerations; (6) HFpEF clinical trial enrollment; and (7) challenges and future directions for HFpEF clinical programs. We conclude that it is feasible to create HFpEF clinical programs that fulfill the major unmet need of identifying and caring for patients with HFpEF. These clinics are essential for confirming the HFpEF diagnosis, providing standardized treatment, and facilitating clinical trial enrollment. It is our hope that the information provided here will encourage others to establish their own specialized HFpEF programs, thereby allowing for comprehensive care for these complex patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Heart failure with preserved ejection fraction (HFpEF) is a common, debilitating syndrome that primarily affects elderly patients [1]. HFpEF is now known to cause nearly 50 % of all hospitalizations for heart failure (HF) in the USA, and it is associated with a high mortality rate of approximately 65 % at 5 years after HF hospitalization [1, 2]. Randomized controlled trials have been very successful for the identification of treatments for HF with reduced ejection fraction (HFrEF), but have not had the same success in HFpEF [3••]. The high rate of morbidity and mortality, coupled with lack of improvement in clinical trials, underscores the fact that the HFpEF syndrome is heterogenous, complex, and poorly characterized [4].
To our knowledge, prior to the creation of the Northwestern University HFpEF Program in 2007, a specific clinical program for HFpEF patients had never before been implemented. Furthermore, despite the increasing interest in HFpEF and the creation of additional HFpEF specialty clinics, the number of clinics for HFpEF patients pales in comparison to specific clinics and programs for HFrEF, particularly for patients pre- and post-cardiac transplantation and ventricular assist device placement. In addition, while general HF clinics do not typically exclude patients with HFpEF, large studies of HF clinics have shown that the proportion of patients with HFpEF in these clinics is typically quite low. For example, in the multicenter COACH trial, which studied disease management programs in HF clinics, only 157/1023 (15 %) of enrolled patients had an ejection fraction ≥40 % despite the inclusion of all HF patients in these clinics (regardless of ejection fraction) [5, 6•].
The reasons for the general lack of HFpEF clinics may be that there are few if any proven treatments for HFpEF. Currently, although these patients are common and frequently hospitalized, internists, hospitalists, family physicians, and general cardiologists frequently care for these patients. Occasionally, these patients (typically with advanced HFpEF and/or those with rare etiologies of HFpEF such as cardiac amyloidosis) are referred to a general HF clinic, although the approach and treatment in these clinics are geared towards HFrEF, and the referral of HFpEF patients to a HF specialist is often haphazard. Therefore, there is a continued unmet need for expansion of HFpEF clinics to care for these patients.
Here, we discuss (1) the rationale for the development of a specialized HFpEF clinical program; (2) strategies for the systematic identification of HFpEF patients; (3) a standardized diagnostic and therapeutic approach; (4) validation of the HFpEF clinical program paradigm; (5) staffing and reimbursement considerations; (6) HFpEF clinical trial enrollment; and (7) challenges and future directions for HFpEF clinical programs. Our goal is to provide practical advice for the development and implementation of HFpEF programs so that more of these challenging patients can receive optimal care and so that we can continue to advance the field by enhancing enrollment in HFpEF clinical trials.
Rationale for the Development of a Specialized HFpEF Program
For many complex and severe diseases and clinical syndromes, specialty clinics have arisen as a way to give multidisciplinary and comprehensive care with the goal of improving outcomes. The impetus for disease-specific clinics appears to be the availability of specialized therapies. For example, within cardiology, clinics exist for hypertrophic cardiomyopathy, pulmonary hypertension, heart transplantation, and lipid problems, among others. Outside of cardiology, many specialized clinics—such as cancer-specific clinics (e.g., lung cancer), rheumatologic disorder-specific clinics (e.g., systemic sclerosis), and human immunodeficiency virus (HIV) clinics—exist in order to give multidisciplinary, specialized, and comprehensive care for patients with these chronic medical conditions.
When considered in the context of the aforementioned examples of specialty clinics in other fields in medicine, three major impediments to the development of specific HFpEF programs can be identified: (1) the long-standing under-appreciation of the HFpEF syndrome; (2) the lack of clear and consistent diagnostic criteria for HFpEF; and (3) the perceived lack of therapies for HFpEF.
It is now clear that HFpEF is a true and distinct clinical syndrome that is not simply a collection of comorbidities [7]. In addition, several studies have shown that HFpEF is increasingly common and is associated with high morbidity and mortality [1, 2]. These types of studies, along with inclusion of HFpEF in HF clinical guidelines [8, 9], have increased the attention to the HFpEF syndrome and likely have led to increased frequency of diagnosis. Dedicated HFpEF clinical programs can help with increasing recognition and acceptance of HFpEF as a true clinical syndrome.
Although there is controversy in the most appropriate definition for HFpEF, there is increasing consensus about diagnostic criteria. Two factors have likely led to confusion about HFpEF diagnostic criteria. First, because HFpEF was previously termed “diastolic heart failure”, it was thought that patients with HFpEF must have significant diastolic dysfunction. However, the echocardiographic diagnosis of diastolic dysfunction can vary widely from reader to reader [10], as the diagnosis relies on multiple different criteria that are not always easy to apply in a consistent manner. Second, patients with HFpEF, especially in the outpatient setting, can have a BNP or NTproBNP value that is considered to be in the “normal” range (e.g., <100 pg/ml for BNP). However, we and others have shown that up to 30 % of outpatients have a normal BNP level [11], likely due to the high prevalence of obesity in HFpEF (which is associated with increased BNP clearance and decreased BNP production [12]). In addition, compared to HFrEF, diastolic wall stress is lower in HFpEF than HFrEF, which is another reason why BNP levels may be low in HFpEF [13]. Because the criteria that include diastolic dysfunction and BNP are so problematic, we advocate the use of a diagnostic strategy (Table 1) that includes (1) symptoms and signs of the HF syndrome, which can be based on clinical history and testing, or in equivocal cases may require specific exercise testing; (2) preserved ejection fraction (i.e., LVEF >45–50 %); and (3) evidence that a cardiac problem compatible with HFpEF is present. The last criteria typically requires the presence of LV hypertrophy or left atrial enlargement or elevated E/e’ ratio on echocardiography or elevated BNP (or NTproBNP) or elevated LV filling pressures at rest (pulmonary capillary wedge pressure [PCWP] >15 mmHg or LV end-diastolic pressure >12 mmHg) or with exercise (PCWP >25 mmHg during exercise). An important aspect of specialized HFpEF clinical programs is that they are the de facto destination for patients to receive a definitive diagnosis of HFpEF.
The final impediment to the creation of dedicated HFpEF clinical programs is the perceived lack of specific therapies for HFpEF. Many clinicians have a sense of “therapeutic nihilism” when it comes to HFpEF patients [14]. While it is true that large-scale HFpEF clinical trials have not met their primary outcome, many therapies that have been tested have shown benefit in some way, as outlined below. Furthermore, there are simple things that can be done in the HFpEF clinic (risk factor modification, diet and exercise education, medication management, etc.) that can have a major impact on the lives of HFpEF patients. Finally, the relative lack of therapies for HFpEF compared to other cardiovascular disorders dictates that we perform more clinical trials to identify new therapies; however, poor enrollment in HFpEF clinical trials remains a major problem. Dedicated HFpEF programs can provide a robust method to increase enrollment success, as detailed below.
For the reasons outlined above, the creation of dedicated HFpEF clinical programs is able to counter the aforementioned impediments by increasing awareness of the HFpEF syndrome; providing a centralized place for diagnosis of the HFpEF syndrome; and providing comprehensive treatment for HFpEF patients. As general HF clinics (which predominantly have focused on HFrEF patients) have shown, a multidisciplinary approach to HF patients can improve quality of life and reduce HF hospitalizations [15, 16].
Development of the Northwestern HFpEF Program
In 2007, the first dedicated HFpEF clinical program was developed and implemented at Northwestern University. To date >1500 HFpEF patients have been cared for in the Northwestern HFpEF Program. Patients in the Northwestern HFpEF Program have been studied extensively (as part of a prospective HFpEF registry [ClinicalTrials.gov; NCT01030991]) [11, 17–24, 25••, 26], and the large reservoir of HFpEF patients in the program have led to successful, leading enrollment in several major HFpEF clinical trials including TOPCAT [27] (n = 77) and NEAT-HFpEF [28] (n = 22). The success of the HFpEF program has centered on standardized procedures for the identification, diagnosis, and treatment of HFpEF patients. As described below, the clinical, echocardiographic, and invasive hemodynamic characteristics of patients enrolled in the Northwestern HFpEF Program, along with replication of the HFpEF program at other medical centers, have validated the ability to create successful HFpEF programs.
How to Identify Potential HFpEF Patients Systematically
Several “low-tech” and “high-tech” strategies can be used to identify HFpEF patients in a systematic fashion in order to build up referrals to HFpEF clinics, which can be particularly important when starting HFpEF programs. Of note at some institutions, identification of patients systematically will require approval from their local institutional review board, although this requirement is not universal. Besides jump-starting HFpEF clinic enrollment in the early stages of an HFpEF clinical program, systematic screening and identification of patients also helps ensure that patients who are evaluated by the HFpEF clinical program are likely to have the HFpEF syndrome.
Easy to implement, simple strategies to identify HFpEF patients include systematic screening of “hot spots” for HFpEF patients. These “hot spots” are outlined in Table 2. More sophisticated strategies include implementation of natural language processing (NLP) of the electronic health record (EHR). NLP—a branch of computer science that combines artificial intelligence and linguistics—uses machine learning algorithms to facilitate computer reading and interpretation of unstructured text that is commonplace in the EHR [29, 30]. NLP can be quite useful as a way to derive data from the EHR due to the large amount of unstructured, free text entries in hospital and clinic notes, discharge summaries, imaging reports, procedure reports, and the like.
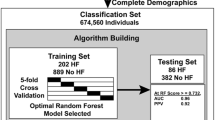
In the Northwestern HFpEF Program, potential patients were initially identified by an automated, NLP-based daily query of the inpatient EHR at Northwestern Memorial Hospital (at the time of hospitalization) using the following search criteria: (1) diagnosis of heart failure or the term heart failure in hospital notes; or (2) BNP >100 pg/mL; or (3) administration of ≥2 doses of intravenous diuretics. Identified patients were offered post-discharge follow-up in the Northwestern HFpEF Clinic if they met the following three inclusion criteria: age ≥21 years, LVEF ≥50 %, and presence of HF as defined by Framingham criteria [31]. After the index hospitalization, the HF diagnosis is confirmed in the outpatient HFpEF clinic. Although not required for the diagnosis, all patients enrolled in this way have been found to meet the European Society of Cardiology criteria for the diagnosis of HFpEF [32], as published previously [19, 25••, 26]. All patients who meet the aforementioned criteria are cared for in the HFpEF program; however, those with more than moderate valvular disease, previous cardiac transplantation, previous history of a reduced LVEF <40 % (i.e., recovered EF), severe LV dilation (LV end-diastolic volume >97 mL/m2), or constrictive pericarditis are excluded from HFpEF clinical studies and trials. As the Northwestern HFpEF Program has matured and become increasingly recognized, traditional referral pathways have increased; thus, although automated queries of inpatients with HFpEF still occur, many patients are referred as outpatients to the HFpEF program from referring providers.
Standardized Diagnosis and Assessment of HFpEF Patients
Treatment of HFpEF starts with an accurate diagnosis of the presence of HFpEF, its underlying etiology, and the pathophysiological factors that are present. It is important to note that the HFpEF diagnosis is often missed. Table 1 displays the diagnostic criteria for HFpEF that are used at Northwestern and other HFpEF programs. If there is doubt about the diagnosis (e.g., dyspneic patient without obvious fluid overload and normal BNP level), a right heart catheterization to measure hemodynamics and/or exercise testing to bring out the diagnosis should be entertained. If exercise testing during invasive hemodynamics is not available, a fluid challenge or even a passive leg raise maneuver can be helpful in making the HFpEF diagnosis [33].
Once the diagnosis is made, the next step is to look for the etiology of HFpEF. While it is easy to ascribe all HFpEF to common comorbidities (i.e., “garden variety” HFpEF), it is important to carefully evaluate for rare causes of HFpEF such as infiltrative cardiomyopathies and constrictive pericarditis, as these causes of HFpEF frequently have specific treatments that differ from other forms of HFpEF [34•]. Once rare causes of HFpEF are excluded, it is important to screen for common comorbidities. Supplementary Table S1 lists the standard laboratory, imaging, and other ancillary tests performed at Northwestern and other HFpEF programs when evaluating for the etiology and comorbidities underlying HFpEF. Supplementary Figure S1 displays the systematic screening for coronary artery disease in HFpEF patients. If the patient does not have a history of atrial fibrillation, cardiac rhythm monitoring should be performed given evidence to suggest that by the time atrial fibrillation is detected on surveillance electrocardiography sub-clinical cerebral infarcts are already present and are associated with measureable cognitive deficits [35].
Standardized Therapeutic Approach to HFpEF Patients
A standardized approach to treatment of HFpEF is an essential aspect of the HFpEF clinical program. Figure 1 displays a stepwise approach to the treatment of patients with HFpEF. This strategy includes general treatment recommendations (likely to be beneficial in the majority of HFpEF patients) and specific recommendations for phenotypic subsets (based on etiology, pathophysiology, or type of clinical presentation).
Stepwise approach to the treatment of heart failure with preserved ejection fraction: general approaches and tailored treatment based on phenotypic subtypes. HFpEF heart failure with preserved ejection fraction, ACE angiotensin converting enzyme, CAD coronary artery disease, LV left ventricular, BP blood pressure, PH pulmonary hypertension, CAD coronary artery disease, RHF right heart failure, AF atrial fibrillation, HCM hypertrophic cardiomyopathy
Once the diagnosis of HFpEF has been established, there are general treatment principles that will likely benefit the majority of patients with common forms of HFpEF. These management strategies (e.g., sodium/fluid restriction, blood pressure control [especially ACE-inhibitors or angiotensin receptor blockers], and diuretic therapy [particularly spironolactone]) are broadly applicable because they relate to the central manifestations of HF that are present in all HFpEF patients (fluid retention, sodium avidity, and elevated left atrial pressure) or they relate to common comorbidities (e.g., systemic hypertension). Intensive management of comorbidities has not been formally tested in HFpEF-specific clinical trials; nevertheless, our practice in our HFpEF programs is to managed comorbidities aggressively [36] (see Supplementary Table S2) given that these conditions are very common in HFpEF and compete with HFpEF to worsen prognosis [37]. Supplementary Figures S2–S3 display algorithms for the treatment of systemic hypertension [38] and use of mineralocorticoid receptor antagonists in HFpEF [27, 39–41]. Supplementary Table S3 summarizes the current evidence base for pharmacologic and non-pharmacologic treatment of HFpEF, which can be quickly recalled in the clinical setting using the mnemonic “ABCDE-LMNOP”. Finally, ongoing follow-up and prevention of HF hospitalizations are important aspects of dedicated HFpEF programs, mirroring many of the most helpful qualities of general HF clinics.
Validation of the HFpEF Clinical Program Paradigm
Although the Northwestern HFpEF Program has been able to enroll a large number of HFpEF patients consistently over a long-term period, proof of the validity of the program rests on several criteria. First, it is important to note that the patients identified using automated NLP-based search queries and ultimately enrolled into the Northwestern HFpEF program truly have objective criteria for the HFpEF diagnosis, as documented previously [17, 25••]. Second, patients enrolled in the Northwestern HFpEF Program are similar to those enrolled in epidemiology studies, observational registries, and HFpEF clinical trials as shown in Supplementary Table S4. Finally, and most importantly, since the creation of the original Northwestern HFpEF Program in 2007, the paradigm of a specialized HFpEF clinical program has been replicated at several other institutions, as described below (see also Table 3 which lists practical advice for starting and maintaining a HFpEF program).
University of Minnesota HFpEF Program
The University of Minnesota HFpEF program began in September 2013. Patients are identified using a standardized EHR list of patients hospitalized at the University of Minnesota Medical Center who have either (1) a diagnosis of heart failure or (2) elevated natriuretic peptide levels (NTproBNP >300 pg/ml). A trained clinic staff member screens the EHR list (which is generated daily) a few times a week using the algorithm outlined in Supplementary Figure S4. For identified patients who meet Framingham criteria for HF and who are likely to be able to come to clinic (i.e., no late-stage cancer diagnosis, hospice status, or extreme frailty), the clinic staff contacts the inpatient team or discharge coordinator, and rapid follow-up in the HFpEF clinic is arranged.
Besides standardized recruitment strategies, the Minnesota HFpEF Program has increased awareness of their HFpEF clinic through educational programs (outreach through grand rounds presentations to cardiologists, internists, geriatricians, pulmonologists, etc., and presentations to fellows in these programs). Similar strategies have been utilized at the Northwestern site as well.
The standardized diagnostic work-up and treatment of HFpEF patients at the University of Minnesota is similar to those outlined above. The Minnesota HFpEF Program has been quite successful. In its first 3 years, >250 patients with documented HFpEF have been cared for in the program, and these patients have been enrolled in a prospective research registry for improved phenotyping of HFpEF patients. In addition, these patients have been screened for and ultimately enrolled in the large-scale Novartis PARAGON-HF trial (a randomized controlled trial of LCZ696 [angiotensin receptor-neprilysin inhibitor] vs. placebo), making the Minnesota HFpEF Program a leading US enroller for the trial.
Johns Hopkins University HFpEF Program
The Johns Hopkins University HFpEF program began in July 2014. Patients were initially identified using a systematic search of all inpatients with the diagnosis of HF or symptoms and sign of decompensated HF, after which criteria for HFpEF (as described in Table 1) were applied. Currently, the primary referral source of patients for the Johns Hopkins HFpEF clinic is the HF Bridge Clinic, a HF outpatient clinic that is staffed by nurse practitioners. This clinic is primarily focused on patient visits for those recently discharged from hospital, with the goal to prevent readmission. The Johns Hopkins HF Bridge Clinic averages approximately ∼1000 visits per year, and nearly 50 % of the patients enrolled have HFpEF. Patients seen in the HF Bridge Clinic are referred to the HFpEF Clinic if they meet the criteria in Table 1.
Once referred to the Johns Hopkins HFpEF Program, the patients undergo a standardized evaluation that is similar to the ones used at the Northwestern and Minnesota HFpEF programs, as outlined in Supplementary Table S2. The Johns Hopkins HFpEF Program is unique in that it is predominantly African American, younger by nearly a decade, and with less of a female predominance compared to epidemiology studies and registries [42]. These differences likely reflect the urban environment and communities surrounding Johns Hopkins Hospital.
Since initiation of the Johns Hopkins HFpEF Program, >200 patients have been cared for in the program, and 94 patients have been enrolled in HFpEF clinical trials including ROPA-DOP, a single-center randomized controlled study of diuretic strategy and dopamine in acute decompensated HFpEF admitted to Johns Hopkins Hospital (clinicaltrials.gov identifier: NCT01901809); PARAGON-HF; and NEAT-HFpEF [28].
The Multidisciplinary Dyspnea Clinic: An Alternate Approach to a HFpEF Program
The University of Utah has taken an alternate approach to developing a HFpEF program by creating a multidisciplinary “Dyspnea Clinic” that is a joint venture between cardiologists and pulmonologists. In this particular program, the focus is on unexplained dyspnea, which is often due to HFpEF but could also be due to an alternate cause. Given the ubiquitous presence of dyspnea in HFpEF patients, the Dyspnea Clinic approach to HFpEF has been quite successful at the University of Utah.
The University of Utah Dyspnea Clinic began in July 2013. Patients are identified via traditional referral methods for the diagnoses of unexplained dyspnea, pulmonary hypertension, HFpEF, or connective tissue disease with dyspnea. Approximately 40 % of patients are referred internally from general medicine, cardiothoracic surgery, pulmonary, cardiology, and rheumatology clinics at the University of Utah; 40 % of patients are referred externally from surrounding hospitals and practices; and 20 % of patients are referred after a hospital discharge diagnosis of HFpEF or pulmonary hypertension. Patients seen in the Utah Dyspnea Clinic undergo a standardized diagnostic evaluation. From July 2015 to June 2016, the Utah Dyspnea Clinic had a total of 2912 patient visits (704 new patient visits, 2208 return patient visits). The Utah program has been a leading US enroller in the PARAGON-HF trial.
Because much of the surrounding region has a long-standing problem with physician shortages, the Utah Dyspnea Clinic has developed algorithms to evaluate and treat referrals within a large, 500-mile radius from their location. The clinic has also developed telemedicine and outreach programs (including mobile echocardiography) to care for their referral population, thereby allowing for the diagnosis of HFpEF over a large geographic region.
Staffing Needs and Reimbursement
The specific staffing needs and reimbursement models vary from institution to institution; however, it is clear from our collective experience that a multidisciplinary approach is essential. In some instances, such as the Utah Dyspnea Clinic, multiple subspecialities (e.g., cardiology and pulmonary) are represented in these clinics. A nurse and/or nurse practitioner (or other allied health professional) is essential for the care of patients with HFpEF, as shown repeatedly in research on general HF clinics. Given the high likelihood of polypharmacy, a pharmacist can also be quite helpful as part of the team. The multifaceted aspects of the HFpEF syndrome make it a perfect example of a clinical syndrome in need of a “patient-centered medical home” concept [43, 44].
Adequate reimbursement for services provided by HFpEF programs is essential for funding the personnel who staff these programs. However, given the typical older age of these patients (i.e., Medicare-eligible age range), the commitment of most hospitals to reduce HF (including HFpEF) readmissions as a quality metric; the high complexity of patient visits; and the multiple diagnostic tests and therapeutic modalities required for the optimal care for these patients, we have found that the economic rationale for HFpEF programs is readily apparent. Nevertheless, the costs (and potential savings) of HFpEF programs require further study.
Enrollment in HFpEF Clinical Trials
Enrollment in HFpEF clinical trials has proven to be quite challenging, likely because of poor recognition of the HFpEF syndrome, the therapeutic nihilism describe above, and the lack of awareness of the availability of clinical trials. For example, in the TOPCAT trial [27], which required 270 enrolling sites in six countries, the average enrollment rate was a dismal 2.3 patients per site per year worldwide, and even worse in the US (1.4 patients per site per year). One of the major benefits of dedicated HFpEF programs is that they augment HFpEF clinical trial enrollment (e.g., the rate of enrollment in TOPCAT at Northwestern University was 23.3 patients per year). Given the pressing need for the identification of novel therapies for HFpEF, it is important to optimize clinical trial enrollment in order to increase the efficiency and effectiveness of HFpEF clinical trials. Dedicated HFpEF clinical programs provide several advantages in that they have a large number of HFpEF patients who are cared for in a single place, they know how to diagnose HFpEF accurately, and they provided standardized care for these patients. The success of the four HFpEF programs described above serves as a testament to the utility of forming HFpEF clinical programs for the purpose of increasing HFpEF clinical trial enrollment.
Potential Challenges and Future Directions
Some may view HFpEF programs as examples of the “over-specialization” that plagues modern medicine, fragmenting medical care for these complex patients. Furthermore, some generalists may refrain from referring their patients to HFpEF programs because they fear that the specialty program will not provide collaborative care and instead will take over the care of their patient. We have found that contrary to these challenges, the development of HFpEF programs provides a chance for more holistic, comprehensive, multidisciplinary care, and could be viewed as a model for the multidisciplinary patient-centered medical home given the high comorbidity burden in the HFpEF syndrome. In addition, we have found it to be critically important to promote a collaborative care environment between the HFpEF specialist and the generalist, as advocated for other specialty programs.
The creation of dedicated HFpEF programs is still in its relative infancy. Progress towards transitioning these programs to the model of a patient-centered medical home, and validation of the clinical and economic effectiveness of HFpEF programs will be essential future initiatives. Finally, further expansion of HFpEF clinical programs to an increasing number of both academic and community healthcare institutions in geographically and socioeconomically diverse areas will be important to continue to increase HFpEF clinical trial enrollment and other scientific research initiatives for the HFpEF syndrome.
Conclusions
It is feasible to create HFpEF clinical programs that fulfill the major unmet need of identifying and caring for patients with HFpEF. These clinics are essential for confirming the HFpEF diagnosis, providing standardized treatment and facilitating clinical trial enrollment. It is our hope that the information provided here will encourage others to establish their own specialized HFpEF programs. Ultimately, we believe these HFpEF programs will serve as a model for patient-centered medical homes, thereby allowing for multidisciplinary care for these complex HFpEF patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Oktay AA, Rich JD, Shah SJ. The emerging epidemic of heart failure with preserved ejection fraction. Curr Heart Fail Rep. 2013;10(4):401–10.
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355(3):251–9.
••Shah SJ, Kitzman DW, Borlaug BA, et al. Phenotype-specific treatment of heart failure with preserved ejection fraction: a multiorgan roadmap. Circulation. 2016;134(1):73–90. This paper is a state of the art review on the current approach to treatment of HFpEF. Essential background reading for anyone interested in starting a HFpEF clinic.
Shah SJ, Katz DH, Deo RC. Phenotypic spectrum of heart failure with preserved ejection fraction. Heart Fail Clin. 2014;10(3):407–18.
Jaarsma T, van der Wal MH, Lesman-Leegte I, et al. Effect of moderate or intensive disease management program on outcome in patients with heart failure: Coordinating Study Evaluating Outcomes of Advising and Counseling in Heart Failure (COACH). Arch Intern Med. 2008;168(3):316–24.
Meijers WC, Hoekstra T, Jaarsma T, van Veldhuisen DJ, de Boer RA. Patients with heart failure with preserved ejection fraction and low levels of natriuretic peptides. Neth Heart J. 2016;24(4):287–95. This investigation, a secondary analysis of the multicenter COACH trial, which examined the efficacy of HF clinics, shows that natriuretic peptide levels are within the “normal” range in 30% of patients and that HFpEF patients makeup a very small part of current HF clinics.
Campbell RT, Jhund PS, Castagno D, Hawkins NM, Petrie MC, McMurray JJ. What have we learned about patients with heart failure and preserved ejection fraction from DIG-PEF, CHARM-preserved, and I-PRESERVE? J Am Coll Cardiol. 2012;60(23):2349–56.
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):e240–327.
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200.
Unzek S, Popovic ZB, Marwick TH. Effect of recommendations on interobserver consistency of diastolic function evaluation. J Am Coll Cardiol Img. 2011;4(5):460–7.
Anjan VY, Loftus TM, Burke MA, et al. Prevalence, clinical phenotype, and outcomes associated with normal B-type natriuretic peptide levels in heart failure with preserved ejection fraction. Am J Cardiol. 2012;110(6):870–6.
Kitzman DW, Shah SJ. The HFpEF obesity phenotype: the elephant in the room. J Am Coll Cardiol. 2016;68(2):200–3.
Iwanaga Y, Nishi I, Furuichi S, et al. B-type natriuretic peptide strongly reflects diastolic wall stress in patients with chronic heart failure: comparison between systolic and diastolic heart failure. J Am Coll Cardiol. 2006;47(4):742–8.
Shah SJ. Matchmaking for the optimization of clinical trials of heart failure with preserved ejection fraction: no laughing matter. J Am Coll Cardiol. 2013;62(15):1339–42.
Gustafsson F, Arnold JM. Heart failure clinics and outpatient management: review of the evidence and call for quality assurance. Eur Heart J. 2004;25(18):1596–604.
Thomas R, Huntley A, Mann M, et al. Specialist clinics for reducing emergency admissions in patients with heart failure: a systematic review and meta-analysis of randomised controlled trials. Heart. 2013;99(4):233–9.
Burke MA, Katz DH, Beussink L, et al. Prognostic importance of pathophysiologic markers in patients with heart failure and preserved ejection fraction. Circ Heart Fail. 2014;7(2):288–99.
Burkhoff D, Maurer MS, Joseph SM, et al. Left atrial decompression pump for severe heart failure with preserved ejection fraction: theoretical and clinical considerations. JACC Heart Fail. 2015;3(4):275–82.
Freed BH, Daruwalla V, Cheng JY, et al. Prognostic Utility and Clinical Significance of Cardiac Mechanics in Heart Failure With Preserved Ejection Fraction: Importance of Left Atrial Strain. Circ Cardiovasc Imaging. 2016;9(3):1–10.
Katz DH, Beussink L, Sauer AJ, Freed BH, Burke MA, Shah SJ. Prevalence, clinical characteristics, and outcomes associated with eccentric versus concentric left ventricular hypertrophy in heart failure with preserved ejection fraction. Am J Cardiol. 2013;112(8):1158–64.
Katz DH, Burns JA, Aguilar FG, Beussink L, Shah SJ. Albuminuria is independently associated with cardiac remodeling, abnormal right and left ventricular function, and worse outcomes in heart failure with preserved ejection fraction. JACC Heart Fail. 2014;2(6):586–96.
Klein DA, Katz DH, Beussink-Nelson L, Sanchez CL, Strzelczyk TA, Shah SJ. Association of chronic kidney disease with chronotropic incompetence in heart failure with preserved ejection fraction. Am J Cardiol. 2015;116(7):1093–100.
Selvaraj S, Ilkhanoff L, Burke MA, et al. Association of the frontal QRS-T angle with adverse cardiac remodeling, impaired left and right ventricular function, and worse outcomes in heart failure with preserved ejection fraction. J Am Soc Echocardiogr. 2014;27(1):74–82.e72.
Selvaraj S, Klein I, Danzi S, Akhter N, Bonow RO, Shah SJ. Association of serum triiodothyronine with B-type natriuretic peptide and severe left ventricular diastolic dysfunction in heart failure with preserved ejection fraction. Am J Cardiol. 2012;110(2):234–9.
Shah SJ, Katz DH, Selvaraj S, et al. Phenomapping for novel classification of heart failure with preserved ejection fraction. Circulation. 2015;131(3):269–79. This paper shows the heterogeneity of the HFpEF syndrome, a major reason why it is under-diagnosed. This paper also describes the Northwestern HFpEF program in detail, and is an example of the research performed using data from patients enrolled in the program.
Unger ED, Dubin RF, Deo R, et al. Association of chronic kidney disease with abnormal cardiac mechanics and adverse outcomes in patients with heart failure and preserved ejection fraction. Eur J Heart Fail. 2016;18(1):103–12.
Pitt B, Pfeffer MA, Assmann SF, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370(15):1383–92.
Redfield MM, Anstrom KJ, Levine JA, et al. Isosorbide mononitrate in heart failure with preserved ejection fraction. N Engl J Med. 2015;373(24):2314–24.
Hirschberg J, Manning CD. Advances in natural language processing. Science. 2015;349(6245):261–6.
Nadkarni PM, Ohno-Machado L, Chapman WW. Natural language processing: an introduction. J Am Med Inform Assoc. 2011;18(5):544–51.
McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971;285(26):1441–6.
Paulus WJ, Tschope C, Sanderson JE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28(20):2539–50.
Borlaug BA, Nishimura RA, Sorajja P, Lam CS, Redfield MM. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ Heart Fail. 2010;3(5):588–95.
Oktay AA, Shah SJ. Diagnosis and management of heart failure with preserved ejection fraction: 10 key lessons. Curr Cardiol Rev. 2015;11(1):42–52. This review article provides practical advice on how to diagnose and treat HFpEF, with pearls that can be quite helpful to those considering starting their own HFpEF program.
Chen LY, Lopez FL, Gottesman RF, et al. Atrial fibrillation and cognitive decline-the role of subclinical cerebral infarcts: the atherosclerosis risk in communities study. Stroke. 2014;45(9):2568–74.
Shah SJ, Gheorghiade M. Heart failure with preserved ejection fraction: treat now by treating comorbidities. JAMA. 2008;300(4):431–3.
Ather S, Chan W, Bozkurt B, et al. Impact of noncardiac comorbidities on morbidity and mortality in a predominantly male population with heart failure and preserved versus reduced ejection fraction. J Am Coll Cardiol. 2012;59(11):998–1005.
Oktay AA, Shah SJ. Current perspectives on systemic hypertension in heart failure with preserved ejection fraction. Curr Cardiol Rep. 2014;16(12):545.
Mitter SS, Shah SJ. Spironolactone for management of heart failure with preserved ejection fraction: Whither to After TOPCAT? Curr Atheroscler Rep. 2015;17(11):64.
Pfeffer MA, Braunwald E. Treatment of heart failure with preserved ejection fraction: reflections on its treatment with an aldosterone antagonist. JAMA Cardiol. 2016;1(1):7–8.
Flatt DM, Brown MC, Mizeracki AM, King BJ, Weber KT. Mineralocorticoid Receptor Antagonists in the Management of Heart Failure and Resistant Hypertension: A Review. JAMA Cardiol. 2016. (in press).
Sharma K, Hill T, Grams M, et al. Outcomes and worsening renal function in patients hospitalized with heart failure with preserved ejection fraction. Am J Cardiol. 2015;116(10):1534–40.
Arend J, Tsang-Quinn J, Levine C, Thomas D. The patient-centered medical home: history, components, and review of the evidence. Mt Sinai J Med. 2012;79(4):433–50.
Jackson GL, Powers BJ, Chatterjee R, et al. Improving patient care. The patient centered medical home. A Systematic Review. Ann Intern Med. 2013;158(3):169–78.
Acknowledgments
American Heart Association (0835488 N, 16SFRN28780016, and 15CVGPSD27260148) and National Institutes of Health (R01 HL107557 and R01 HL127028) to SJS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
Sanjiv J. Shah has received grant support from Actelion, Novartis, and AstraZeneca and consulting fees from Alnylam, AstraZeneca, Bayer, Merck, Novartis, Pfizer, and Sanofi.Rebecca Cogswell, John J. Ryan, and Kavita Sharma declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Heart Failure
Rights and permissions
About this article
Cite this article
Shah, S.J., Cogswell, R., Ryan, J.J. et al. How to Develop and Implement a Specialized Heart Failure with Preserved Ejection Fraction Clinical Program. Curr Cardiol Rep 18, 122 (2016). https://doi.org/10.1007/s11886-016-0802-1
Published:
DOI: https://doi.org/10.1007/s11886-016-0802-1