Abstract
The avoidance of wheat- and gluten-containing products is a worldwide phenomenon. While celiac disease is a well-established entity, the evidence base for gluten as a trigger of symptoms in patients without celiac disease (so-called ‘non-celiac gluten sensitivity’ or NCGS) is limited. The problems lie in the complexity of wheat and the ability of its carbohydrate as well as protein components to trigger gastrointestinal symptoms, the potentially false assumption that response to a gluten-free diet equates to an effect of gluten withdrawal, and diagnostic criteria for coeliac disease. Recent randomized controlled re-challenge trials have suggested that gluten may worsen gastrointestinal symptoms, but failed to confirm patients with self-perceived NCGS have specific gluten sensitivity. Furthermore, mechanisms by which gluten triggers symptoms have yet to be identified. This review discusses the most recent scientific evidence and our current understanding of NCGS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Avoidance of wheat-containing products is a worldwide phenomenon. People are avoiding wheat and gluten for putative health benefits. Gluten has been linked to a wide range of conditions including various skin problems [1], fatigue and migraine [2], weight gain [3] and autism [4]. Moreover, wheat and gluten are most often blamed for gastrointestinal symptoms [5]. Unfortunately, this whole area has been complicated by the assumption by many that benefits of a gluten-free or wheat-free diet equate to a problem caused by gluten. The role of dietary components in inducing gastrointestinal symptoms is a complex area. As wheat has multiple constituents, discussion of gluten-mediated problems cannot be divorced from considering the role of other components in wheat. These and other wheat-related conditions will also be considered.
Components of Wheat
Protein
Gluten is the main storage protein contained within the germ of wheat grains [6]. Gluten is a complex mixture of hundreds of related but distinct proteins, mainly gliadin and glutenin. Similar proteins to the gliadin found in wheat exist as secalin in rye, hordein in barley and avenins in oats, and are collectively referred to as ‘gluten’. Derivatives of these grains such as triticale and malt and other ancient wheat varieties such as spelt and kamut also contain gluten. Non-gluten proteins include α-amylase/trypsin inhibitors and have recently been suggested to induce intestinal inflammation [7•].
Carbohydrate
The wheat carbohydrates that have excited most interest with regard to intestinal health are those that are indigestible, because they are a key substrate for bacterial metabolism and growth, and their fermentation releases short-chain fatty acids such as butyrate, which have multiple beneficial effects on the colonic mucosa. Long-chain carbohydrates, particularly non-starch polysaccharides have important roles in laxation and prevention of colorectal cancer [8•], and wheat bran is often used therapeutically as a rich source of dietary fibre. Wheat is also rich in short-chain carbohydrates. The oligosaccharides, particularly fructans (chains of fructose joined by β(2–1) bonds with a terminal glucose) have emerged as potentially exerting health benefits via a prebiotic effect [9] and as important inducers of functional gastrointestinal symptoms (reviewed in [10]).
The human small intestine does not produce a hydrolase to digest fructans to absorbable single sugars. Ingested fructans, being relatively small molecules, will have an osmotic effect in the small intestine increasing the water content of the lumen [11]. After delivery to the colon, fermentation releases gases, hydrogen, carbon dioxide and methane. These effects result in luminal distension, a major stimulus to the gut’s nervous system (see below). Fructans are part of a family of poorly absorbed dietary short-chain carbohydrates (termed fodmaps) [12•]. Fodmaps all behave similarly in the intestine, and their effects on luminal distension and on symptoms are additive. Since fodmaps are found in a wide variety of foods (detailed in Table 1), they are usually consumed in combination. Interestingly, recent grain and cereal composition data has highlighted that wheat- and rye-derived products contain the highest fodmap content, predominantly fructans and galacto-oligosaccharides [14••]. Cereal products with the lowest fodmap contents are mostly gluten-free, based on rice, oat, quinoa and corn ingredients.
Other Components
Little attention has been paid to the lipid component (1–2 %) of wheat, nor to other constituents such as polyphenols contained within whole grains. Wheat also contains lectin activity and wheat germ agglutinin (WGA) is the best studied (reviewed in [15•]). This binds to N-glycolylneuraminc acid found in cell membranes in epithelia of the gut. It can be taken up by the epithelium transcellularly via endocytosis or paracellularly. In studies in vitro, WGA in nanomolar concentrations has several pro-inflammatory effects on a variety of cells in vitro and increases epithelial permeability in cell lines. However, a pathogenic role for WGA in changes in IBS, for example, by changing intestinal permeability or inducing symptoms, is unexplored.
Clinical Problems
There are three clinical conditions in which wheat has a pathogenic role in either the underlying disease or in causing the symptoms.
Irritable Bowel Syndrome
IBS affects approximately 10 % of population across the world [16] and is characterized by abdominal pain, bloating, wind, distension and altered bowel habit but with no abnormal pathology. Although there has been no single biological abnormality identified to explain the recurrence of symptoms in IBS, the physiological bases for the genesis of many functional gut symptoms are likely to be an excessive response to sensory input to the intestine (termed visceral hypersensitivity) and/or abnormal motility responses to such stimulation. Since luminal distension is a major stimulus to the gut via stretch receptors, factors that induce luminal distension, particularly the ingestion of fodmaps, will act as important inducers of symptoms. A diet low in fodmaps provides relief of such functional gut symptoms in three out of four patients with IBS, evidence for efficacy spanning observational, comparative, randomised and blinded placebo-controlled trials (as recently reviewed) [12•]. Indeed, in Australia and other countries, the low fodmap diet is increasingly being accepted as the primary management strategy for IBS, and has been recently adopted by the 2011 Australian National Therapeutic Guidelines [17].
Celiac Disease
Dietary gluten unequivocally causes celiac disease, a common immune-mediated disease that affects 1 % of Western populations and variable proportions across the world [18]. The immune response triggered is specific to toxic peptides within the gliadin fraction of the gluten protein [19] and initiates an immune response causing mucosal inflammation and injury in the small intestine. The damage in the small intestine can cause common functional gastrointestinal symptoms (diarrhea, constipation, excessive wind, bloating) that may or may not relate to malabsorption. Celiac disease patients are exposed to the risk of a wide range of long-term complications from osteoporosis to infertility to lymphoma [20].
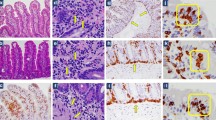
As recently reviewed [21•], the pathological process of celiac disease is well understood where, in the small intestine, gliadin escapes degradation and undergoes post-translational modification (deamidation) by tissue transglutaminase (tTG) forming negatively charged amino acids. These bind to the disease-associated human leukocyte antigen (HLA)-DQ2 or -DQ8 receptors on the cell surface of antigen-presenting cells. Once bound, this complex is presented with high affinity to T-cells. The CD4+ T-cell activation leads to the secretion of pro-inflammatory cytokines, inflammation and damaged intestinal villi.
The immunogenicity of α-gliadin is under control of the HLA genes [22], where the genetic susceptibility locus (HLA-DQ2 and/or HLA-DQ8) is expressed in 99.4 % of celiac patients [23, 24]. Given this genetic association, high-risk groups for celiac disease include relatives of celiac patients and those with co-existing autoimmune conditions, including insulin-dependent diabetes mellitus, Down’s syndrome, multiple sclerosis, and Williams or Turner syndrome [25].
The prevalence of celiac disease appears to be increasing. The most likely contributors to this are an increase in clinical awareness and an improved definition and improvements in diagnostic tests, although evidence is suggesting there is an unexplained real increase [26]. Despite this, celiac disease remains undiagnosed in the majority of patients, where it is estimated that there are approximately 7–10 undiagnosed cases for each diagnosed celiac patient [27]. As outlined in Table 2, the diagnosis of celiac disease is made using a combination of (1) histological findings from small bowel biopsy (via gastroscopy) including villous atrophy, crypt hyperplasia and intra-epithelial lymphocytosis; (2) raised circulating levels of celiac disease-associated antibodies (serology) such as transglutaminase IgA; (3) histological, serological or clinical improvement after adherence to a gluten-free diet (GFD); and (4) specific allelic variants in the two HLA genes: HLA-DQA and HLA-DQB [28••, 29••, 30–33]. Controversy lies in the ‘grey’ area where, for example, only duodenal intra-epithelial lymphocytosis is present or serology is suggestive but biopsy is negative.
The only available treatment for celiac disease is life-long strict avoidance of all gluten-containing foods. As little as 50 mg (present in 1/80th of a slice of wheat bread) is generally considered to be the minimum quantity of gluten needed to induce damage to the lining of the small intestine [34]. Clinical effectiveness of the GFD as treatment for celiac disease is well documented, including for clinical improvement of symptoms and nutrition, healing of the intestinal lesion in many and prevention of long-term complications [20]. Recent guidelines for patient management with celiac disease have been published by the British Society and the American College of Gastroenterology [30, 32, 33].
Food Hypersensitivity
There is little doubt that wheat can cause food hypersensitivity reactions, but how commonly this occurs in controversial. There are two apparent varieties of wheat hypersensitivity.
-
‘Wheat allergy’: This has been classified into classical food allergy affecting the skin, gastrointestinal tract or respiratory tract; wheat-dependent, exercise-induced anaphylaxis (WDEIA); occupational asthma (baker’s asthma) and rhinitis; and contact urticaria [28••]. There has been little progress in understanding the mechanisms of food allergy, particularly those involved at the molecular level. It is thought that wheat allergy involves cross-linking of immunoglobulin E (IgE) by repeat sequences in gluten peptides, which triggers the release of chemical mediators including histamine from basophils and mast cells [35]. There is no direct evidence to suggest that classical IgE-mediated type 1 allergic reactions to food antigens play a role in the symptoms of IBS [36].
-
‘Wheat sensitivity’: This has been defined in 30 % of a large cohort of patients with IBS by an Italian group according to exclusion diet, double-blind, placebo-controlled, re-challenge methodology [37••]. Evidence that this is an inflammatory/immune-mediated phenomenon has comprised the association with atopic phenotype, the induction of symptoms with only small amounts of wheat (i.e. could not be fodmaps), the finding of eosinophilic infiltration of the small and large intestinal mucosa and, interestingly, the intraepithelial compartment in about one-third of patients, the presence of anti-gliadin antibodies in about 40 %, and the presence of eosinophilic cationic protein in faeces and a positive basophil activation test in the majority of patients [38, 39, 40•]. The authors identified two varieties—those whose hypersensitivity was specific to wheat and those who had multiple food hypersensitivities. Reservations about these data include the almost lack of placebo responses in these patients during food challenges (unusual in this patient population), and the lack of information about the effectiveness of wheat-free dietary approaches in the short or long term. The data need confirmation by an independent group.
The Not-So-New Clinical Entity of Non-Celiac Gluten Sensitivity
The term ‘non-celiac gluten sensitivity’ (NCGS), has recently reached consensus agreement in terms of its name and the diagnostic criteria [28••, 29••]. Patients are considered to be NCGS if celiac disease has been excluded and if the gastrointestinal IBS-like symptoms markedly improve on a GFD. Stricter criteria could also be the absence of evidence of allergic or immune mechanisms, or a positive response to blinded, placebo-controlled gluten challenge. Even though the term was only agreed upon recently, the entity has been talked about for decades.
Evaluation of ‘exclusion diets’ has consistently shown wheat to be one of the most common factors inducing GI symptoms [41]. Dickerson and colleagues first identified that wheat may cause different kinds of chronic ill-health in individuals without celiac disease in 1978 [42]. Ellis and Linaker described normal biopsies and normal lymphocyte counts existing in combination with rapid disappearance of symptoms when their patients withdrew gluten from the diet [43]. Cooper and colleagues also described patients experiencing gluten-sensitive diarrhea, but without celiac disease [44]. These early descriptions did not acknowledge the presence of other components of wheat, particularly fructans, or wheat sensitivity that might be responsible for the symptoms.
The frequency of patients presenting with IBS-type symptoms similar to celiac disease who are reportedly responding well to a GFD, but have no other clinical or diagnostic biomarkers of celiac disease, is increasing and has been suggested to affect up to 15 % of the population [45]. The growing gluten-free market may now be between 15–20 % of the population, those with celiac disease being a minority contributor [46]. Gluten has also been linked to a wide range of conditions other than IBS as above. There is also considerable emotive power behind gluten as a causative agent and now commercial interests add to that pressure. There is an urgent need for quality evidence.
Evidence from In Vitro and Animal Studies
Studies in vitro and animal experiments may provide clues to possible mechanisms that can be applied to subsequent human studies. Gliadin has been shown in vitro to increase epithelial permeability and alter protein expression of components of the tight junctions in Caco-2 cell monolayers, used as a surrogate model for the human gut epithelium [47]. Gliadin also induced apoptosis [48, 49] and increased oxidative stress in that cell line [50]. Studies using animal models of gluten-sensitivity (not celiac disease) have also directly investigated the role of gluten challenge in inducing gut dysfunction [48], and changes in neuromotor function and microbiota independently of inducing intestinal inflammation or injury were reported [51].
Evidence from Clinical Studies
Studies from several groups have attempted to characterize the phenotypic, genotypic and immune markers of patients with NCGS, where the diagnosis has been based upon a response to GFD, but without evidence of celiac disease. A group from Germany identified a sub-group of patients with diarrhea-predominant IBS who carried the HLA-DQ2 allele, did not have villous atrophy on duodenal biopsy, had varying pathological, immunological (positive IgA anti-gliadin or anti-TTG antibodies and increased density of IELs) and who had symptomatic improvement on a GFD [52, 53]. In two other studies, HLA-DQ2 was not overrepresented in the NCGS cohort studied [54, 55••]. Sapone et al. provided evidence that abnormalities of innate immunity without epithelial barrier dysfunction of the intestinal mucosa were found in NCGS in contrast to patients with celiac disease [56]. A study from Bologna reported 56 % of 78 patients with NCGS had IgG AGA antibodies with mostly negative specific celiac antibodies, although many of the patients had abnormalities on duodenal histopathology [57]. In an older study, immunological markers (including serum IgE, eosinophil counts, histamine release) have appeared normal in NCGS [41]. Finally, a recent comparative study of a cohort of patients with diarrhea-predominant IBS suggested that patients had improved stool frequency on gluten-free, but not gluten-containing, diet and that intestinal permeability was worse on the gluten-containing diet [58•]. This observation was consistent with the effects of gliadin on cell monolayers (see above) but inconsistent with reduced permeability reported in another study where patient selection was quite different [56]. All the studies above have suffered from methodological limitations that include the fact that varying proportions of the patients studied would now be considered to have celiac disease. Furthermore, the specificity of observations to gluten itself (rather than GFD), while implied by the investigational teams, was not demonstrated.
Recently, a series of interventional re-challenge studies from Australia were designed to address the issues of whether gluten can specifically induce symptoms and whether current diagnostic criteria for NCGS are actually identifying patients with NCGS. Two important methodological innovations were included. First, the gluten used was free from contamination by carbohydrates with the potential to induce symptoms (i.e. it was devoid of fodmaps). Secondly, celiac disease had been definitively excluded by accepting only patients with normal duodenal histology and negative serology, or those who were HLA-DQ2/8 negative. Additionally, the second report assessed all patients by utilising an assay that can identify with high sensitivity patients with celiac disease who are currently on a GFD. The first study was a randomised double-blind, placebo-controlled trial of a single dose of gluten (16 g/day) without a controlled dietary background in parallel groups [55••]. Thirty-four patients were randomised to receive two slices of gluten-free bread and one gluten-free muffin, either with or without gluten added, over 6 weeks, whilst continuing their usual GFD. The test foods were indistinguishable and were fodmap-free. The gluten group had greater gastrointestinal symptoms and tiredness induced compared to those induced in the placebo group within the first week. There were no differences for intestinal permeability, faecal lactoferrin and highly sensitive C-reactive protein, and no elevated celiac antibodies. These results were considered the first specific evidence towards the existence of NCGS.
The same research group went onto conduct a follow-up dietary trial in identically selected patients using a crossover design and supplying a controlled diet [59••]. Following a 2-week run-in period on a low fodmap diet, 37 patients with NCGS and IBS who were symptomatically controlled on a GFD underwent a double-blind, placebo-controlled, randomised crossover trial of placebo, low-gluten (2 g/day) or high-gluten (16 g/day) for 1 week, followed by a 2-week washout period, before crossing over to the next diet. All meals and snacks were provided. The food was low in fodmaps and gluten-free, and protein levels were balanced with whey protein. Symptoms consistently and significantly improved on restriction of fodmap intake, but significantly worsened to a similar degree during each dietary treatment period, irrespective of diet. Only six participants (16 % of total cohort) had symptoms significantly induced on the high-gluten arm. A subject-expectancy or order effect was found with the first intervention inducing greater symptomatic changes than the second or third challenges, regardless of what it contained. There were no changes in celiac serology, faecal concentrations of eosinophil cationic protein, calprotectin or human ß-defensin-2, or any gliadin-specific T-cells induced. There were no differences in any end-point in those with and without DQ2/DQ8.
A double-blind, placebo-controlled, randomised crossover re-challenge was then conducted in 22 of these patients, where they were randomized to receive gluten (16 g/day), whey (16 g/day) or placebo for 3 days each, with a minimum 3-day washout [59••]. All food was provided, but in addition to the food being low in fodmaps and gluten-free, dairy products and food chemicals were also controlled to minimise all potential triggers of gut symptoms. The results showed poor reproducibility of symptom induction to a specific protein. Moreover, only two participants had symptoms significantly induced on the gluten arm in the 3-day re-challenge, and they were not the same two participants who had a positive response to the gluten (16 g/day) arm in the 7-day trial. A very high nocebo response was found in both trials, regardless of all background dietary triggers being controlled. Either the patients did not have NCGS as self-reported or the trial design precluded its recognition. It may also be possible that gluten may not be a specific trigger of functional gut symptoms once dietary fodmaps are reduced.
Conclusions
Non-celiac gluten sensitivity is an entity awaiting validation, better diagnostic criteria, and, if it does exist, pathogenic mechanisms. Progress will only ensue if the methodologies for the design and execution of studies, and their interpretation markedly improve. The reluctance to acknowledge other components of wheat, such as fructans, non-gluten proteins and WGA, as potential pathogenic factors has often hampered good interpretation of clinical observations. Essential rules for future studies should include the following. First, celiac disease has to be seriously excluded by HLA studies and/or strict histological and immunological criteria. The inclusion of patients with intraepithelial lymphocytosis will always raise the issue of whether they really have celiac disease with a milder intestinal lesion. Secondly, the use of blinded placebo-controlled food re-challenge methodology to prove gluten sensitivity is present is not reliable, especially in patients who believe they have NCGS. Perhaps the selection of patients for study should be those with IBS naïve to a GFD. Thirdly, the trap of assuming that response to a GFD or exacerbation of symptoms due to a gluten-containing diet reflects specific effects of gluten should be outlawed and credence be given to the other wheat-related food constituents that can also cause gastrointestinal symptoms. Perhaps if these rules were followed, we would now be a lot closer to defining mechanisms by which gluten might act, might have developed biomarkers to identify patients who truly do have NCGS and perhaps, most importantly, answered the question of whether NCGS does really exist. On current evidence the existence of the entity of NCGS remains unsubstantiated.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fry L. Dermatitis herpetiformis. In: Marsh M, editor. Coeliac disease. Oxford: Blackwell Scientific Publications; 1992.
Hadjivassiliou M, Grunewald RA, Davies-Jones GAB. Gluten sensitivity as a neurological illness. J Neurol Neurosurg Psychiatry. 2002;72(5):560–3.
Dickey W, Kearney N. Overweight in celiac disease: prevalence, clinical characteristics, and effect of a gluten-free diet. Am J Gastoenterol. 2006;101(10):2356–9.
Lucarelli S, Frediani T, Zingoni AM, Ferruzzi F, Giardini O, Quintieri F, et al. Food allergy and infantile autism. Panminerva Medica. 1995;37(3):137–41.
Hadley SK, Gaarder SM. Treatment of irritable bowel syndrome. Am Fam Physician. 2005;72(12):2501–6.
Wieser H. Chemistry of gluten proteins. Food Microbiol. 2007;24(2):115–9.
• Junker Y, Zeissig S, Kim SJ, Barisani D, Wieser H, Leffler DA, et al. Wheat amylase trypsin inhibitors drive intestinal inflammation via activation of toll-like receptor 4. J Exp Med. 2012;209(13):2395–408. Demonstration of a proinflammatory effect of a non-gluten protein in wheat.
• Eswaran S, Muir J, Chey WD. Fiber and functional gastrointestinal disorders. Am J Gastroenterol. 2013;108:718–27. Up-to-date review of fibre and its potential in symptom induction and therapy in functionial gastrointestinsl disorders.
Kelly G. Inulin-type prebiotics: a review. (Part 2). Altern Med Rev. 2009;14:36–55.
Gibson PR, Newnham E, Barrett JS, Shepherd SJ, Muir JG. Review article: fructose malabsorption and the bigger picture. Aliment Pharmacol Ther. 2007;25(4):349–63.
Barrett JS, Gearry RB, Muir JG, Irving PM, Rose R, Rosella O, et al. Dietary poorly absorbed, short-chain carbohydrates increase delivery of water and fermentable substrates to the proximal colon. Aliment Pharmacol Ther. 2010;31(8):874–82.
• Shepherd SJ, Lomer MC, Gibson PR. Short-chain carbohydrates and functional gastrointestinal disorders. Am JGastroenterol. 2013;108(5):707–17. Up-to-date review of short-chain carbohydrates on functional gastrointestinal disorders focussing mostly on fodmaps.
• Monash University Low FODMAP App (homepage on the internet). Melbourne, Monash University. Available from: http://www.med.monash.edu/cecs/gastro/fodmap/iphone-app.html. Recently released app containing up-to-date listing of the fodmap content of foods as found on the Monash University database.
•• Biesiekierski JR, Rosella O, Rose R, Liels K, Barrett JS, Shepherd SJ, et al. Quantification of fructans, galacto-oligosacharides and other short-chain carbohydrates in processed grains and cereals. J Hum Nutr Diet 2011;24(2):154–76. Demonstration that gluten-containing grains are rich in fructans and vice-versa.
• de Punder K, Pruimboom L. The dietary intake of wheat and other cereal grains and their role in inflammation. Nutritents. 2013;5:771–87. Useful review with particular reference to wheat germ agglutinin to remind that potentially pathogenic lectins are also present in wheat.
Quigley EM, Abdel-Hamid H, Barbara G, Bhatia SJ, Boeckxstaens G, De Giorgio R, et al. A global perspective on irritable bowel syndrome: a consensus statement of the World Gastroenterology Organisation Summit Task Force on irritable bowel syndrome. J Clin Gastroenterol. 2012;46:356–66.
Anonymous. Therapeutic Guidelines: Gastrointestinal Version 5, 2011, Therapeutic Guidelines Limited: Melbourne, Australia.
Catassi C, Anderson RP, Hill ID, Koletzko S, Lionetti E, Mouane N, Schumann M, Yachha SK. World perspective on celiac disease. J Pediatr Gastroenterol Nutr 2012;55(5):494–9.
Anderson RP et al. In vivo antigen challenge in celiac disease identifies a single transglutaminase-modified peptide as the dominant A-gliadin T-cell epitope. Nat Med. 2000;6(3):337–42.
Haines ML, Anderson RP, Gibson PR. Systematic review: the evidence base for long-term management of coeliac disease. Aliment Pharmacol Ther. 2008;28(9):1042–66.
• Kupfer SS, Jabri B. Pathophysiology of celiac disease. Gastrointest Endosc Clin N Am. 2012;22:639–60. Up-to-date review on developments in the pathogenesis of celaic disease in terms of genetics, immunology and environment.
Kagnoff MF. Two genetic loci control the murine immune response to A-gliadin, a wheat protein that activates coeliac sprue. Nature. 1982;296(5853):158–60.
Lundin KE, Scott H, Hansen T, Paulsen G, Halstensen TS, Fausa O, et al. Gliadin-specific, HLA-DQ(alpha 1*0501, beta 1*0201) restricted T cells isolated from the small intestinal mucosa of celiac disease patients. J Exp Med. 1993;178(1):187–96.
Lundin KE, Gjertsen HA, Scott H, Sollid LM, Thorsby E. T cells from the small intestinal mucosa of a DR4, DQ7/DR4, DQ8 celiac disease patient preferentially recognize gliadin when presented by DQ8. Hum Immunol. 1994;41(4):285–91.
Sollid LM. Coeliac disease: dissecting a complex inflammatory disorder. Nat Rev Immunol. 2002;2(9):647–55.
Catassi C, Kryszak D, Bhatti B, Sturgeon C, Helzlsouer K, Clipp SL, et al. Natural history of celiac disease autoimmunity in a USA cohort followed since 1974. Ann Med. 2010;42(7):530–8.
Holtmeier W, Caspary WF. Celiac disease. Orphanet J Rare Dis. 2006;1:3.
•• Sapone A, Bai JC, Ciacci C, Dolinsek J, Green PH, Hadjivassiliou M, et al. Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Med. 2012;10:13. Important international effort to provide consensus opinion on a classification of gluten-related disorders.
•• Ludvigsson JF, Leffler DA, Bai JC, Biagi F, Fasano A, Green PH, et al. The Oslo definitions for coeliac disease and related terms. Gut. 2013;62(1):43–52. Important international effort to define various issues in celiac disease.
Husby S, Koletzko S, Korponay-Szabó IR, Mearin ML, Phillips A, Shamir R, et al. ESPGHAN Working Group on Coeliac Disease Diagnosis; ESPGHAN Gastroenterology Committee; European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol Nutr. 2012;54(1):136–60.
Rubio-Tapia A, Hill ID, Kelly CP, Calderwood AH, Murray JA. ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol. 2013;108:656–76.
Bai JC, Fried M, Corazza GR, Schuppan D, Farthing M, Catassi C, et al. World gastroenterology organisation global guidelines on celiac disease. J Clin Gastroenterol. 2013;47(2):121–6.
Catassi C, Fabiani E, Iacono G, D'Agate C, Francavilla R, Biagi F, et al. A prospective, double-blind, placebo-controlled trial to establish a safe gluten threshold for patients with celiac disease. Am J Clin Nutr. 2007;85(1):160–6.
Tanabe S. Analysis of food allergen structures and development of foods for allergic patients. Biosci Biotechnol Biochem. 2008;72(3):649–59.
Brandtzaeg P. Food allergy: separating the science from the mythology. Nat Rev Gastroenterol Hepatol. 2010;7(7):380–400.
•• Carroccio A, Mansueto P, Iacono G, Soresi M, D’Alcamo A, Cavataio F, et al. Non-celiac wheat sensitivity diagnosed by double-blind placebo-controlled challenge: exploring a new clinical entity. Am J Gastroenterol. 2012;107(12):1898–906. Provocative study suggesting that many patients with irritable bowel syndrome have wheat hypersensitivity, many having specific histopathological findings. The findings need to be reproduced at other centres.
Carroccio A, Brusca I, Mansueto P, Pirrone G, Barrale M, Di Prima L, et al. A cytologic assay for diagnosis of food hypersensitivity in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2010;8(3):254–60.
Carroccio A, Brusca I, Mansueto P, Soresi M, D’Alcamo A, Ambrosiano G, et al. Fecal assays detect hypersensitivity to cow’s milk protein and gluten in adults with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2011;9(11):965–71.
• Carroccio A, Brusca I, Mansueto P, D’alcamo A, Barrale M, Soresi M, et al. A comparison between two different in vitro basophil activation tests for gluten- and cow’s milk protein sensitivity in irritable bowel syndrome (IBS)-like patients. Clin Chem Lab Med. 2013;51(6):1257–63. Study confirming the potential value of the basophil activation test in identifying patients with wheat intolerance and irritable bowel syndrome.
Jones VA. Food intolerance: A major factor in the pathogenesis of irritable bowel syndrome. Lancet. 1982;2(8308):1115–7.
Dickerson JWT, Ballantine L, Hastrop K. Food allergy. Lancet. 1978;1(8061):773.
Ellis A, Linaker BD. Non-coeliac gluten sensitivity? Lancet. 1978;1(8061):1358.
Cooper BT, Holmes GK, Ferguson R, Thompson RA, Allan RN, Cooke WT Gluten-sensitive diarrhea without evidence of celiac disease. Gastroenterology. 1980;79:801–6.
Suter D, Fleming F. Cereal food allergy issues, opportunities and the way forward for industry. in 41st AIFST Convention. 2008. Sydney, Australia.
Vinning G,McMahon G. Gluten-free Grains. A demand-and-supply analysis of prospects for the Australian grains industry. Rural industries Research and Development Corporation: Canberra. 2006. 21(5): p. 359–65.
Sander GR, Cummins AG, Powell BC. Rapid disruption of intestinal barrier function by gliadin involves altered expression of apical junctional proteins. FEBS Lett. 2005;579(21):4851–5.
Giovannini C, Sanchez M, Straface E, Scazzocchio B, Silano M, De Vincenzi M. Induction of apoptosis in Caco-2 cells by wheat gliadin peptides. Toxicology. 2000;145(1):63–71.
Hadjivassiliou M, Williamson CA, Woodroofe N. The immunology of gluten sensitivity: Beyond the gut. Trends Immunol. 2004;25(11):578–82.
Rivabene R, Mancini E, DeVincenzi M. In vitro cytotoxic effect of wheat gliadin-derived peptides on the Caco-2 intestinal cell line is associated with intracellular oxidative imbalance: implications for coeliac disease. Biochim Biophys Acta. 1999;1453:152–60.
Verdu EF, Huang X, Natividad J, Lu J, Blennerhassett PA, David CS, et al. Gliadin-dependent neuromuscular and epithelial secretory responses in gluten-sensitive HLA-DQ8 transgenic mice. Am J Physiol Gastrointest Liver Physiol. 2008;294(1):G217–25.
Wahnschaffe U, Ullrich R, Riecken EO, Schulzke JD. Celiac disease-like abnormalities in a subgroup of patients with irritable bowel syndrome. Gastroenterology. 2001;121:1329–38.
Wahnschaffe U, Schulzke JD, Zeitz M, Ullrich R. Predictors of clinical response to gluten-free diet in patients diagnosed with diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol. 2007;5(7):844–50.
Picarelli A, Maiuri L, Mazzilli MC, Coletta S, Ferrante P, Di Giovambattista F, et al. Gluten-sensitive disease with mild enteropathy. Gastroenterology. 1996;111:608–16.
•• Biesiekierski JR, Newnham ED, Irving PM, Barrett JS, Haines M, Doecke JD, et al. Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am J Gastroenterol. 2011;106(3):508–14. The first randomised controlled parallel-group re-challenge trial of fodmap-deplete gluten in patients with self-perceived non-celiac gluten sensitivity showing gluten-specific induction of gastrointestinal symptoms and tiredness. Mechansism were not identified.
Sapone A, Lammers KM, Casolaro V, Cammarota M, Giuliano MT, De Rosa M, et al. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: Celiac disease and gluten sensitivity. BMC Med. 2011;9:23.
Volta U, Tovoli F, Cicola R, Parisi C, Fabbri A, Piscaglia M, et al. Serological tests in gluten sensitivity (nonceliac gluten intolerance). J Clin Gastroenterol. 2012;46(8):680–5.
• Vazquez-Roque MI, Camilleri M, Smyrk T, Murray JA, Marietta E, O'Neill J, et al. A controlled trial of gluten-free diet in patients with irritable bowel syndrome-diarrhea: effects on bowel frequency and intestinal function. Gastroenterology. 2013;144(5):903–11. Detailed study of gluten-containing and gluten-free diets in patients with diarrhea-predominant irrtiable bowel sydnrome, indicating that intestinal permeability is higher on the gluten-containing diet. However, the effect was not defined as gluten-specific.
•• Biesiekierski JR, Peters SL, Newnham ED, Rosella O, Muir JG, Gibson PR. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology. 2013;145(2):320–328. Cross-over, re-challenge study of fodmap-deplete gluten in patients with self-perceived non-celiac gluten sensitivity on a low fodmap background. Diets were rigorously controlled. While patients did improve on initial fodmap restriction, no gluten-specific effect on gastrointestinal symtpoms was identified.
Compliance with Ethics Guidelines
Conflict of Interest
Jessica R. Biesiekierski, Jane G. Muir, and Peter R. Gibson declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with animal subjects performed by the authors. With regard to the authors’ research cited in this paper, all procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Biesiekierski, J.R., Muir, J.G. & Gibson, P.R. Is Gluten a Cause of Gastrointestinal Symptoms in People Without Celiac Disease?. Curr Allergy Asthma Rep 13, 631–638 (2013). https://doi.org/10.1007/s11882-013-0386-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11882-013-0386-4