Abstract
“To go too far is as bad as to fall short.”Confucius (BC 551-BC 479) Chinese philosopher
Echocardiography has contributed most to our current understanding and indeed our current dilemma regarding the heart of the endurance athlete. Echocardiography assesses and characterizes nicely the effects of Endurance exercise training. It allows us to assess both systolic and diastolic cardiac variables as they change with structure and function associated with intense sporting activity. Much research work using echocardiography has characterized the left and right ventricle of the endurance athlete over the last year. Indeed evidence suggests that intense prolonged exercise may result in myocardial dysfunction which predominantly affects the RV, and that chronic RV remodelling may represent a substrate for ventricular arrhythmias in athletes. This has been the source of many debates and articles over the last 12 months. The reasons underlying the predilection towards RV dysfunction with intense prolonged exercise and the variation between individuals in its occurrence are still under dispute. This article seeks to describe the recent literature over the last year which outlines the different areas research has focused on when we assess the heart of the endurance athletes using echocardiography. Ultimately the goal of all research on the heart of the endurance athletes is to search for the holy grail of when enough is enough and therefore recognize and embrace the delicate balance of endurance intensity, in other words the border line when endurance exercise is no longer beneficial but slumps and slides into the realms of induced cardiac pathology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction: Endurance Athletes and Echocardiography
While many of the unique clinical and physiologic features present in endurance athletes have been described by astute observers for many years, echocardiography has revolutionized the understanding of the anatomy and physiology of the athletic heart. Echocardiography provides a window to the adaptive changes in cardiac size and function that occur in tandem with athletic training and also helps distinguish physiologic from pathologic adaptation. In this manuscript, the authors describe some of the key insights into the athlete’s heart.
The elite endurance athlete invariably suggests someone of excellent health and well-being. Sudden death therefore in athletes provides the greatest catastrophe in sport because of its unexpectedness. Identifying those athletes at risk remains a great challenge because the athlete’s heart undergoes adaptive changes in response to regular physical exercise that can mask some abnormal characteristics. The human heart is adept in changing its mass by at least 100 % with increases or decreases in load [1]. This has been well demonstrated with changes in cardiac morphology associated with chronic or intermittent loading situations. It is a fact that remodelling is a direct response to allow for the enhancement of cardiac performance and to compensate for the intermittent increases in wall stress caused by strenuous exercise. The overall physical adaptations to the human heart muscle of the athlete have been a source of captivation for all of us in cardiac research from the student to the far-reaching scientist. It is often therefore difficult to distinguish physiological adaptations from path physiological processes. Problems with routine widespread screening of athletes include the limitations inherent in the analytical value of available diagnostic procedures and the cost of testing large populations. Therefore broad methods are presently employed to help guide the athletic population through the medical riddle of left ventricular hypertrophy (physiological) or left ventricular hypertrophy (path physiological). Awareness of this issue, as well as the corresponding consideration of athletic screening before training, has been heightened by a number of recent high-profile cases of elite basketball and football players who died suddenly and unexpectedly from suspected cardiovascular disease. Added to our scientific dilemma is the “hype” out there in the broad community. A recent example of “hype” were headlines from an article appearing in the Wall Street Journal (WSJ), entitled "One Running Shoe in the Grave." The article by Kevin Helliker comments on an editorial by James O'Keefe, MD, entitled, "Run for your life at a comfortable speed and not too far" that was published in the British Heart Journal [2••].
However numerous large observational and cohort studies have subsequently confirmed the graded benefit of exercise on cardiovascular health and mortality [3–6]. The question from the last year of research using echocardiography and its modalities into investigations of the athletic heart is where to stop with endurance. Also what are the criteria if any we have for recognizing where the benefit of high intensity sport and duration stops? Are the American Heart Association consensus guidelines for physical activity with its cautions about high intensity sport enough [7]. Where and at what point of cardiovascular endurance can we recognize scientifically that exercise is no longer beneficial but in fact, slides into the realms of induced pathology? This discussion is, indeed highly controversial? How can echocardiography help going forward?
As we know over the many decades following the invention of echocardiography this technique has contributed most to our current understanding of cardiac morphology in athletes and is likely to remain critical to assessment given its low cost, widespread availability and lack of ionizing radiation. Echocardiography uses ultrasound waves in the megahertz range (typically 1.0 to 30 MHz) to assess cardiac structure and function. Structural imaging uses M-mode, 2-dimensional and 3-dimensional datasets to generate images of the heart derived from reflected ultrasound energy. M-mode imaging provides extremely high temporal and spatial resolution but in only a single dimension whilst 2-D imaging enables a more comprehensive evaluation by enabling simultaneous assessment of cardiac motion and structure. 3-D echocardiography is still advancing and has significant theoretical advantages in that it represents true geometry and movement rather than relying on multiple non-simultaneous planes and geometric assumptions in their integration. However, there are trade-offs in temporal and spatial resolution as well as some increased complexity in image acquisition. As we know blood velocity and myocardial tissue velocities derived from Doppler echocardiography and deformation imaging is the study of the degree to which muscle thickens and lengthens. This can be described in the extent to which this occurs relative to the resting muscle length, called strain (ε) and the rate at which strain changes (strain rate). Two dimensional strain images can also be used to evaluate left ventricular torsion-parameters that describe the wringing or twisting of the base and apex of the heart relative to one another.
Advancement of echocardiographic imaging techniques, many of which now provide highly sophisticated and detailed anatomic data, coupled with the availability of smaller, portable echocardiographic equipment has greatly expanded the imaging of the athlete’s heart. In addition to providing high quality resting images, the increased portability of imaging now allows the further study of athletes at the site of competition [8, 9].
The Left Ventricle of the Endurance Athlete
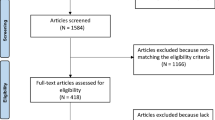
Given the recent interest in reducing the risk of sudden cardiac death, there is great emphasis on the early detection of cardiac abnormalities in modern elite athletes. Prolonged intense training is characterized by left ventricular hypertrophy (LVH) and chamber dilatation, so it is important to distinguish physiological changes from pathological abnormalities. Doppler echocardiographic tissue indices may be useful in this regard as shown by King et al. [10]. Elite rowers showed an increase in LVEDD, with a modest parallel increase in septal and posterior wall thickness. At this level of exercise the end-diastolic and end systolic volumes increase in parallel, increasing the stroke volume, and so the EF remained the same [7]. While left ventricular ejection fraction by echocardiography is a traditional parameter of systolic function, subtle acute changes may be more difficult to discern. Left ventricular myocardial strain and torsion may offer further insights into subtle changes in systolic function. Following exposure to a bout of high intensity exercise, left ventricular function as assessed by torsion was demonstrated to augment significantly in a group of elite masters rowers [11]. Baggish and colleagues in a longitudinal study examined changes in clinical and echocardiographic parameters following a three month period of regular endurance training in a group of collegiate rowers. While there was no significant change in the overall LVEF in the athletes, all other measures of systolic function including mitral annular systolic velocities, radial and circumferential strain. Interestingly, changes in LV septal circumferential strain decreased and this change was associated with a corresponding increase in the RV diameter, thus demonstrating an interaction between the left and right ventricle (Fig. 1) [12].
Correlation between changes in left ventricular septal circumferential strain and right ventricular end-diastolic area and peak systolic tissue velocity after 90 days of endurance exercise training. (From: Baggish AL, Yared K, Wang F, Weiner RB, Hutter AM Jr, Picard MH, Wood MJ. The impact of endurance exercise training on left ventricular systolic mechanics. Am J Physiol Heart Circ Physiol. 2008 Sep; 295(3):H1109-H1116) [12]
Body size, sporting discipline and ethnicity have an independent impact on LV remodelling. With regard to ethnicity, current research in May 2012 [13••] using echocardiography showed that African athletes show a different pattern of LV remodelling compared with Caucasians, characterized by a greater increase in LV wall thicknesses, mass, and relative wall thickness but similar cavity size. This “disproportionate” wall thickening suggests that undefined determinants associated with black race may amplify the physiological wall thickening in response to volume overload associated with chronic exercise. With regard to overall remodelling a further study in 2012 using advanced echocardiographic techniques showed systematically smaller atria and ventricular dimensions and volumes, and larger wall thickness and mass, when echocardiography was compared to cardiac MRI. The authors suggested that modification of the echocardiographic formulas used could facilitate better inter technique comparability [14•]. These findings should be taken into account in the interpretation of cardiac MRI findings in athletic subjects in whom hypertrophic cardiomyopathy is suspected on echocardiography.
Left ventricular diastolic function has been well studied and characterized using echocardiographic techniques including transmitral and pulmonary pulsed wave Doppler tissue Doppler and diastolic strain and strain rate imaging. Cross sectional studies have demonstrated enhanced diastolic function in well trained endurance athletes. This functional adaptation leads to increased cardiac efficiency. A longitudinal study of diastolic function in strength and endurance athletes demonstrated further enhancement in diastolic function with endurance training while strength athletes demonstrated diminution in diastolic function [15].
Further studies using strain and strain rate deformation technology looked at the function of the left atrium of the endurance athlete’s heart and compared it to the non-athletic heart. The findings concluded that LA myocardial deformation is significantly impaired in patients with HCM compared to athletes and healthy controls. LA strain and strain rate assessed by 2D speckle tracking should be incorporated in the evaluation of trained athletes with LVH and LA dilatation [16].
Endurance exercise inflicts increased hemodynamic demands that alter the loading conditions of the heart, particularly among athletes participating in sports requiring sustained elevations in cardiac work, such as long-distance running, rowing, swimming, and cycling [17]. As discussed high endurance training on an athlete causes development of cardiac adaptations including enlarged LV and RV volumes, increased LV wall thickness and cardiac mass, and increased left atrial size. All of these parameters are easily measured by echocardiography [18–20], These alterations, together with a preserved LV ejection fraction as demonstrated in the study of elite rowers, have been considered typical findings of the “athlete’s heart”[7, 18]. However it has been suggested that some of the changes that occur in endurance athletes may not be entirely normal [11, 21–23]. In a study by Pelliccia et al., left ventricular remodelling was evident after long-term detraining, with significant reduction in cavity size and normalization of wall thickness. However, the return of cavity dimension was incomplete, and substantial chamber dilatation persisted in >20 % of athletes. This may have future long-term clinical implications in some individuals [24].
The Right Ventricle of the Endurance Athlete
There is without doubt compelling evidence for the cardiovascular benefits of regular physical exercise and recent studies have shown that transient right ventricular myocardial damage may occur during intense training regimes and prolonged exercise, especially in amateur participants. The Heidbuchel group (2003) at the University of Leuven in Belgium demonstrated that mild RV dysfunction was common amongst athletes with complex ventricular arrhythmias and a significant number resulted in sudden death. Heidbuchel coined the term “exercised induced right ventricular cardiomyopathy” and subsequently demonstrated that endurance athletes with ventricular arrhythmias had a lower RV ejection fraction as determined by the gold standard of ventriculography than athletes without ventricular arrhythmias [25].
We have known for years that habitual endurance exercise results in structural and functional cardiac changes which are termed “athlete’s heart syndrome”. We know that all chambers of the heart undergo remodelling which is believed to represent an adaptive response providing the means for enhanced cardiovascular performance during exercise. However the differentiation between long term loading-induced RV remodelling and reduced RV contractility may have important therapeutic and prognostic implications for the elite athlete. Recently a syndrome has been reported whereby the right ventricle in some high end endurance elite athletes undergoes structural and electrical remodelling which may create substrate arrhythmias including life threatening arrhythmias.
Latest research shows that the lower resting values of right ventricular (RV) myocardial % strain may represent a physiologic change rather than subclinical myocardial damage. Therefore, load independent changes to the RV as a consequence of high intensity training were made by measuring the isovolumic acceleration (IVA) of the free wall of the RV in conjunction with NT pro-BNP measured by an electrochemiluminescence assay. In this study by King et al. [26], it was demonstrated that right ventricular sub-clinical changes do occur after training in elite endurance rowers. Reduced global % strain, was more prevalent in the elite endurance athlete than in the semi-professional footballers or controls and may reflect ventricular loading and geometry rather than underlying myocardial properties. There was also an increase in isovolumic acceleration of the free wall of the right ventricle in the elite endurance rower. It was therefore hypothesize that reductions in IVA may be a more robust indicator of myocardial pathology, although this remains to be tested.
Gender Differences in Cardiovascular Remodelling in Athletes
Cardiovascular adaptations to exercise vary not only with type of exercise but also with gender. Male and female athletes who undergo chronic exposure to exercise training exhibit augmentation of stroke volume through multiple mechanisms including enlargement of the cardiac chambers and enhanced diastolic filling of the left ventricle. As previously described, endurance/isotonic exercise typically leads to greater increases in cavity dimensions and lower relative wall thickness (interventricular septum + posterior wall thickness/LV diastolic cavity dimension) compared to strength/isometric exercise. A great deal of overlap between strength and endurance training exists between many sporting disciplines and the degree to which these changes are manifest may depend on gender and body habitus.
Female athletes traditionally exhibit less robust physiologic remodelling than do their male counterparts. While this may reflect the sporting discipline (fewer women participate in sports known to be associated with substantial physiologic remodelling including rowing and football), gender based differences may also affect the cardiac response to regular exercise.
Pellicia and colleagues [27] performed a cross-sectional analysis of LV dimensions and wall thickness in a cohort of 600 female athletes from 27 different sporting disciplines and compared them to a group of similar aged sedentary controls. The athletes exhibited a greater degree of LV cavity dilation and greater wall thicknesses than the sedentary controls. The majority of female athletes demonstrated LV wall thicknesses from 7–9 mm (mean (8.2 +/− 0.9 mm vs. 7.2 +/− 0.6 mm in controls; P < .001) with wall thicknesses varying from 6–12 mm. The female athletes demonstrated increased LV end-diastolic cavity dimensions compared with sedentary controls. Left ventricular cavity dimension varied from 40 mm to 66 mm in the athletes (49 +/− 4 mm in athletes vs 46 +/− 3 mm in controls P < 0.001) and exceeded normal limits ( > 54 mm) in 47 women (8 %). Only four athletes (1 %) were found to have LV cavity dimensions large enough to be suggestive of a dilated cardiomyopathy (> 60 mm). The greatest degree of LV dilation was observed in female athletes who participated in endurance sports including cross country skiing, rowing and cycling.
Pelliccia and colleagues further examined gender differences in cardiac remodelling in 1309 athletes from 38 distinct sporting disciplines [18]. Wide variation in the LV end-diastolic cavity dimensions (varying from 38 to 66 mm (mean 48 mm)) was observed in women. Larger diastolic dimensions were observed in men (ranging from 43 to 70 mm (mean 55 mm)). LV diastolic dimension was greatest in male athletes and those with the greatest body mass. As has previously been demonstrated by others, smaller LV mass was demonstrated in athletic and sedentary females compared to males.
As demonstrated in male athletes, racial differences in cardiovascular remodelling have also been observed in female athletes. Rawlins and colleagues described electrocardiographic and echocardiographic features in 440 black and white female athletes [28•]. Black women demonstrated significantly increased left ventricular wall thickness and mass compared to the white women (wall thicknesses of 9.2+/−1.2 mm and mass of 187.2+/−42 g in black athletes versus 8.6+/−1.2 mm and 172.3+/−42 g in the white athletes).
Conclusion
Our understanding of the athlete’s heart has progressed considerably since its first description by Henschen [29] and Darling in 1899 [30]. Body size, gender, sporting discipline and ethnicity have an independent impact on overall cardiac remodelling and physiology. Although there is no data that vigorous long-term endurance training and competition leads to LV dysfunction, there is evidence for exercise induced atrial and RV arrhythmogenic remodelling. Atrial remodelling is more pronounced in male athletes. Several physiologic and clinical questions remain. The relationship between intensity, frequency, duration, and type of sports and cardiac remodelling has to be defined more clearly in longitudinal studies. Most importantly, the question of whether high intensity endurance sport may act as an advocate (and not only as a trigger) of cardiac dysfunction and arrhythmias has to be clarified. Sophisticated diagnostic imaging allied with echocardiography and all of its modalities have to be deployed to help answer this question. The availability and portability of sophisticated echocardiographic imaging have also further advanced the understanding of the athletic heart.
A paradox exists now whereby we spent years seeing an increase in morbidity associated with a lack of habitual exercise and the consequences being assessed by echocardiography. Now we have a simultaneous increase in the number of people performing exercise far in excess of recommendations. This group is also being assessed by echocardiography in the quest of the Holy Grail or “magic number” which would apply a limit on helpful doses of exercise. We hope with further advances in echocardiography and all its new modalities that this technique now in its 60th year can be seen as a diagnostic tool with a penchant to protect the high end endurance athletes’ myocardium from going too far.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hill JA, Olson EN. Cardiac plasticity. N Engl J Med. 2008;358(13):1370–80.
•• O Keefe J, Levie C. Run for your life … at a comfortable speed and not too far. Heart doi: 10.1136/heartjnl-2012-302886. This highly controversial manuscript describes the potential detrimental effects of prolonged endurance exercise on the health of athletes.
Barengo NC, Hu G, Lakka TA, Pekkarinen H, Nissinen A, Tuomilehto J. Low physical activity as a predictor for total and cardiovascular disease mortality in middle-aged men and women in Finland. Eur Heart J. 2004;25(24):2204–11.
Lee IM, Skerrett PJ. Physical activity and all-cause mortality: what is the dose–response relation? Med Sci Sports Exerc. 2001;33(6 Suppl):S459–71. discussion S493-454.
Manson JE, Greenland P, LaCroix AZ, Stefanick ML, Mouton CP, Oberman A, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347(10):716–72.
Sesso HD, Paffenbarger Jr RS, Lee IM. Physical activity and coronary heart disease in men: the Harvard alumni health study. Circulation. 2000;102(9):975–80.
Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the AmericanCollege of Sports Medicine and the American HeartAssociation. Circulation. 2007;116(9):1081–93.
Neilan TG, Tono-Nu TT, Jassal DS, et al. Myocardial adaptation to short-term high-intensity exercise in highly trained athletes. J Am Soc Echocardiogr. 2006;19(10):1280–5.
Poh KK, Tournoux FB, Ton-Nu TT, Picard MH, Wood MJ. Myocardial adaptation and efficiency in response to intensive physical training in elite speedskaters. Int J Cardiol. 2007;126(3):346–51.
King G, Murphy R, Almuntaser I, Bennett K, Ho E, Brown S. Alterations in myocardial stiffness in elite athletes assessed by a new Doppler index. Heart Br Cardiac Soc. 2008;94(10):1323–5.
Neilan TG, Januzzi JL, Lee-Lewandrowski E, et al. Myocardial injury and ventricular dysfunction related to training levels among non elite participants in the Boston marathon. Circulation. 2006;114(22):2325–33.
Baggish AL, Yared K, Wang F, Weiner RB, Hutter Jr AM, Picard MH, et al. The impact of endurance exercise training on left ventricular systolic mechanics. Am J Physiol Heart Circ Physiol. 2008;295(3):H1109–16.
•• Di Paolo FM, Schmied C, Zerguini YA, Junge A, Quattrini F, Culasso F, et al. The athlete's heart in adolescent Africans an electrocardiographic and echocardiographic study. J Am Coll Cardiol. 2012;59(11):1029–36. This study describes unique electrocardiographic and echocardiographic findings in young African athletes.
• Prakkem NHJ, Teske AJ, Cramer MJ, Mosterd A, Bosker AC, Mali WP, et al. Head-to-head comparison between echocardiography and cardiac mri in the evaluation of the athlete' heart. Br J Sports Med. 2012;46(5):348–54. This study compares differences in quantification of left ventricular size and wall thickness in athletes and suggests correction of echocardiographic formulas to allow for better intertechnique evaluation of cardiac function.
Baggish AL, Wang F, Weiner RB, et al. Training-specific changes in cardiac structure and function: a prospective and longitudinal assessment of competitive athletes. J Appl Physiol. 2008;104:1121–8.
Gabrielli L, Enríquez A, Córdova S, Yáñez F, Godoy I, Corbalán R. Assessment of left atrial function in hypertrophic cardiomyopathy and athlete's heart: a left atrial myocardial deformation study. Echocardiography. 2012;29(8):943–9.
Middleton N, Shave R, George K, et al. Altered left ventriculardiastolic filling following a marathon is a reproducible phenomenon. Int J Cardiol. 2007;122(1):87–9.
Pelliccia A, Culasso F, Di Paolo FM, Maron BJ. Physiologic leftventricular cavity dilatation in elite athletes. Ann Intern Med. 1999;130(1):23–31.
Pelliccia A, Maron BJ, Di Paolo FM, et al. Prevalence and clinicalsignificance of left atrial remodelling in competitive athletes. J Am Coll Cardiol. 2005;46(4):690–6.
Pelliccia A, Maron BJ, Spataro A, Proschan MA, Spirito P. Theupper limit of physiologic cardiac hypertrophy in highly trainedelite athletes. N Engl J Med. 1991;324(5):295–301.
Pluim BM, Zwinderman AH, van der Laarse A, van der Wall EE. The athlete’s heart: a meta-analysis of cardiac structure and function. Circulation. 2000;101(3):336–44.
Maron BJ, Pelliccia A. The heart of trained athletes: cardiacremodelling and the risks of sports, including sudden death. Circulation. 2006;114(15):1633–44.
Spirito P, Pelliccia A, Proschan MA, et al. Morphology of the” athlete’s heart” assessed by echocardiography in 947 elite athletes representing 27 sports. Am J Cardiol. 1994;74(8):802–6.
Pelliccia A, Maron BJ, De Luca R, Di Paolo FM, Spataro A, Culasso F. Remodelling of left ventricular hypertrophy in elite athletes after long-term deconditioning. Circulation. 2002;105(8):944–9.
Heidbüchel H, Hoogsteen J, Fagard R, et al. High prevalence of right ventricular involvement in endurance athletes with ventricular arrhythmias. Role of an electrophysiologic study in risk stratification. Eur Heart J. 2003;16:1473–80.
King G, Murphy R, Almuntaser I, Clarke J, Brown SG. Reduced right ventricular myocardial strain in the elite athlete may not be a consequence of myocardial damage, “Cream Masquerades as Skimmed Milk”. Echocardiography. 2013. doi:10.1111/echo.12153.
Pelliccia A, Maron BJ, Culasso F, Spataro A, Caselli G. Athlete’s heart in women. Echocardiographic characterization of highly trained elite female athletes. JAMA. 1996;276(3):211–5.
• Rawlins J, Carre F, Kervio G, Papadakis M, Chandra N, Edwards C, et al. Ethnic differences in physiological cardiac adaptation to intense physical exercise in highly trained female athletes. Circulation. 2010;121(9):1078–85. This paper compares echocardiographic and electrocardiographic features and discusses differences between and white female athletes.
Henschen S. Skidlauf und skidwettlauf: eine medizinische sportstudie. Mitt Med Klin Upsala. 1899;2.
Darling EA. The effects of training: a study of the Harvard University crews. Boston Med Surg J. 1899;161:229–33.
Compliance with Ethics Guidelines
Conflict of Interest
Gerard King and Malissa J. Wood declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Echocardiography
Rights and permissions
About this article
Cite this article
King, G., Wood, M.J. The Heart of the Endurance Athlete Assessed by Echocardiography and Its Modalities: “Embracing the Delicate Balance”. Curr Cardiol Rep 15, 383 (2013). https://doi.org/10.1007/s11886-013-0383-1
Published:
DOI: https://doi.org/10.1007/s11886-013-0383-1