Abstract
The rising prevalence of diabetes in South Asians has significant health and economic implications. South Asians are predisposed to the development of diabetes due to biologic causes which are exacerbated by lifestyle and environmental factors. Furthermore, they experience significant morbidity and mortality from complications of diabetes, most notably coronary artery disease, cerebrovascular disease, and chronic kidney disease. Therefore, understanding the pathophysiology and genetics of diabetes risk factors and its associated complications in South Asians is paramount to curbing the diabetes epidemic. With this understanding, the appropriate screening, preventative and therapeutic strategies can be implemented and further developed. In this review, we discuss in detail the biologic and lifestyle factors that predispose South Asians to diabetes and review the epidemiology and pathophysiology of microvascular and macrovascular complications of diabetes in South Asians. We also review the ongoing and completed diabetes prevention and management studies in South Asians.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of diabetes worldwide is predicted to increase by 69 % in adults in developing countries between 2010 and 2030 [1]. Between 2010 and 2030, diabetes prevalence is expected to increase by 72 % in India, from 7.6 % to 9.1 %, with an estimated 87 million diabetic adults by year 2030 [1]. Data from the U.S. National Health Interview Survey from 1997-2008 showed that age- and sex-adjusted prevalence of type 2 diabetes in the U.S. was higher in Asian Americans (4.3-8.2 %) than in whites (3.8-6.0 %) and most notably, Asian Indians had the highest odds of diabetes [2]. A population-based study of U.S. Asian Indians found diabetes prevalence in adults was 17 % compared to 8 % in non-Hispanic whites, 13 % in non-Hispanic blacks, 10 % in Hispanic Latinos and 15 % in Native Americans/Alaskan natives [3]. Dampening the risk of diabetes across the South Asian population has significant health and economic implications.
This higher prevalence of diabetes in South Asians is multifactorial – due to both biologic and lifestyle factors, with urbanization and immigration playing a large role. South Asians have more visceral adiposity and insulin resistance, impaired β-cell function, and a genetic predisposition to diabetes which culminates in a markedly increased risk of diabetes [4–6]. Additionally, urbanization across Asia is leading to decreased physical activity, increased intake of dietary fats and processed foods and increased mental stress which amplify the effects of insulin resistance and abdominal obesity [4, 6]. Migration to more affluent countries has further contributed to the increasing prevalence of diabetes [6].
The health burden of diabetes and associated mortality is largely due to its microvascular and macrovascular complications – particularly cardiovascular disease. South Asians newly diagnosed with type 2 diabetes have a higher prevalence of complications at the time of diagnosis compared to Europeans – macrovascular disease (15.7 % vs. 9.4 %) and microvascular disease (27.3 % vs. 16.5 %) including retinopathy and nephropathy [7]. Several studies have demonstrated that compared to other ethnic groups, South Asians with diabetes have a higher mortality rate [8, 9].
The increasing prevalence of diabetes among South Asians along with the higher complication and mortality rate in this population urge the need for further research investigating the risk factors that predispose South Asians to diabetes and culturally tailored interventions that delay or prevent diabetes development. There is an urgent need for healthcare providers to identify and treat modifiable risk factors and for health organizations to develop and sustain programs that focus on diabetes prevention in South Asians. In this review, we discuss in detail the risk factors that predispose South Asians to diabetes, the macrovascular and microvascular complications among South Asians and preventative strategies that aim to curb this epidemic.
Factors that Predispose South Asians to Diabetes
Biologic Factors
Insulin Resistance
South Asians have a higher degree of insulin resistance (IR) compared to other ethnic groups and it plays a vital role in the development of diabetes. In the 1980s, Mohan et al. evaluated differences in the insulin response to an oral glucose load in Asian Indians compared to Europeans [10]. In both non-diabetic and diabetic Asian Indians, basal insulin levels were higher and insulin response to a glucose load was also higher suggesting that Asian Indians need higher levels of insulin to maintain euglycemia and secrete insulin at higher rates in response to the same amount of glucose [10].
This higher degree of IR in South Asians is partly explained by fetal adaptations that have become detrimental during modern day. The “thrifty genotype” hypothesis proposes that individuals can efficiently store energy during times of food abundance giving them a survival advantage during times of famine. With urbanization and immigration, this genotype now predisposes individuals to IR and diabetes [11]. The alternative explanation is the “thrifty phenotype” hypothesis which proposes that poor intrauterine nutrition leads to fetal adaptations in preparation for a life of starvation which leads to IR as these adaptations persist into childhood and adulthood [11]. Bavdekar et al. [12] demonstrated in 8 year old Indian children that lower birth weight was associated with higher IR as measured by homeostasis model assessment (HOMA). In a healthy adolescent urban South Indian population, IR was found in 30-55 % of adolescents [13]. IR is associated with cardiometabolic risk factors, including elevated triglycerides, elevated fasting plasma glucose and elevated blood pressure and with body composition parameters, including body mass index (BMI), waist circumference and body fat percentage [13].
This predisposition to IR persists into adulthood. Scholfield et al. demonstrated that Asian Indian vegetarians had significantly higher insulin levels compared to American vegetarians both in the fasting state and after an oral glucose load and a higher insulinogenic index [14]. Despite having comparable diets, Asian Indians were more likely to be insulin resistant. Also, Asian Indian men tend to be more insulin resistant than Caucasian men independent of truncal and generalized adiposity implying a metabolic defect [15]. A multi-ethnic study of healthy, young, lean adults demonstrated that Asian Indians, especially men, had a 2-3 fold higher prevalence of IR compared to other ethnic groups [16].
Pancreatic β-cell Dysfunction
Further increasing the risk of diabetes in South Asians is β-cell dysfunction. Once there is hyperglycemia, β-cell dysfunction is evident in those with type 2 diabetes [17]. However, β-cell dysfunction precedes the development of hyperglycemia and diabetes in South Asians. Petersen et al. evaluated β-cell responsiveness to an oral glucose load in healthy, lean Asian Indian and Caucasian men [16]. Asian Indians had a 28 % higher basal β-cell responsiveness compared with Caucasian men, but it was inadequate for their degree of IR as reflected by a 60 % lower disposition index [16]. In Indians living in South Africa, those with impaired glucose tolerance had delayed insulin responses after an oral glucose load [18] suggesting early β-cell dysfunction. A recent study done in Asian Indians in Chennai, India demonstrated that the oral disposition index, a marker of β-cell function, was more closely associated with dysglycemia than HOMA-IR [19].
Body Composition
For a given BMI, South Asians have a higher amount of total body fat compared to Caucasians [20] and higher amounts of abdominal adipose tissue including both subcutaneous fat and visceral fat [15, 21]. Adipose tissue is an active endocrine organ and intra-abdominal adipose tissue is strongly linked to IR in South Asians [22]. The higher risk of diabetes in South Asians is partly explained by body composition.
This predisposition to adiposity and IR begins during fetal development in South Asians. Yajnik et al. found that Indian babies were lighter and had smaller anthropometric measurements compared to babies born in the U.K., however, the skinfold thickness was the most preserved measurement [23]. This demonstrated that Indian babies preserved body fat during their intrauterine development which predisposes to future IR. Similar results were found in a study of South Indian children [24] in which subscapular skinfold thickness was larger in the Indian children while the other body measurements were smaller. Predictors of neonatal subscapular thickness included maternal BMI, maternal nutrition and socioeconomic status [23, 24]. This finding led to the concept of the thin-fat Indian baby where these babies are actually thin by weight but have relatively more adipose tissue. This higher subscapular thickness indicates a propensity for central body fat preservation [23, 24] which is associated with IR. This concept supports the “thrifty phenotype” hypothesis discussed above. Bhargava et al. followed a cohort born in Delhi that had a 10.8 % impaired glucose tolerance and 4.4 % diabetes prevalence as young adults. These adults had low BMI up to the age of two years followed by an early adiposity rebound and an accelerated increase in BMI until adulthood, with an average BMI of 26.2 kg/m2 [25]. Thinness in infancy was associated with abnormalities in glucose metabolism in adulthood.
Several studies in South Asian adults have investigated the role of body composition, especially abdominal obesity, in the development of IR and metabolic abnormalities. McKeigue et al. found that glucose intolerance was more strongly associated with waist-hip ratio (WHR) than with BMI and skinfold measures in a South Asian and European population [26]. For a given BMI, compared to Caucasians, Asian Indians have higher levels of generalized obesity, including more total body fat, subcutaneous fat and visceral fat, which are not always reflected in their non-obese BMI [27–30]. This higher visceral fat has been associated with more IR, dyslipidemia and metabolic syndrome which increase the risk for diabetes and cardiovascular disease [27–30]. Chandalia et al. demonstrated that larger adipocytes in the subcutaneous adipose tissue of South Asian men correlated with IR [31]. Therefore, both more visceral adipose tissue and larger adipocytes in the subcutaneous adipose tissue may play a role in the development of IR in South Asians by the adipose tissue’s function as an endocrine organ, increasing the risk of diabetes.
Biomarkers
Adipose tissue secretes adipokines that have metabolic consequences and further increase the risk of diabetes in South Asians.
Adiponectin is thought to play a role in the modulation of glucose and lipid metabolism in insulin sensitive tissues and decreased circulating adiponectin levels have been implicated in the pathogenesis of IR and diabetes [32]. Compared to Caucasians, Asian Indian men have lower levels of adiponectin independent of body fat content and distribution [33]. Lower levels of adiponectin correlate with insulin resistance; Asian Indians with diabetes have the lowest adiponectin levels [33, 34]. There is an inverse correlation between adiponectin and resistin, a pro-inflammatory cytokine [34].
Leptin, another hormone produced by adipocytes, is known to have insulin sensitizing and anorexigenic effects [35]. However, obese patients develop hyperleptinemia and become leptin resistant, which suppresses insulin action and contributes to IR [35]. Compared to Caucasian men, Asian Indian men have higher leptin levels irrespective of body composition [33]. Leptin levels are higher in South Asians with diabetes than those with impaired glucose tolerance and normal glucose tolerance [34].
C-reactive protein (CRP) is a pro-inflammatory marker that is associated with a higher risk of diabetes and cardiovascular disease [36, 37]. CRP levels are higher in South Asians compared to Europeans which is accounted for by central obesity and insulin resistance [38, 39]. Nondiabetic Asian Indian men have higher degrees of IR and higher levels of high sensitivity (hs)-CRP compared to Caucasian men, implying that a pro-inflammatory state is contributing to the increased risk of diabetes in this population [40]. Mohan et al. showed that in an urban south Indian population, hs-CRP levels were higher in diabetic individuals and values increased with increases in tertiles of HbA1c and body fat [41]. Therefore, CRP does seem to provide a link between adiposity and diabetes. These biomarkers may serve as clinical diagnostic tools in the future.
Genetic Risk Factors
Given the increasing prevalence of diabetes in South Asians, it is important to understand the underlying genetic predisposition. Genome-wide association studies have led to the discovery of approximately 60 genes associated with diabetes risk [42].
In South Asians, several polymorphisms have been discovered that are associated with risk factors that predispose to diabetes – including insulin resistance [43–46], pancreatic β-cell function [47–54], adiposity [44, 47, 49, 50, 55–64], and the metabolic syndrome [65–68]. There are several polymorphisms in South Asians that are associated with type 2 diabetes [43, 47–49, 51, 56, 57, 69] (Table 1). The EpiDREAM study investigated whether a gene score (calculated based on 16 single nucleotide polymorphisms (SNPs) associated with diabetes) could help predict the risk of incident type 2 diabetes [70•]. They found that South Asians have a greater genetic load for type 2 diabetes compared to Europeans and Latinos (12 % increased risk for each additional SNP vs. 8 %) but the gene score adds only marginal information when combined with clinical risk factors [70•]. Regardless, understanding the genetic underpinnings of type 2 diabetes and associated risk factors in South Asians will further elucidate the pathophysiology and potentially modifiable risk factors of diabetes in this high-risk population.
Lifestyle Factors
The Role of Urbanization and Migration
Rapid urbanization and migration with subsequent lifestyle changes have been implicated in the rising rates of diabetes in South Asians [71].
Singh et al. showed that urban inhabitants in Moradabad, India had a higher prevalence of diabetes compared to rural subjects (7.9 % vs. 2.5 %), comparable to the rates observed in migrants to the U.K. [72] The urban subjects also had a higher prevalence of dyslipidemia and the men had a greater WHR [72]. A study in southern India showed that villages had the lowest prevalence of diabetes at 9.2 % compared to 18.6 % in the city and 16.4 % in the town [71]. Over time, there has been an increased prevalence of diabetes even in the villages [71]. Therefore, urbanization is associated with an increased risk of diabetes. This was demonstrated by Ramachandran et al. where a sedentary lifestyle was an important predictor of diabetes [73].
Migration of South Asians to affluent countries like the U.S. results in a high prevalence of diabetes [74, 75]. Migrant Asian Indians from Gujarat to the U.K. had greater dietary energy intake, fat intake, cholesterol, triglycerides, non-esterified fatty acids and CRP than in non-migrants but diabetes prevalence was high in both populations [76].
Diet
The typical South Asian diet includes low intake of monounsaturated fatty acids, polyunsaturated fatty acids, and fiber and high intake of saturated fats, carbohydrates and trans-fatty acids [77]. These dietary factors have been associated with IR and dyslipidemia [77].
Urbanization and migration have further exacerbated some of these unhealthy dietary factors. In a population survey comparing rural and urban subjects in North India, Singh et al. showed that urban subjects ate more total and saturated fat, cholesterol and refined carbohydrates and fewer total and complex carbohydrates compared to rural subjects, and had a higher prevalence of diabetes and dyslipidemia [72].
Evaluation of diet in Indian migrants to the U.S. has shown that consumption of fruit juice, chips, margarine, cola, and alcoholic beverages has increased regardless of length of time in the U.S. [78]. However, longer term U.S. residents have decreased their consumption of high fat products such as ghee (clarified butter), butter, and milk [78]. The Oslo Immigrant Health study found that the majority of Sri Lankan migrants to Norway had increased their consumption of meat, milk, butter, margarine, and potatoes and about half of the Pakistani migrants had increased consumption of oil, meat, fish, and potatoes [79]. Both groups reported a decrease in bean and lentil consumption [79]. Increased consumption of these calorie- and energy-rich foods increases the risk of developing IR and subsequently diabetes [80].
Physical Inactivity
Physical activity is known to be effective in delaying and/or preventing the onset of type 2 diabetes [81–83]. However, with urbanization and migration, South Asians have been participating in less physical activity. A population survey of rural and urban dwellers in North India showed that energy expenditure during routine and spare time physical activity was higher in rural subjects [72]. A systematic review from the U.K. showed that South Asians were participating in approximately 50-75 % less physical activity compared to their European counterparts [84].
These low levels of physical activity have adverse consequences in South Asians. In a study of an urban South Indian population, the prevalence of diabetes was higher among those with less physical activity and HOMA-IR was higher in those who did light-grade activity compared with heavy-grade activity [85]. Similarly, in a migrant South Asian population in the U.K., Europeans were found to be more physically active than all South Asian groups and level of physical activity inversely correlated with blood glucose and insulin along with other components of the metabolic syndrome [86].
Macrovascular Complications of Diabetes (Table 2)
With the higher prevalence of diabetes in South Asians [1–3, 87], diabetes-related cardiovascular disease is expected to have a large health and economic burden amongst the South Asian population.
Coronary Artery Disease (CAD)
South Asians, with a three-fold higher prevalence of diabetes, have a higher incidence of CAD compared to Europeans [88]. In an 11-year follow-up study of diabetic individuals in the U.K., South Asians were 3.8 times more likely to report a history of myocardial infarction (MI) [9]. However, the U.K. Prospective Diabetes Study did not detect a difference in rates of MI between South Asians and white Europeans [89]. Although it is important to point out that the study authors state that there are potential biases that may have led to this finding including: the fact that they excluded subjects who had an MI in the year before diagnosis of diabetes and therefore South Asians included in this study may have been at a lower risk of MI to start with, that this may reflect a shorter duration of diabetes, and finally that the better socioeconomic status of South Asians in this particular study may have placed them at a lower risk of MI than the general diabetic South Asian population [89]. Similarly, in a large diabetes registry in Northern California, incidence of MI was similar between South Asians and Whites, and much higher than in other U.S. ethnic groups [90•]. Larger and longer term studies are needed to determine if South Asians with diabetes are at increased risk for MI and CAD compared to other ethnic groups.
However, diabetic South Asians have increased mortality from cardiovascular disease [8, 9, 91]. Studies investigating the mortality of South Asians with diabetes post-MI have had conflicting results. Wilkinson et al. [92] found that South Asians in London had a higher risk of death in the six months post-MI which was attributed to the higher prevalence of diabetes in the group [92]. On the other hand, a large retrospective cohort study from Canada showed that at median follow-up of 3.5 years, South Asians had a lower mortality rate compared to their Canadian counterparts [93].
Many studies have been done to determine what risk factors predispose diabetic South Asians to mortality from CAD. Game et al. investigated the applicability of the Framingham equation to a population of South Asian diabetes patients and found that the 10-year CAD risks were similar in South Asians and white Caucasians in the U.K. [94]. However, factors contributing to this risk differed in the two ethnic groups with South Asians having lower high-density lipoprotein (HDL) levels and higher total: HDL cholesterol ratios [94]. The authors proposed that different management of risk factors may account for the higher mortality from CAD in diabetic South Asians. However, there remain reservations about the applicability of the Framingham risk score and other scoring systems for South Asians as other studies have shown that they grossly underestimate the risk [95]. In addition, reference ranges that have been developed for various metabolic parameters have been derived using Western populations and therefore, may not apply to South Asians [95]. Some have proposed that adding 10 years to the age of South Asian patients gives a reasonably accurate measure of CAD risk [95].
The pathophysiology and genetic factors related to the increased CAD incidence and mortality in diabetic South Asians has been studied. Deepa et al. found that urban South Indian diabetic individuals with CAD had increased platelet activation, as measured by collagen induced glycoprotein (GP) IIb/IIIa binding, compared to non-diabetic South Asians without CAD [96]. Furthermore, results of a regression analysis showed that increased platelet activation was associated with CAD even after adjustment for HbA1c [96]. Paraoxonase1 (PON1) is an esterase that protects against oxidative modification of low-density lipoprotein and apolipoprotein A5 (APOA5) is an important determinant of plasma triglyceride levels [97]. Polymorphisms in both genes (see Table 2) were associated with CAD in diabetic South Indians [97]. Mannose-binding lectin (MBL) activates the lectin pathway of complement activation which causes vascular damage and hence atherosclerosis [98]. A study of type 2 diabetic South Asians in the Netherlands followed for 8 years showed that low MBL levels were associated with cardiovascular events [98]. Oxidative stress plays a role in the development of atherosclerotic plaque and subsequent ulceration and thrombosis [99]. NADPH oxidase and poly (ADP-ribose) polymerase-1 (PARP1) play a role in the formation of reactive oxygen species (ROS) and cellular dysfunction and death and polymorphisms in these genes can contribute to CAD and MI [99]. Several pathophysiologic mechanisms exist which may explain the increased incidence of and mortality from CAD in diabetic South Asians.
Cerebrovascular Disease
Several studies have shown a strong association between diabetes and stroke in South Asians. South Asians suffer most commonly from lacunar strokes which suggests small vessel disease attributed to the greater diabetes prevalence in South Asians [100]. A U.S. study found that South Asians with cerebrovascular events were three-fold more likely to have intracranial atherothrombosis and a greater prevalence of diabetes compared to European-Americans [101]. A community-based study in Pakistan demonstrated an overall 4.8 % prevalence of stroke and 11.6 % overall prevalence of diabetes, however, the prevalence of diabetes in the stroke population was much higher at 33.3 % [102]. Finally, a study in Qatar of patients with ischemic stroke, 32 % of whom were South Asian, showed that diabetes was present in 46.4 % of South Asians [103]. South Asians experience higher mortality from stroke compared to Europeans which has also been associated with diabetes [100, 104]. Results of the West Birmingham Stroke Project found that diabetes in migrant South Asians with ischemic stroke was associated with mortality [105].
Carotid intimal medial thickness (CIMT) is known to be a marker of atherosclerosis and a predictor of cardiovascular disease morbidity and mortality, including stroke [106, 107]. In India, the U.S. and Canada, diabetes has also been strongly associated with higher CIMT among South Asians [87, 106, 108] . In a Canadian study, every 0.9 % increase in HbA1c was associated with a 0.026 mm increase in CIMT and the curvilinear relationship was most evident at HbA1c levels > 5.7 % among South Asians [106]. The Chennai Urban Rural Epidemiology Study showed that even among those with normal glucose tolerance, increasing HbA1c was associated with significant increases in CIMT (mean CIMT of 0.651 mm for HbA1c <5.2 % compared to CIMT of 0.738 mm for HbA1c >5.8 %) [107]. Elevated homocysteine levels play a role in inflammation and the development of subclinical atherosclerosis [109]. The methylenetetrahydrofolate reductase (MTHFR) gene is involved in the metabolism of homocysteine and the C677T polymorphism is associated with increased homocysteine levels in South Asians [109].
Researchers have begun to study pathophysiologic mechanisms that can explain this association. In a study of South Asians stroke patients in the U.K., Gunarathne et al. showed that glycemic status was independently associated with impaired endothelial function and increased arterial stiffness; both mechanisms were worse among diabetic subjects [110]. Glycemic status impacts production of nitric oxide by the endothelium leading to decreased vascular smooth muscle relaxation and increased arterial stiffness [110]. In South Asians with ischemic stroke, there was a clustering of thrombotic factors (tissue plasminogen activator – t-PA, plasminogen activator inhibitor 1 – PAI-1, and fibrinogen) in those who had insulin resistance [111]. Therefore, glycemic status negatively impacts vascular function and increases thrombosis, both mechanisms observed in South Asian stroke patients.
Peripheral Arterial Disease (PAD)
PAD is an important complication of diabetes and South Asians with diabetes have higher rates of PAD. Diabetic South Asians in the U.K. had significantly higher ankle pressures compared to non-diabetic individuals [112]. In the Chennai Urban Population Study, the prevalence of PAD (ankle-brachial index [ABI] < 0.9) in those with normal glucose tolerance, impaired glucose tolerance and diabetes was 2.7, 2.9, and 6.3 %, respectively, and those with known diabetes had a 7.8 % PAD prevalence compared to 3.5 % in those newly diagnosed with diabetes [113]. South Asians tend to have more distal PAD which may be due to the higher diabetes prevalence and hence the predilection for smaller vessels [114].
However, South Asians seem to have lower rates of PAD compared to Europeans. In a study of European and Asian Indian men with a range of coronary disease, Asian Indians had less lower limb atherosclerosis and femoral intimal medial thickness for a given level of coronary disease and established risk factors did not explain this difference [115]. Diabetic South Asians in the U.K. had ankle pressures that were similar to those of diabetic Europeans who were 10 years older [112]. The Northwest Diabetes Foot Study showed that South Asians were less likely to have PAD compared to Europeans (9 % vs 24 %) and also had a lower risk of amputation [116]. South Asians were also found to have a lower risk of diabetic foot ulcers compared to Europeans – prevalence 5.5 % vs 1.8 % which was partly attributed to the lower rate of PAD [117].
Why this difference exists is not well understood. Some have hypothesized that due to early mortality from cardiovascular disease, South Asians do not live long enough to develop significant PAD [112, 114, 116]. Also, different vascular beds may respond differently to diabetes depending on the ethnicity of the patient [112, 114]. Finally, less smoking in the South Asian population may partially explain the lower rates of PAD [116, 117]. Studies to elucidate the biologic mechanisms behind the lower rates of PAD in diabetic South Asians are warranted.
Microvascular Complications of Diabetes (Table 3)
South Asians newly diagnosed with type 2 diabetes have a higher prevalence of microvascular complications, including retinopathy and nephropathy, at the time of diagnosis compared to Europeans – 27.3 % vs. 16.5 % [7]. Therefore, it is critical to understand the natural history of these complications in South Asians.
Diabetic Retinopathy (DR)
Diabetic retinopathy is a progressive disorder of the microcirculation of the retina and is the most common microvascular complication of diabetes [118, 119]. Retinopathy leads to visual impairment and is one of the leading causes of blindness [118]. Sight-threatening retinopathy includes proliferative retinopathy, severe non-proliferative retinopathy and clinically significant macular edema [119].
Several studies have demonstrated that South Asians have a higher prevalence of DR compared to Caucasians. Over 11 years of follow-up in the Southall Diabetes Survey, laser treatment for DR was more common in South Asians compared to Europeans – 36 % vs. 27 % [9]. In a diabetes clinic in the U.K., South Asians had three-fold higher odds of having sight-threatening retinopathy (STR) compared to Caucasians [120]; and for the same level of retinopathy, compared to South Asians, Caucasians were 12.5 years older and had diabetes for 12.5 years longer, suggesting that South Asians develop DR at a younger age and earlier in the course of disease [120]. The AdRem study found that 46 % of South Asians had DR compared to 31 % of Caucasians [118]. Similarly, the U.K. Asian Diabetes Study Retinopathy Study Group found that compared to Europeans, South Asians had a significantly higher prevalence of DR (45 % vs. 37 %) and STR (16 % vs. 12 %) [121]. Similarly, the DRIVE UK study found higher prevalence of DR (42 % vs. 38 %) and STR (10 % vs. 6 %) in South Asians vs. Europeans [119].
DR is not the only complication in this group. Retinal vascular lesions such as focal arterial narrowing and arteriovenous nicking are also seen in diabetes and are markers of subclinical vascular disease [118]. The AdRem study found that compared to Caucasians, South Asians had a higher prevalence of venous beading (6.3 % vs. 2.1 %) and arteriovenous nicking (8.5 % vs. 7.5 %) [118]. South Asians also had higher prevalence of visual impairment compared to white Europeans in the DRIVE UK study – 6.9 % vs. 3.3 % [122].
These data highlight the importance of understanding the risk factors associated with DR in South Asians. In a cross-sectional study of diabetic South Indians, duration of diabetes, HbA1c, male sex, macroalbuminuria, and insulin therapy were independent risk factors for severity of DR [123]. Raymond et al. found that South Asians with DR tended to have higher systolic and diastolic blood pressure, HbA1c, total cholesterol, and younger age at diagnosis [121]. The same was noted in South Asians with retinal vascular lesions [118]. Therefore, intensive control of these modifiable risk factors may help to decrease the prevalence of DR and its complications in South Asians.
Researchers are beginning to understand the genetic underpinnings of DR in South Asians. Several genes have been implicated including insulin-like growth factor 1 (IGF-1), endothelial nitric oxide synthase (eNOS), vascular endothelial growth factor (VEGF), inducible nitric oxide synthase (iNOS), tumor necrosis factor β (TNFβ), and aldose reductase (ALR2) [124–127]. IGF-1 triggers a cascade of molecular events that initiate retinal angiogenesis and in a diabetic South Indian cohort, the frequency of the 18 cytosine-adenine repeat genotype was higher in those with DR suggesting that it is a susceptibility genotype for DR [124]. The eNOS gene is involved in hypoxia-induced angiogenesis and therefore is thought to play a role in retinopathy associated neovascularization [125]. Certain genetic polymorphisms of VEGF have been associated with DR, however, no association was seen in a South Indian cohort [126]. Aldose reductase activity is increased in hyperglycemia [127]. In mice, knocking out iNOS leads to protection against DR [127], and TNFβ leads to an increase in vascular cell adhesion molecules which leads to recruitment of inflammatory cells to the site of vascular injury [127]. Specific allelic variations in each of these three genes were associated with susceptibility to DR in a South Indian cohort (Table 3) [127].
Diabetic Nephropathy (DNP) – Albuminuria and Chronic Kidney Disease (CKD)
Nephropathy is another complication of diabetes and CKD from diabetes is the leading cause of end-stage renal disease worldwide [128]. Albuminuria, an early measure of nephropathy, is an independent predictor of cardiovascular and all-cause mortality [129]. Ethnicity also influences the risk of DNP. Early studies showed that diabetics of Asian origin have much higher rates of end-stage renal failure compared to Caucasians [130, 131] and they are 5.8 times more likely to accept renal replacement therapy [132]. Therefore, a better understanding of the risk factors for and pathophysiology of DNP in South Asians is critical.
Many studies have found that the prevalence of nephropathy – both albuminuria and CKD -- is higher in the South Asian population. In a cross-sectional study in the U.K., the prevalence of microalbuminuria was greater in South Asians compared to Europeans (40 % vs. 33 % in men and 33 % vs. 19 % in women) [133]. South Asians had poorer glycemic control and more hypertension although this did not entirely account for the difference [133]. In the UKAD study, the proportion of South Asians with microalbuminuria was three times higher compared to white Europeans even with normal blood pressure [129]. The prevalence of proteinuria was 21 % in South Asians compared to 14 % in Whites [134]. Chandie Shaw et al. found that South Asians were four times more likely to develop albuminuria compared to Europeans and that loss of GFR was 1.45 times higher in South Asians after five years of follow-up [135]. Therefore, South Asians also have faster progression of their renal disease.
The prevalence of CKD in South Asians with diabetes is high. Stage 3 CKD was more prevalent in Whites compared to South Asians but stage 4-5 CKD was more common among South Asians [134]. Asian Indians had an almost 40-fold increased risk of end-stage diabetic nephropathy compared to the native Dutch population [136].
Understanding the pathophysiology of DNP in South Asians is important in preventing onset of the disease and delaying its progression. The renin-angiotensin-aldosterone system (RAAS) plays an important role in diabetic kidney disease [128]. Angiotensin II serves as a potent vasoconstrictor and causes an increase in intraglomerular pressure which results in proteinuria and glomerulosclerosis [128]. Polymorphisms in the angiotensinogen, aldosterone synthase, chymase, and angiotensin II receptor (AGTR1) are associated with diabetic CKD and DNP in Asian Indians [128, 137].
Cytokines also play an important role in the development of diabetic CKD [138]. Transforming growth factor β1 (TGFβ1) induces renal hypertrophy and fibrosis while cytokines like TNFα and monocyte chemoattractant protein-I (MCP-I, also known as CCL2 or chemokine (C-C motif) ligand 2), whose effects are mediated by chemokine receptors – CCR2 and CCR5, mediate infiltration of macrophages into the kidney [138]. Interleukin-8 (IL-8) is another chemokine produced by macrophages that has been found in the urine of patients with DNP and is associated with inflammatory renal injury [139]. Matrix metallopeptidase 9 (MMP9) is a collagenase that is involved in the breakdown of extracellular matrix (ECM), therefore, underexpression or decreased affinity for ECM can lead to excess accumulation of ECM and renal damage [139]. Polymorphisms in these genes can induce glomerulosclerosis and interstitial fibrosis, hence increasing risk of CKD. Studies have discovered several polymorphisms in these genes that are associated with diabetic CKD and higher risk of DNP in Asian Indians (see Table 3) [138, 139].
Another mechanism hypothesized to play a role in diabetic CKD is the dopaminergic pathway since dopamine is a natriuretic hormone that is involved in the regulation of blood pressure and salt-water reabsorption in the kidney [140]. Dopamine levels are determined by catechol-O-methyltransferase (COMT), the enzyme that metabolizes dopamine [140]. Dopamine receptors also influence components of the RAAS, and polymorphisms in dopamine receptor-2 and COMT are significantly associated with susceptibility to CKD in diabetic Asian Indians [140].
The oxidative stress pathway plays a role in the development of diabetic complications. In a case-control study of South and North Indians, there was differential genetic susceptibility in the oxidative stress pathway genes to diabetic CKD in South Indians and North Indians (see Table 3) [141]. Another study found that polymorphisms in the receptor for advanced glycation end products (RAGE) and glutamine:fructose-6-phosphate amidotransferase (GFPT2) genes were associated with diabetic CKD in Asian Indians [142]. Interaction between RAGE and its ligands leads to pro-inflammatory gene activation while expression of GFPT in mesangial cells leads to increased sclerosis by upregulating transcription of TGFβ1 and increase the risk of CKD [142].
Polymorphisms in the acetyl-coenzyme A carboxylase beta (ACACβ) and carnosine dipeptidase 1 (CNDP1) genes are also associated with DNP risk in South Asians [137, 143]. The, ACACβ gene is involved in fatty acid metabolism and expression of this gene can lead to accumulation of free fatty acids in cells and hence lipotoxicity [137]. The product of the CNDP1 gene is important for the breakdown of carnosine which is a ROS expressed in the human kidney and decreased gene expression can lead to nephropathy [143].
Diabetic Neuropathy (DNU)
Neuropathy is a very debilitating complication of diabetes and increases the risk of foot ulcers which may require eventual amputations, especially among patients with underlying PAD.
In a South Indian population, prevalence of DNU in patients attending a diabetes clinic was 19 % [144]. The Chennai Urban Rural Epidemiology Study showed that the prevalence of DNU was 26 % [145]. Risk factors associated with DNU included age, duration of diabetes, and glycated hemoglobin [144, 145].
Interestingly, the risk of DNU and its complications are lower in South Asians compared to Caucasians. The U.K. Prospective Diabetes Study Group showed that Asian Indians with newly diagnosed diabetes had lower rates of neuropathy (4 % vs. 13 %) diagnosed using the vibration sensation threshold [146]. Abbott et al. found that Asian Indians have significantly less large and small fiber neuropathy compared to Europeans [147]. The Northwest Diabetes Foot Care Study found that significantly fewer South Asians had abnormal vibration sensation and abnormal temperature sensation [117]. Other studies have also found that South Asians have significantly less neuropathy than Europeans [116, 148]. The lower prevalence of neuropathy has been attributed to shorter height, less smoking, and more favorable skin microcirculation [147].
Accompanying the lower risk of neuropathy, South Asians also have a lower risk of diabetes-related amputations and foot ulcers [90•]. Between 1980-1985, the rate of lower extremity amputation was lower in Asians compared to Caucasians – 3.4 vs. 14.2 cases per 10,000 patient-years [149]. Data from the Northwest Diabetes Foot Study showed that South Asians had significantly lower odds of both amputation and foot ulcer when compared to Europeans [116, 117]. The lower risk of these complications is partly attributed to the lower prevalence of neuropathy in the South Asian population as well as less smoking, lower prevalence of PAD, less insulin use, and lower prevalence of foot deformities [116, 117].
Detection and Prevention of Diabetes in South Asians
Given the rising prevalence of diabetes in the South Asian population and the morbidity and mortality associated with diabetes and its complications, strategies to detect and prevent the onset of diabetes are important.
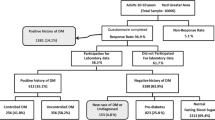
Detection of Diabetes
There are multiple diabetes risk scores [150, 151], however, these have not been validated in South Asians. Using both urban and rural populations in India, investigators developed and validated the Indian Diabetes Risk Score (IDRS) to detect undiagnosed diabetes in Indians [152••]. The score takes into account age, sex, waist circumference, physical activity, and family history and can be calculated on-line (http://www.drmohansdiabetes.com/), with a score of ≥ 60 out of 100 considered high risk [152••]. This score has not been tested against other existing diabetes risk scores. However, one notable difference between the American Diabetes Association (ADA) risk score and the IDRS is that the IDRS uses waist circumference instead of BMI which is likely a better predictor of diabetes risk in South Asians. Therefore, the IDRS can serve as a cost-effective screening tool in South Asians that can be implemented on a large scale and easily identify modifiable risk factors [153].
Prior Studies of Prevention
Studies focusing on diabetes prevention in South Asians have had promising results and translation of these findings to the community is likely to have a significant impact.
The Indian Diabetes Prevention Programme-1 (IDPP-1) was a randomized controlled trial of 531 South Asians recruited from the workplace with impaired glucose tolerance (IGT, mean age 45.9 years) that studied the effect of metformin and lifestyle modification on progression to diabetes [154]. Participants were followed for a median of 30 months and the 3-year cumulative incidence of diabetes was: 55 % in the control group, 39.3 % in the lifestyle modification group, 40.5 % in the metformin group, and 39.5 % in the combined lifestyle modification and metformin group [154]. The number needed to prevent one incident case of diabetes was 6.4 for lifestyle modification, 6.9 for metformin, and 6.5 for combined lifestyle modification and metformin [154]. Therefore, both metformin and the lifestyle interventions were successful in reducing the incidence of diabetes although there was no added benefit from combining both interventions. Snehalatha et al. found that these beneficial outcomes occurred due to improved insulin action and sensitivity caused by the intervention strategies [155].
A follow-up study, the IDPP-2, was done to evaluate the effects of pioglitazone [156]. The study included 407 subjects with IGT (mean age 45.3 years) who were randomized to pioglitazone 30 mg or placebo with lifestyle modification in both arms and followed for 3 years for diabetes outcomes [156]. There was no significant difference in diabetes incidence between the two groups – 29.8 % in the pioglitazone group and 31.6 % in the placebo group [156]. In contrast to other positive studies of thiazolidinediones [157], this finding may suggest an ethnicity-related difference.
The United Kingdom Asian Diabetes Study (UKADS) was a cluster randomized controlled trial of 1486 South Asians with type 2 diabetes that investigated the effectiveness of a culturally sensitive, enhanced care package in U.K. general practices in improving cardiovascular risk factors over 2 years [158]. The intervention included additional time with the practice nurse and support from a link worker and diabetes-specialist nurse [158]. While the intervention was not cost-effective, they did achieve significant decreases in systolic and diastolic blood pressure and cholesterol across the whole study population attributed to the use of anti-hypertensive medications and statins [158]. While the clinical outcomes of this study were modest and glycemic control did not improve, the study suggests that intensive management can be effective in this population although significant work to enhance effectiveness of healthcare delivery remains to be done [158].
Ongoing Studies of Prevention
There are several ongoing studies investigating methods to prevent diabetes in South Asians.
In India, the Diabetes Community Lifestyle Improvement Program (D-CLIP, Clinical Trials Registry No; NCT 01283308) study is an ongoing randomized trial evaluating the effectiveness, cost-effectiveness, and sustainability of a culturally appropriate lifestyle intervention and metformin in diabetes prevention in high-risk individuals in Chennai, India over 3 years of follow-up [159]. The results of this study will help frame policy and public health recommendations.
In the U.K., the Prevention of Diabetes and Obesity in South Asians (PODOSA) study is an ongoing cluster, randomized controlled trial evaluating the effects of weight loss and increased physical activity in preventing the onset of type 2 diabetes in a high-risk Indian and Pakistani population [160]. The intervention is intensive counseling with 15 dietician visits, with weight change over 3 years being the primary outcome [160].
In the U.S., the South Asian Health and Prevention Education (SHAPE, Clinical Trials Registry No; NCT 01084928) study is evaluating the effectiveness of a culturally appropriate lifestyle intervention in the prevention of diabetes in the South Asian community with pre-diabetes [161]. The intervention is based on the Diabetes Prevention Program but tailored to the needs of the community based on feedback gathered from focus groups [161]. Participants are being followed for two years and the primary outcome is weight change [161].
Results from these ongoing studies and prior studies will aid in making recommendations for diabetes prevention in South Asians and eventually lead to the development of large scale prevention programs.
Conclusion
Type 2 diabetes in South Asians is expected to rise over the next several years with India projected to have the largest diabetic population in 2030 [1]. South Asians have several underlying risk factors that predispose them to diabetes including more insulin resistance, higher visceral adiposity despite a non-obese BMI, impaired β-cell function, an abnormal adipokine profile, and certain high risk genetic polymorphisms. In addition, urbanization and migration have led to detrimental lifestyle changes affecting diet and physical activity. The underlying biologic and genetic predisposition in combination with the lifestyle changes have ignited this epidemic of diabetes. Mortality in South Asians with diabetes is higher than that of other ethnic groups, primarily due to cardiovascular disease. Compared to Caucasians, South Asians have a higher incidence of CAD and cerebrovascular disease but a lower incidence of PAD, which is not entirely understood. In terms of microvascular complications, compared to Caucasians, South Asians have a higher incidence of retinopathy and nephropathy but a lower incidence of neuropathy which is also not well understood. Research is underway to understand the biologic mechanisms and genetic polymorphisms that play a role in the development of these diabetes complications. Given the great economic and health burden of diabetes and its complications in South Asians, the focus should be on prevention. Lifestyle modification and metformin therapy have been proven to prevent or delay diabetes in South Asians. Several ongoing studies are investigating the effectiveness of different culturally tailored lifestyle interventions [159–161]. We are optimistic that the results of these studies will help to foster changes in public health and health policy and thereby help to reduce the incidence of diabetes and its complications in the South Asian community worldwide.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14.
Lee JW, Brancati FL, Yeh HC. Trends in the prevalence of type 2 diabetes in Asians versus Whites: Results from the United States National Health Interview Survey, 1997-2008. Diabetes Care. 2011;34(2):353–7.
Misra R, Patel T, Kotha P, et al. Prevalence of diabetes, metabolic syndrome, and cardiovascular risk factors in US Asian Indians: Results from a national study. J Diabetes Complicat. 2010;24(3):145–53.
Mohan V. Why are Indians more prone to diabetes? J Assoc Physicians India. 2004;52:468–74.
Chan JC, Malik V, Jia W, et al. Diabetes in Asia: Epidemiology, risk factors, and pathophysiology. JAMA. 2009;301(20):2129–40.
Ramachandran A, Ma RC, Snehalatha C. Diabetes in Asia. Lancet. 2010;375(9712):408–18.
Chowdhury TA, Lasker SS. Complications and cardiovascular risk factors in South Asians and Europeans with early-onset type 2 diabetes. QJM. 2002;95(4):241–6.
Swerdlow AJ, Laing SP, Dos Santos SI, et al. Mortality of South Asian patients with insulin-treated diabetes mellitus in the United Kingdom: A cohort study. Diabet Med. 2004;21(8):845–51.
Mather HM, Chaturvedi N, Fuller JH. Mortality and morbidity from diabetes in South Asians and Europeans: 11-year follow-up of the Southall Diabetes Survey, London, UK. Diabet Med. 1998;15(1):53–9.
Mohan V, Sharp PS, Cloke HR, Burrin JM, Schumer B, Kohner EM. Serum immunoreactive insulin responses to a glucose load in Asian Indian and European type 2 (non-insulin-dependent) diabetic patients and control subjects. Diabetologia. 1986;29(4):235–7.
Hu FB. Globalization of diabetes: The role of diet, lifestyle, and genes. Diabetes Care. 2011;34(6):1249–57.
Bavdekar A, Yajnik CS, Fall CH, et al. Insulin resistance syndrome in 8-year-old Indian children: Small at birth, big at 8 years, or both? Diabetes. 1999;48(12):2422–9.
Ramachandran A, Snehalatha C, Yamuna A, Murugesan N, Narayan KM. Insulin resistance and clustering of cardiometabolic risk factors in urban teenagers in southern India. Diabetes Care. 2007;30(7):1828–33.
Scholfield DJ, Behall KM, Bhathena SJ, Kelsay J, Reiser S, Revett KR. A study on Asian Indian and American vegetarians: Indications of a racial predisposition to glucose intolerance. Am J Clin Nutr. 1987;46(6):955–61.
Chandalia M, Abate N, Garg A, Stray-Gundersen J, Grundy SM. Relationship between generalized and upper body obesity to insulin resistance in Asian Indian men. J Clin Endocrinol Metab. 1999;84(7):2329–35.
Petersen KF, Dufour S, Feng J, et al. Increased prevalence of insulin resistance and nonalcoholic fatty liver disease in Asian-Indian men. Proc Natl Acad Sci U S A. 2006;103(48):18273–7.
Kahn SE. The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of type 2 diabetes. Diabetologia. 2003;46(1):3–19.
Motala AA, Omar MA. Evidence for impaired pancreatic beta cell function in South African Indians with impaired glucose tolerance. Diabet Med. 1994;11(5):437–44.
Staimez LR, Weber MB, Ranjani H, et al. Evidence of reduced beta-cell function in Asian Indians with mild dysglycemia. Diabetes Care. 2013;36(9):2772–8.
Deurenberg-Yap M, Schmidt G, van Staveren WA, Deurenberg P. The paradox of low body mass index and high body fat percentage among Chinese, Malays and Indians in Singapore. Int J Obes Relat Metab Disord. 2000;24(8):1011–7.
Lear SA, Humphries KH, Kohli S, Chockalingam A, Frohlich JJ, Birmingham CL. Visceral adipose tissue accumulation differs according to ethnic background: Results of the Multicultural Community Health Assessment Trial (M-CHAT). Am J Clin Nutr. 2007;86(2):353–9.
Sharp PS, Mohan V, Levy JC, Mather HM, Kohner EM. Insulin resistance in patients of Asian Indian and European origin with non-insulin dependent diabetes. Horm Metab Res. 1987;19(2):84–5.
Yajnik CS, Fall CH, Coyaji KJ, et al. Neonatal anthropometry: The thin-fat Indian baby. The Pune Maternal Nutrition Study. Int J Obes Relat Metab Disord. 2003;27(2):173–80.
Krishnaveni GV, Hill JC, Veena SR, et al. Truncal adiposity is present at birth and in early childhood in South Iindian children. Indian Pediatr. 2005;42(6):527–38.
Bhargava SK, Sachdev HS, Fall CH, et al. Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med. 2004;350(9):865–75.
McKeigue PM, Pierpoint T, Ferrie JE, Marmot MG. Relationship of glucose intolerance and hyperinsulinaemia to body fat pattern in South Asians and Europeans. Diabetologia. 1992;35(8):785–91.
Banerji MA, Faridi N, Atluri R, Chaiken RL, Lebovitz HE. Body composition, visceral fat, leptin, and insulin resistance in Asian Indian men. J Clin Endocrinol Metab. 1999;84(1):137–44.
Raji A, Seely EW, Arky RA, Simonson DC. Body fat distribution and insulin resistance in healthy Asian Indians and Caucasians. J Clin Endocrinol Metab. 2001;86(11):5366–71.
Sandeep S, Gokulakrishnan K, Velmurugan K, Deepa M, Mohan V. Visceral & subcutaneous abdominal fat in relation to insulin resistance & metabolic syndrome in non-diabetic South Indians. Indian J Med Res. 2010;131:629–35.
Indulekha K, Anjana RM, Surendar J, Mohan V. Association of visceral and subcutaneous fat with glucose intolerance, insulin resistance, adipocytokines and inflammatory markers in Asian Indians (CURES-113). Clin Biochem. 2011;44(4):281–7.
Chandalia M, Lin P, Seenivasan T, et al. Insulin resistance and body fat distribution in South Asian men compared to Caucasian men. PLoS One. 2007;2(8):e812.
Chandran M, Phillips SA, Ciaraldi T, Henry RR. Adiponectin: More than just another fat cell hormone? Diabetes Care. 2003;26(8):2442–50.
Abate N, Chandalia M, Snell PG, Grundy SM. Adipose tissue metabolites and insulin resistance in nondiabetic Asian Indian men. J Clin Endocrinol Metab. 2004;89(6):2750–5.
Wasim H, Al-Daghri NM, Chetty R, McTernan PG, Barnett AH, Kumar S. Relationship of serum adiponectin and resistin to glucose intolerance and fat topography in South-Asians. Cardiovasc Diabetol. 2006;5:10.
Rabe K, Lehrke M, Parhofer KG, Broedl UC. Adipokines and insulin resistance. Mol Med. 2008;14(11–12):741–51.
Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM. C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA. 2001;286(3):327–34.
Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336(14):973–9.
Forouhi NG, Sattar N, McKeigue PM. Relation of C-reactive protein to body fat distribution and features of the metabolic syndrome in Europeans and South Asians. Int J Obes Relat Metab Disord. 2001;25(9):1327–31.
Chambers JC, Eda S, Bassett P, et al. C-reactive protein, insulin resistance, central obesity, and coronary heart disease risk in Indian Asians from the United Kingdom compared with European whites. Circulation. 2001;104(2):145–50.
Chandalia M, Cabo-Chan Jr AV, Devaraj S, Jialal I, Grundy SM, Abate N. Elevated plasma high-sensitivity C-reactive protein concentrations in Asian Indians living in the United States. J Clin Endocrinol Metab. 2003;88(8):3773–6.
Mohan V, Deepa R, Velmurugan K, Premalatha G. Association of C-reactive protein with body fat, diabetes and coronary artery disease in Asian Indians: The Chennai Urban Rural Epidemiology Study (CURES-6). Diabet Med. 2005;22(7):863–70.
Gujral UP, Pradeepa R, Weber MB, Narayan KM, Mohan V. Type 2 diabetes in South Asians: Similarities and differences with white Caucasian and other populations. Ann N Y Acad Sci. 2013;1281:51–63.
Kooner JS, Saleheen D, Sim X, et al. Genome-wide association study in individuals of South Asian ancestry identifies six new type 2 diabetes susceptibility loci. Nat Genet. 2011;43(10):984–9.
Chambers JC, Elliott P, Zabaneh D, et al. Common genetic variation near MC4R is associated with waist circumference and insulin resistance. Nat Genet. 2008;40(6):716–8.
Abate N, Carulli L, Cabo-Chan Jr A, Chandalia M, Snell PG, Grundy SM. Genetic polymorphism PC-1 K121Q and ethnic susceptibility to insulin resistance. J Clin Endocrinol Metab. 2003;88(12):5927–34.
Vaidya A, Williams JS. Vitamin D and insulin sensitivity: Can gene association and pharmacogenetic studies of the vitamin D receptor provide clarity? Metabolism. 2012;61(6):759–61.
Sanghera DK, Ortega L, Han S, et al. Impact of nine common type 2 diabetes risk polymorphisms in Asian Indian Sikhs: PPARG2 (Pro12Ala), IGF2BP2, TCF7L2 and FTO variants confer a significant risk. BMC Med Genet. 2008;9:59-2350-9-59.
Chauhan G, Spurgeon CJ, Tabassum R, et al. Impact of common variants of PPARG, KCNJ11, TCF7L2, SLC30A8, HHEX, CDKN2A, IGF2BP2, and CDKAL1 on the risk of type 2 diabetes in 5,164 Indians. Diabetes. 2010;59(8):2068–74.
Rees SD, Hydrie MZ, Shera AS, et al. Replication of 13 genome-wide association (GWA)-validated risk variants for type 2 diabetes in Pakistani populations. Diabetologia. 2011;54(6):1368–74.
Sanghera DK, Demirci FY, Been L, et al. PPARG and ADIPOQ gene polymorphisms increase type 2 diabetes mellitus risk in Asian Indian Sikhs: Pro12Ala still remains as the strongest predictor. Metabolism. 2010;59(4):492–501.
Humphries SE, Gable D, Cooper JA, et al. Common variants in the TCF7L2 gene and predisposition to type 2 diabetes in UK European whites, Indian Asians and Afro-Caribbean men and women. J Mol Med (Berl). 2006;84(12):1005–14.
Tan JT, Nurbaya S, Gardner D, Ye S, Tai ES, Ng DP. Genetic variation in KCNQ1 associates with fasting glucose and beta-cell function: A study of 3,734 subjects comprising three ethnicities living in Singapore. Diabetes. 2009;58(6):1445–9.
Been LF, Ralhan S, Wander GS, et al. Variants in KCNQ1 increase type II diabetes susceptibility in South Asians: A study of 3,310 subjects from India and the US. BMC Med Genet. 2011;12:18-2350-12-18.
Sanghera DK, Been L, Ortega L, et al. Testing the association of novel meta-analysis-derived diabetes risk genes with type II diabetes and related metabolic traits in Asian Indian Sikhs. J Hum Genet. 2009;54(3):162–8.
Chauhan G, Tabassum R, Mahajan A, et al. Common variants of FTO and the risk of obesity and type 2 diabetes in Indians. J Hum Genet. 2011;56(10):720–6.
Ramya K, Radha V, Ghosh S, Majumder PP, Mohan V. Genetic variations in the FTO gene are associated with type 2 diabetes and obesity in South Indians (CURES-79). Diabetes Technol Ther. 2011;13(1):33–42.
Yajnik CS, Janipalli CS, Bhaskar S, et al. FTO gene variants are strongly associated with type 2 diabetes in South Asian Indians. Diabetologia. 2009;52(2):247–52.
Vasan SK, Fall T, Neville MJ, et al. Associations of variants in FTO and near MC4R with obesity traits in South Asian Indians. Obesity (Silver Spring). 2012;20(11):2268–77.
Rees SD, Islam M, Hydrie MZ, et al. An FTO variant is associated with type 2 diabetes in South Asian populations after accounting for body mass index and waist circumference. Diabet Med. 2011;28(6):673–80.
Radha V, Vimaleswaran KS, Ayyappa KA, Mohan V. Association of lipoprotein lipase gene polymorphisms with obesity and type 2 diabetes in an Asian Indian population. Int J Obes (Lond). 2007;31(6):913–8.
Cassell PG, Saker PJ, Huxtable SJ, et al. Evidence that single nucleotide polymorphism in the uncoupling protein 3 (UCP3) gene influences fat distribution in women of European and Asian origin. Diabetologia. 2000;43(12):1558–64.
Bhagat N, Agrawal M, Luthra K, Vikram NK, Misra A, Gupta R. Evaluation of single nucleotide polymorphisms of Pro12Ala in peroxisome proliferator-activated receptor-gamma and Gly308Ala in tumor necrosis factor-alpha genes in obese Asian Indians: A population-based study. Diabetes Metab Syndr Obes. 2010;3:349–56.
Qi L, Tai ES, Tan CE, et al. Intragenic linkage disequilibrium structure of the human perilipin gene (PLIN) and haplotype association with increased obesity risk in a multiethnic Asian population. J Mol Med (Berl). 2005;83(6):448–56.
Shen H, Qi L, Tai ES, Chew SK, Tan CE, Ordovas JM. Uncoupling protein 2 promoter polymorphism -866G/A, central adiposity, and metabolic syndrome in Asians. Obesity (Silver Spring). 2006;14(4):656–61.
Guettier JM, Georgopoulos A, Tsai MY, et al. Polymorphisms in the fatty acid-binding protein 2 and apolipoprotein C-III genes are associated with the metabolic syndrome and dyslipidemia in a South Indian population. J Clin Endocrinol Metab. 2005;90(3):1705–11.
Vimaleswaran KS, Radha V, Mohan V. Thr54 allele carriers of the Ala54Thr variant of FABP2 gene have associations with metabolic syndrome and hypertriglyceridemia in urban South Indians. Metabolism. 2006;55(9):1222–6.
Dodani S, Henkhaus R, Dong L, Butler MG. Apolipoprotein A1 gene polymorphisms predict cardio-metabolic risk in South Asian immigrants. Dis Markers. 2012;32(1):9–19.
Ranjith N, Pegoraro RJ, Rom L. Lipid profiles and associated gene polymorphisms in young Asian Indian patients with acute myocardial infarction and the metabolic syndrome. Metab Syndr Relat Disord. 2009;7(6):571–8.
Vimaleswaran KS, Radha V, Ghosh S, et al. Peroxisome proliferator-activated receptor-gamma co-activator-1alpha (PGC-1alpha) gene polymorphisms and their relationship to type 2 diabetes in Asian Indians. Diabet Med. 2005;22(11):1516–21.
Anand SS, Meyre D, Pare G, et al. Genetic information and the prediction of incident type 2 diabetes in a high-risk multiethnic population: The EpiDREAM genetic study. Diabetes Care. 2013;36(9):2836–42. This study investigated the role of a gene score (using 16 polymorphisms known to be associated with diabetes) in predicting incident diabetes. They looked at several ethnic groups, including South Asians.
Ramachandran A, Mary S, Yamuna A, Murugesan N, Snehalatha C. High prevalence of diabetes and cardiovascular risk factors associated with urbanization in India. Diabetes Care. 2008;31(5):893–8.
Singh RB, Ghosh S, Niaz AM, et al. Epidemiologic study of diet and coronary risk factors in relation to central obesity and insulin levels in rural and urban populations of North India. Int J Cardiol. 1995;47(3):245–55.
Ramachandran A, Snehalatha C, Latha E, Manoharan M, Vijay V. Impacts of urbanisation on the lifestyle and on the prevalence of diabetes in native Asian Indian population. Diabetes Res Clin Pract. 1999;44(3):207–13.
Abate N, Chandalia M. Ethnicity, type 2 diabetes & migrant Asian Indians. Indian J Med Res. 2007;125(3):251–8.
Mohanty SA, Woolhandler S, Himmelstein DU, Bor DH. Diabetes and cardiovascular disease among Asian Indians in the United States. J Gen Intern Med. 2005;20(5):474–8.
Patel JV, Vyas A, Cruickshank JK, et al. Impact of migration on coronary heart disease risk factors: Comparison of Gujaratis in Britain and their contemporaries in villages of origin in India. Atherosclerosis. 2006;185(2):297–306.
Misra A, Khurana L, Isharwal S, Bhardwaj S. South Asian diets and insulin resistance. Br J Nutr. 2009;101(4):465–73.
Raj S, Ganganna P, Bowering J. Dietary habits of Asian Indians in relation to length of residence in the United States. J Am Diet Assoc. 1999;99(9):1106–8.
Wandel M, Raberg M, Kumar B, Holmboe-Ottesen G. Changes in food habits after migration among South Asians settled in Oslo: The effect of demographic, socio-economic and integration factors. Appetite. 2008;50(2–3):376–85.
Garduno-Diaz SD, Khokhar S. Prevalence, risk factors and complications associated with type 2 diabetes in migrant South Asians. Diabetes Metab Res Rev. 2012;28(1):6–24.
Helmrich SP, Ragland DR, Leung RW, Paffenbarger Jr RS. Physical activity and reduced occurrence of non-insulin-dependent diabetes mellitus. N Engl J Med. 1991;325(3):147–52.
Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403.
Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20(4):537–44.
Fischbacher CM, Hunt S, Alexander L. How physically active are South Asians in the United Kingdom? A literature review. J Public Health (Oxf). 2004;26(3):250–8.
Mohan V, Gokulakrishnan K, Deepa R, Shanthirani CS, Datta M. Association of physical inactivity with components of metabolic syndrome and coronary artery disease–the Chennai Urban Population Study (CUPS no. 15). Diabet Med. 2005;22(9):1206–11.
Hayes L, White M, Unwin N, et al. Patterns of physical activity and relationship with risk markers for cardiovascular disease and diabetes in Indian, Pakistani, Bangladeshi and European adults in a UK population. J Public Health Med. 2002;24(3):170–8.
Kanaya AM, Wassel CL, Mathur D, et al. Prevalence and correlates of diabetes in South Asian Indians in the United States: Findings from the Metabolic Syndrome and Atherosclerosis in South Asians Living in America Study and the Multi-Ethnic Study of Atherosclerosis. Metab Syndr Relat Disord. 2010;8(2):157–64.
Tillin T, Hughes AD, Mayet J, et al. The relationship between metabolic risk factors and incident cardiovascular disease in Europeans, South Asians, and African Caribbeans: SABRE (Southall and Brent revisited) – a prospective population-based study. J Am Coll Cardiol. 2013;61(17):1777–86.
Ethnicity and cardiovascular disease. The incidence of myocardial infarction in white, South Asian, and Afro-Caribbean patients with type 2 diabetes (U.K. Prospective Diabetes Study 32). Diabetes Care. 1998;21(8):1271-1277.
Kanaya AM, Adler N, Moffet HH, et al. Heterogeneity of diabetes outcomes among Asians and Pacific Islanders in the US: The Diabetes Study of Northern California (DISTANCE). Diabetes Care. 2011;34(4):930–7. This paper discusses ethnic differences in complications of diabetes in a large northern California population, focusing specifically on the large differences among different Asian American populations.
Forouhi NG, Sattar N, Tillin T, McKeigue PM, Chaturvedi N. Do known risk factors explain the higher coronary heart disease mortality in South Asian compared with European men? Prospective follow-up of the Southall and Brent studies, UK. Diabetologia. 2006;49(11):2580–8.
Wilkinson P, Sayer J, Laji K, et al. Comparison of case fatality in South Asian and white patients after acute myocardial infarction: Observational study. BMJ. 1996;312(7042):1330–3.
Nijjar AP, Wang H, Dasgupta K, Rabi DM, Quan H, Khan NA. Outcomes in a diabetic population of South Asians and whites following hospitalization for acute myocardial infarction: A retrospective cohort study. Cardiovasc Diabetol. 2010;9:4-2840-9-4.
Game FL, Jones AF. Ethnicity and risk factors for coronary heart disease in diabetes mellitus. Diabetes Obes Metab. 2000;2(2):91–7.
Barnett AH, Dixon AN, Bellary S, et al. Type 2 diabetes and cardiovascular risk in the UK South Asian community. Diabetologia. 2006;49(10):2234–46.
Deepa R, Mohan V, Premanand C, et al. Accelerated platelet activation in Asian Indians with diabetes and coronary artery disease–the Chennai Urban Population Study (CUPS-13). J Assoc Physicians India. 2006;54:704–8.
Bhaskar S, Ganesan M, Chandak GR, et al. Association of PON1 and APOA5 gene polymorphisms in a cohort of Indian patients having coronary artery disease with and without type 2 diabetes. Genet Test Mol Biomarkers. 2011;15(7–8):507–12.
Siezenga MA, Shaw PK, Daha MR, Rabelink TJ, Berger SP. Low mannose-binding lectin (MBL) genotype is associated with future cardiovascular events in type 2 diabetic South Asians. A prospective cohort study. Cardiovasc Diabetol. 2011;10:60-2840-10-60.
Narne P, Ponnaluri KC, Singh S, Siraj M, Ishaq M. Relationship between NADPH oxidase p22phox C242T, PARP-1 Val762Ala polymorphisms, angiographically verified coronary artery disease and myocardial infarction in South Indian patients with type 2 diabetes mellitus. Thromb Res. 2012;130(5):e259–65.
Gunarathne A, Patel JV, Gammon B, Gill PS, Hughes EA, Lip GY. Ischemic stroke in South Asians: A review of the epidemiology, pathophysiology, and ethnicity-related clinical features. Stroke. 2009;40(6):e415–23.
Moussouttas M, Aguilar L, Fuentes K, et al. Cerebrovascular disease among patients from the Indian subcontinent. Neurology. 2006;67(5):894–6.
Jafar TH. Blood pressure, diabetes, and increased dietary salt associated with stroke–results from a community-based study in Pakistan. J Hum Hypertens. 2006;20(1):83–5.
Deleu D, Hamad AA, Kamram S, El Siddig A, Al Hail H, Hamdy SM. Ethnic variations in risk factor profile, pattern and recurrence of non-cardioembolic ischemic stroke. Arch Med Res. 2006;37(5):655–62.
Gholap N, Davies M, Patel K, Sattar N, Khunti K. Type 2 diabetes and cardiovascular disease in South Asians. Prim Care Diabetes. 2011;5(1):45–56.
Gunarathne A, Patel JV, Potluri R, et al. Increased 5-year mortality in the migrant South Asian stroke patients with diabetes mellitus in the United Kingdom: The West Birmingham Stroke Project. Int J Clin Pract. 2008;62(2):197–201.
Gerstein HC, Anand S, Yi QL, et al. The relationship between dysglycemia and atherosclerosis in South Asian, Chinese, and European individuals in Canada: A randomly sampled cross-sectional study. Diabetes Care. 2003;26(1):144–9.
Venkataraman V, Amutha A, Anbalagan VP, et al. Association of glycated hemoglobin with carotid intimal medial thickness in Asian Indians with normal glucose tolerance. J Diabetes Complicat. 2012;26(6):526–30.
Chow CK, McQuillan B, Raju PK, et al. Greater adverse effects of cholesterol and diabetes on carotid intima-media thickness in South Asian Indians: Comparison of risk factor-IMT associations in two population-based surveys. Atherosclerosis. 2008;199(1):116–22.
Kelemen LE, Anand SS, Hegele RA, et al. Associations of plasma homocysteine and the methylenetetrahydrofolate reductase C677T polymorphism with carotid intima media thickness among South Asian, Chinese and European Canadians. Atherosclerosis. 2004;176(2):361–70.
Gunarathne A, Patel JV, Kausar S, Gammon B, Hughes EA, Lip GY. Glycemic status underlies increased arterial stiffness and impaired endothelial function in migrant South Asian stroke survivors compared to European Caucasians: Pathophysiological insights from The West Birmingham Stroke Project. Stroke. 2009;40(7):2298–306.
Kain K, Catto AJ, Grant PJ. Clustering of thrombotic factors with insulin resistance in South Asian patients with ischaemic stroke. Thromb Haemost. 2002;88(6):950–3.
Kain K, Brockway M, Ishfaq T, et al. Ankle pressures in UK South Asians with diabetes mellitus: A case control study. Heart. 2013;99(9):614–9.
Premalatha G, Shanthirani S, Deepa R, Markovitz J, Mohan V. Prevalence and risk factors of peripheral vascular disease in a selected South Indian population: The Chennai Urban Population Study. Diabetes Care. 2000;23(9):1295–300.
Bennett PC, Silverman S, Gill PS, Lip GY. Ethnicity and peripheral artery disease. QJM. 2009;102(1):3–16.
Chaturvedi N, Coady E, Mayet J, et al. Indian Asian men have less peripheral arterial disease than European men for equivalent levels of coronary disease. Atherosclerosis. 2007;193(1):204–12.
Chaturvedi N, Abbott CA, Whalley A, Widdows P, Leggetter SY, Boulton AJ. Risk of diabetes-related amputation in South Asians vs. Europeans in the UK. Diabet Med. 2002;19(2):99–104.
Abbott CA, Garrow AP, Carrington AL, et al. Foot ulcer risk is lower in South-Asian and African-Caribbean compared with European diabetic patients in the U.K.: The Northwest Diabetes Foot Care Study. Diabetes Care. 2005;28(8):1869–75.
Stolk RP, van Schooneveld MJ, Cruickshank JK, et al. Retinal vascular lesions in patients of Caucasian and Asian origin with type 2 diabetes: Baseline results from the ADVANCE retinal measurements (AdRem) study. Diabetes Care. 2008;31(4):708–13.
Sivaprasad S, Gupta B, Gulliford MC, et al. Ethnic variations in the prevalence of diabetic retinopathy in people with diabetes attending screening in the United Kingdom (DRIVE UK). PLoS One. 2012;7(3):e32182.
Pardhan S, Gilchrist J, Mahomed I. Impact of age and duration on sight-threatening retinopathy in South Asians and Caucasians attending a diabetic clinic. Eye (Lond). 2004;18(3):233–40.
Raymond NT, Varadhan L, Reynold DR, et al. Higher prevalence of retinopathy in diabetic patients of South Asian ethnicity compared with white Europeans in the community: A cross-sectional study. Diabetes Care. 2009;32(3):410–5.
Sivaprasad S, Gupta B, Gulliford MC, et al. Ethnic variation in the prevalence of visual impairment in people attending diabetic retinopathy screening in the United Kingdom (DRIVE UK). PLoS One. 2012;7(6):e39608.
Pradeepa R, Anitha B, Mohan V, Ganesan A, Rema M. Risk factors for diabetic retinopathy in a South Indian type 2 diabetic population–the Chennai Urban Rural Epidemiology Study (CURES) Eye Study 4. Diabet Med. 2008;25(5):536–42.
Uthra S, Raman R, Mukesh BN, et al. Diabetic retinopathy and IGF-1 gene polymorphic cytosine-adenine repeats in a Southern Indian cohort. Ophthalmic Res. 2007;39(5):294–9.
Uthra S, Raman R, Mukesh BN, et al. Intron 4 VNTR of endothelial nitric oxide synthase (eNOS) gene and diabetic retinopathy in type 2 patients in Southern India. Ophthalmic Genet. 2007;28(2):77–81.
Uthra S, Raman R, Mukesh BN, et al. Association of VEGF gene polymorphisms with diabetic retinopathy in a South Indian cohort. Ophthalmic Genet. 2008;29(1):11–5.
Uthra S, Raman R, Mukesh BN, et al. Diabetic retinopathy: Validation study of ALR2, RAGE, iNOS and TNFB gene variants in a South Indian cohort. Ophthalmic Genet. 2010;31(4):244–51.
Prasad P, Tiwari AK, Kumar KM, et al. Chronic renal insufficiency among Asian Indians with type 2 diabetes: I. Role of RAAS gene polymorphisms. BMC Med Genet. 2006;7:42.
Dixon AN, Raymond NT, Mughal S, et al. Prevalence of microalbuminuria and hypertension in South Asians and white Europeans with type 2 diabetes: A report from the United Kingdom Asian Diabetes Study (UKADS). Diab Vasc Dis Res. 2006;3(1):22–5.
Burden AC, McNally PG, Feehally J, Walls J. Increased incidence of end-stage renal failure secondary to diabetes mellitus in Asian ethnic groups in the United Kingdom. Diabet Med. 1992;9(7):641–5.
Karter AJ, Ferrara A, Liu JY, Moffet HH, Ackerson LM, Selby JV. Ethnic disparities in diabetic complications in an insured population. JAMA. 2002;287(19):2519–27.
Roderick PJ, Raleigh VS, Hallam L, Mallick NP. The need and demand for renal replacement therapy in ethnic minorities in England. J Epidemiol Community Health. 1996;50(3):334–9.
Mather HM, Chaturvedi N, Kehely AM. Comparison of prevalence and risk factors for microalbuminuria in South Asians and Europeans with type 2 diabetes mellitus. Diabet Med. 1998;15(8):672–7.
Dreyer G, Hull S, Aitken Z, Chesser A, Yaqoob MM. The effect of ethnicity on the prevalence of diabetes and associated chronic kidney disease. QJM. 2009;102(4):261–9.
Chandie Shaw PK, Baboe F, van Es LA, et al. South-Asian type 2 diabetic patients have higher incidence and faster progression of renal disease compared with Dutch-European diabetic patients. Diabetes Care. 2006;29(6):1383–5.
Chandie Shaw PK, Vandenbroucke JP, Tjandra YI, et al. Increased end-stage diabetic nephropathy in Indo-Asian immigrants living in the Netherlands. Diabetologia. 2002;45(3):337–41.
Shah VN, Cheema BS, Sharma R, et al. ACAC-β gene (rs2268388) and AGTR1 gene (rs5186) polymorphism and the risk of nephropathy in Asian Indian patients with type 2 diabetes. Mol Cell Biochem. 2013;372(1–2):191–8.
Prasad P, Tiwari AK, Kumar KM, et al. Association of TGF-β-1, TNF-α, CCR2 and CCR5 gene polymorphisms in type-2 diabetes and renal insufficiency among Asian Indians. BMC Med Genet. 2007;8:20.
Ahluwalia TS, Khullar M, Ahuja M, et al. Common variants of inflammatory cytokine genes are associated with risk of nephropathy in type 2 diabetes among Asian Indians. PLoS One. 2009;4(4):e5168.
Prasad P, Kumar KM, Ammini AC, Gupta A, Gupta R, Thelma BK. Association of dopaminergic pathway gene polymorphisms with chronic renal insufficiency among Asian Indians with type-2 diabetes. BMC Genet. 2008;9:26-2156-9-26.
Tiwari AK, Prasad P, B KT, et al. Oxidative stress pathway genes and chronic renal insufficiency in Asian Indians with type 2 diabetes. J Diabetes Complicat. 2009;23(2):102–11.
Prasad P, Tiwari AK, Kumar KM, et al. Association analysis of ADPRT1, AKR1B1, RAGE, GFPT2 and PAI-1 gene polymorphisms with chronic renal insufficiency among Asian Indians with type-2 diabetes. BMC Med Genet. 2010;11:52-2350-11-52.
Mooyaart AL, van Valkengoed IG, Shaw PK, et al. Lower frequency of the 5/5 homozygous CNDP1 genotype in South Asian Surinamese. Diabetes Res Clin Pract. 2009;85(3):272–8.
Ashok S, Ramu M, Deepa R, Mohan V. Prevalence of neuropathy in type 2 diabetic patients attending a diabetes centre in South India. J Assoc Physicians India. 2002;50:546–50.
Pradeepa R, Rema M, Vignesh J, Deepa M, Deepa R, Mohan V. Prevalence and risk factors for diabetic neuropathy in an urban South Indian population: The Chennai Urban Rural Epidemiology Study (CURES-55). Diabet Med. 2008;25(4):407–12.
UK Prospective Diabetes Study. XII: Differences between Asian, Afro-Caribbean and white Caucasian type 2 diabetic patients at diagnosis of diabetes. UK Prospective Diabetes Study group. Diabet Med. 1994;11(7):670-677.
Abbott CA, Chaturvedi N, Malik RA, et al. Explanations for the lower rates of diabetic neuropathy in Indian Asians versus Europeans. Diabetes Care. 2010;33(6):1325–30.
Abbott CA, Malik RA, van Ross ER, Kulkarni J, Boulton AJ. Prevalence and characteristics of painful diabetic neuropathy in a large community-based diabetic population in the U.K. Diabetes Care. 2011;34(10):2220–4.
Gujral JS, McNally PG, O'Malley BP, Burden AC. Ethnic differences in the incidence of lower extremity amputation secondary to diabetes mellitus. Diabet Med. 1993;10(3):271–4.
http://www.diabetes.org/diabetes-basics/prevention/diabetes-risk-test/.
Lindstrom J, Tuomilehto J. The diabetes risk score: A practical tool to predict type 2 diabetes risk. Diabetes Care. 2003;26(3):725–31.
Mohan V, Anbalagan VP. Expanding role of the Madras Diabetes Research Foundation - Indian Diabetes Risk Score in clinical practice. Indian J Endocrinol Metab. 2013;17(1):31–6. This paper discusses the role of a diabetes risk score that was developed and validated in a South Asian population and reviews it myriad applications.
Joshi SR. Indian diabetes risk score. J Assoc Physicians India. 2005;53:755–7.
Ramachandran A, Snehalatha C, Mary S, et al. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006;49(2):289–97.
Snehalatha C, Mary S, Selvam S, et al. Changes in insulin secretion and insulin sensitivity in relation to the glycemic outcomes in subjects with impaired glucose tolerance in the Indian Diabetes Prevention Programme-1 (IDPP-1). Diabetes Care. 2009;32(10):1796–801.
Ramachandran A, Snehalatha C, Mary S, et al. Pioglitazone does not enhance the effectiveness of lifestyle modification in preventing conversion of impaired glucose tolerance to diabetes in asian indians: Results of the Indian Diabetes Prevention Programme-2 (IDPP-2). Diabetologia. 2009;52(6):1019–26.
DREAM (Diabetes REduction Assessment with ramipril and rosiglitazone Medication) Trial Investigators, Gerstein HC, Yusuf S, et al. Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trial. Lancet. 2006;368(9541):1096–105.
Bellary S, O'Hare JP, Raymond NT, et al. Enhanced diabetes care to patients of South Asian ethnic origin (The United Kingdom Asian Diabetes Study): A cluster randomised controlled trial. Lancet. 2008;371(9626):1769–76.
Narayan V. National Institutes of Health. A randomized trial of diabetes prevention through lifestyles changes in India (D-CLIP). http://clinicaltrials.gov/ct2/show/NCT01283308. Updated 30 March 2012.
Douglas A, Bhopal RS, Bhopal R, et al. Design and baseline characteristics of the PODOSA (Prevention of Diabetes & Obesity in South Asians) trial: A cluster, randomised lifestyle intervention in Indian and Pakistani adults with impaired glycaemia at high risk of developing type 2 diabetes. BMJ Open. 2013;3(2):e002226. doi:10.1136/bmjopen-2012-002226.
Narayan V. National Institutes of Health. A Culturally tailored lifestyle intervention to prevent diabetes in South Asians (SHAPE). http://clinicaltrials.gov/ct2/show/NCT01084928. Updated 30 March 2012.
Compliance with Ethics Guidelines
Conflict of Interest
Arti Shah and Alka M. Kanaya declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Diabetes and Cardiovascular Disease
Rights and permissions
About this article
Cite this article
Shah, A., Kanaya, A.M. Diabetes and Associated Complications in the South Asian Population. Curr Cardiol Rep 16, 476 (2014). https://doi.org/10.1007/s11886-014-0476-5
Published:
DOI: https://doi.org/10.1007/s11886-014-0476-5