Abstract
This review examines the emerging role of endothelial shear stress (ESS) and blood viscosity on the initiation and progression of atherosclerosis in peripheral arterial disease. Among the variables determining ESS, blood viscosity has to date been the most overlooked by clinical researchers. Blood viscosity is a laboratory assessment that is minimally invasive and modifiable using pharmacologic therapy as well as by hemodilution. Monitoring and controlling blood viscosity not only modulates ESS, but also reduces peripheral vascular resistance and increases blood flow to the lower extremities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lower extremity peripheral arterial disease (PAD) is an atherothrombotic disease state affecting 5 to 12 million in the USA [1]. Progressive arterial narrowing in the arteries that deliver blood to the lower extremities impedes blood flow that may result in ischemic pain, injury or limb loss. The ischemic pain usually manifests as intermittent claudication with pain during ambulation in the calf muscles or other lower extremities that resolves with rest [2]. Claudication occurs when blood flow to the lower extremities fails to meet the metabolic demands of skeletal muscle during exercise such as walking. Symptom relief is possible with exercise training, pharmacotherapy, and cessation of smoking. The risk of limb-loss becomes substantial when there is resting pain, ischemic ulceration, or gangrene [2]. The risk of lower extremity amputation, however, is often overshadowed by the risk of mortality from coexistent coronary artery and cerebrovascular atherosclerosis. The relative risk of cardiovascular disease (CVD) events and death for patients with PAD is comparable with those having coronary or cerebrovascular disease [3]. Patients with PAD are at high risk for myocardial infarction and ischemic stroke, and those with critical limb ischemia have greater than a threefold increased risk for all-cause and CVD mortality compared with patients with only intermittent claudication, even after adjustment for traditional major risk factors such as age, established CVD, smoking, systemic hypertension, diabetes and serum cholesterol [4, 5, 6•].
Non-invasive testing is conventionally used for the screening and diagnosis of PAD. Ankle-brachial index (ABI) is used to screen for PAD and assess the risk of CVD, and the link between lower ABI measurements and CVD events is well-established [5]. Despite widespread use however, the accuracy of ABI as a screening methodology for PAD is not firmly established, and ABI measurements are not reliable when arteries are incompressible as for instance in diabetes. In patients with non-compressible arteries, the toe-brachial index (TBI) is often used. In addition, ABI is not recommended for asymptomatic adults who do not have a prior diagnosis of PAD, CVD, severe chronic kidney disease or diabetes [7•].
Analogous to ABI, blood viscosity is a quantifiable hemodynamic parameter that is physiologically related to blood flow and blood pressure. Site-specific lesions have long provided pathological support for the critical involvement of hemodynamic forces in the initiation and progression of atherosclerotic lesions. Among several hemodynamic forces that have been studied extensively, one in particular—endothelial shear stress—has emerged as a key link in the localization of atherosclerotic plaques.
Hemodynamic Endothelial Shear Stress in Peripheral Arterial Disease
Endothelial shear stress (ESS) is the tangential frictional force per unit area [N/m2 or Pa] applied by blood flow upon the endothelial wall and, for decades, has been implicated as a factor in the development of atherosclerosis or atherothrombosis [8••, 9–12]. A number of researchers have previously reported that in order to preserve endothelial function, blood flow should maintain a steady laminar ESS within a physiologic range of between 10 dyne/cm2 to 70 dyne/cm2 [8••]. Outside the physiologic range under turbulent oscillatory ESS or low ESS below 4 dyne/cm2 at arterial bifurcations or distal segments of plaques, endothelial cell integrity is compromised with an apoptosis rate in endothelial cells that increased as much as sevenfold [13]. Oscillatory ESS can be quantified in terms of shear stress gradients over time (i.e., \( \frac{d}{ dt}{\tau}_w \)), which, if outside the physiologic range, can induce adverse morphological and functional changes in the endothelium in regions of disturbed flow, contributing to the formation and disruption of atherosclerotic lesions [14, 15]. Endothelial cells exposed to low ESS lose their elongated phalanx structure, adopting a rounder profile associated with augmented expression of inflammatory genes responsible for increased synthesis of endothelial-localized adhesion molecules, transmigration of mononuclear cells into subendothelial space, and intrusion and incorporation of lipoproteins into tissue macrophages [16–23]. Using coronary intravascular ultrasound (IVUS) to characterize atherosclerotic plaque volume in humans, low ESS predicted histopathological features of inflammation, thin fibrous cap and development of other vulnerable plaque attributes associated with ischemic events [24]. Importantly, it has been observed that atherosclerotic plaques, which have begun to intrude into the lumen, are exposed to high ESS especially at the proximal neck of plaque, playing a role in plaque rupture [25, 26••] (see Fig. 1).
Differential distribution of shear stress in an arterial segment with lumen-protruding plaque with necrotic core (NC). Modified from [26••]
Mathematically, ESS is defined as the product of blood viscosity and shear rate, where the shear rate is essentially the ratio of flow velocity to lumen diameter, 4 V/d. As such, ESS, τw, can be determined as the product of blood viscosity, μ, and shear rate, 4 V/d, as
where V is the maximum velocity at the center, and d is the lumen diameter. Changes in viscosity directly modulate ESS (i.e., friction at the vascular wall). In PAD, the combined effect of the narrowed lumen and an abnormally increased blood viscosity could profoundly impair blood flow to the extremities.
The localization of atherosclerotic plaques at arterial segments subjected to disturbed blood flow and low ESS has been reported for several decades [9, 27]. More recently however, using magnetic resonance angiography (MRA) and IVUS data, various researchers have reconstructed coronary and carotid arteries in 3D to demonstrate linkages between low ESS and plaque progression as well as new plaque formation [24, 26••, 28]. In these investigations and many others, ESS is calculated using an idealized Newtonian blood viscosity model, and only a select few studies used non-Newtonian blood viscosity models to account for the high variability of viscosity as a function of shear rate [15, 28, 29•, 30–35]. None measured the patients’ own blood viscosity profiles nor incorporated patient-specific blood viscosity measurements into the calculation of ESS values. The vast majority of studies in the role of ESS in atherosclerosis have been focused on coronary and carotid arteries with only a select few directed to the femoral arteries.
In a preliminary study of 44 patients with PAD, having ABI < 0.9, using 2D phase-contrast magnetic resonance imaging of femoral arteries, patients with femoral plaques showed significant increases in peak systolic ESS when compared with patients with neither wall thickening nor signs of plaque. Greater eccentricity in systolic ESS distribution was observed in patients with loose matrix / necrotic core and calcified plaques as compared with PAD patients without femoral wall abnormalities, reflecting deranged blood flow profiles likely due to asymmetric narrowing of the lumen [36•]. Earlier studies using angiography to characterize femoral artery atherosclerosis have also implicated disturbed blood flow regimes in curved arterial segments in the promotion of plaque growth [37, 38].
Tortuosity and curvature in the femoral artery have been previously linked to the development of atherosclerosis [39]. Using 3D reconstruction of MRA from 18 apparently healthy young adults, mean ESS was demonstrated to be lower in males than in females. Both ESS and blood viscosity values are velocity and lumen-diameter dependent, varying widely through a single cardiac cycle. In this study, pulsatile flow simulation revealed greater spatial variations in men than in women, indicating greater variation in ESS in the male and exposure to a wider range of hemodynamic frictional forces [40]. These data indicate that sex differences related to body size and the anatomical course of the femoral artery may contribute to increased risk of focal atherosclerosis in the adductor canal. Both tortuosity and curvature of femoral arteries were reported to be significantly greater for men than women. In both sexes, tortuosity increased from mid-thigh to the popliteal fossa. The greatest curvature was found within the distal quarter of the superficial femoral artery (SFA).
The flow in the vessels at the lower extremities has strong spiral flow patterns due to tortuosity and curvature, categorically different from separated disturbed flow in the region of carotid sinus [41]. Tortuosity in the adductor region induces a helical flow pattern with highly non-uniform, helical distribution of flow and, consequently, low ESS. Spiral patterns of early atheroma in the femoral artery may be directly related to spiral blood flow regimes [40, 42]. Common features of flow in the SFA include the occurrence of skewed velocity profiles toward the outer wall of curved regions, with marked sex differences in ESS patterns and the degree of development of spiral flow along the vessel.
Endothelial shear stress is a hemodynamic parameter with the potential to link tortuosity and blood flow regimes specific to PAD on one hand, together with endothelial function and permeability in atherosclerotic plaque development, on the other [43]. Regions of low ESS in the femoral arteries are prone to atherogenesis and progression of atherosclerotic lesions. Furthermore, they may account for increased prevalence of stenoses in the adductor region of the SFA [44] and sex differences in PAD. Oscillatory ESS and flow separation may not be the only hemodynamic factors implicated in the etiology of focal atherosclerosis. Increased cyclical variation in ESS or wider ranges of ESS variation within a cardiac cycle may also provide increased mechanical stimulus for localized plaque generation [41] as well as plaque erosion [13, 45] and thrombosis.
Blood Viscosity
The viscosity of a fluid represents the frictional resistance between a moving fluid and a stationary wall [46]. Blood viscosity represents the thickness and stickiness of blood and is defined as its inherent resistance to flow. Since about 45 % of blood volume is made up of suspended cellular particles, primarily erythrocytes, the blood behaves as a non-Newtonian fluid, meaning its viscosity varies with shear rate. The dynamic range of blood viscosity is relatively large—as wide as 4-45 cP during a single cardiac cycle from peak-systole to end-diastole [47, 48].
When blood moves at high velocity during systole through any large artery having a diameter greater than about 3 mm (with the exception of the left coronary), erythrocytes are well-dispersed and maximally deformed to an elliptical shape for minimal flow resistance [47, 49]. Under such conditions, blood is less viscous. The apparent blood viscosity corresponding to this high shear rate (i.e., ≥300 s-1) is approximately 3-5 times that of water [47]. When blood moves slowly (e.g., <0.01 cm/s), it is significantly more viscous as erythrocytes tend to aggregate. Under such low shear rate flow regimes, the apparent blood viscosity increases to 10-40 times that of water depending on the aggregation behavior of red blood cells [50•].
Blood viscosity is a dynamic property varying as a function of lumen diameter and flow velocity. The principal determinants of blood viscosity are hematocrit, plasma protein concentrations, erythrocyte aggregation and deformability (i.e., the structural responsiveness of red cells to applied forces), and plasma viscosity as depicted in Fig. 2 [48, 49, 50•, 51]. Of these, hematocrit has the greatest effect on blood viscosity: a 10 % increase of hematocrit increases high-shear blood viscosity by around 5 % [52], whereas the same increase in hematocrit increases low-shear blood viscosity by approximately 30 % [53]. It is important to note that although oxygen molecules are transported by hemoglobin within erythrocytes, an increase in hematocrit does not necessarily increase oxygen delivery, particularly at the tissue level, because higher hematocrit simultaneously increases peripheral vascular resistance via elevations in blood viscosity, which in some cases outweighs the increase in hemoglobin [53].
Plasma proteins such as fibrinogen and immunoglobulins are also important determinants of viscosity. These proteins are instrumental in erythrocyte aggregation in the microcirculation and Rouleaux formation [48, 50•, 54, 55]. Both fibrinogen and immunoglobulins are relatively long chain molecules that promote aggregation [50•, 54, 56]. In contrast, albumin has been reported to suppress aggregation [57]. Low-density lipoprotein (LDL) molecules have also been shown to promote erythrocyte aggregation, increasing blood viscosity at low shear rates, whereas HDL molecules have been reported to suppress aggregation [48, 50•, 58–60].
Numerous studies have examined the relationship between viscosity and triglyceride levels. The West of Scotland Coronary Prevention Study followed 6,595 hypercholesterolemic adult males prospectively for an average of 4.9 years and reported that plasma viscosity and whole blood viscosity were both significantly associated with triglycerides and VLDL concentration [61]. In a study of 126 healthy nonsmoking adults, blood viscosity was shown to correlate with triglyceride concentration (r = 0.41, p = 0.0007) [62]. Using hematocrit-adjusted blood viscosity levels at high-shear and low-shear rates, blood viscosity was shown to be significantly associated with triglycerides in a cross-sectional study of 257 adults who were being assessed for cardiovascular risk factors (high-shear viscosity r = 0.35, low-shear viscosity r = 0.22, both p values < 0.0005) [63]. In addition, isolated chylomicrons, VLDL and LDL added to plasma or serum in vitro cause a dose-dependent and exponential rise in viscosity [64, 65]. VLDL was accompanied by a greater viscosity change than LDL, thereby supporting the influence of plasma protein size on viscosity [65].
Blood viscosity measured at low shear rates reflects flow conditions at end-diastole and, simultaneously, microcirculatory behavior such as the flow-retarding effect of cell aggregation, which in turn is influenced by plasma proteins such as fibrinogen [54, 66, 67]. On the other hand, blood viscosity measured at high shear rates reflects higher velocity blood flow regimes as in large arteries at the peak of systole, where viscosity is dependent largely on hematocrit and the deformability of erythrocytes [49].
Hemorheological Abnormalities in Peripheral Arterial Disease
A number of researchers have investigated whether or not hemorheological abnormalities are present in PAD patients. In an earlier prospective study of 62 patients with intermittent claudication followed for up to three years, Dormandy et al., observed a significant correlation between the progressive deterioration of peripheral circulatory disturbances and initial blood viscosity levels, as well as the plasma fibrinogen level and the susceptibility of red cell membrane lipids to autoxidation [68]. A second study by the same group reported that blood viscosity was higher in PAD patients with resting pain than in those with intermittent pain. Furthermore, blood viscosity was higher in patients with a claudication distance of less than 91 m than in those less severely disabled (i.e., >91 m) [69]. The researchers suggested that hyperviscosity may be the determining cause of claudication in some PAD patients.
A third study by Dormandy et al., compared 120 patients having intermittent claudication with normal age-matched controls and found blood viscosity was significantly higher among claudicants (p < 0.001) with the greatest difference in blood viscosity observed at lowest shears [70]. At high shear rates, patients with blood viscosity above 4.5 cP had mean claudication distance of 126 meters compared to 289 meters for patients with high-shear viscosity below that threshold. Hyperviscosity among claudicants was not attributable to differences in hematocrit but rather to plasma fibrinogen. The researchers sought to examine if the principal cause of circulatory insufficiency in patients with symptoms of intermittent claudication was an abnormally high blood viscosity rather than narrowing of the arteries. They found that many patients with abnormally high blood viscosity have normal arteriograms despite severe symptoms of claudication and suggested the use of the term rheological claudication to describe approximately 25 % of moderate to severe claudicants with hyperviscosity of blood having significantly worse prognoses [70] (Table 1).
Separately, plasma viscosity was shown to be significantly elevated in individuals with intermittent claudication compared with healthy age-matched controls [71]. Plasma viscosity levels in Fontaine IIb and III stage PAD patients correlated with plasma fibrinogen concentrations. Furthermore, the blood filtration rate, a measure of erythrocyte deformability, varied with walking distance and inversely with the stage of disease.
In the Edinburgh Artery Study, which followed a random sample of 1,581 men and women 55 to 74 years of age with symptomatic or asymptomatic PAD, blood viscosity (at high shear rate over 300 s-1, p < 0.05) and fibrinogen (p < 0.01) were independently associated with peripheral arterial narrowing [72]. A positive interaction was found between fibrinogen and smoking in the association with arterial narrowing, and plasma viscosity was also associated with claudication. The risk of claudication for patients in the upper quintile of plasma viscosity was 3.4 times greater than the risk for those in the lowest plasma viscosity quintile. The authors implicated blood rheologic factors in the pathogenesis of lower limb ischemia in the general population. The Edinburgh Artery Study also showed that plasma viscosity is a significant predictor for development of PAD over 17 years of follow-up in a population of subjects free from PAD at baseline [73].
Similarly, a study of 90 PAD patients and 180 controls showed a significant association between the highest tertiles of plasma viscosity and PAD [74••]. After adjustment for traditional vascular disease risk factors, the highest tertiles of plasma viscosity remained significantly associated with PAD. The researchers suggested that an alteration of plasma viscosity may modulate predisposition to the disease.
Hemorheologic Therapies in Peripheral Arterial Disease
Medical care for PAD patients with intermittent claudication includes a walking exercise program, smoking cessation, treatment of atherosclerosis risk factors, evaluation for associated CVD and, in some patients, drug treatment for symptomatic relief. Treatments for obesity and hypertension, as well as antiplatelet and statin therapies are often utilized to reduce the risk of secondary CVD events. When risk of limb-loss becomes substantial, interventions such as balloon angioplasty, stenting and surgical revascularization are considered for patients with critical limb ischemia. The choice of intervention is dependent on the anatomy of the stenotic or occlusive lesion; percutaneous interventions are appropriate when the lesion is focal and short but longer lesions must be treated with surgical revascularization to achieve acceptable long-term outcomes [2]. Surgical or endovascular intervention is usually reserved for patients with severe, lifestyle-limiting symptoms that do not adequately respond to more conservative management, including pharmacologic treatment.
Pharmacological Therapies
Antiplatelet drugs and cilostazol are the only pharmacologic treatments shown to be effective for patients with claudication [75•]. Cilostazol, a phosphodiesterase inhibitor with antiplatelet and vasodilator effects [76], is among the most effective drugs presently available for PAD [2, 77–80]. In a double-blind, placebo-controlled, parallel-arm trial in 37 outpatient vascular medicine clinics to evaluate the safety and efficacy of cilostazol for the treatment of intermittent claudication, 516 patients 40 years or older with a diagnosis of moderately severe chronic, stable, symptomatic intermittent claudication were randomized to receive cilostazol (50 or 100 mg bid orally) or placebo for 24 weeks. After 24 weeks, patients administered cilostazol showed increases in the mean change for pain-free walking distance by 59 % (p < 0.001) and 48 % (p < 0.001), respectively, in high-dose and low-dose cilostazol groups compared with placebo [79]. These results were corroborated by the results of subjective quality-of-life assessments and functional status.
A meta-analysis involving 2,702 patients with stable, moderate-to-severe claudication enrolled in eight randomized, double-blind, placebo-controlled trials examined the effect of cilostazol treatment (50-100 mg daily over 12-24 weeks) on pain-free and maximal walking distance and quality of life measures. Cilostazol therapy was reported to increase maximal and pain-free walking distances by 50 % and 67 %, respectively. In an analysis of subgroups, cilostazol was shown to increase pain-free and maximal walking distance similarly in men and women, in both older (≥65 years) and younger patients, as well as in patients with and without diabetes [76]. Cilostazol has also been observed to reduce triglyceride concentrations by 16 % and elevate HDL cholesterol by 13 % [48].
In a randomized controlled trial to evaluate the relative efficacy and safety of cilostazol and pentoxifylline in PAD patients with moderate-to-severe claudication from 54 outpatient vascular clinics, there were 922 consenting patients. There were 698 who met the inclusion criteria and were randomly assigned to blinded treatment with either cilostazol (100 mg orally twice a day), pentoxifylline (400 mg orally 3 times a day), or placebo. After 24 weeks of treatment, mean maximal walking distance increased by 107 meters (a 54 % increase from baseline) in the cilostazol group, significantly more than the 64-meter improvement (a 30 % percent increase) with pentoxifylline (p < 0.001), which was similar to that in the placebo group (65 meters, a 34 % percent increase) [80, 81]. Cilostazol was significantly more effective than pentoxifylline or placebo for increasing walking distance in PAD patients with intermittent claudication but also associated with a greater frequency of side effects.
In a retrospective meta-analysis of the data that involved 1,751 patients pooled from six randomized, double-blind, placebo-controlled studies, patients were assessed as to whether or not cilostazol (50 or 100 mg bid for 12, 16, or 24 weeks) improved treadmill and community-based walking ability and health-related quality of life in patients with intermittent claudication resulting from PAD [82]. The mean age of the patients was 65 ± 9 years. All subjects had a history of PAD for at least six months and an ABI of 0.90 or less. Maximal treadmill walking distance and health-related quality of life improved significantly with cilostazol treatment compared with placebo (p < 0.0001 for both assessments).
In the only study investigating the rheologic effects of cilostazol, a reduction in blood viscosity, measured using a cone-and-plate viscometer, was not observed [83].
Pentoxifylline is a xanthine derivative that appears to improve erythrocyte deformability and lower fibrinogen, with mild platelet anti-aggregatory effects [2]. In an earlier 8-week randomized double-blind trial with 60 PAD patients (Fontaine stage II or III), patients receiving pentoxifylline (400 mg) demonstrated a mean improvement in walking distance of 47 % (p ≤ 0.05) as compared with patients administered nylidrin, a vasodilator. This effect was attributed to reductions in blood viscosity and improved erythrocyte fluidity, suggesting that pentoxifylline counteracts tissue hypoxia in the capillaries, increasing perfusion and enabling patients to tolerate increased exercise [84].
A study of 30 patients with severe PAD reported significant improvements in absolute walking distance and relief from resting pain after pentoxifylline (600 mg) treatment over three weeks with parallel improvements in erythrocyte aggregation and filterability [71]. Although pentoxifylline is considered by some to be a viscosity-lowering therapy, there are conflicting reports on this effect. Pentoxifylline has been shown in five different peer-reviewed studies to reduce blood viscosity [85–89]. In five other peer-reviewed studies, pentoxifylline was demonstrated to increase blood viscosity or have no effect on viscosity [83, 90–93].
Dormandy et al., studied the efficacy of clofibrate (2 g daily) in 62 PAD patients with intermittent claudication over a minimum of six months. Clofibrate was associated with a steep and sustained fall in blood viscosity measured over a wide range of shear rates (0.77, 2.62 23, 230 s-1) with an average viscosity reduction of 34 % when measured at a low shear rate of 0.77 s-1 (p < 0.05) and an associated 21.4 % reduction in mean plasma-fibrinogen levels from 420 at baseline to 330 mg/dL (p < 0.01) [66]. An increased proportion of patients on treatment showed evidence of clinical improvement.
In a randomized controlled trial of atorvastatin (10 or 80 mg per day) in 354 patients with intermittent claudication attributable to PAD, pain-free walking time increased by 90 ± 18 s after 12 months of high-dose treatment compared with placebo (p = 0.025) [94]. As atorvastatin has been reported to reduce blood viscosity in observational studies [95, 96], we speculate that increases in pain-free walking time with atorvastatin therapy may be linked with improvements in ESS at the lower extremities. Increased pain-free walking times were observed after 12 months of therapy with atorvastatin [94], whereas similar improvements by pentoxifylline and cilostazol was observed in a timescale of weeks instead of months [81, 82]. Statin therapy has been shown to increase endothelium-dependent vasodilation [97], which reduces vascular resistance and, thereby, increases blood flow through collateral vessels of the lower extremities.
Ticlopidine, a thienopyridine, was shown to lower values of fibrinogen (p < 0.05), hematocrit (p < 0.05), and blood viscosity at high and low shear rates (p < 0.01) as compared with placebo in a randomized controlled trial of 44 PAD patients with intermittent claudication [98]. Patients received ticlopidine treatment (250 mg bid) for 21 months. In addition to the known antiplatelet activity of the drug, the effects of ticlopidine observed on fibrinogen and blood viscosity were suggested as possible contributors to clinical improvements reported in the larger group of claudicants to which this substudy group belonged [98]. In contrast to this report, a smaller randomized controlled study of 16 patients with intermittent claudication showed that three years of ticlopidine therapy had no significant effect on blood viscosity as compared with placebo [99].
Hemodilution Therapy
Ernst et al. [53] investigated the efficacy of isovolemic hemodilution (replacing 500-mL blood with 10 % hydroxyethyl starch HES-200) in 24 men who had stable claudication with long, collateralized femoro-popliteal obstructions in a double-blind, placebo-controlled, crossover study. Three weeks of hemodilution lowered hematocrit by a mean of 14 % (p < 0.01) and blood viscosity measured at a high shear rate of 94.5 s-1 by a mean of 11 % (p < 0.05). Hemodilution also increased resting blood flow by a mean of 15 % (p < 0.01) and pain-free walking distance by 50 % (p < 0.01) [53]. In contrast, sham therapy produced no such favorable changes. Since hemodilution reduces both hematocrit and blood viscosity, a precondition for effective enhancement of perfusion is that the viscosity effect outweighs that of hematocrit, which would be expected in patients with low or oscillatory ESS in the peripheral arteries. Although hemodilution therapy is time-consuming and considered by many to be outdated, this treatment modality should be revisited, especially in cases with multiple, long collateralized vascular obstructions and could be expected to have a profound effect on ESS.
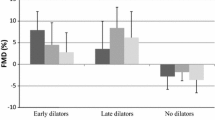
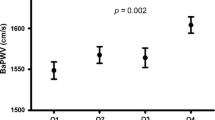
More recently, Kim et al. [100••] investigated whether or not isovolemic hemodilution could reduce the rate of major amputations in 28 critical limb ischemia patients, who had tissue loss of Rutherford Grade III, Category 5 or 6. The subjects were divided into two arms: standard of care (n = 15) and hemodilution (n = 13). Weekly isovolemic hemodilution was performed over four consecutive weeks, replacing 250 mL of whole blood with hydroxyethyl starch solution. Mean hematocrit and low shear blood viscosity levels (measured at a shear rate of 1 s-1) both decreased over four weeks of hemodilution. The hematocrit-to-viscosity ratio increased by 50 % to 60 % with hemodilution, suggesting an overall improvement of perfusion. No sham therapy was used, and the average rate of major lower extremity amputations with standard of care was 93 % (14 of 15), as compared with 31 % for patients undergoing lower extremity amputation after hemodilution (4 of 13) (p = 0.001). The average time-to-amputation was 2.7 ± 3.5 months with standard care and 11.1 ± 13.0 months with hemodilution (p = 0.004). Isovolemic hemodilution treatment of PAD patients with end-stage limb ischemia was reported to be well-tolerated and sharply reduced the rate of major amputations resulting from the deterioration of critical limb ischemia.
Conclusions
Although atherosclerosis is conventionally attributed to systemic risk factors such as hypertension, hypercholesterolemia and diabetes, focal endothelial injury and dysfunction from oscillatory or low endothelial shear stress (ESS) are well-known to occur primarily at bifurcations or along the inner wall of curved vessels. Accordingly, the tortuosity and curvature in femoral arteries amplify the injurious effect of ESS. Among the variables determining ESS, blood viscosity has to date been the most overlooked by clinical researchers. Blood viscosity is a laboratory assessment that is minimally invasive and modifiable using pharmacologic therapy as well as by hemodilution. We propose that incorporation of patient-specific blood viscosity profiles may be able to enhance the emerging field of ESS research. In addition, both blood viscosity and ESS assessments have the potential to provide clinically relevant insights into the mechanism of existing and new PAD therapies. Additional clinical research is needed to determine whether or not blood viscosity monitoring and ESS assessment can be used to stratify PAD patients or for diagnostic targeting in the treatment of PAD, claudication and limb ischemia.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States results from the National Health and Nutrition Examination Survey, 1999–2000. Circulation. 2004;110(6):738–43.
Ouriel K. Peripheral arterial disease. Lancet. 2001;358(9289):1257–64.
Golomb BA, Dang TT, Criqui MH. Peripheral arterial disease morbidity and mortality implications. Circulation. 2006;114(7):688–99.
Pasqualini L, Schillaci G, Vaudo G, Innocente S, Ciuffetti G, Mannarino E. Predictors of overall and cardiovascular mortality in peripheral arterial disease. Am J Cardiol. 2001;88(9):1057–60.
Criqui MH, Langer RD, Fronek A, Feigelson HS, Klauber MR, McCann TJ, et al. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med. 1992;326(6):381–6.
Joosten MM, Pai JK, Bertoia ML, Rimm EB, Spiegelman D, Mittleman MA, et al. Associations between conventional cardiovascular risk factors and risk of peripheral artery disease in men. JAMA. 2012;308(16):1660–7. The study reported that in male PAD patients, smoking, hypertension, hypercholesterolemia, and type 2 diabetes account for the majority of risk associated with development of clinically significant PAD.
Moyer VA. Screening for peripheral artery disease and cardiovascular disease risk assessment with the ankle–brachial index in adults: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159(5):342–8. This study reviewed the evidence on the use of resting ankle-brachial index (ABI) as a screening test for PAD or as a risk predictor for cardiovascular disease (CVD) and concluded that the current evidence is insufficient to assess the balance of benefits and harms of screening for PAD and CVD risk assessment with the ABI in adults.
Malek AM, Alper SL, Izumo S. Hemodynamic shear stress and its role in atherosclerosis. JAMA. 1999;282(21):2035–42. This classic study identified hemodynamic shear stress as an important determinant of endothelial function and phenotype. Arterial-level shear stress (>15 dyne/cm2) induces endothelial quiescence and an atheroprotective gene expression profile, while low shear stress (<4 dyne/cm2), which is prevalent at atherosclerosis-prone sites, stimulates an atherogenic phenotype.
Zarins CK, Giddens DP, Bharadvaj B, Sottiurai VS, Mabon RF, Glagov S. Carotid bifurcation atherosclerosis. Quantitative correlation of plaque localization with flow velocity profiles and wall shear stress. Circ Res. 1983;53(4):502–14.
Davies PF. Hemodynamic shear stress and the endothelium in cardiovascular pathophysiology. Nat Clin Pract Cardiovasc Med. 2009;6(1):16–26.
Langille BL, O'Donnell F. Reductions in arterial diameter produced by chronic decreases in blood flow are endothelium-dependent. Science. 1986;231(4736):405–7.
Fukumoto Y, Hiro T, Fujii T, Hashimoto G, Fujimura T, Yamada J, et al. Localized elevation of shear stress is related to coronary plaque rupture: a 3-dimensional intravascular ultrasound study with in-vivo color mapping of shear stress distribution. J Am Coll Cardiol. 2008;51(6):645–50.
Tricot O, Mallat Z, Heymes C, Belmin J, Leseche G, Tedgui A. Relation between endothelial cell apoptosis and blood flow direction in human atherosclerotic plaques. Circulation. 2000;101(21):2450–3.
DePaola N, Gimbrone M, Davies PF, Dewey C. Vascular endothelium responds to fluid shear stress gradients. Arterioscler Thromb Vasc Biol. 1992;12(11):1254–7.
Schirmer CM, Malek AM. Estimation of wall shear stress dynamic fluctuations in intracranial atherosclerotic lesions using computational fluid dynamics. Neurosurgery. 2008;63(2):326–34.
White CR, Frangos JA. The shear stress of it all: the cell membrane and mechanochemical transduction. Philos Trans R Soc Lond B Biol Sci. 2007;362(1484):1459–67.
Chachisvilis M, Zhang YL, Frangos JA. G protein-coupled receptors sense fluid shear stress in endothelial cells. Proc Natl Acad Sci. 2006;103(42):15463–8.
Eng E, Ballermann BJ. Diminished NF-kappaB activation and PDGF-B expression in glomerular endothelial cells subjected to chronic shear stress. Microvasc Res. 2003;65(3):137–44.
Li YS, Haga JH, Chien S. Molecular basis of the effects of shear stress on vascular endothelial cells. J Biomech. 2005;38(10):1949–71.
Malek AM, Jiang L, Lee I, Sessa WC, Izumo S, Alper SL. Induction of nitric oxide synthase mRNA by shear stress requires intracellular calcium and G-protein signals and is modulated by PI 3 kinase. Biochem Biophys Res Commun. 1999;254(1):231–42.
Dardik A, Chen L, Frattini J, Asada H, Aziz F, Kudo FA, et al. Differential effects of orbital and laminar shear stress on endothelial cells. J Vasc Surg. 2005;41(5):869–80.
Dardik A, Yamashita A, Aziz F, Asada H, Sumpio BE. Shear stress-stimulated endothelial cells induce smooth muscle cell chemotaxis via platelet-derived growth factor-BB and interleukin-1 [alpha]. J Vasc Surg. 2005;41(2):321–31.
Glagov S, Zarins C, Giddens DP, Ku DN. Hemodynamics and atherosclerosis. Insights and perspectives gained from studies of human arteries. Arch Pathol Lab Med. 1988;112(10):1018–31.
Chatzizisis YS, Jonas M, Coskun AU, Beigel R, Stone BV, Maynard C, et al. Prediction of the localization of high-risk coronary atherosclerotic plaques on the basis of low endothelial shear stress: an intravascular ultrasound and histopathology natural history study. Circulation. 2008;117(8):993–1002.
Groen HC, Gijsen FJ, van der Lugt A, Ferguson MS, Hatsukami TS, van der Steen AF, et al. Plaque rupture in the carotid artery is localized at the high shear stress region: a case report. Stroke. 2007;38(8):2379–81.
Stone PH, Saito S, Takahashi S, Makita Y, Nakamura S, Kawasaki T, et al. Prediction of progression of coronary artery disease and clinical outcomes using vascular profiling of endothelial shear stress and arterial plaque characteristics the PREDICTION study. Circulation. 2012;126(2):172–81. Although the PREDICTION study focused on endothelial shear stress in the coronary arteries and not peripheral, it demonstrated clear correlation between plaque progressions and low endothelial shear stress. Like many other shear stress studies, blood viscosity was assumed to be a constant Newtownian value. However, the relationship between plaque growth and shear stress is noteworthy.
Friedman MH, Bargeron CB, Deters OJ, Hutchins GM, Mark FF. Correlation between wall shear and intimal thickness at a coronary artery branch. Atherosclerosis. 1987;68(1–2):27–33.
Stone PH, Coskun AU, Kinlay S, Clark ME, Sonka M, Wahle A, et al. Effect of endothelial shear stress on the progression of coronary artery disease, vascular remodeling, and in-stent restenosis in humans in vivo 6-month follow-up study. Circulation. 2003;108(4):438–44.
Hayase H, Tokunaga K, Nakayama T, Sugiu K, Nishida A, Arimitsu S, et al. Computational fluid dynamics of carotid arteries after carotid endarterectomy or carotid artery stenting based on postoperative patient-specific computed tomography angiography and ultrasound flow data. Neurosurgery. 2011;68(4):1096–101; discussion 1101. The study compared the postoperative rheological conditions after CAS with those after CEA with patch angioplasty (patch CEA) through the use of computational fluid dynamics (CFD) based on patient-specific data. Rotational slow flow was observed in the internal carotid artery bulb after patch CEA. ESS analysis found regional low ESS near the outer wall of the bulb.
Groen HC, Simons L, van den Bouwhuijsen QJ, Bosboom EM, Gijsen FJ, van der Giessen AG, et al. MRI-based quantification of outflow boundary conditions for computational fluid dynamics of stenosed human carotid arteries. J Biomech. 2010;43(12):2332–8.
Papathanasopoulou P, Zhao S, Kohler U, Robertson MB, Long Q, Hoskins P, et al. MRI measurement of time-resolved wall shear stress vectors in a carotid bifurcation model, and comparison with CFD predictions. J Magn Reson Imaging. 2003;17(2):153–62.
Schirmer CM, Malek AM. Wall shear stress gradient analysis within an idealized stenosis using non-Newtonian flow. Neurosurgery. 2007;61(4):853–63.
Schirmer CM, Malek AM. Prediction of complex flow patterns in intracranial atherosclerotic disease using computational fluid dynamics. Neurosurgery. 2007;61(4):842–51, discussion 852.
Takeuchi S, Karino T. Flow patterns and distributions of fluid velocity and wall shear stress in the human internal carotid and middle cerebral arteries. World Neurosurg. 2010;73(3):174–85, discussion e127.
Younis HF, Kaazempur-Mofrad MR, Chan RC, Isasi AG, Hinton DP, Chau AH, et al. Hemodynamics and wall mechanics in human carotid bifurcation and its consequences for atherogenesis: investigation of inter-individual variation. Biomech Model Mechanobiol. 2004;3(1):17–32.
Galizia MS, Barker A, Liao Y, Collins J, Carr J, McDermott MM, et al. Wall morphology, blood flow and wall shear stress: MR findings in patients with peripheral artery disease. Eur Radiol. 2013:(In press). The clinical study demonstrated the feasibility of combining multi-contrast morphological imaging of the peripheral arterial wall with PC-MRI with three-directional velocity encoding. Velocities, oscillatory shear stress and total flow were similar between patients with normal arteries and wall thickening/plaque. Patients with plaques demonstrated regionally increased peak systolic WSS and enhanced WSS eccentricity.
Smedby O, Nilsson S, Bergstrand L. Development of femoral atherosclerosis in relation to flow disturbances. J Biomech. 1996;29(4):543–7.
Smedby O, Johansson J, Molgaard J, Olsson AG, Walldius G, Erikson U. Predilection of atherosclerosis for the inner curvature in the femoral artery. A digitized angiography study. Arterioscler Thromb Vasc Biol. 1995;15(7):912–7.
Smedby O, Bergstrand L. Tortuosity and atherosclerosis in the femoral artery: what is cause and what is effect? Ann Biomed Eng. 1996;24(4):474–80.
Wood NB, Zhao SZ, Zambanini A, Jackson M, Gedroyc W, Thom SA, et al. Curvature and tortuosity of the superficial femoral artery: a possible risk factor for peripheral arterial disease. J Appl Physiol (1985). 2006;101(5):1412–8.
Ku DN, Giddens DP, Zarins CK, Glagov S. Pulsatile flow and atherosclerosis in the human carotid bifurcation. Positive correlation between plaque location and low oscillating shear stress. Arterioscler Thromb Vasc Biol. 1985;5(3):293–302.
Wensing PJ, Meiss L, Mali WP, Hillen B. Early atherosclerotic lesions spiraling through the femoral artery. Arterioscler Thromb Vasc Biol. 1998;18(10):1554–8.
Tarbell JM. Mass transport in arteries and the localization of atherosclerosis. Annu Rev Biomed Eng. 2003;5(1):79–118.
Scholten FG, Warnars GA, Mali WPTM, van Leeuwen MS. Femoropopliteal occlusions and the adductor canal hiatus, Duplex study. Eur J Vasc Surg. 1993;7(6):680–3.
Magid R, Murphy TJ, Galis ZS. Expression of matrix metalloproteinase-9 in endothelial cells is differentially regulated by shear stress. Role of c-Myc. J Biol Chem. 2003;278(35):32994–9.
Rosenson R. Viscosity and ischemic heart disease. J Vasc Med Biol. 1993;4:206.
Cocklet GR, Meiselman HJ. Macro- and micro-rheological properties of blood. In: Baskurt OK HM, Rampling MW, Meiselman HJ, editors. Handbook of hemorheology and hemodynamics. Amsterdam: IOS Press; 2007. p. 45–71.
Stoltz JF, Singh M, Riha P. Hemorheology in practice. Wahington DC: IOS Press; 1999.
Chien S. Determinants of blood viscosity and red cell deformability. Scand J Clin Lab Investig. 1981;41(S156):7–12.
Baskurt OK, Meiselman HJ. Erythrocyte aggregation: Basic aspects and clinical importance. Clin Hemorheol Microcirc. 2013;53(1):23–37. The study by two leading rheology researchers articulates that the extent of aggregation of erythrocytes is the main determinant of low shear blood viscosity. A detailed understanding of aggregation effects is important from a clinical point of view because red blood cell aggregation is increased during a variety of pathophysiological processes, including infections, circulatory and metabolic disorders, hematological pathologies and several other disease states.
Kwaan HC. Role of plasma proteins in whole blood viscosity: a brief clinical review. Clin Hemorheol Microcirc. 2010;44(3):167–76.
Guyton AC, Hall JE. Textbook of medical physiology (Guyton physiology). 10th ed. Philadelphia: Saunders; 2000.
Ernst E, Matrai A, Kollar L. Placebo-controlled, double-blind study of haemodilution in peripheral arterial disease. Lancet. 1987;1(8548):1449–51.
Pulanic D, Rudan I. The past decade: fibrinogen. Coll Antropol. 2005;29(1):341–9.
Baskurt OK, Meiselman HJ. Blood rheology and hemodynamics. Semin Thromb Hemost. 2003;29(5):435–50.
Fantl P, Ward HA. Molecular weight of human fibrinogen derived from phosphorus determinations. Biochem J. 1965;96(3):886–9.
Fung YC. Biomechanics. New York: Spriner-Verlag; 1981.
Sloop GD, Mercante DE. Opposite effects of low-density and high-density lipoprotein on blood viscosity in fasting subjects. Clin Hemorheol Microcirc. 1998;19(3):197–203.
Stamos TD, Rosenson RS. Low high density lipoprotein levels are associated with an elevated blood viscosity. Atherosclerosis. 1999;146(1):161–5.
Slyper A, Le A, Jurva J, Gutterman D. The influence of lipoproteins on whole-blood viscosity at multiple shear rates. Metabolism. 2005;54(6):764–8.
Lowe GD, Rumley A, Norrie J, Ford I, Shepherd J, Cobbe S, et al. Blood rheology, cardiovascular risk factors, and cardiovascular disease: the West of Scotland Coronary Prevention Study. Thromb Haemost. 2000;84(4):553–8.
Rosenson RS, McCormick A, Uretz EF. Distribution of blood viscosity values and biochemical correlates in healthy adults. Clin Chem. 1996;42(8 Pt 1):1189–95.
Rosenson RS, Shott S, Tangney CC. Hypertriglyceridemia is associated with an elevated blood viscosity: triglycerides and blood viscosity. Atherosclerosis. 2002;161(2):433–9.
Seplowitz AH, Chien S, Smith FR. Effects of lipoproteins on plasma viscosity. Atherosclerosis. 1981;38(1):89–95.
Leonhardt H, Arntz HR, Klemens UH. Studies of plasma viscosity in primary hyperlipoproteinemia. Atherosclerosis. 1977;28:29–40.
Dormandy JA, Gutteridge JM, Hoare E, Dormandy TL. Effect of clofibrate on blood viscosity in intermittent claudication. Br Med J. 1974;4(5939):259–62.
Weiss N. Lipid apheresis and rheopheresis for treatment of peripheral arterial disease. Atheroscler Suppl. 2009;10(5):62–9.
Dormandy J, Hoare E, Khattab A, Arrowsmith D, Dormandy T. Prognostic significance of rheological and biochemical findings in patients with intermittent claudication. Br Med J. 1973;4(5892):581–3.
Dormandy JA, Hoare E, Colley J, Arrowsmith DE, Dormandy TL. Clinical, haemodynamic, rheological, and biochemical findings in 126 patients with intermittent claudication. Br Med J. 1973;4(5892):576–81.
Dormandy JA, Hoare E, Postlethwaite J. Importance of blood viscosity. Rheological claudication. Proc R Soc Med. 1974;67(6 Pt 1):446–7.
Angelkort B, Spurk P, Habbaba A, Mahder M. Blood flow properties and walking performance in chronic arterial occlusive disease. Angiology. 1985;36(5):285–92.
Lowe GD, Fowkes FG, Dawes J, Donnan PT, Lennie SE, Housley E. Blood viscosity, fibrinogen, and activation of coagulation and leukocytes in peripheral arterial disease and the normal population in the Edinburgh Artery Study. Circulation. 1993;87(6):1915–20.
Tzoulaki I, Murray GD, Lee AJ, Rumley A, Lowe GD, Fowkes FG. Inflammatory, haemostatic, and rheological markers for incident peripheral arterial disease: Edinburgh Artery Study. Eur Heart J. 2007;28(3):354–62.
Ricci I, Sofi F, Liotta AA, Fedi S, Macchi C, Pratesi G, et al. Alterations of haemorheological parameters in patients with peripheral arterial disease. Clin Hemorheol Microcirc. 2013;55(2):271–6. This recent clinical study of 90 PAD patients and 180 control subjects showed a significant association between the highest tertiles of plasma viscosity and PAD.
Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss L, et al. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA Guideline Recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(14):1555–70. The most recent practice guidelines for the management of patients with peripheral artery disease highlighted cilostazol and antiplatelet drug therapy as the only pharmacologic treatments clearly shown to be effective for PAD patients with claudication.
Thompson PD, Zimet R, Forbes WP, Zhang P. Meta-analysis of results from eight randomized, placebo-controlled trials on the effect of cilostazol on patients with intermittent claudication. Am J Cardiol. 2002;90(12):1314–9.
Elam M, Heckman J, Crouse J, Hunninghake D, Herd J, Davidson M, et al. Effect of the novel antiplatelet agent cilostazol on plasma lipoproteins in patients with intermittent claudication. Arterioscler Thromb Vasc Biol. 1998;18(12):1942–7.
Money SR, Herd JA, Isaacsohn JL, Davidson M, Cutler B, Heckman J, et al. Effect of cilostazol on walking distances in patients with intermittent claudication caused by peripheral vascular disease. J Vasc Surg. 1998;27(2):267–75.
Beebe HG, Dawson DL, Cutler BS, Herd JA, Strandness Jr DE, Bortey EB, et al. A new pharmacological treatment for intermittent claudication: results of a randomized, multicenter trial. Arch Intern Med. 1999;159(17):2041–50.
Dawson DL, Cutler BS, Meissner MH, Strandness DE. Cilostazol has beneficial effects in treatment of intermittent claudication results from a multicenter, randomized, prospective, double-blind trial. Circulation. 1998;98(7):678–86.
Dawson DL, Cutler BS, Hiatt WR, Hobson II RW, Martin JD, Bortey EB, et al. A comparison of cilostazol and pentoxifylline for treating intermittent claudication. Am J Med. 2000;109(7):523–30.
Regensteiner JG, Ware JE, McCarthy WJ, Zhang P, Forbes WP, Heckman J, et al. Effect of cilostazol on treadmill walking, community‐based walking ability, and health‐related quality of life in patients with intermittent claudication due to peripheral arterial disease: meta‐analysis of six randomized controlled trials. J Am Geriatr Soc. 2002;50(12):1939–46.
Dawson DL, Zheng Q, Worthy SA, Charles B, Bradley Jr DV. Failure of pentoxifylline or cilostazol to improve blood and plasma viscosity, fibrinogen, and erythrocyte deformability in claudication. Angiology. 2002;53(5):509–20.
Accetto B. Beneficial hemorheologic therapy of chronic peripheral arterial disorders with pentoxifylline: results of double-blind study versus vasodilator-nylidrin. Am Heart J. 1982;103(5):864–9.
Berman W, Berman N, Pathak D, Wood S. Effects of pentoxifylline (Trental) on blood flow, viscosity, and oxygen transport in young adults with inoperable cyanotic congenital heart disease. Pediatr Cardiol. 1994;15(2):66–70.
Di Perri T, Carandente O, Vittoria A, Guerrini M, Messa GL. Studies of the clinical pharmacology and therapeutic efficacy of pentoxifylline in peripheral obstructive arterial disease. Angiology. 1984;35(7):427–35.
Perego M, Sergio G, Artale F, Giunti P, Danese C. Haemorrheological improvement by pentoxifylline in patients with peripheral arterial occlusive disease. Curr Med Res Opin. 1986;10(2):135–8.
Solerte SB, Fioravanti M, Cerutti N, Severgnini S, Locatelli M, Pezza N, et al. Retrospective analysis of long-term hemorheologic effects of pentoxifylline in diabetic patients with angiopathic complications. Acta Diabetol. 1997;34(2):67–74.
Sonkin P, Sinclair S, Hatchell D. The effect of pentoxifylline on retinal capillary blood flow velocity and whole blood viscosity. Am J Ophthalmol. 1993;115(6):775–80.
Billett H, Kaul D, Connel M, Fabry M, Nagel R. Pentoxifylline (Trental) has no significant effect on laboratory parameters in sickle cell disease. Nouv Rev Fr Hématol. 1989;31(6):403–7.
Karandashov V, Petukhov E, Zrodnikov V. Effects of pentoxifylline drugs and UV photohemotherapy on blood viscosity. Bull Exp Biol Med. 1998;126(5):1155–6.
Perhoniemi V, Salmenkivi K, Sundberg S, Johnsson R, Gordin A. Effects of flunarizine and pentoxifylline on walking distance and blood rheology in claudication. Angiology. 1984;35(6):366–72.
Reilly D, Quinton D, Barrie W. A controlled trial of pentoxifylline (Trental 400) in intermittent claudication: clinical, haemostatic and rheological effects. N Z Med J. 1987;100(828):445–7.
Mohler ER, Hiatt WR, Creager MA. Cholesterol reduction with atorvastatin improves walking distance in patients with peripheral arterial disease. Circulation. 2003;108(12):1481–6.
Banyai S, Banyai M, Falger J, Jansen M, Alt E, Derfler K, et al. Atorvastatin improves blood rheology in patients with familial hypercholesterolemia (FH) on long-term LDL apheresis treatment. Atherosclerosis. 2001;159(2):513–9.
Empen K, Geiss HC, Lehrke M, Otto C, Schwandt P, Parhofer KG. Effect of atorvastatin on lipid parameters, LDL subtype distribution, hemorrheological parameters and adhesion molecule concentrations in patients with hypertriglyceridemia. Nutr Metab Cardiovasc Dis. 2003;13(2):87–92.
Plutzky J. Effect of lipid-lowering therapy on vasomotion and endothelial function. Curr Cardiol Rep. 1999;1(3):238–43.
Palareti G, Poggi M, Torricelli P, Balestra V, Coccheri S. Long-term effects of ticlopidine on fibrinogen and haemorheology in patients with peripheral arterial disease. Thromb Res. 1988;52(6):621–9.
Fagher B, Persson S, Persson G, Larsson H. Blood viscosity during long-term treatment with ticlopidine in patients with intermittent claudication. A double-blind study. Angiology. 1993;44(4):300–6.
Kim D, Cho DJ, Kim YB, Cho YI. Reduced amputation rate with hemorheological therapy in critical limb ischemia patients. Clin Hemorheol Microcirc. 2014;(In press). This observational clinical study demonstrated that weekly isovolemic hemodilution performed over four consecutive weeks reduced mean hematocrit and low shear blood viscosity levels, resulting in an overall improvement of perfusion. The average rate of major lower extremity amputations with standard of care was 93 % (14 of 15), as compared with 31 % of patients undergoing lower extremity amputation after hemodilution (4 of 13) (p = 0.001).
Compliance with Ethics Guidelines
Conflict of Interest
Robert S. Rosenson received honoraria from Aegerion, Amgen, GSK, Janssen, LipoScience, Novartis, Regeneron, and Sanofi; and received royalties from UpToDate.
Young I Cho and Daniel J. Cho declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Vascular Biology
Rights and permissions
About this article
Cite this article
Cho, Y.I., Cho, D.J. & Rosenson, R.S. Endothelial Shear Stress and Blood Viscosity in Peripheral Arterial Disease. Curr Atheroscler Rep 16, 404 (2014). https://doi.org/10.1007/s11883-014-0404-6
Published:
DOI: https://doi.org/10.1007/s11883-014-0404-6