Abstract
Aortic stenosis affects a significant number of patients worldwide, and carries a dismal prognosis once symptoms develop. Unfortunately, a large number of patients present a prohibitive risk for surgical aortic valve replacement. Therefore, transcatheter aortic valve implantation has emerged as a promising technology for providing treatment to this group of patients. Currently available valves include the balloon-expandable Edwards SAPIEN valve (Edwards Lifesciences, Irvine, CA), which is usually implanted via a transfemoral or transapical approach, and the self-expanding CoreValve ReValving system (Medtronic, Minneapolis, MN), which uses only the transfemoral route. Early experience with the procedure performed on a compassionate-use basis was encouraging, and led to a number of first-in-man and feasibility studies. These trials demonstrated the safety and efficacy of valve implantation and led to CE (European Conformity) mark approval of both valves in Europe. Use of the SAPIEN valve in the United States is limited to the recently completed PARTNER (Placement of Aortic Transcatheter Valve) randomized trial comparing transcatheter and surgical aortic valve replacement in high-risk patients, and its post-trial registry. The CoreValve is not yet available in the United States. With improved device technology, better understanding of patient selection and pre- and periprocedural imaging, and greater procedural experience, widespread diffusion of transcatheter aortic valve implantation is expected.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As life expectancy has increased, so too has the incidence of aortic stenosis (AS), with a prevalence of almost 5% in patients over the age of 75 years [1].The development of symptoms with severe AS predicts death in greater than 50% of patients within 2 years [2]. Aortic valve replacement (AVR) reduces symptoms and prolongs life, but more than one third of patients may be denied surgery due to advanced age, significant left ventricular dysfunction, previous chest surgery or radiation, or other comorbidities [3, 4]. Traditionally, these patients’ options were limited to medical therapy or balloon valvuloplasty, both of which are ineffective in prolonging survival in most patients with symptomatic AS [5]. Percutaneous approaches to AVR have heralded a new era in the treatment of degenerative AS. In this paper, we review the major aspects of patient selection and imaging for transcatheter aortic valve implantation (TAVI), outline the procedure and potential complications, and revisit the clinical trials that have been reported thus far.
Patient Selection
In Europe, both the Edwards SAPIEN valve (Edwards Lifesciences, Irvine, CA) and the CoreValve ReValving System (Medtronic, Minneapolis, MN) may be used when clinically appropriate under the CE (European Conformity) mark, based on the clinical trials detailed below. Since approval, more than 2500 procedures have been performed with each device. The inclusion and exclusion criteria for use, as outlined by the European Association of Cardio-Thoracic Surgery and the European Society of Cardiology, are detailed in Table 1. In the United States, transcatheter approaches to the treatment of severe AS are currently reserved for patients enrolled in the randomized PARTNER US clinical trial, with inclusion and exclusion criteria similar to those used in previous studies (Table 2).
Screening patients for TAVI is best accomplished using a multidisciplinary approach that consists of cardiologists, cardiothoracic surgeons, and specialists in cardiovascular imaging. Initial evaluation requires a thorough clinical evaluation and assessment of comorbidities. Formal evaluation of surgical risk using published calculators should also be undertaken. However, investigators have demonstrated a significant overestimation of predicted mortality by both the additive and logistic versions of the European System for Cardiac Risk Operative Score (EuroSCORE) in patients undergoing isolated surgical AVR [6]. This issue is especially germane to those evaluating patients for TAVI on the basis of prohibitive operative risk.
In contrast, the Society of Thoracic Surgeons Predicted Risk of Mortality (STS-PROM) is a more contemporary model derived from a group of patients undergoing valvular and nonvalvular OHS. Comparisons of the EuroSCORE and STS-PROM in patients undergoing isolated surgical AVR have shown that the latter more accurately predicts operative mortality. All calculators, however, consistently overestimate the mortality of isolated surgical AVR, emphasizing the need for new risk calculators as well as thoughtful decision making regarding patient selection for TAVI. Additionally, a large number of patients in contemporary trials of TAVI suffer mid- and long-term mortality as a result of noncardiac causes, further highlighting the importance of assessing comorbid conditions and appropriate patient selection [7].
Finally, comprehensive imaging is imperative, and consists of CT scan of the aorta and pelvic vasculature, transthoracic (and if needed transesophageal) echocardiography, coronary angiography with ascending and pelvic aortography, as well as lower extremity arterial ultrasound mapping at the discretion of the operator. These studies are required to assess a patient’s anatomic candidacy for safe device manipulation and successful valve implantation.
Role of Imaging
Along with improvements in procedural technique and skill, the use of various imaging modalities has improved the success of transcatheter therapies.
Echocardiography
Transthoracic echocardiography (TTE) remains the mainstay for the initial diagnosis of AS severity. It allows the identification of valve morphology (ie, bicuspid vs tricuspid), measurement of annulus size, degree of aortic regurgitation (AR), and assessment of left ventricular systolic function; all are integral components in evaluating the feasibility of TAVI.
Prior to the procedure, transesophageal echocardiography (TEE) may also be used for preimplantation measurements of the aortic annulus and left ventricular outflow tract (LVOT) for more precise valve sizing if TTE is inadequate. Additionally, aortic and mitral valve calcifications may be used as landmarks for device positioning. Deployment is traditionally performed under fluoroscopy. Many operators also use adjunctive TEE guidance for immediate assessment of post-deployment outcome. This is especially important in the prompt diagnosis of serious complications such as severe AR, coronary ostium impingement, pericardial effusion and cardiac tamponade, or interference with the mitral valve apparatus. Acoustic shadowing due to the valve prosthesis or cardiac calcium can make echocardiographic localization difficult, in which case operators must rely on fluoroscopic guidance.
Computed Tomography
Although TEE is considered the method of choice for making TAVI-related decisions, experience with multidetector computed tomography (MDCT) is increasing. MDCT allows detailed evaluation of the aortic valve, adjacent structures (ie, the coronary arteries), calcification, and the geometry of the ascending aorta and aortic valve in relation to the LVOT, all of which have implications for device placement and success [8–10]. Few studies have compared the three imaging modalities (TTE, TEE, and MDCT). Recently, Messika-Zeitoun et al. [11] demonstrated that the use of MDCT, although anatomically helpful, would have resulted in a significant number of patients being denied TAVI (who had undergone successful implantation using TEE guidance). This implies that information from all three modalities be used together rather than in isolation.
In addition to ileofemoral angiography, CT is used in assessing the pelvic and lower extremity anatomy prior to TAVI. Many patients with AS also have significant peripheral arterial disease, which predicts complicated vascular access and may affect the procedural approach (ie, transfemoral [TF] vs transapical [TA] implantation). Therefore, comprehensive contrast-enhanced CT aortography to mid-thigh is routinely performed to assess the following considerations for TAVI: significant aortic arch atheroma or porcelain aorta, minimal luminal diameter of the common iliac, external iliac, or common femoral artery of less than 8 mm, greater than 60% circumferential calcification at the external/internal iliac bifurcation, and significant common/external iliac angulation (< 90o). Although none of these factors are an absolute contraindication to TF TAVI, they must be considered with regard to risk of stroke, equipment manipulation, and size of sheath system required for the procedure. Investigators have demonstrated the use of direct aortic contrast injection (15–20 mL) with CT acquisition to abrogate the risk of contrast nephropathy, although this has not gained widespread use [12].
Fluoroscopy
Fluoroscopic imaging is the cornerstone of the catheterization laboratory. Sheath insertion and advancement of all wires and equipment are accomplished under fluoroscopic guidance. Biplane imaging minimizes dye load and procedural time in TAVI cases. Fluoroscopy is used to evaluate the relationship between the ascending aorta and the LVOT, and assess calcifications in the aorta, aortic valve, and mitral annulus. Small contrast injections in the aortic root may be helpful to properly delineate the anatomy of interest. To correctly visualize the aortic valve plane to facilitate device positioning, proper positioning of the x-ray beam is essential. During balloon inflation for valvuloplasty, motion of the balloon should be assessed fluoroscopically, and contrast injection in the left sinus via a pigtail catheter may be helpful to provide assurance that the left main coronary artery is unobstructed.
Valves and Their Implantation
TAVI is performed using one of two valves: the Edwards SAPIEN valve or the CoreValve ReValving System (Fig. 1) [13]. The Edwards SAPIEN valve and its predecessors have been used in the United States in various clinic trials; the CoreValve system is awaiting clinical trials in the United States and is not yet available in this country. Both are used in Europe under the CE mark.
Overview of transcatheter aortic valve implantation. Percutaneous aortic valve replacement is done via a retrograde, antegrade, or transapical approach. Each has its challenges. In all three approaches, the positioning of the prosthetic valve is determined by the patient’s native valvular structure and anatomy and is guided by fluoroscopic imaging, supra-aortic angiography, and transesophageal echocardiography. Current prosthetic valves are made from equine or bovine pericardial tissue. The insets at the bottom show the position of the aortic valve prosthesis; it is placed at mid-position in the patient’s aortic valve so as not to impinge on the coronary ostia or to impede the motion of the anterior mitral leaflet (a). The prosthesis is deployed by inflating (b), rapidly deflating, and quickly withdrawing the delivery balloon (c). (Adapted from Singh et al. [44]; with permission)
The Edwards SAPIEN valve, based on the original Cribier-Edwards valve (Edwards Lifesciences), is a trileaflet bovine pericardial valve mounted on a balloon-inflatable stainless steel stent. Current prosthetic sizes include 23- and 26-mm devices (inserted via 22- and 24-F sheaths, respectively), which are expanded as necessary for aortic annulus diameters between 18 to 22 mm and 21 to 25 mm, respectively. When deployed, the valve sits at the aortic annulus, precisely beneath the coronary ostia. Initial studies used an antegrade transseptal approach for placement of the valve [14, 15]. However, due to the complicated nature of the procedure regarding septal puncture and concerns of anterior mitral leaflet damage, this has been abandoned in favor of a TF or apical approach (Fig. 1) [16, 17].
The CoreValve ReValving system is a trileaflet valve composed of porcine pericardium, and is mounted on a self-expanding nitinol backbone. The prosthesis extends from the LVOT to the supracoronary ascending aorta; the wide mesh frame allows blood flow into the coronary vessels. In contrast to the Edwards SAPIEN valve, the CoreValve may only be implanted in a retrograde fashion via an 18-F sheath system, and is available in 26- and 29-mm sizes.
Transfemoral Placement
Using the TF approach, arterial access is gained by percutaneous puncture or by surgical cutdown of the femoral artery. The aortic valve is usually crossed using a left Amplatz catheter and straight wire. This is exchanged for a long stiff wire, which is advanced into the left ventricle and allowed to form a large loop. A temporary pacing wire is also placed in the right ventricle, as rapid pacing at the time of valve deployment minimizes unintentional motion of the valve.
Initially, the aortic valve is dilated using a 20- to 23-mm balloon (during rapid pacing). The valve prosthesis is then advanced across the aortic valve and positioned accurately in the predefined location under fluoroscopy. TEE is used for adjunctive imaging at this step. The valve is then deployed while pacing the heart at 180 to 220 bpm. The CoreValve is deployed by unsheathing the valve (without the need for rapid pacing), and allows for partial repositioning after deployment. In the setting of a very heavily calcified aortic valve, post-deployment ballooning of the CoreValve system may be necessary to achieve appropriate apposition to the aortic wall and minimize paravalvular aortic insufficiency (AI) [18].
Transapical Placement
Access for the TA approach is obtained via a mini-thoracotomy to provide access to the left ventricular apex. Two layers of purse-string sutures are then placed at the intended puncture site, and a cannulating needle is introduced in the apex. A wire is advanced antegrade across the aortic valve, which is then dilated with a balloon and stented during rapid pacing as in the TF route. Care must be taken to mount the Edwards SAPIEN valve appropriately with its sleeve on the ventricular side of the valve. As mentioned previously, the CoreValve has not been used for this application.
Trans-subclavian Placement
There has been interest in obtaining arterial access via the left subclavian artery for patients with significant peripheral arterial disease or other anatomic considerations that preclude use of a TF approach. Fraccaro et al. [19] recently published their feasibility study of CoreValve implantation in three patients with severe AS who were unsuitable for TF placement due to ileofemoral disease. Procedural success was achieved in all three patients without major adverse cardiovascular events at 30 days, and all patients were alive at 3 months with good functional capacity. Case reports of successful right subclavian artery approach have also been published [20].
Complications
Although TAVI has been accomplished with increasing success and safety in high-risk patients with significant comorbidities, complications related to the procedure may arise.
Peripheral Vascular
Vascular access site complications (eg, bleeding, perforation, dissection, and endothelial avulsion) plagued the early trials of TF TAVI, due to both inadequate screening for peripheral arterial disease and the large size of the introducer systems used. More contemporary trials have benefited from downsizing of the sheath system, better ileofemoral disease screening, and improved vascular access complication identification and management. As demonstrated in the SOURCE registry, the presence of vascular complications was not a significant predictor of death [16]. Nevertheless, the rate of adverse events related to access in trials of TF TAVI is still significant, underscoring the need for vigilant surveillance for complications.
The delivery systems and stented valve prostheses used in the TF approach are large. As a result, unroofing of aortic atheroma and aortic dissection are rare but significant concerns during TAVI. Dissection of the ascending aorta has also been reported as an infrequent complication. Rupture of the aortic root or annulus as a result of excessive balloon dilation or valve oversizing has been reported and carries a dismal prognosis.
Stroke
In addition to debris embolization from the calcified aortic valve, patients with AS are also likely to have other risk factors for stroke, including aortic and cerebrovascular atherosclerotic disease. As such, the risk of stroke in major TAVI trials has been up to 6%, although more contemporary trials have demonstrated rates as low as 0.6% [16, 21, 22•, 23, 24•]. Therefore, the procedure should be performed under therapeutic anticoagulation [25•].
Coronary
Due to the proximity of the coronary ostia to the stented valve prosthesis, obstruction is possible, although rare (seen in < 1 % in major trials). This may be due to impingement of the prosthetic stent on the ostium, but is more likely due to a bulky native leaflet acting as an obstacle. Therefore, preprocedural screening should include measurement of aortic leaflet height in relation to the coronary ostia. If there is any doubt as to the potential for obstruction, a coronary wire should be placed in the left anterior descending artery at the time of valve expansion, although this may not always allow access to the left main coronary artery in the event of occlusion. This complication is frequently fatal; however, there are reports of successful management using percutaneous intervention with mechanical hemodynamic support [26]. Emergent coronary bypass is not ideal due to the high-risk nature of the patients and the extensive amount of myocardium in jeopardy [26]. Thus, it is imperative that close attention is paid to signs of hemodynamic collapse, significant electrocardiogram changes, or loss of coronary flow or significant left ventricular dysfunction on TEE after valve deployment.
Valvular
During the TF approach, trauma to the anterior mitral apparatus (resulting in acute mitral regurgitation) may occur due to valve perforation by the stiff wire placed in the left ventricle, or impingement by the left ventricular side of the stented bioprosthesis. In the TA approach, anterior mitral valve damage may occur due to valve perforation or interference of the wires, sheath, or devices with the mitral chordae. This is another rare but serious complication.
Paravalvular AR is often seen with TAVI, but is usually well tolerated and clinically insignificant. The presence of ≤ 2+ AR is included in trials as an indicator of procedural success. Significant paravalvular AR, conversely, is quite rate but manifests with hemodynamic instability and should be evaluated promptly using TEE. It may be treated successfully using balloon reinflation to better appose the stented prosthesis to the aortic annulus. Significant annular and subvalvular calcification increases the risk of this complication.
Myocardium/pericardium
Injury to the myocardium due to wires and device manipulation resulted in perforation and tamponade in up to 7% of patients undergoing TAVI in the initial series [25•]. With time, the incidence has decreased significantly and occurred in only 0.3% of patients in a recent large trial [24•]. Unexplained hypotension is the typical presentation, and pericardiocentesis is usually adequate to address this complication. Fatal myocardial stunning and dysfunction due to contusion as a result of valve oversizing has also been reported and should be considered [27].
In patients undergoing TA TAVI, major complications due to accessing the left ventricular apex present with a frequency similar to vascular access complications with TF access (∼ 15%) [24•, 28]. These complications include hypoventilation requiring prolonged ventilatory support due to chest wall discomfort, pneumothorax and pleural bleeding, pericardial tamponade due to inadequate access site closure, ventricular tear requiring cardiopulmonary bypass and repair, epicardial coronary trauma, and pseudoaneurysm formation requiring repair [25•].
Conduction System
The need for permanent pacemaker due to complete heart block (CHB) has been demonstrated in between 1% and 10% in major trials of TF and TA TAVI with the Edwards SAPIEN valve (Data courtesy of Edwards Lifesciences, May 2009) [23, 29]. Permanent pacemaker implantation in some studies using the CoreValve has been greater than 25% [30]. This is also a known complication of traditional AVR in 3% to 8% of patients. TAVI-related CHB is thought to be due to the proximity of the atrioventricular nodal conduction tissue to the noncoronary aortic cusp. Expansion of the stented prosthesis in the aortic position exerts pressure on this tissue, resulting in conduction disturbances including left bundle branch block and CHB. With regard to CoreValve positioning, Piazza et al. [31] demonstrated that CHB is more common with more proximal placement (ie, the ventricular side of the device projects more into the LVOT). Therefore, proper placement should focus on not only annulus and coronary-related complications, but also the proximity of the conduction tissue.
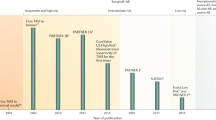
Clinical Trials
Edwards Valve
The plausibility of TAVI was first established in 1992 by Andersen et al. [32], who successfully implanted stented porcine bioprosthetic aortic valves in the ascending aorta or aortic root of seven pigs. The first report of successful TAVI in humans was provided by Cribier et al. [14] in 2002 using the percutaneous heart valve (Percutaneous Valve Technologies, Fort Lee, NJ). They implanted the stented bovine bioprosthetic valve using the antegrade transseptal approach in a patient with severe AS and cardiogenic shock. The same group reported successful TAVI in 5 of 6 patients who had been denied open heart surgery [15]. Following these reports, multiple registries and prospective trials have been conducted to evaluate the safety and efficacy of percutaneous aortic valve replacement.
With experience from initial studies, significant modifications were made to the sheath, transcatheter delivery system, and valve prosthesis (ie, anticalcific treatment). Additionally, investigators have become more cognizant of anatomic landmarks for valve deployment, and valve oversizing is performed to reduce complications of paravalvular AI. Therefore, more recent trials have provided greater procedural success and fewer complications with implantation of the Edwards SAPIEN valve.
First-in-Man Studies
Compassionate-use implantation of the Cribier-Edwards stented valve was performed by Cribier’s group under the I-REVIVE trial (which was continued as the RECAST trial) [23]. Of the 36 patients selected, implantation was attempted in 26 using the transseptal technique and in seven using a retrograde approach; implantation was not attempted in three patients due to sudden cardiac death, death during balloon valvuloplasty, or inappropriate native valve size. The investigators demonstrated successful implantation in 82% of patients (n = 26), achieving greater success with the antegrade approach (85% vs 57%). Aortic valve area (AVA) increased to 1.7 cm2 and mean transvalvular gradient was decreased to 10 mm Hg, with resultant improvements in left ventricular ejection fraction and New York Heart Association (NYHA) class. Moderate or moderate-to-severe AI was noted in 15 patients (58%), and there were six deaths (23%) at 30-day follow-up.
Efficacy and safety of the retrograde TF approach were first established by Webb et al. [16] in 2005 (reported in 2006). Using the Cribier-Edwards stented equine bioprosthetic valve, they performed the procedure in 18 patients who were selected on the basis of prohibitive surgical risk. Successful implantation was achieved in 14 patients (78%). One patient was unsuccessful due to iliofemoral tortuosity, and one patient was unsuccessful due to difficulty crossing the native aortic valve. Two patients experienced valve embolization after balloon deflation; one had the valve ultimately deployed in the aortic arch, and the other in the descending aorta. Neither faced complications as a result. In patients with procedural success, AVA increased from 0.6 to 1.6 cm2, and mean gradient decreased from 50 to 13 mm Hg. No patients experienced severe AI after implantation, although all patients had mild-to-moderate paravalvular regurgitation. At 30 days, there were two deaths (11%); one due to iliac artery perforation, and one due to left main coronary artery occlusion by a native aortic valve leaflet excrescence.
The same group extended their study to a total of 50 patients with severe calcific AS who were too high risk to undergo traditional AVR [29]. Availability of a larger, 26-mm stented valve (in addition to the original 23-mm valve), as well as a significant learning curve, greatly improved outcomes. Successful implantation increased from 76% among the first 25 patients to 96% among the second 25 patients. Similarly, 30-day mortality fell from 16% to 8%, with an estimated logistic EuroSCORE mortality of 28% for the group. No patients were left with severe paravalvular regurgitation.
Feasibility Studies
Multicenter registries in the United States (REVIVAL-II), European Union (EU) (REVIVE II), and Canada (Canadian Special Access) were organized to recruit patients to evaluate the feasibility of implantation of the Cribier-Edwards valve. All patients had severe AS with prohibitive surgical risk. The 161 patients undergoing TF implantation in REVIVAL experienced a device success rate (including ≤ 2+ AI) of 88%, and 30-day survival was 89%. The Canadian experience was recently published, and included a total of 168 patients for TF TAVI (in addition to 177 patients for TA TAVI). The patients implanted transfemorally experienced procedural success in 90.5%, with 30-day stroke and mortality rates of 3.0% and 9.5%, respectively. Permanent pacemaker implantation was necessary in 3.6%, and 13% of patients suffered a major access site complication [24•].
Postmarketing Studies
The PARTNER EU registry was begun as a feasibility trial and continues as a postmarketing evaluation (after CE mark) of TF and TA TAVI using the Edwards SAPIEN valve [33]. In the TF group enrolled for the initial feasibility study, valve implantation was defined as successful (a composite metric that included < 2+ AI) in 91% of 61 patients (Data courtesy of Edwards Lifesciences, May 2009). There were also durable improvements in ejection fraction and NYHA functional class at 6-month follow-up. In the same period, survival was 90%, and three patients suffered strokes.
The SOURCE postmarketing evaluation of the SAPIEN valve had enrolled 463 patients for its TF arm by January 2009, with an overall logistic EuroSCORE of 26%. Device success (defined as appropriate placement and < 2+ AI) was achieved in 92.4% of cases. At 30 days, mortality was 6.3% (29 patients), and 2.4% of patients suffered a stroke [8]. The investigators also found that vascular access complications, a significant source of mortality in early studies of TF TAVI, were no longer a significant predictor of death. This reflects a significant learning curve for both TAVI implantation and the recognition and management of vascular complications.
Randomized Studies
With the experience gained in the first-in-man studies and registries detailed above, enrollment was begun in the United States for the randomized PARTNER US trial. The study, which has two arms, is the first randomized, prospective study of TAVI and is conducted at 23 US sites. One arm (cohort A) aims to prove the noninferiority of TAVI versus surgical AVR in patients with high surgical risk (estimated operative mortality > 15%); the other (cohort B) aims to prove the superiority of TAVI over medical management (with or without balloon valvuloplasty) in patients who are not surgical candidates. In cohort A, TA implantation will be used for patients with inadequate TF anatomy. Enrollment has recently been completed for both arms, and 1-year outcome data should be available in the near future.
Transapical Placement
The initial experience of TA TAVI was provided by Lichtenstein et al. [17], who performed the procedure in seven patients with severe AS who were too high risk for traditional AVR and unsuitable for a TF approach due to excessive tortuosity or peripheral atherosclerosis. Implantation was successful in all seven patients; one patient (14%) died at 12 days of pneumonia, and the other six were well at 3 months. Further experience was provided by Walther et al. [34] in 59 patients. Successful implantation (defined as “proper positioning”) was achieved in 93%; postprocedural echocardiography revealed greater than 2+ AR in one patient, and 30-day mortality was 13.6%.
In the TA arm of REVIVAL, Svensson et al. [28] demonstrated an 84% device success (including ≤ 2+ AR) and a 30-day mortality of 18% in a total of 40 patients. Larger series’ of TA placement include the TRAVERCE study and the TA arms of both the SOURCE and PARTNER EU registries. Of the 172 patients in TRAVERCE, 90% experienced procedural success, and 30-day mortality was 15%. Patients in SOURCE (n = 575) and PARTNER EU (n = 69) experienced similar rates of procedural success (91%), although 30-day mortality was 10% and 19%, respectively. The recently published Canadian Experience included 177 patients implanted with a TA approach. Success was achieved in 96.1%, with 30-day stroke and mortality rates of 1.7% and 11.3%, and a 13% risk of a major access site complication [24•]. Further insight into the safety and efficacy of TA TAVI in patients deemed appropriate for open surgery or TAVI will be provided by the PARTNER US trial.
CoreValve ReValving System
The first implantation of the self-expanding CoreValve was reported in 2005 by Grube et al. [35], who provided the treatment to a 73-year-old woman with severe AS. The same group ultimately published its experience with a total of 25 patients in the “first-in-man” study of the device [36]. The procedure was performed while patients were supported on cardiopulmonary bypass. They reported an 88% immediate device success rate, although five patients (20%) in-hospital and a total of eight patients (32%) suffered a major in-hospital complication. The first 10 patients were treated using the first-generation 24-F device, whereas patients 11 to 25 were treated using the second-generation 21-F device; as expected, major bleeding was significantly less with the latter (50% vs 6.7%). The investigators subsequently provided their experience with the second- and third-generation (18-F) device in a total of 86 patients [18]. Use of the 18-F device obviated the need for extracorporeal hemodynamic support, providing a major advance in the technique. Acute procedural success was achieved in 74% of patients, no patients suffered greater than 2+ AI, and 30-day mortality was 12%.
Based on these results, the CoreValve ReValving system became the first percutaneous valve to be granted the CE mark in May 2007. After this approval, a multicenter expanded evaluation registry was created, and results were published by Piazza et al. [22•]. In a total of 646 patients, procedural success was achieved in 97%, and all patients had ≤ 2+ AI. All-cause mortality at 30 days was 8% (52 patients), 4.2% (27 patients) of which was attributed to procedural causes. Results of the expanded 18-F registry were recently presented, and in the group of 1243 patients procedural success was achieved in 98% with a 6.7% 30-day mortality [13]. Other investigators have reported similar results using the third-generation system [37].
Valve-in-Valve
Given the large number of patients who have already undergone traditional AVR, a natural evolution of the percutaneous procedure is toward use in patients with bioprosthetic AS. Thus far, only a handful of case reports on the “valve-in-valve” technique are available, but the initial experience has been encouraging. Wenaweser et al. [38] reported the first successful use of the CoreValve in a patient with severe aortic bioprosthesis degeneration and AR. Khawaja et al. [39] recently reported the successful implantation of the CoreValve in four patients with degenerative AS or AR of a bioprosthesis. Ruiz et al. [40] demonstrated the successful placement of a CoreValve within a CoreValve due to malposition of the first device too proximal in the LVOT. At 3-year follow-up, their patient is doing well with normal device function. Other investigators have confirmed the feasibility of both of these approaches, although large-scale trials have not yet validated this application of TAVI for widespread use [41–43].
Conclusions
Severe calcific AS is a significant source of morbidity and mortality among the aging population. Due to prohibitive surgical risk, many patients are not candidates for life-saving surgical AVR. To fill this unmet need, experience with TAVI has grown exponentially since its inception. With increasing experience, there is better insight regarding appropriate patient selection as well as improved procedural skill. Furthermore, device manufacturers have provided significant technologic innovations to the platform. As a result, TAVI has become both safer and more successful, resulting in CE mark approval in Europe. Diffusion of the procedure throughout the United States has begun under the investigational track, and results of the randomized PARTNER US trial are eagerly awaited.
Abbreviations
- I-REVIVE:
-
Initial Registry of Endovascular Implantation of Valves in Europe
- PARTNER:
-
Placement of Aortic Transcatheter Valve
- RECAST:
-
Registry of Endovascular Critical Aortic Stenosis Treatment
- REVIVAL-II:
-
Transcatheter Endovascular Implantation of Valves II
- REVIVE II:
-
Registry of Endovascular Implantation of Valves in Europe II
- SOURCE:
-
A European Registry of Transcatheter Aortic Valve Implantation Using the Edwards Sapien Valve
- TRAVERCE:
-
Trans-Apical Surgical Delivery of the Cribier-Edwards Aortic Bioprosthesis Clinical Feasibility.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Nkomo VT, Gardin JM, Skelton TN, et al.: Burden of valvular heart diseases: a population-based study. Lancet 2006, 368:1005–1011.
Carabello BA: Clinical practice. Aortic stenosis. N Engl J Med 2002, 346:677–682.
Iung B, Cachier A, Baron G, et al.: Decision-making in elderly patients with severe aortic stenosis: why are so many denied surgery? Eur Heart J 2005, 26:2714–2720.
Bouma BJ, van Den Brink RB, van Der Meulen JH, et al.: To operate or not on elderly patients with aortic stenosis: the decision and its consequences. Heart 1999, 82:143–148.
Otto CM, Mickel MC, Kennedy JW, et al.: Three-year outcome after balloon aortic valvuloplasty. Insights into prognosis of valvular aortic stenosis. Circulation 1994, 89:642–650.
Osswald BR, Gegouskov V, Badowski-Zyla D, et al.: Overestimation of aortic valve replacement risk by EuroSCORE: implications for percutaneous valve replacement. Eur Heart J 2009, 30:74–80.
Iung B, Himbert D, Vahanian A: A step forward in the evaluation of transcatheter aortic valve implantation. J Am Coll Cardiol 2010, 55:1091–1092.
Tuzcu EM, Kapadia SR, Schoenhagen P: Multimodality quantitative imaging of aortic root for transcatheter aortic valve implantation: more complex than it appears. J Am Coll Cardiol 2010, 55:195–197.
John D, Buellesfeld L, Yuecel S, et al.: Correlation of device landing zone calcification and acute procedural success in patients undergoing transcatheter aortic valve implantations with the self-expanding CoreValve prosthesis. JACC Cardiovasc Interv 2010, 3:233–243.
Akhtar M, Tuzcu EM, Kapadia SR, et al.: Aortic root morphology in patients undergoing percutaneous aortic valve replacement: evidence of aortic root remodeling. J Thorac Cardiovasc Surg 2009, 137:950–956.
Messika-Zeitoun D, Serfaty JM, Brochet E, et al.: Multimodal assessment of the aortic annulus diameter: implications for transcatheter aortic valve implantation. J Am Coll Cardiol 2010, 55:186–194.
Nietlispach F, Leipsic J, Al-Bugami S, et al.: CT of the ilio-femoral arteries using direct aortic contrast injection: proof of feasibility in patients screened towards percutaneous aortic valve replacement. Swiss Med Wkly 2009, 139:458–462.
Zajarias A, Cribier AG: Outcomes and safety of percutaneous aortic valve replacement. J Am Coll Cardiol 2009, 53:1829–1836.
Cribier A, Eltchaninoff H, Bash A, et al.: Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation 2002, 106:3006–3008.
Cribier A, Eltchaninoff H, Tron C, et al.: Early experience with percutaneous transcatheter implantation of heart valve prosthesis for the treatment of end-stage inoperable patients with calcific aortic stenosis. J Am Coll Cardiol 2004, 43:698–703.
Webb JG, Chandavimol M, Thompson CR, et al.: Percutaneous aortic valve implantation retrograde from the femoral artery. Circulation 2006, 113:842–850.
Lichtenstein SV, Cheung A, Ye J, et al.: Transapical transcatheter aortic valve implantation in humans: initial clinical experience. Circulation 2006, 114:591–596.
Grube E, Schuler G, Buellesfeld L, et al.: Percutaneous aortic valve replacement for severe aortic stenosis in high-risk patients using the second- and current third-generation self-expanding CoreValve prosthesis: device success and 30-day clinical outcome. J Am Coll Cardiol 2007, 50:69–76.
Fraccaro C, Napodano M, Tarantini G, et al.: Expanding the eligibility for transcatheter aortic valve implantation the trans-subclavian retrograde approach using: the III generation CoreValve revalving system. JACC Cardiovasc Interv 2009, 2:828–833.
Ruge H, Lange R, Bleiziffer S, et al.: First successful aortic valve implantation with the CoreValve ReValving System via right subclavian artery access: a case report. Heart Surg Forum 2008, 11:E323–E324.
Schaechinger V: Results from The PARTNER EU Trial: Primary Endpoint Analysis. Presented at the EuroPCR. Barcelona, Spain; May 19–22, 2009.
• Piazza N, Grube E, Gerckens U, et al.: Procedural and 30-day outcomes following transcatheter aortic valve implantation using the third generation (18 Fr) corevalve revalving system: results from the multicentre, expanded evaluation registry 1-year following CE mark approval. EuroIntervention 2008, 4:242–249. This paper discusses the results of a large, contemporary series of patients undergoing TAVI using the CoreValve ReValving system.
Cribier A, Eltchaninoff H, Tron C, et al.: Treatment of calcific aortic stenosis with the percutaneous heart valve: mid-term follow-up from the initial feasibility studies: the French experience. J Am Coll Cardiol 2006, 47:1214–1223.
• Rodes-Cabau J, Webb JG, Cheung A, et al.: Transcatheter aortic valve implantation for the treatment of severe symptomatic aortic stenosis in patients at very high or prohibitive surgical risk: acute and late outcomes of the multicenter Canadian experience. J Am Coll Cardiol 2010, 55:1080–1090. This paper discusses the recently published Canadian experience of TF and TA TAVI.
• Masson JB, Kovac J, Schuler G, et al.: Transcatheter aortic valve implantation: review of the nature, management, and avoidance of procedural complications. JACC Cardiovasc Interv 2009, 2:811–820. This is a comprehensive review of complications encountered with TAVI.
Kapadia SR, Svensson L, Tuzcu EM: Successful percutaneous management of left main trunk occlusion during percutaneous aortic valve replacement. Catheter Cardiovasc Interv 2009, 73:966–972.
Babaliaros V: Presented at the American College of Cardiology’s 59th Annual Scientific Session and i2 Summit. Atlanta, GA; March 14–16, 2010.
Svensson LG, Dewey T, Kapadia S, et al.: United States feasibility study of transcatheter insertion of a stented aortic valve by the left ventricular apex. Ann Thorac Surg 2008, 86:46–54; discussion 54–55.
Webb JG, Pasupati S, Humphries K, et al.: Percutaneous transarterial aortic valve replacement in selected high-risk patients with aortic stenosis. Circulation 2007, 116:755–763.
theheart.org: FRANCE: Transcatheter-valve registry permits "observation" of CoreValve, Sapien differences. Available at http://www.theheart.org/article/1021541.do. Accessed December 7, 2009.
Piazza N, Onuma Y, Jesserun E, et al.: Early and persistent intraventricular conduction abnormalities and requirements for pacemaking after percutaneous replacement of the aortic valve. JACC Cardiovasc Interv 2008, 1:310–316.
Andersen HR, Knudsen LL, Hasenkam JM: Transluminal implantation of artificial heart valves. Description of a new expandable aortic valve and initial results with implantation by catheter technique in closed chest pigs. Eur Heart J 1992, 13:704–708.
theheart.org: Low 30-day and six-month mortality for transfemoral valve implantation in PARTNERS EU and SOURCE. Available at http://www.theheart.org/article/910857.do. Accessed November 2, 2009.
Walther T, Simon P, Dewey T, et al.: Transapical minimally invasive aortic valve implantation: multicenter experience. Circulation 2007, 116(11 Suppl):I240–I245.
Grube E, Laborde JC, Zickmann B, et al.: First report on a human percutaneous transluminal implantation of a self-expanding valve prosthesis for interventional treatment of aortic valve stenosis. Catheter Cardiovasc Interv 2005, 66:465–469.
Grube E, Laborde JC, Gerckens U, et al.: Percutaneous implantation of the CoreValve self-expanding valve prosthesis in high-risk patients with aortic valve disease: the Siegburg first-in-man study. Circulation 2006, 114:1616–1624.
Tamburino C, Capodanno D, Mule M, et al.: Procedural success and 30-day clinical outcomes after percutaneous aortic valve replacement using current third-generation self-expanding CoreValve prosthesis. J Invasive Cardiol 2009, 21:93–98.
Wenaweser P, Buellesfeld L, Gerckens U, Grube E: Percutaneous aortic valve replacement for severe aortic regurgitation in degenerated bioprosthesis: the first valve in valve procedure using the Corevalve Revalving system. Catheter Cardiovasc Interv 2007, 70:760–764.
Khawaja MZ, Haworth P, Ghuran A, et al.: Transcatheter aortic valve implantation for stenosed and regurgitant aortic valve bioprostheses CoreValve for failed bioprosthetic aortic valve replacements. J Am Coll Cardiol 2010, 55:97–101.
Ruiz CE, Laborde JC, Condado JF, et al.: First percutaneous transcatheter aortic valve-in-valve implant with three year follow-up. Catheter Cardiovasc Interv 2008, 72:143–148.
Ussia GP, Mule M, Tamburino C: The valve-in-valve technique: transcatheter treatment of aortic bioprothesis malposition. Catheter Cardiovasc Interv 2009, 73:713–716.
Ng AC, van der Kley F, Delgado V, et al.: Percutaneous valve-in-valve procedure for severe paravalvular regurgitation in aortic bioprosthesis. JACC Cardiovasc Imaging 2009, 2:522–523.
Bruschi G, Demarco F, Oreglia J, et al.: Transcatheter aortic valve-in-valve implantation of a CoreValve in a degenerated aortic bioprosthesis. J Cardiovasc Med (Hagerstown) 2010, 11:182–185.
Singh IM, Tuzcu EM, Shishehbor MH, et al.: Percutaneous treatment of aortic valve stenosis. Cleve Clin J Med 2008, 75:805–812.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krishnaswamy, A., Tuzcu, E.M. & Kapadia, S.R. Update on Transcatheter Aortic Valve Implantation. Curr Cardiol Rep 12, 393–403 (2010). https://doi.org/10.1007/s11886-010-0126-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-010-0126-5