Abstract
Much controversy surrounds the use of high-sensitivity C-reactive protein (hs-CRP) as a marker of cardiovascular (CV) risk. Although data regarding the association of hs-CRP with CV disease is extensive and consistent, its role in clinical practice remains unclear. The American Heart Association (AHA) recently published a scientific statement regarding criteria for evaluation of novel markers of CV risk. This article provides a comprehensive review of data regarding hs-CRP as a risk marker for CV disease in the context of these AHA criteria. The impact of the JUPITER trial on the utility of hs-CRP as a risk marker is emphasized. The review concludes with an evidence-based statement regarding the current role of hs-CRP in CV risk prediction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
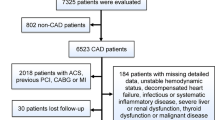
Inflammation plays a major role in the various stages of atherosclerosis, from the development of the initial fatty streak to plaque rupture to resultant thrombosis. Current prevention and treatment guidelines for coronary artery disease (CAD) depend on the assessment of an individual’s risk of cardiovascular (CV) events using algorithms such as the Framingham risk model. Accurate estimation of CV risk is therefore of paramount importance.
The association between C-reactive protein (CRP) and CAD was first described more than two decades ago [1, 2]. Since then, CRP has been the focus of intense investigation and has been proposed as an important and independent risk factor for CAD. Its measurement is thought to aid in further risk stratifying those individuals who are classified as intermediate risk (ie, 10-year risk of CV events between 10% and 20% using the Framingham risk model) [3, 4]. However, there still remains strong debate about the role of CRP measurement in clinical practice and whether it can improve risk prediction beyond that provided by traditional risk factors. In 2008, the results of the Justification for the Use of Statins in Primary Prevention (JUPITER): An Intervention Trial Evaluation of Rosuvastatin, provoked further debate about the utility of CRP in primary prevention of CAD [5••].
A recently released scientific statement by the American Heart Association (AHA) described six criteria for the evaluation of novel markers of cardiovascular risk [6]. In this review, we discuss CRP as marker of CV risk as it relates to these AHA criteria, with special emphasis on the implications of the JUPITER trial.
C-Reactive Protein
CRP was discovered in the early decades of the 20th century and named for its binding of pneumococcal C-polysaccharide. The associated “high sensitivity” term refers to the measurement of CRP in serum or plasma samples using immunoassay methods with sufficient sensitivity to quantify CRP throughout its normal range [7•]. CRP is an acute-phase protein that is produced by the liver in response to numerous inflammatory cytokines, primarily interleukin-6 [8]. CRP levels increase 6 h after an acute stimulus and peak within 48 h [9]. Although CRP levels fall to baseline within 1 to 2 days [10], its long half-life of approximately 19 h allows for levels to remain stable long enough to make random measurements clinically relevant [11].
The exact biologic role of CRP in inflammation and atherosclerosis remains a matter of debate. CRP binds to low-density lipoprotein (LDL) [12, 13], very low-density lipoprotein (VLDL) [14], and platelet activation factor [15]. CRP also binds to complement factors and activates the classical complement pathway, thus contributing to host defense against infection by promoting an inflammatory response [16]. CRP has been shown to be present in atherosclerotic plaques [17].
Skeptics argue that CRP is “an innocent bystander” and that elevated levels of CRP do not cause inflammation or CVD [18]. This is supported by a study showing that injection of large amounts of human CRP into animals produces no adverse inflammatory effects [19]. Another study demonstrated certain genetic polymorphisms associated with elevated CRP levels were not associated with higher rates of ischemic or cerebrovascular events [20••]. Whether CRP is a critical component of atherosclerotic development or a true innocent bystander remains unresolved.
C-Reactive Protein and Cardiovascular Risk Prediction
In 2009, the AHA published a scientific statement proposing six criteria for evaluation of novel markers of cardiovascular risk [6]. The statement proposed standards for the critical appraisal of risk assessment methods and emphasized the utility of novel markers in improving risk prediction beyond established risk predictors. Additionally, the statement emphasized that markers should be assessed by their effect on clinical decisions and ultimately on clinical outcomes. The statement outlines six elements for evaluation of a novel marker: 1) proof of concept, 2) prospective evaluation, 3) incremental value, 4) clinical utility, 5) clinical outcomes, and 6) cost effectiveness.
Proof of Concept and Prospective Validation
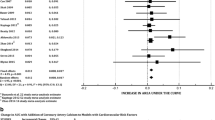
“Proof of concept” refers to the difference in marker levels between subjects with and without disease, whereas “prospective validation” addresses a marker’s ability to predict the development of specific future outcomes. CRP has been studied extensively as an independent risk factor for CVD after adjusting for traditional Framingham risk factors. In 2004, Danesh et al. [21], in a meta-analysis of 22 prospective studies that included a total of 7068 patients, found that the adjusted odds ratio of coronary heart disease (CHD) was 1.45 (95% CI, 1.25–1.68) in those whose CRP levels were in the third tertile compared with subjects whose levels were in the first tertile. More recently, Buckley et al. [22] conducted a meta-analysis that included 22 prospective studies encompassing 23 cohorts. The relative risk for high (>3 mg/L) versus low (<1 mg/L) CRP levels in this study was 1.60 (95% CI, 1.43–1.78). When the analysis was restricted to high-quality studies that adjusted for all Framingham risk variables (10 studies in 11 cohorts), the relative risk of CHD was 1.58 (95% CI, 1.37–1.83) for CRP level greater than 3.0 mg /L compared with levels less than 1.0 mg/L. The study concluded that there was strong evidence indicating that CRP is independently associated with CHD events [22]. Similar results were reported in a more recent meta-analysis by The Emerging Risk Factors Collaboration [[23]. The study showed that the risk ratio for CHD per 1-standard deviation of higher log CRP concentration was 1.37 (95% CI, 1.27–1.48). This effect was higher than that of hypertension or high-density lipoprotein (HDL) cholesterol [23].In summary, these studies demonstrate proof of concept and prospective validation by showing that CRP is independently and moderately associated with CVD.
Incremental Value (discrimination and calibration)
“Incremental value” answers the question, “does the novel marker add predictive information to established, standard risk markers?” Discrimination and calibration of the specific risk prediction model are used to define this answer. Discrimination is the ability to rank subjects in order of risk, such that those who experience the event of interest have a higher predicted risk than those who do not experience it. If discrimination is poor, then people above the threshold will receive treatment unnecessarily and people below the threshold will experience the outcome but will not receive preventive treatment [24]. Discriminatory ability of a model has been traditionally measured by the area under the Receiver Operating Characteristic (ROC) curve (also called the C-statistic). The value of the C-statistic ranges from 0 to 1, with 0.5 having no discriminatory ability and a value of 1 suggesting perfect discriminatory power. Others have described the C statistic as a measure of how well models can rank order cases and non-cases. However, the C statistic is not a function of the actual predicted probabilities. For instance, a model that assigns all cases a value of 0.52 and all non-cases a value of 0.51 would have perfect discrimination despite very close probabilities [25]. Therefore, it is clear that the C-statistic has little to do with actual risk and more with ranking subjects as cases and controls. Multiple studies have compared the C-statistic with and without CRP in multivariate models [3, 21, 26–31]. None of these studies showed improvement in the C-statistic when CRP was added to the traditional risk factors for CVD.
The impact of CRP on the C-statistic value was found to be similar to that of LDL, a well established risk factor. One study showed that the addition of LDL to a model that included all other traditional CV risk factors changed the C-statistic marginally from 0.76 to 0.77 [25].Similarly, no significant change in the C-statistic was reported with HDL or hypertension [25]. In light of this, researchers have questioned the use of the C-statistic as an appropriate measure to determine risk factor selection and have called for the use of other statistical modalities that measures global model accuracy rather than just measuring values of the C-statistic [3, 32, 33••] . In summary, CRP does not improve discrimination as measured by the C-statistic; neither do other traditional CV risk factors, such as LDL, HDL, or hypertension.
Calibration measures the accuracy of the model predictions. In essence, calibration measures how well predicted probabilities agree with actual observed risk. If the average predicted risk from the model within subgroups of a prospective cohort matches the proportion that actually develops disease, then the model is well calibrated [25]. The Hosmer-Lemeshow statistic, a statistic that measures goodness of fit, is a popular means to assess model calibration because it directly compares the predicted risk with the observed risk [34]. Other statistics can also provide measures of global model accuracy and calibration, such as likelihood ratio Chi-squared, Bayes Information Criterion (BIC), Aikake’s Information Criterion (AIC), and Brier score.
Although both discrimination and calibration are measures of model accuracy in risk prediction, only two studies have examined the additive effect of CRP on calibration. The first study, by Cook et al. [3], assessed the effect of adding CRP to a global cardiovascular risk prediction model in 15,048 initially healthy American women in the Women’s Health Study (WHS). All measures of model calibration, including AIC, BIC, likelihood ratio Chi-squared, and Brier score, improved with the addition of CRP to a model that already included other traditional CV risk factors [3]. The second study of 3435 white men from southern Germany showed that the addition of CRP to corresponding Framingham Risk Scores improved global risk assessment and calibration as measured by a difference of 13 points in AIC [31]. This was especially true in those subjects who fell in the intermediate-risk category (10-year risk of CVD 6%–15%) [31]. In summary, limited data support the addition of CRP to a model that already considers other traditional risk factors that improve model calibration. However, given that this data is sparse, larger and more comprehensive studies that include both men and women are needed to accurately determine the effect of CRP on calibration of CV risk prediction models.
Clinical Utility (reclassification)
Reclassification refers to the net proportion of individuals who cross a clinically relevant risk threshold as a result of using the new risk marker [6]. In other words, does measurement of CRP change the classification of a significant proportion of patients to a more accurate level of risk? Will this new level of risk lead to a difference in clinical management, such as initiation or withholding of intervention? The best summary measure of this concept is the Net Reclassification Index (NRI) as proposed by Pencina et al. [33••]
The NRI method provides a rigorous statistical approach to assess the improvement in reclassification by including new biomarker information into prediction models. The effect of including the biomarker into the prediction model of risk category reclassification is assessed separately for cases and for controls. When cases (those who develop the outcome) are reclassified to a higher risk category, such movement is considered an improvement. On the other hand, reclassification downward is considered a failure for persons who develop an event. Conversely, among persons who do not experience an event, reclassification upward is considered disadvantageous, and reclassification downward is considered advantageous [35]. The NRI is the sum of the difference of proportions of cases and controls that are reclassified in the advantageous direction. The higher the NRI, the better the risk factor is in accurately reclassifying individuals. Table 1 shows all studies published to date that directly assesses the effect of CRP on reclassification as measured by NRI. Cook et al. [3] initially estimated that CRP reclassified about 20% of patients in the intermediate-risk category (10-year CVD risk of 5%–20%) using a less vigorous statistical approach than the NRI. However, using the NRI method applied to the same population, CRP reclassified only 15% of patients in the intermediate-risk category [36]. Wilson et al. [35], in the Framingham Offspring Study, showed that the NRI of adding CRP to the Framingham Risk Score is 5.6% for CVD and 11.8% for the hard endpoints of CHD (myocardial infarction and CHD-related death). When the 6% to 20% risk category was studied, the NRI went up to 14.7% for CVD and 24% for the hard endpoints of CHD [35]. This indicates that CRP improves reclassification mainly in patients who are in the intermediate-risk category.
Two studies from European populations showed different results. The Northwick Park Health Study (NPHS) is a prospective population-based study that included 3012 middle-aged men (50–64 years), and the Edinburgh Artery Study (EAS) included 1592 men and women [37]. In these populations, when CRP was added to a Framingham-based model using four categories of 10-year CHD risk, the proportion of subjects correctly reclassified was almost matched by the proportion incorrectly reclassified. The NRI was only 8.5% (−1.3% to 18.3%) in NPHS and 8.8% (−1.3% to 18.9%) in EAS. The NRI was reduced further to 4.9% (0.8% to 9.0%) in NPHS and 3.0% (−3.0% to 9.2%) in EAS when 15% 10-year risk cutoff was used. It is important to note the smaller sample size of these two populations compared to the WHS and Framingham Offspring Study. In summary, the current data support the use of CRP in accurately reclassifying CV risk in 5% to 15% of those in the intermediate-risk category.
Clinical Outcomes and Cost Effectiveness
The most important and clinically relevant question is whether measuring CRP in the target population favorably influences clinical outcome. The optimal means to answer this question is through a clinical trial in which the outcomes of individuals whose management is guided by CRP are compared with the outcomes of patients who are managed without CRP measurement. The clinical outcome of interest would be the development of CV disease or CV-related death. To our knowledge, no such trial has yet been conducted. The JUPITER trial, described below, is the study that is frequently and mistakenly cited as such a trial. However, this study did not randomize patients to testing with CRP versus no CRP testing. Instead, JUPITER required that all subjects undergo CRP testing and have a CRP = 2 mg/L in order to be included in the trial.
Some studies have shown that statin treatment is associated with greater CV event reduction in patients with higher hs-CRP levels than in those with lower hs-CRP levels. This held true even when lipid levels were below the cutoff point for initiation of statin therapy [38, 39]. Of note, these studies were retrospective, secondary analyses and patients were not randomized to statin therapy according to their hs-CRP levels. In addition, the interaction between hs-CRP and statin treatment was not significant in both studies (P = 0.06).
The cost effectiveness of CRP testing and screening is another major knowledge gap owing to a lack of clinical trials on CRP testing. However, few authors have tried to approximate the added cost of including CRP into the CV risk assessment algorithm. If we apply the data of the JUPITER study to the general US population, 11 million new patients would be eligible for statin therapy [40]. In the light of this large number, the cost effectiveness of hs-CRP testing should merit full consideration.
Recent cost effective analysis by Lee et al. [41] compared three scenarios of initiating statin therapy for primary prevention in intermediate and low CV risk individuals. In the analysis, the current Adult Treatment Panel (ATP) III practice guidelines were compared to two strategies. The first strategy was that of hs-CRP screening in those without an indication for statin treatment per current practice guidelines, followed by treatment in those with elevated hs-CRP levels. The second strategy was based on statin therapy at specified predicted risk thresholds without hs-CRP testing. Screening for hs-CRP was found to be comparable, but not superior, to ATP III practice guidelines. Screening with hs-CRP would indeed be the optimal strategy if the relative risk reduction from statin therapy in those with normal hs-CRP levels was substantially less than in those with elevated hs-CRP. In other words, the ability of hs-CRP to identify those with higher risk is not sufficient by itself to make it a cost-effective screening tool. The JUPITER study failed to show this effect because no significant interaction between hs-CRP levels with treatment (P = 0.15) was demonstrated. Two other studies showed risk reduction by statins in those with elevated CRP but not with normal hs-CRP However, the interaction of hs-CRP with statin treatment in those two studies was not significant (P = 0.06) [38, 39].
Additionally, cost effectiveness of hs-CRP is highly dependent on the risk and cost associated with statin therapy. The expected decrease in cost of statin therapy in the future will have a favorable impact on the cost-effectiveness equation of hs-CRP. Treatment with 80 mg of simvastatin for those with elevated hs-CRP but normal cholesterol (equivalent to 20 mg of rosuvastatin, as used in JUPITER) was found to be cost effective at $20,000/QALY (quality-adjusted life year) in one study [42]. However, the study did not show whether hs-CRP was superior to the current practice guidelines. Statin treatment without hs-CRP and regardless of lipid levels for those with a 10-year Framingham Risk Score of 5% to 20% has been shown to be cost effective in three cost-analysis studies [43–45]. However, until the definite effect of statin therapy on those with low hs-CRP is established, the cost effectiveness of hs-CRP screening remains to be confirmed.
The JUPITER Trial
JUPITER was a large, double-blind, placebo-controlled multinational trial. A total of 17,802 apparently healthy men and women with LDL cholesterol levels of less than 130 mg/dL and hs-CRP levels of 2.0 mg/L or higher were randomly assigned to 20 mg/d of rosuvastatin or placebo [5••]. Patients were followed for the occurrence of the combined primary end points of myocardial infarction, stroke, arterial revascularization, hospitalization for unstable angina, or death from cardiovascular causes. The trial included men over the age of 50 years and postmenopausal women over the age of 60 years. Thirty-eight percent of subjects were women and 25% were black or Hispanic.
Aspirin was used by 17% of participants, 41% had the metabolic syndrome, 16% used tobacco, and 11% had a family history of heart disease. In both the rosuvastatin and placebo groups, the median LDL cholesterol level was 108 mg/dL, the median HDL cholesterol level was 49 mg/dL, and the median triglyceride level was 118 mg/dL. The median hs-CRP level was 4.2 and 4.3 mg/L in the rosuvastatin and placebo groups, respectively. At 12 months, among patients treated with rosuvastatin, LDL levels decreased by approximately 50% to 55 mg/dL, median triglyceride levels were lowered by 17%, and C-reactive protein levels were reduced to 2.2 mg/L.
The JUPITER trial was terminated early after a mean of 1.9 years of follow-up (scheduled for 5 years) by an independent data and safety monitoring board. Only 142 first major CV events had occurred in the rosuvastatin group compared with 251 in the placebo group. The absolute risk reduction was 1.2%, with the primary endpoint occurring in 2.8% of patients in the placebo arm versus 1.6% of patients in the rosuvastatin group. The primary endpoint was reduced by 44% in the rosuvastatin arm, with a 20% reduction in all-cause mortality. Relative hazard reductions in the rosuvastatin group were similar for women (46%) and men (42%) and were observed in every subgroup evaluated, including subgroups according to age, race/ethnic group, region of origin, status with regard to traditional risk factors, and Framingham Risk Score. Rosuvastatin was associated with a small but significant increase in the rate of physician-reported diabetes as well as a small, though significant, increase in the median value of glycated hemoglobin.
The external validity of the JUPITER trial results has been called into question by some studies because at least 41% of the JUPITER study population had metabolic syndrome and were candidates for statin therapy regardless of their CRP level [46••]. In addition, the JUPITER population was arguably not a “healthy population,” as more than 50% were overweight and 25% had hypertension. It was suggested that the effect of rosuvastatin in the JUPITER trial may have been diminished if the study population had received current standard of care [46••, 47]. For example, whereas aspirin was recommended in 50% of the JUPITER population (those with 10-year CHD risk = 10%), less than 17% of the study subjects were, in fact, using aspirin.
The long-term safety of rosuvastatin therapy has not been fully established. There was a slight, but significant, increase in the rate of physician-reported diabetes in the rosuvastatin group. However, a new meta-analysis of 13 statin trials with 91,140 participants concluded that there is a 9% increased risk of development of diabetes associated with statin therapy (odds ratio of 1.09; 95% CI, 1.02–1.17) [48•]
Implications of JUPITER Trial hs-CRP on CV Risk Prediction
hs-CRP meets four of the six AHA statement criteria for use as a novel cardiovascular risk marker (proof of concept, prospective validation, incremental value beyond risk factors, and clinical utility). The clinical utility of hs-CRP was largely evident in individuals in the intermediate-risk group (Framingham Risk Score of 10%–20%). hs-CRP was able to accurately reclassify 8% to 15% of those in the intermediate-risk category to a higher or lower risk category. This reclassification has an impact on clinical decision-making regarding starting intervention (ie, initiation of statin therapy). However, there is a clear shortage of data on the impact of clinical outcomes, cost effectiveness of reclassification, and on routine measurement of hs-CRP. Should we start screening every individual for hs-CRP without clinical trials that demonstrate improved clinical outcomes associated with CRP testing? Or should we continue the current Centers for Disease Control (CDC)/AHA guidelines for hs-CRP stating that the use of hs-CRP levels may be useful in patients at intermediate risk? It should be noted that other well-established risk factors such as HDL and triglyceride levels have not been shown to fulfill all the AHA criteria for risk markers. However, HDL and triglycerides have direct causative association with coronary atherosclerosis, an effect that CRP does not have.
The JUPITER trial itself did not test the clinical utility of hs-CRP measurement and neither did it provide data on cost effectiveness of hs-CRP measurement. It did, however, suggest that elevated hs-CRP may identify a population of patients who do not otherwise meet current guideline criteria for statin therapy but nonetheless appear to benefit from it. It provided no information about the clinical outcome of hs-CRP measurement because it did not randomize patients to hs-CRP measurement versus no hs-CRP measurement. The JUPITER study may have only proven that lowering LDL reduces primary CV risk in persons without apparent CAD or CAD equivalents.
Conclusions
Advocating for the widespread use of hs-CRP for CV prediction is premature without randomized controlled trials that include subjects with both low and high hs-CRP levels and without a careful assessment of cost effectiveness. Until such trials are conducted, we advocate the limited use of hs-CRP in intermediate-risk (10-year CV risk of 10%–20%) individuals as currently recommended by the AHA/CDC guidelines. However, hs-CRP use can be extended to those with 10-year risk as low as 5%.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Berk B, Weintraub W, Alexander R. Elevation of C-reactive protein in active coronary artery disease. Am J Cardiol. 1990;65(3):168–72.
Liuzzo G, Biasucci L, Gallimore J, Grillo R, Rebuzzi A, Pepys M, et al. The prognostic value of C-reactive protein and serum amyloid A protein in severe unstable angina. N Engl J Med. 1994;331(7):417.
Cook NR, Buring JE, Ridker PM. The effect of including C-reactive protein in cardiovascular risk prediction models for women. Ann Intern Med. 2006;145(1):21.
Ridker PM. C-reactive protein and the prediction of cardiovascular events among those at intermediate risk: moving an inflammatory hypothesis toward consensus. J Am Coll Cardiol. 2007;49(21):2129–38.
•• Ridker PM, Danielson E, Fonseca FAH, Genest J, Gotto Jr AM, Kastelein JJP, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359(21):2195. This is the main article of the JUPITER study. It showed the rosuvastatin therapy in those “apparently” healthy population with elevated hs-CRP of >2 mg/L and low LDL (<130 mg/dL) had decreased cardiovascular risk with the use of rosuvastatin.
Hlatky MA, Greenland P, Arnett DK, Ballantyne CM, Criqui MH, Elkind MSV, et al. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2009;119(17):2408.
• Bajpai A, Goyal A, Sperling L. Should we measure C-reactive protein on Earth or just on JUPITER? Clin Cardiol. 2010;33(4):190–8. This article provides a comprehensive review of the data regarding cardiovascular risk and hs-CRP with an emphasis on the JUPITER trial .It concludes with an evidence-based analysis of the role of hs-CRP in cardiovascular risk assessment.
Hirschfield G, Pepys M. C-reactive protein and cardiovascular disease: new insights from an old molecule. QJM. 2003;96(11):793.
Kushner I. C-reactive protein and the acute-phase response. Hosp Pract (Off ed). 1990;25(3):13.
Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340(6):448.
Vigushin D, Pepys M, Hawkins P. Metabolic and scintigraphic studies of radioiodinated human C-reactive protein in health and disease. J Clin Investig. 1993;91:1351–1.
De Beer F, Soutar A, Baltz M, Trayner I, Feinstein A, Pepys M. Low density lipoprotein and very low density lipoprotein are selectively bound by aggregated C-reactive protein. J Exp Med. 1982;156(1):230.
Pepys M, Rowe I, Baltz M. C-reactive protein: binding to lipids and lipoproteins. Int Rev Exp Pathol. 1985;27:83.
Chang M, Binder C, Torzewski M, Witztum J. C-reactive protein binds to both oxidized LDL and apoptotic cells through recognition of a common ligand: phosphorylcholine of oxidized phospholipids. Proc Natl Acad Sci USA. 2002;99(20):13043.
Vigo C. Effect of C-reactive protein on platelet-activating factor-induced platelet aggregation and membrane stabilization. J Biol Chem. 1985;260(6):3418.
Volanakis J, Narkates A. Binding of human C4 to C-reactive protein-pneumococcal C-polysaccharide complexes during activation of the classical complement pathway. Mol Immunol. 1983;20(11):1201–7.
Zhang Y, Cliff W, Schoefl G, Higgins G. Coronary C-reactive protein distribution: its relation to development of atherosclerosis. Atherosclerosis. 1999;145(2):375–9.
Nordestgaard BG, Zacho J. Lipids, atherosclerosis and CVD risk: Is CRP an innocent bystander? Nutr Metab Cardiovasc Dis. 2009;19(8):521–4.
Casas J, Shah T, Hingorani A, Danesh J, Pepys M. C-reactive protein and coronary heart disease: a critical review. J Intern Med. 2008;264(4):295–314.
•• Zacho J, Tybjaerg-Hansen A, Jensen JS, Grande P, Sillesen H, Nordestgaard BG. Genetically elevated C-reactive protein and ischemic vascular disease. N Engl J Med. 2008;359(18):1897. This landmark genetic study showed that polymorphisms in the CRP gene are associated with marked increases in CRP levels but with no increase risk of ischemic vascular disease.
Danesh J, Wheeler JG, Hirschfield GM, Eda S, Eiriksdottir G, Rumley A, et al. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N Engl J Med. 2004;350(14):1387.
Buckley DI, Fu R, Freeman M, Rogers K, Helfand M. C-reactive protein as a risk factor for coronary heart disease: a systematic review and meta-analyses for the US Preventive Services Task Force. Ann Intern Med. 2009;151(7):483.
Kaptoge S, Di Angelantonio E, Lowe G, Pepys MB, Thompson SG, Collins R. Emerging Risk Factors Collaboration. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010;375:132–40.
May M, Lawlor D, Brindle P, Patel R, Ebrahim S. Cardiovascular disease risk assessment in older women: can we improve on Framingham? British Women’s Heart and Health prospective cohort study. Br Med J. 2006;92(10):1396.
Cook NR. Use and misuse of the receiver operating characteristic curve in risk prediction. Circulation. 2007;115(7):928.
Cao J, Arnold A, Manolio T, Polak J, Psaty B, Hirsch C, et al. Association of carotid artery intima-media thickness, plaques, and C-reactive protein with future cardiovascular disease and all-cause mortality: the Cardiovascular Health Study. Circulation. 2007;116(1):32.
Sattar N, Murray H, McConnachie A, Blauw G, Bollen E, Buckley B, et al. C-reactive protein and prediction of coronary heart disease and global vascular events in the Prospective Study of Pravastatin in the Elderly at Risk (PROSPER). Circulation. 2007;115(8):981.
Shlipak M, Fried L, Cushman M, Manolio T, Peterson D, Stehman-Breen C, et al. Cardiovascular mortality risk in chronic kidney disease: comparison of traditional and novel risk factors. JAMA. 2005;293(14):1737.
Wilson PWF, Nam BH, Pencina M, D’Agostino Sr RB, Benjamin EJ, O’Donnell CJ. C-reactive protein and risk of cardiovascular disease in men and women from the Framingham Heart Study. Arch Intern Med. 2005;165(21):2473.
Rutter M, Meigs J, Sullivan L, Sr D’Agostino R, Wilson P. C-reactive protein, the metabolic syndrome, and prediction of cardiovascular events in the Framingham Offspring Study. Circulation. 2004;110(4):380.
Koenig W, Lowel H, Baumert J, Meisinger C. C-reactive protein modulates risk prediction based on the Framingham Score: implications for future risk assessment: results from a large cohort study in southern Germany. Circulation. 2004;109(11):1349.
Janes H, Pepe M, Gu W. Assessing the value of risk predictions by using risk stratification tables. Ann Intern Med. 2008;149(10):751.
•• Pencina MJ, D’Agostino Sr RB, Jr D’Agostino RB, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27(2):157–72. This article intoduces the Net Reclassification Index (NRI) as a novel way of measuring the additive effect of a variable to a model in reclassifying individuals to different risk category.
Hosmer D, Lemesbow S. Goodness of fit tests for the multiple logistic regression model. Commun Stat-Theory Methods. 1980;9(10):1043–69.
Wilson P, Pencina M, Jacques P, Selhub J, Sr D’Agostino R, O’Donnell C. C-reactive protein and reclassification of cardiovascular risk in the Framingham Heart Study. Circ Cardiovasc Qual Outcomes. 2008;1(2):92.
Cook N. Comments on ‘Evaluating the added predictive ability of a new marker: From area under the ROC curve to reclassification and beyond’ by MJ Pencina et al., Statistics in Medicine (DOI. Stat Med. 2008;27(2):191–5.
Shah T, Casas JP, Cooper JA, Tzoulaki I, Sofat R, McCormack V, et al. Critical appraisal of CRP measurement for the prediction of coronary heart disease events: new data and systematic review of 31 prospective cohorts. Int J Epidemiol. 2009;38:217–31.
McMurray J, Kjekshus J, Gullestad L, Dunselman P, Hjalmarson A, Wedel H, et al. Effects of statin therapy according to plasma high-sensitivity C-reactive protein concentration in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA): a retrospective analysis. Circulation. 2009;120(22):2188.
Ridker PM, Rifai N, Clearfield M, Downs JR, Weis SE, Miles JS, et al. Measurement of C-reactive protein for the targeting of statin therapy in the primary prevention of acute coronary events. N Engl J Med. 2001;344(26):1959.
Spatz ES, Canavan ME, Desai MM. From here to JUPITER: identifying new patients for statin therapy using data from the 1999–2004 National Health and Nutrition Examination Survey. Circ Cardiovasc Qual Outcomes. 2009;2(1):41.
Lee K, Cipriano L, Owens D, Go A, Hlatky M. Cost-Effectiveness of Using High-Sensitivity C-Reactive Protein to Identify Intermediate-and Low-Cardiovascular-Risk Individuals for Statin Therapy. Circulation. 2010;122:1478–87.
Slejko JF, Page 2nd RL, Sullivan PW. Cost-effectiveness of statin therapy for vascular event prevention in adults with elevated C-reactive protein: implications of JUPITER. Curr Med Res Opin. 2010;26(10):2485–97.
Mihaylova B, Briggs A, Hlatky M, Armitage J, Parish S, Gray A, et al. Statin cost-effectiveness in the United States for people at different vascular risk levels. Circ Cardiovasc Qual Outcomes. 2009;2(2):65–72.
Pletcher M, Lazar L, Bibbins-Domingo K, Moran A, Rodondi N, Coxson P, et al. Comparing impact and cost-effectiveness of primary prevention strategies for lipid-lowering. Ann Intern Med. 2009;150(4):243.
Hayward R, Krumholz H, Zulman D, Timbie J, Vijan S. Optimizing statin treatment for primary prevention of coronary artery disease. Ann Intern Med. 2010;152(2):69.
•• Kappagoda CT, Amsterdam EA. Another look at the results of the JUPITER trial. Am J Cardiol. 2009;104(11):1603–5. This articles analyzes the methodology and results of the JUPITER study. It shows significant epidemiologic and methodologic inconsistencies in the JUPITER study that warrant consideration. The article emphasizes that the study population was not a healthy population and that standard medical care was not provided to the population that could have changed the result of the study significantly.
Gibbons R, Fugh-Berman A, Chan P, Nallamothu B, Hayward R, Jenny-Avital E, et al. Rosuvastatin in patients with elevated C-reactive protein. N Engl J Med. 2009;360(10):1038.
• Sattar N, Preiss D, Murray H, Welsh P, Buckley B, de Craen A, Seshasai S, McMurray J, Freeman D, Jukema J. Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet 2010. This study is a meta-analysis of the risk of diabetes mellitus with statin therapy. It concludes that statin therapy is associated with a slightly increased risk of development of diabetes, but the risk is low.
Disclosure
The authors report no potential conflicts of interest relevant to this article.
Dr. Antonio Gotto, Editor-in-Chief of Current Atherosclerosis Reports, reviewed this article and provided comments and suggestions. He was a member of the JUPITER Steering Committee, for which he received honoraria, and has served as a consultant for AstraZeneca. He has no financial relationship with the manufacturer of the hs-CRP test.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abd, T.T., Eapen, D.J., Bajpai, A. et al. The Role of C-Reactive Protein as a Risk Predictor of Coronary Atherosclerosis: Implications from the JUPITER Trial. Curr Atheroscler Rep 13, 154–161 (2011). https://doi.org/10.1007/s11883-011-0164-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11883-011-0164-5