Abstract
In November 2013, the American College of Cardiology and American Heart Association (ACC/AHA) released a clinical practice guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease (ASCVD) risk in adults. The guideline recommendations were developed from a rigorous systematic review of randomized, controlled trials (RCTs) and meta-analyses of RCTs that evaluated ASCVD outcomes. Major recommendations address a healthy lifestyle, identification of groups of patients most likely to experience a net benefit form statin therapy, appropriate intensity of statin therapy to reduce ASCVD, safety, decision-making in primary prevention, monitoring therapy, and appropriate use of nonstatin therapy. Areas of controversy are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The long-awaited Adult Treatment Panel (ATP) IV guidelines were finally released in the fall of 2013 as the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) Guideline for the Treatment of Blood Cholesterol to Reduce ASCVD Risk in Adults [1••]. Convened by the National Heart, Lung and Blood Institute in 2008, the Panel undertook a rigorous systematic review of randomized, controlled trials (RCTs) of cholesterol-lowering drug therapy that had atherosclerotic cardiovascular disease (ASCVD) outcomes, and meta-analyses of these trials. The guideline development process adhered to most of the principles that were subsequently advocated by the Institute of Medicine for developing trustworthy guidelines [2]. Based on the design and results of the randomized trials and meta-analyses published through July 2013, the 2013 ACC/AHA cholesterol recommendations represent a new paradigm for treating cholesterol focused on using the appropriate intensity of statin therapy for those most likely to benefit. This is in contrast to the previous ATP III guideline that recommended treatment to specific low-density lipoprotein cholesterol (LDL-C) and non-high density lipoprotein cholesterol (non-HDL-C) treatment goals. Not surprisingly, this paradigm shift has not been without controversy. The 2013 cholesterol recommendations are reviewed and areas of controversy highlighted. A listing of the major guideline recommendations can be found in the Table 1. Refer to the 2013 ACC/AHA cholesterol guideline report for a complete listing of the recommendations.
This is a Comprehensive Guideline for Treating Cholesterol to Reduce ASCVD Risk
The Panel considered only RCTs and meta-analyses of RCTs of drug therapy with ASCVD outcomes. Laboratory, animal, epidemiologic, and other observational data were not considered. Although this approach has been criticized, recommendations based only on RCTs data are the most relevant for clinical practice. Although the Panel fully acknowledged the extensive body of evidence demonstrating a causal relationship between cholesterol and ASCVD, the Panel also required there to be evidence that a cholesterol-lowering drug reduce ASCVD events with an acceptable margin of safety. Therefore, RCTs were considered the most unbiased assessment of drug treatment effects and adverse effects. Given the wide range of patient populations included in statin RCTs, the Panel was able to confidently make recommendations that would apply to the majority of patients who would be considered candidates for statin therapy. It is unlikely observational data could override the findings from the statin RCTs, or extend the lack of evidence from nonstatin RCTs. Observational data has many well understood limitations, which include biases in who is treated and who is adherent to therapy, as well as multiple measurement biases, including verification of statin use, type and dose of statin used, consistency of use over time, and ascertainment of ASCVD outcomes and adverse effects. These limitations are addressed in intent-to-treat analyses of RCTs, which is why the FDA now requires well-designed RCTs for drug approval.
Elimination of LDL-C and non-HDL-C Treatment Targets & Focus on Intensity of Statin Therapy
Two critical questions evaluated the evidence for treatment to specific LDL-C and non-HDL-C goals in secondary and primary prevention. A systematic review of secondary and primary prevention statin RCTs was unable to identify any RCTs in which titration to achieve a specific LDL-C (and/or non-HDL-C) goal in a treatment group was compared to another goal or treatment strategy. Rather, RCTs used fixed doses of a statin. Strong evidence showed moderate intensity statin therapy reduced ASCVD events in secondary and primary prevention populations. Strong evidence was also found that high intensity statin therapy (with an average ≥50 % reduction in LDL-C) reduced ASCVD events more than moderate intensity statin therapy (with an average 30 to <50 % reduction in LDL-C). Therefore, high intensity statin therapy is recommended for groups of patients that are most likely to experience the greatest margin of benefit from the reduction in ASCVD risk given the greater potential for adverse effects (Emphasis on Net Benefit from Statin Therapy). Moderate intensity statin therapy is recommended when conditions influencing safety are present, or in primary prevention patients less likely to experience a net benefit from high intensity statin therapy (Initiate Statins for Primary Prevention Based on 10-Year ASCVD Risk Estimate and a Clinician-Patient Discussion).
High intensity statins lower LDL-C by ≥50 % (atorvastatin 40–80 mg or rosuvastatin 20–40 mg). Moderate intensity statins lower LDL-C by 30 to <50 % (atorvastatin 10–20 mg, fluvastatin 80 mg, lovastatin 40 mg, pitvastatin 2–4 mg, pravastatin 40 mg, rosuvastatin 5–10 mg, and simvastatin 20–40 mg). Statins and doses in bold were found to have an ASCVD event reduction benefit in the RCTs evaluated by the Panel.
In light of the extensive and consistent evidence supporting use of high and moderate intensity statin therapy, the panel considered there to be the potential for harm from continued use of the treat to target strategy. For example, a patient with clinical ASCVD might be considered at goal with LDL-C <100 mg/dl on a low intensity statin, thereby depriving them of the potential for an additional ASCVD risk reduction benefit from evidence-based high intensity statin therapy. In addition, a patient with clinical ASCVD might have an LDL-C of 105 mg/dl on a high intensity statin. The next step in a treat-to-target approach would be to add another LDL-C lowering drug. However, there is little evidence that adding a non-statin drug to high-intensity statin therapy further reduces ASCVD events or has an acceptable margin of safety (Measure a Fasting Lipid Panel at Baseline and During Follow-up).
Emphasis on Net Benefit from Statin Therapy
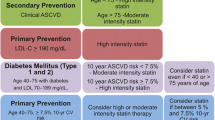
Strong evidence supports the use of statin therapy in four groups of patients based on the ASCVD risk reduction benefit far exceeding the potential for adverse effects:
-
I.
Clinical ASCVD
-
Age ≤75 years and no safety concerns: High intensity statin
-
Age >75 years or safety concerns: Moderate intensity statin
-
-
II.
Primary prevention – primary LDL-C ≥190 mg/dl
-
Age ≥21 years: High intensity statin
-
-
III.
Primary prevention - Diabetes age 40–75 years and LDL-C 70–189 mg/dl
-
Moderate intensity statin
-
Consider high intensity statin when ≥7.5 % 10 year ASCVD risk using the Pooled Cohort Equations
-
-
IV.
Primary prevention – No diabetes ≥7.5 % 10-year ASCVD risk age 40–75 years and LDL-C 70–189 mg/d
-
Moderate or high intensity statin
-
Moderate evidence also supports a net benefit for the use of moderate intensity statins for primary prevention in those with 5 to <7.5 % 10-year ASCVD risk. Two groups of patients have not been shown to experience an ASCVD event reduction benefit from the routine initiation of statin therapy: those with New York Heart Association Class II-IV heart failure and those undergoing maintenance hemodialysis.
Muscle symptoms are common in statin-treated patients but not necessarily caused by statin therapy. Establish the relationship of mild to moderate muscle, or other symptoms, to statin therapy by discontinuing the statin until symptoms resolve, then restarting the same or a different statin at a lower dose. Repeat this process until a well-tolerated statin and dose are identified. Severe myopathy, rhabdomyolysis and potentially hemorrhagic stroke are rare complications of statin therapy. Statins have no significant hepatotoxicity so a measure of hepatic transaminases is indicated only if symptoms develop during follow-up.
A modest excess of diabetes from statin therapy was observed in RCTs. Nonetheless, the ASCVD risk reduction benefit from moderate intensity statins exceeds the risk of diabetes in all but the lowest risk individuals. For high intenisty statins, the excess risk of adverse events begins to appraoch the ASCVD event reduction beenfit when the 10-year ASCVD risk is <7.5 %. Screening and prevention of diabetes should occur according to current guidelines for diabetes.
Initiate Statins for Primary Prevention Based on 10-Year ASCVD Risk Estimate and a Clinician-Patient Discussion
When determining whether to initiate statin therapy in patients without ASCVD or diabetes, the first step is to estimate the 10-year ASCVD risk using the newly developed Pooled Cohort Equations recommended by the 2013 ACC/AHA Guideline for the Assessment of Cardiovascular Risk [3•]. Desktop, iPhone and Android versions of the Pooled Cohort Equations risk calculator can be found at http://my.americanheart.org/professional/StatementsGuidelines/PreventionGuidelines/Prevention-Guidelines_UCM_457698_SubHomePage.jsp. These equations estimate the risk of nonfatal myocardial infarction, coronary heart disease death, and nonfatal and fatal stroke in white and African American women and men who are not receiving statin therapy and have an untreated LDL-C <190 mg/dl. It may also be helpful to use the Pooled Cohort equations to estimate 10-year ASCVD risk in patients with diabetes when deciding whether to initiate high intensity statin therapy.
The Pooled Cohort Equations has been criticized by Drs. Ridker and Cook, who have reported that the Equations overestimate 10-year ASCVD risk in their cohorts of health professionals and clinical trial participants from the Women’s Health Initiative [4]. They instead promote the use of inclusion criteria from the statin trials as the basis for initiating statin therapy. In response, the authors of the 2013 ACC/AHA Risk Assessment Guideline, Drs. Lloyd-Jones and colleagues have pointed out that the cohorts evaluated by Drs. Ridker and Cook are low risk white populations that not representative of the US population of white and African American individuals [5••]. Indeed, that is why these three cohorts were not included with the five representative U.S. cohorts of white and African American men and women used to develop the Pooled Cohort Equations. Dr. Lloyd-Jones further observed the Pooled Cohort Equations estimate risk quite accurately in lower risk individuals in whom the treatment decision is being made. Overestimation only occurs in higher risk individuals for whom a treatment decision is already clear. Moreover, it should be noted use of the statin trial RCT inclusion criteria identifies >45 % of those with <5 % 10-year ASCVD risk as candidates for statin therapy, while failing to identify >35 % of those with ≥7.5 % 10-year ASCVD risk as a candidate for statin therapy [1••]. This is because important risk factors such as smoking and the increase in ASCVD risk with advancing age are not accounted for in the dichotomous age and risk factor cut-offs used for the statin trial eligibility.
Once 10-year ASCVD risk has been estimated, the clinician and patient should discuss initiating statin therapy. The discussion should include the potential for an ASCVD risk reduction benefit, adverse effects, drug-drug interactions, and patient preferences. Other factors may be considered when a risk-based decision is unclear: LDL-C ≥160 mg/dl, family history of premature ASCVD, lifetime ASCVD risk, high sensitivity–C-reactive protein ≥2.0 mg/L, coronary artery calcification (CAC) score ≥ 300 Agatston units or ankle–brachial index (ABI) <0.9.
Measure a Fasting Lipid Panel at Baseline and During Follow-up
A fasting lipid panel at baseline is needed to rule out severe hypertriglyceridemia (≥500 mg/dl, which requires evaluation and treatment) and establish baseline untreated LDL-C. To monitor response to statin and lifestyle therapy, percent reduction in LDL-C levels from the untreated baseline consistent with the intensity of statin should be assessed with 4–12 weeks of statin initiation, and, subsequently, every three to 12 months as indicated. The anticipated therapeutic response for high intensity statin is an approximately ≥50 % reduction in LDL-C from baseline, and for moderate intensity statins is approximately 30 % to <50 %. If the baseline LDL-C levels are unknown, it was observed that an LDL-C <100 mg/dl was achieved by most individuals receiving a high intensity statin in the high versus moderate intensity statin RCTs. If a less than anticipated reduction in LDL-C occurs after initiating a statin, lifestyle and drug adherence should be re-addressed. Statin therapy may be up-titrated as tolerated. The addition of non-statin therapy may also be considered in selected individuals.
Limited Role for Non-Statin Drug Therapy
To date, there has been limited RCT evidence to determine whether adding a non-statin lipid-lowering drug further reduces ASCVD events in statin-treated individuals. Moreover, there is no evidence to determine the safety of non-statin therapy added to high-intensity statin therapy, the gold standard therapy for ASCVD risk reduction. That being said, there are select patients who could benefit from the addition of nonstatin LDL-C-lowering therapy. Individuals with genetic hypercholesterolemia as evidenced by untreated LDL-C ≥190 mg/dl may still need additional LDL-C lowering even on a high intensity statin. High risk individuals, such as those with clinical ASCVD or diabetes aged 40–75 years, unable to tolerate the recommended intensity of statin therapy, may also benefit from the addition of a nonstatin LDL-C lowering drug. Once intolerance to any dose of statin has been established, nonstatin drugs can be considered. Preference should be given to drugs that have been shown to reduce ASCVD events and to have an acceptable margin of safety.
Lifestyle as the Foundation for Drug Therapy to Reduce ASCVD Risk
All cholesterol-lowering drug RCTs were performed in the background of healthy lifestyle recommendations. A healthy lifestyle can prevent development or worsening of the risk factors contributing the increased ASCVD risk. The Cholesterol Panel endorsed the 2013 ACC/AHA Lifestyle Management Guideline [6•]. The Lifestyle Guideline recommends adherence to a diet low in saturated fat, trans-fat and sodium, and high in vegetables, fruits, whole grains, low fat dairy products, poultry, fish, legumes, non-tropical vegetable oils and nuts and limiting intake of sweets, sugar-sweetened beverages, salt and red meats. Regular aerobic physical activity and maintaining a healthy body weight are also recommended. Blood pressure control, diabetes prevention and management, and avoidance of smoking also are essential for ASCVD prevention.
Conclusion
The 2013 ACC/AHA cholesterol guideline is an evidence-based approach to reducing ASCVD risk. These recommendations provide an patient-centered approach to drug treatment based on the potential for a net ASCVD risk reduction benefit and the unique characteristics and preferences of each patient.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Stone N, Robinson J, Lichtenstein A, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults. Circulation. 2013. doi:10.1161/1101.cir.0000437738.0000463853.0000437737a. This is the 2013 U.S cholesterol guideline as discussed in this paper.
Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. Clinical Practice Guidelines We Can Trust:, 2011: Institute of Medicine;2011.
Goff DC, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013. doi:10.1161/1101.cir.0000437741.0000448606.0000437798. This is the 2013 U.S risk assessment guideline discussed in this paper.
Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013.
Lloyd-Jones D, Goff D, Stone N. Letter to the editor: Statins, risk assessment, and the new American prevention guidelines. Lancet. 2014;383:600–2. The letter addresses criticisms of the Pooled Cohort Equations for ASCVD risk prediction.
Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. November 12, 2013 2013. This is the 2013 U.S lifestyle guideline discussed in this paper.
Disclosures
Research grants to Institution: Amarin, Amgen, Astra-Zeneca, Daiichi-Sankyo, Genentech/Hoffman La Roche, Glaxo-Smith Kline, Merck, Regeneron/Sanofi, Zinfandel/Takeda.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Jennifer G. Robinson has consulted for Amgen, Hoffman LaRoche, Merck, Pfizer, and Sanofi.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on 2013 Cholesterol Treatment Guidelines
Rights and permissions
About this article
Cite this article
Robinson, J.G. 2013 ACC/AHA Cholesterol Guideline for Reducing Cardiovascular Risk: What is so Controversial?. Curr Atheroscler Rep 16, 413 (2014). https://doi.org/10.1007/s11883-014-0413-5
Published:
DOI: https://doi.org/10.1007/s11883-014-0413-5