Abstract
MicroRNAs (miRNAs) are a class of post-transcriptional regulators that provide a mechanism of gene silencing by translational repression or degradation of the targeted gene. Gene expression regulation by miRNAs is involved in most if not all physiological and pathophysiological processes. Atherosclerosis is a major cardiovascular disease pathology regulated by miRNAs. Recent miRNA profiling studies have implicated the potential use of miRNAs as biomarkers in patients with atherosclerosis, as both diagnostic and prognostic indicators. This review will discuss the clinical and basic science research information that has been gleaned regarding miRNA roles in dyslipidemia, diabetes, obesity, and insulin resistance which are the major stimulators for the development of atherosclerosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most experts credit Victor Amboros and associates for the initiation of the microRNA (miRNA) era over 20 years ago, with the discovery of miRNA in C. elegans [1]. Since that first observation, others have added the necessary components to translate the field into the clinical arena with the identification of biomarkers that reflect pathology, the development of pharmaceutical agents that target specific miRNAs, and the further elucidation of miRNA biological effects [2•]. Currently, websites like (www.microrna.org and www.mirbase.org) are increasing the knowledge base for translational research by providing an organized compilation of results. The regulation of gene expression by miRNAs is complex. For example, one miRNA may regulate several hundred target genes, and currently approximately 1,100 miRNAs in the human genome and about 700 miRNAs in mice have been identified. Because miRNA has a very important function in regulating the production of proteins and is a significant coordinator of biological functions, miRNAs are a potentially viable source of biomarkers for diagnosing atherosclerosis disease states, identifying drug targets, or assessing treatment efficacy.
In this review, we summarize current knowledge on miRNA influences on atherosclerosis.
What are miRNAs?
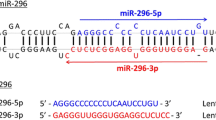
MiRNAs are a class of post-transcriptional regulators found in the nucleus that have complementary sequences within mRNA molecules, usually resulting in gene silencing by translational repression or target degradation. MiRNAs are originally transcribed from the cell genome by RNA polymerase, forming large pre-miRNA transcripts. These pre-miRNAs are managed in the nucleus by RNase III enzyme (Dorsha), and the pre-miRNAs are exposed to the cytoplasm. In the cytoplasm, pre-miRNAs are broken down to generate mature miRNA duplexes. These mature miRNAs are combined into RNA-induced silencing complexes (RISC) to the target mRNAs. In this way, miRNAs induce transcriptional repression or target mRNA degradation. How transcriptional regulators affect miRNA expression to alter gene regulation and modulate biological functions is shown in Fig. 1.
Atherosclerosis and miRNAs
Atherosclerosis continues to be one of the most important areas of cardiovascular (CV) research. As an inflammatory disease, this is manifested by increased oxidative stress leading to endothelial dysfunction and, over time, increased atherosclerosis. As a consequence, one finds infiltration of leukocytes and a deposition of modified lipoproteins, resulting in the development of foam cells. The cytotoxic effects of oxidized low-density lipoprotein (LDL) initiate further accumulation of leukocytes, the secretion of cytokines and growth factors, which accelerate the inflammatory response. Atherosclerotic lesions develop, followed by apoptosis, the formation of a necrotic core, the proliferation of vascular smooth muscle cells (VSMCs), and enhanced extracellular matrix formation leads to the narrowing of the artery lumen with amplified pro-atherothrombotic potential. The fibrous cap covering the necrotic core of the plaque can erode or rupture, and initiate the formation of a pro-thrombotic state cumulating into the occlusion of arteries and cardiovascular ischemia.
Recently, Raitoharju and associates completed miRNA expression profiles on human tissue from the Tampere Vascular Study [3•]. Samples from human atherosclerotic plaques were compared to non-atherosclerotic left internal thoracic arteries. A total of 12 atherosclerotic plaques were obtained from aortic, carotid, and femoral atherosclerotic arteries for comparison. The analyses were performed using Agilent’s miRNA microarray platform. The study population presented with 70 % having hypertension, 80 % dyslipidemia, and 80 % were smokers and had an average body mass index (BMI) of 25.1. Compared to controls, the carotid artery samples had significant increases in miRNA-21, 34a, and 210. The largest miRNA signal from carotids came from miRNA 210 (p < 0.004). The femoral artery miRNA samples found the highest signal from miRNA 21 followed by miRNA-146b, -146a, -210 and -34a (P < 0.002). Comparisons with aorta samples were similar to the femoral artery vs. control left internal thoracic artery.
Translational implications of these changes can be illustrated by significant down-regulation of predicted targets of miRNA-21, -34a, -146a, -146b-5p. The known atherosclerotic related function of miRNA-21 is related to vascular smooth muscle cell (VSMC) function, inhibition of matrix metalloproteinases (MMPs), and proliferation of VSMC [4]. MiRNA-34a showed a significant relationship with VSMC proliferation, and HDL levels in genome-wide association analysis from the Framingham heart study [5]. MiRNA 146a interactions with SORT1 regulating liver lipoprotein export and has been related to the risk of coronary artery disease (CAD) and LDL release [6]. MMPs contribute to atherosclerotic plaque progression and destabilization, which further causes plaque rupture. Oxidized LDL, which plays a pivotal role in atherosclerosis, is reported to increase miRNA-29b expression, resulting in increase in VSMC migration through MMP-2 and MMP-9 upregulation. This effect is mediated by the downregulation of DNA methyltransferase 3b (DNMT3b) [7•]. In addition, Yuan et al. found the association between 3’-UTR polymorphisms in MMP-9 contributes to the risk for atherosclerotic cerebral infarction [8]. In summary, miRNA expression profiling shows significant differences in atherosclerotic vessels vs. controls.
A second important study was completed by Cipollone et al, who evaluated tissue samples from patients having carotid surgery [9•]. Two independent cohorts of atherosclerotic plaques were collected in two different Italian hospitals, Chieti Hospital and Ancona Hospital. These patients underwent carotid endarterectomy for extracranial high-grade (>70 %) internal carotid artery stenosis. Plaques were divided into two groups: symptomatic (n = 22) and asymptomatic (n =31), according to the presence or absence of stroke, respectively. They found significant differences in miRNA level of expression of five miRNAs (miRNA-100, miRNA-127, miRNA-145, miRNA-133a, and miRNA-133b) in symptomatic versus asymptomatic plaques (Table 1). In summary, this supports prior miRNA results and expands the knowledge base to the potential use of miRNAs as a biomarker in patients with carotid obstructions.
Fichtlscherer et al evaluated human miRNAs samples that were released by cultured cells and blood [10]. Using quantitative PCR, they profiled selected miRNAs in the plasma of 36 patients with coronary artery disease (CAD) that received state-of-the-art pharmacological treatment and 17 healthy volunteers. They reported significantly lower levels of miRNA-126, miRNA-17, miRNA-92a, and the inflammation-associated miR-155 in CAD patients compared with healthy controls. They concluded that circulating levels of inflammatory and vascular associated miRNA were significantly lower in patients with coronary artery disease. Clinically, it is important to recognize that miRNAs highly expressed by endothelial cells can be detected in high concentrations in the circulation. Two important features from this paper need to be highlighted. First, miRNAs that had increased expression in the vascular wall (e.g., miR-17, miR-92a or miR-126) were significantly downregulated in the circulating blood. This suggests that these miRNAs are degraded and reduced in expression, and could be taken up in diseased vessels. Secondly,, in contrast to the vascular wall miRNA levels, miRNAs that are highly expressed in cardiac muscle tend to be higher in the circulation of patients with CAD. In summary, this paper adds more information specific to stable CAD and in addition found that patients with diabetes have more marked reductions in miRNA-126, -155, and -145 than patients with CAD (Table 1).
Metabolics and miRNA
Metabolics is one of the most important areas to be addressed in risk factor modification. Treatment of hyperlipidemia patients with statins has reduced CV events and LDL in patients with hyperlipidemia. Currently, high-density lipoprotein (HDL) and reverse cholesterol transport is an area of high interest and new information from miRNA technology has made major impacts in research. The reverse cholesterol transport (RCT) system is a key in removal of cholesterol from cells. Cholesterol efflux is under the control of ATP transporters (ABCA-1, ABCG-1). The most famous of these transporters is ABCA-1 which controls HDL biogenesis in the liver. A deficiency in ABCA-1 transporter produces Tangiers disease. This results in a reduced ability to transport cholesterol out of their cells, which leads to an accumulation of cholesterol in many body tissues. In summary, reverse transport pathway involving ABC transporters hold the potential to significantly reduce generalized atherosclerosis.
miRNA research from Wang and colleagues revealed that miRNA -10b directly reduces ABCA1 and ABCG1 in human derived macrophages [11]. They reported that dietary cyanidin-3-O-β-glucoside (Cy-3-G) was metabolized into protocatechuic acid (PCA) by the gut microbiota inducing ABCA1 and ABCG1 expression in macrophages by decreasing the expression of miRNA-10b, which contributes to the accelerated macrophage RCT. In summary, miRNA-10b directly represses ABCA1 and ABCG1 and negatively regulates cholesterol efflux from human-derived macrophages.
A potential new target for atherosclerosis prevention and treatment is the human gut microbiota. Beyond the gut microbiota, Horie and associates found that miRNA-33 deficiency can reduce progression of atherosclerotic plaque in ApoE-/- mice [12]. This currently is the only in vivo study to show increased circulating HDL-cholesterol levels with reduced atherosclerotic progression. However, as pointed out by Horie et al, various genes are changed in miRNA-33-deficient mice, and more detailed research will be needed to establish miRNA-33 targeting therapy in humans.
In summary, clinical studies have discovered an important role for the intestinal microbiota in the pathogenesis of cardiovascular disease. In addition, lifestyle modification with the Mediterranean diet has shown a significant reduction in CV events [13]. Hazen et al reported that increased production of a proatherosclerotic metabolite, trimethylamine-N-oxide (TMAO) increased CV risk [14]. Diets rich in eggs, liver, beef, and pork produce phosphatidylcholine by the formation of the metabolite trimethylamine and conversion to TMAO [15]. In addition, anthocyanins (flavonoids) common byproducts of fruits are well known to have antiatherogenic effects. Two important breakdown products from anthocyanins are Cy-3-G and its metabolite protocatechuic acid. Both inhibited the development of early atherosclerosis in the apolipoprotein null (ApoE −/−) mice [16, 17].
Diabetes continues to be a major CV target for progressive atherosclerosis. The core problem of type 2 diabetes is insulin resistance and, to date, lowering blood sugar number with diabetes medications has not been shown to reduce CV events. Currently, three tissues are primarily involved in diabetes metabolism and glucose homeostasis: namely, liver, adipose tissue, and skeletal muscle. These three insulin targets were evaluated by Herrera and associates using microarrays to obtain global expression profiles of miRNA [18]. They measured the expression of 283 miRNAs in tissue from hyperglycemic (Goto–Kakizaki), intermediate glycemic (Wistar Kyoto) and normoglycemia (Brown Norway) rats (n = 5 for each strain). Their studies found increased expression patterns in miRNA-222, -27a, -195, -103 and -10b in hyperglycemic animals (Table 2). Adipocyte expression patterns of miRNA noted changes in miRNA-222, -27a and -29a. They found 112 miRNAs that affected all three areas and four miRNAs between adipose tissue and liver with only one between skeletal muscle and liver. In summary, miRNA-222 and miRNA-27a are upregulated with hyperglycemic status in adipose tissue, miRNA-195 and miRNA-103 are unregulated in liver, and miR-10b is downregulated in skeletal muscle.
Recently, miRNA-143 has been found to have adverse effects on critical glucose pathways. AKT is a known as a key step in glucose transport. Cellular research by Jordan et al using transgenic obese models found that miRNA-143 specifically inhibits insulin signaling at the level of AKT activation and the upstream receptor signaling remains undamaged (Table 2) [19•]. These opposing effects from miRNA increase the risk for diabetes.
Meerson and colleagues used microarray-based expression profiling to study biopsies from non-diabetes Pima Indians [20]. 233 miRNAs were profiled from subcutaneous abdominal adipose tissue biopsies (Table 2). The results from adipose tissue found that miRNA-221 may add to the development of the insulin resistance that characteristically accompanies obesity by affecting peroxisome proliferator-activated receptor (PPAR) signaling pathways. The strongest correlation with BMI was in women for miRNA-221 (p < .0001). On the other hand, the levels of miR-193a-3p and miR-193b-5p were negatively correlated with BMI.
In summary, miRNA research has the potential to provide important biomarkers to monitor pancreatic beta cell activity in patients with diabetes. Future studies will reveal whether it is possible to monitor miRNA-132 and -212 to tell if the beta cell is being stimulated by diabetic therapies. Agents that increase c-AMP in beta cell (e.g., DPP-IV inhibitors, GLP-1 agonists, GIP, and GPR 119) increase levels of miRNA 132 and 212 in a dose dependent fashion (Table 2). Fortunately, miRNA 132 and 212 are not affected by glucose levels, free fatty acids, insulin or beta cell function. This important area for biomarkers in medicine is at its infancy in development. Durability of medical treatment potentially could be assessed by this method.
Conclusions
miRNA metabolism has added significant clinical information involving progressive atherosclerosis. The correlations with lipids, obesity, and insulin resistance from miRNA research are intriguing and will require additional future research. For example, connecting miRNA levels to inflammation and extracellular matrix remodeling in the vessel wall may reveal novel roles for MMPs. In addition, using proteomic approaches to identify downstream targets of miRs will likely inform us about additional therapeutic targets.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Lee RC, Feinbaum RL, Ambros V. The c. Elegans heterochronic gene lin-4 encodes small rnas with antisense complementarity to lin-14. Cell. 1993;75(5):843–54.
• van Rooij E, Purcell AL, Levin AA. Developing microrna therapeutics. Circ Res. 2012;110(3):496–507. Describes potential for using miRNA for therapeutics.
• Raitoharju E, Lyytikainen LP, Levula M, Oksala N, Mennander A, Tarkka M, et al. Mir-21, mir-210, mir-34a, and mir-146a/b are up-regulated in human atherosclerotic plaques in the tampere vascular study. Atherosclerosis. 2011;219(1):211–7. Identifies particular miRNAs increased in human atherosclerosis.
Caolo V, Schulten HM, Zhuang ZW, Murakami M, Wagenaar A, Verbruggen S, et al. Soluble jagged-1 inhibits neointima formation by attenuating notch-herp2 signaling. Arterioscler Thromb Vasc Biol. 2011;31(5):1059–65.
Ma L, Yang J, Runesha HB, Tanaka T, Ferrucci L, Bandinelli S, et al. Genome-wide association analysis of total cholesterol and high-density lipoprotein cholesterol levels using the framingham heart study data. BMC Med Genet. 2010;11:55.
Kjolby M, Andersen OM, Breiderhoff T, Fjorback AW, Pedersen KM, Madsen P, et al. Sort1, encoded by the cardiovascular risk locus 1p13.3, is a regulator of hepatic lipoprotein export. Cell Metab. 2010;12(3):213–23.
• Chen KC, Wang YS, Hu CY, Chang WC, Liao YC, Dai CY, et al. Oxldl up-regulates microrna-29b, leading to epigenetic modifications of mmp-2/mmp-9 genes: A novel mechanism for cardiovascular diseases. Faseb J. 2011;25(5):1718–28. Identified miRNA-29b as modifying MMP activity.
Yuan M, Zhan Q, Duan X, Song B, Zeng S, Chen X, et al. A functional polymorphism at mir-491-5p binding site in the 3′-utr of mmp-9 gene confers increased risk for atherosclerotic cerebral infarction in a chinese population. Atherosclerosis. 2013;226(2):447–52.
• Cipollone F, Felicioni L, Sarzani R, Ucchino S, Spigonardo F, Mandolini C, et al. A unique microrna signature associated with plaque instability in humans. Stroke. 2011;42(9):2556–63. Identified the miRNA signature that yields unstable plaque.
Fichtlscherer S, De Rosa S, Fox H, Schwietz T, Fischer A, Liebetrau C, et al. Circulating micrornas in patients with coronary artery disease. Circ Res. 2010;107(5):677–84.
Wang D, Xia M, Yan X, Li D, Wang L, Xu Y, et al. Gut microbiota metabolism of anthocyanin promotes reverse cholesterol transport in mice via repressing mirna-10b. Circ Res. 2012;111(8):967–81.
Horie T, Baba O, Kuwabara Y, Chujo Y, Watanabe S, Kinoshita M, et al. Microrna-33 deficiency reduces the progression of atherosclerotic plaque in apoe-/- mice. J Am Heart Assoc. 2012;1(6):e003376.
Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, et al. Primary prevention of cardiovascular disease with a mediterranean diet. N Engl J Med. 2013;368(14):1279–90.
Tang WH, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013;368(17):1575–84.
Wang Z, Klipfell E, Bennett BJ, Koeth R, Levison BS, Dugar B, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011;472(7341):57–63. doi:10.1038/nature09922.
Wang D, Zou T, Yang Y, Yan X, Ling W. Cyanidin-3-o-beta-glucoside with the aid of its metabolite protocatechuic acid, reduces monocyte infiltration in apolipoprotein e-deficient mice. Biochem Pharmacol. 2011;82(7):713–9.
Wang D, Wei X, Yan X, Jin T, Ling W. Protocatechuic acid, a metabolite of anthocyanins, inhibits monocyte adhesion and reduces atherosclerosis in apolipoprotein e-deficient mice. J Agric Food Chem. 2010;58(24):12722–8.
Herrera BM, Lockstone HE, Taylor JM, Ria M, Barrett A, Collins S, et al. Global microrna expression profiles in insulin target tissues in a spontaneous rat model of type 2 diabetes. Diabetologia. 2010;53(6):1099–109.
• Jordan SD, Kruger M, Willmes DM, Redemann N, Wunderlich FT, Bronneke HS, et al. Obesity-induced overexpression of mirna-143 inhibits insulin-stimulated akt activation and impairs glucose metabolism. Nat Cell Biol. 2011;13(4):434–46. Identifies miRNA-143 as being increased in impaired glucose metabolism.
Meerson A, Traurig M, Ossowski V, Fleming JM, Mullins M, Baier LJ. Human adipose microrna-221 is upregulated in obesity and affects fat metabolism downstream of leptin and tnf-alpha. Diabetologia. 2013;56(9):1971–9.
Acknowledgments
We acknowledge funding support from the National Institutes of Health NHLBI HHSN 268201000036C (N01-HV-00244) for the San Antonio Cardiovascular Proteomics Center, HL075360 and HL051971, and the Veteran’s Administration (Merit) to MLL.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Hiroe Toba, Dolores Cortez, and Merry L. Lindsey declare that they have no conflict of interest.
Robert J. Chilton received honoraria from Takada and Pfizer and received payment for the development of educational presentations from Lilly and BMS.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Coronary Heart Disease
Rights and permissions
About this article
Cite this article
Toba, H., Cortez, D., Lindsey, M.L. et al. Applications of miRNA Technology for Atherosclerosis. Curr Atheroscler Rep 16, 386 (2014). https://doi.org/10.1007/s11883-013-0386-9
Published:
DOI: https://doi.org/10.1007/s11883-013-0386-9