Abstract
Many epidemiological studies have shown that airborne particulate matter (PM) is a risk factor for multiple respiratory diseases and increased hospitalization rates. Fine PM (PM2.5, diameter <2.5 μm) is considered to be a greater health hazard than coarse PM (PM10, 2.5–10 μm) because it adsorbs more harmful substances and can enter deeper parts of the lungs. We investigated the correlation between hospitalization for pneumonia and PM2.5 levels in Shijiazhuang, a city in northern China. Daily data on hospitalizations for community-acquired pneumonia and ambient air pollution levels in Shijiazhuang were obtained for 2013. A bidirectional case-crossover design was used to investigate the association between hospitalization for pneumonia and atmospheric PM2.5, PM10, SO2, NO2, CO, and O3 levels. The effects of pollutant levels from lag0 (day of hospitalization) to lag5 (five days before lag0) were investigated in both single and multi-pollutant models, adjusted for daily weather variables. For the single-pollutant model, hospitalization for pneumonia correlated positively with higher PM2.5 levels, with an increase of 1.1 % in daily admissions per 10-μg/m3 increase in the PM2.5 level at lag0. In the multi-pollutant model, the observed effects of PM2.5 remained significant. Stratified analysis of exposure based on sex, age, season, and comorbidities showed that the effect of PM2.5 on hospitalization for pneumonia was stronger in males, people younger than 60 years, people without comorbidities, and on warm days. These results indicate that higher levels of PM2.5 increase the risk of hospitalization for pneumonia in Shijiazhuang, China.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A large number of epidemiological studies have confirmed the hazards of airborne particulate matter (PM) on human health (Pope et al. 2004; Schwartz 2004; Analitis et al. 2006; Samet and Krewski 2007; Le Tertre et al. 2002). Inhalable PM (PM10, measured as PM with an aerodynamic diameter <10 μm) can be divided into three categories: coarse PM (PM2.5–10; aerodynamic diameter of 2.5–10 μm), fine PM (PM2.5; aerodynamic diameter of 0.1–2.5 μm), and ultrafine PM (PM0.1; aerodynamic diameter <0.1 μm). Fine PM has larger surface area, adsorbs more pathogenic microorganisms, aromatic hydrocarbons, and other harmful substances, and can enter the deep parts of the lungs, reaching various levels of bronchioles and depositing inside the alveoli. Thus, fine PM exhibits greater toxicity to humans than coarse PM (Wilson and Suh 1997; Pope and Dockery 2006). Many epidemiological studies have demonstrated that fine PM represents a greater health hazard than coarse PM (Cifuentes et al. 2000; Schwartz et al. 1996; Zanobetti et al. 2009; Liao et al. 2011). As a result, the World Health Organization has recommended that PM2.5, rather than PM10, be used as the major indicator for air quality monitoring (Samet et al. 2006).
Epidemiological studies have found that the rate of hospitalization for pneumonia is closely related to the ambient levels of PM (Chiu et al. 2009). Hospitalization for pneumonia has been reported to increase by 0.84 % per 10-μg/m3 increase in the concentration of PM10 (Medina-Ramon et al. 2006), and by 4 % in the cold season and 12 % in the warm season per quartile increase in PM2.5 (Tsai and Yang 2014). Emergency room admissions have been reported to increase by 3 % per 2-μg/m3 increase in the concentration of PM2.5 (Peel et al. 2005). However, most studies in this field have been carried out in Europe and the USA, while relatively few have been undertaken in Asia. China is a developing country with much more serious air pollution than Europe and other developed countries. Furthermore, it is highly likely that there is considerable heterogeneity in the levels and chemical composition of PM in different regions of China, and that this shows seasonal variation within each region. Since the research findings in Europe and other regions of the world may not apply to China, it is extremely important that the effects of PM2.5 on the rate of hospitalization for pneumonia are studied in China.
Real-time monitoring of PM2.5 levels in China started only recently, in January 2013. This monitoring is being undertaken in 74 cities, and the data are being published to facilitate epidemiological analysis. To date, however, no studies have been published regarding the impact of PM2.5 levels on the rate of hospitalization for pneumonia in China. Therefore, the aim of the present study was to examine the association between the ambient levels of PM2.5 and the rate of hospitalization for pneumonia in residents of Shijiazhuang in 2013, using a case-crossover design.
Materials and methods
City characteristics
This was an epidemiological study conducted in Shijiazhuang, a city located in north China, with a population of approximately 3 million inhabitants. Shijiazhuang has a warm, temperate, continental monsoon climate, with an annual mean temperature of 13 °C (range, −6.5 to 32.5 °C). Shijiazhuang is the second-most polluted city among the 74 cities for which PM2.5 monitoring data has been published in China (Ministry of Environmental Protection of the People’s Republic of China. The State of China’s Environment 2013. http://jcs.mep.gov.cn/hjzl/zkgb/2013zkgb).
Hospital admissions data
This study was approved by the Ethics Committee of The Second Hospital of Hebei Medical University. Written informed consent was obtained from all participants. This retrospective study was carried out in the respiratory departments of the seven main tertiary general hospitals in Shijiazhuang, China. These seven hospitals provide about 70 % of all the tertiary hospital beds for respiratory hospital admissions in Shijiazhuang. Patients were included in the study if they were urban residents of Shijiazhuang aged 18 years or more and had been admitted to hospital for community-acquired pneumonia (CAP) between January 1, 2013 and December 31, 2013. The criteria used for the diagnosis of CAP were those provided by the Chinese Medical Association of Respiratory Diseases (2006). Briefly, CAP was defined as chest X-ray evidence of lobar consolidation, cavitation or parenchymal involvement, with or without pleural effusion; plus at least one of the following: (1) new appearance of cough and/or sputum or aggravation of the symptoms of an existing respiratory disease, with production of a purulent sputum with or without chest pain; (2) fever; (3) signs of lung consolidation or wet rales on auscultation; or (4) white blood cell count >10 × 109/L or <4 × 109/L. In addition, the following diseases were excluded: pulmonary tuberculosis, lung tumor, noninfectious pulmonary interstitial disease, pulmonary edema, pulmonary atelectasis, pulmonary embolism, pulmonary infiltration with eosinophilia, and pulmonary vasculitis. Hospitalizations for both primary occurrence and recurrence of CAP were included. The exclusion criteria were the following: patients who were not urban residents of Shijiazhuang, patients with hospital-acquired pneumonia, patients with aspiration pneumonia, or patients with hypersensitivity pneumonitis.
The collection of data from the seven hospitals was carried out by six resident respiratory physicians, each of whom had at least two years of clinical experience in respiratory medicine and had received training in the collection of data for the study. For each patient, the following information was extracted from the medical records: admission date, age, sex, ethnicity, smoking history, and complications. The total number of patients newly admitted for CAP per day was determined; inpatients at the hospital who had not been newly admitted that day were not included in the figures.
Air pollution and meteorological data
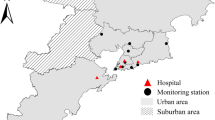
Air pollution data were obtained from the website of the China Environmental Monitoring Center (http://www.cnemc.cn). The data were obtained from seven state-controlled, fully automated monitoring stations for environmental air quality, located in urban (but not rural) regions of Shijiazhuang city (Fig. 1). At each monitoring station, air samples were drawn by sampling pumps into collectors on the roof and transported by pipelines to the analytical devices. The ß-ray method was used to determine the concentrations of PM10 and PM2.5, an ultraviolet fluorescence method was employed to obtain sulfur dioxide (SO2) and ozone (O3) levels, a chemiluminescence method was used to detect nitrogen dioxide (NO2), and a gas filter-correlation infrared absorption method was used to detect carbon monoxide (CO). Each monitoring site provides data on an hourly basis. For each day, the hourly air pollution data from the seven monitoring stations were combined, and the mean hourly values were calculated for each of the pollutants. These mean hourly values were then used to calculate mean daily values for each of the pollutants. Thus, the measurement of pollutant levels was not reliant on random sampling. Daily information on the mean temperature was provided by the Shijiazhuang Meteorological Bureau.
Statistical analysis
A bidirectional case-crossover design (Maclure 1991) was used to assess the influence of exposure to various pollutants on the risk of hospitalization for pneumonia. A time-stratified approach was employed to select control days. Air pollution levels on each of the hospital admission dates were compared with air pollutant levels one week before and one week after the date of admission. The results of previous studies have indicated that an increased number of hospital admissions or emergency room admissions for pneumonia was associated with higher air pollutant levels on the same or previous days, suggesting a lag in the effect of the pollutant (Nascimento et al. 2006; Gouveia et al. 2006; Zanobetti and Schwartz 2006; Santus et al. 2012; Negrisoli and Nascimento 2013). In order to assess pollution exposure, same-day mean exposure and exposures at lagged intervals extending from 1 to 5 days before the case or control event were obtained. Lag0 was defined as the event day, lag1 as the day before the event day, lag2 as the day before lag1, and so forth.
All statistical analyses were performed using the SPSS 19.0 software package (IBM Corp., Armonk, NY, USA). Spearman’s correlation coefficients were calculated to analyze cross-correlations between the various pollutants. The association between hospitalization for pneumonia and levels of PM2.5 was estimated using the odds ratio (OR) and corresponding 95 % confidence intervals (95 % CI), which were calculated using conditional logistic regression with weights equal to the number of hospital admissions on that day. All models included daily temperature as a variable. A single-pollutant model was used initially, and multi-pollutant models were then fitted with different combinations of pollutants to assess the stability of the effect of PM2.5. Stratified analyses of exposure based on age, sex, complications, and season were undertaken to evaluate effect modification. The results of the analyses were expressed as ORs to quantify the increase in risk based on a corresponding increase in exposure of 10 μg/m3 of PM10, 10 μg/m3 of PM2.5, 1 μg/m3 of SO2, 1 μg/m3 of O3, 1 μg/m3 of NO2, and 1 mg/m3 of CO. The warm season was defined as being from April to September. P < 0.05 was considered to indicate statistical significance.
Results
During the study period, there were a total of 2253 hospital admissions for CAP. The distribution of these hospitalizations according to sex, age, season, the presence/absence of comorbidities (including heart disease, diabetes mellitus, and cerebrovascular disease), and the presence/absence of chronic lung disease (including chronic obstructive pulmonary disease, asthma, and bronchiectasis) is presented in Table 1. Among the 2253 patients hospitalized during the study period, 53 % were male, 55 % were aged 60 years or more, and 66 % had comorbidities. All patients were Han Chinese. Figure 2 displays the daily number of hospitalizations for pneumonia for the entire study period and shows that most hospitalizations occurred in August. Over the course of the study period, the mean number of hospital admissions for CAP was 6.17 per day.
Daily number of hospitalizations for pneumonia observed during the study period. The data show the total daily number of hospital admissions for community-acquired pneumonia at the seven hospitals involved in the study (study period: January 1, 2013 to December 31, 2013) together with the corresponding daily PM2.5 levels
Table 2 shows the descriptive statistics (percentiles, interquartile ranges, and means ± standard deviations) for the corresponding environmental data (PM2.5, PM10, SO2, NO2, CO, and O3). PM2.5 and PM10 were observed to be important air pollutants in Shijiazhuang, their mean levels exceeding those of SO2, NO2, and O3. The mean concentration of PM10 was approximately double that of PM2.5 (311 vs. 156 μg/m3). Notably, there were significant variations in the levels of all the pollutants, as shown by the interquartile range values (Table 2).
Calculation of Spearman’s correlation coefficients (Table 3) revealed that there were significant cross-correlations between the various pollutants. PM2.5, PM10, SO2, NO2, and CO all showed significant positive correlations with each other (all P < 0.05), with the strongest associations between PM2.5 and CO (r = 0.92), PM2.5 and PM10 (r = 0.89), and PM10 and CO (r = 0.83). PM2.5, PM10, SO2, NO2, and CO all exhibited significant negative correlations with temperature (all P < 0.05). O3 showed significant negative correlations with the other five pollutants, but was positively associated with temperature (all P < 0.05).
In order to estimate the effects of the individual environmental pollutants on hospitalization for CAP, a single-pollutant model was used to calculate the OR (and 95 % CI) of hospitalization for a 10-μg/m3 increase in PM2.5 or PM10, a 1-μg/m3 increase in SO2, NO2 or O3, or a 1-mg/m3 increase in CO. As shown in Table 4, a 10-μg/m3 rise in PM2.5 was associated with increased odds of hospitalization for pneumonia; the largest effect (OR, 1.011; 95 % CI, 1.005–1.017; P < 0.05) was observed for an increase in PM2.5 on the day of hospitalization (lag0), although significant effects (P < 0.05) were also observed on lag1 to lag5 (Table 4). A 10-μg/m3 rise in PM10 on any of the days from lag0 to lag5 was also associated with an enhanced OR for hospitalization, although the effect of increased PM10 appeared to be numerically smaller than that of PM2.5. Significant effects of increased CO and NO2 on hospitalization for pneumonia were also observed, whereas changes in SO2 or O3 had little or no effect on hospitalization (Table 4).
The stability of the effects of PM2.5 and PM10 was assessed after adjustment for other air pollutants using a multi-pollutant model. As shown in Table 5 and Fig. 3, the effects of PM2.5 on hospitalization for pneumonia remained significant even after accounting for all the other common air pollutants in the multiple-pollutant model. In contrast, in most cases, the effects of PM10 were no longer significant after adjustment for other air pollutants.
Estimates of the effects of fine (PM2.5) and coarse (PM10) particulate matter on hospitalization for community-acquired pneumonia after adjustment for other air pollutants in a multi-pollutant model. Data are plotted as odds ratios and 95 % confidence intervals. Red symbols indicate significant effect, and white symbols non-significant effect. A 10-μg/m3 increase in PM2.5 (upper panel) was associated with a significant effect even after adjustment for other pollutants, whereas a 10-μg/m3 increase in PM10 (lower panel) was in most cases not associated with a significant effect after adjustment for other air pollutants
In order to adjust for possible effect modifiers, further analysis was undertaken with the data stratified for age, sex, the presence/absence of comorbidities, the presence/absence of chronic lung disease, and season. As illustrated in Fig. 4, the effect of a 10-μg/m3 increase in PM2.5 on hospitalization for pneumonia was stronger in males, younger people, people without comorbidities, and on warm days. The effects of a 10-μg/m3 increase in PM10 (lower panel) were significant only in males, older people, people without chronic lung disease, and during the cold season.
Estimates of the effects of fine (PM2.5) and coarse (PM10) particulate matter on hospitalization for community-acquired pneumonia after stratification of data based on possible effect modifiers. Data are plotted as odds ratios and 95 % confidence intervals. Red symbols indicate significant effect, and white symbols non-significant effect. The effect of a 10-μg/m3 increase in PM2.5 (upper panel) appeared to be stronger in males, younger patients, patients without comorbidities or chronic lung disease, and during the warm season. The effects of a 10-μg/m3 increase in PM10 (lower panel) were significant only in males, older patients, patients without chronic lung disease, and during the cold season
Discussion
The present study was designed to investigate the possible association between environmental PM2.5 levels and hospitalization for CAP, during 2013, in urban residents of Shijiazhuang, China. The main findings were that PM2.5 levels were associated with a significant increase in the rate of hospitalization for CAP, with the strongest effect being a 1.1 % increase in the number of daily hospitalizations for a 10-μg/m3 rise in the PM2.5 levels on the day of hospitalization. Furthermore, this effect of PM2.5 remained even after adjustment for other air pollutants (SO2, NO2, CO, and O3). In addition, PM10 was also associated with a higher rate of hospitalization, although the effects were smaller than those of PM2.5 and not as stable after adjustment for other pollutants. Due to the lack of PM2.5 monitoring data before 2013, there is a paucity of epidemiological data specifically addressing the health effects of PM2.5 in China. To the best of our knowledge, the present study is the first to investigate the association between the level of PM2.5 and hospitalization for pneumonia in China. The data in this study reveal that PM2.5 and PM10 were the primary atmospheric pollutants in Shijiazhuang in 2013 and hence, represented the major health hazards. This information may help policy makers to take steps to reduce PM2.5 and PM10 levels in the atmosphere, through appropriate policy interventions and legislations.
The data in this study demonstrate that the levels of PM2.5 and PM10 were positively associated with the daily number of hospitalizations for pneumonia. The observed effects of PM2.5 remained significant even after accounting for other common air pollutants and were strongest at lag0. Investigations of the effects of PM2.5 on hospitalization for pneumonia are rare, and the results have varied between studies. A study in Boston by Zanobetti et al. (Zanobetti and Schwartz 2006) found that the effect of PM2.5 on emergency department admissions for pneumonia was particularly evident at lag0, with a 6.5 % increase in the risk of hospitalization for pneumonia per 17.1-μg/m3 increase in the levels of PM2.5. Another study in the USA determined that emergency department visits for pneumonia increased by 3 % per 2-μg/m3 increase in the levels of PM2.5 (Peel et al. 2005). Santus et al. (Santus et al. 2012) conducted a study in Milan, and their stratified analysis for days lag0–lag2 showed a 10 % risk increase for emergency room admissions due to pneumonia per 10-μg/m3 increase in the levels of PM2.5 during the warm season. In a study in Brazil, a 10-μg/m3 increase in the concentration of PM10 was associated with an increase of nearly 9 % in the risk of pediatric hospitalization due to pneumonia, and the effects of PM10 were strongest at lag4 (Negrisoli and Nascimento 2013). In general, the present study is consistent with the above studies in that it demonstrated significant associations between exposure to PM2.5 and hospital admissions for pneumonia. However, our results differ from those of these previous studies in terms of the magnitude of the effect of PM2.5 and the lag periods. The reasons for these inconsistencies remain unclear but might be related to several factors such as differences between countries in the national healthcare system or in the criteria used for deciding whether or not to admit a patient. Another potentially key factor is the chemical composition of PM2.5 which varies with season and region. Thus, the toxicity of PM2.5 may vary between studies because of differences in its chemical composition (Suh et al. 2011).
The mechanisms through which PM2.5 increases the risk of pneumonia are not fully understood, although hypotheses have been proposed to explain the contribution of PM2.5 to pulmonary pathophysiology. First, PM could impair microbial clearance and pulmonary host defense mechanisms (Clarke et al. 2000; Leonardi et al. 2000) by damaging the mucociliary system of the respiratory tract (Duan et al. 2013; Ferreira-Ceccato et al. 2011), hindering macrophage phagocytosis (Zhou and Kobzik 2007; Lundborg et al. 2001). and causing intense capillary engorgement and loss of epithelium (Knox 2008). Animal studies have supported a role for PM in the impairment of microbial clearance (Phipps et al. 2010). For example, animals infected with Streptococcus pneumoniae and subsequently exposed to concentrated air particles had double the bacterial burden in the lungs 48 h later, compared with animals infected with the bacterium but exposed to filtered air (Zelikoff et al. 1999). Second, PM could induce and sustain alveolar inflammation and thereby aggravate lung diseases via inflammatory mediators and oxidative stress (Samet et al. 2006; Tsai et al. 2013; Ghio et al. 2012). The responses seem to depend on the material adsorbed in the particles, such as metals, organic carbon, ions (sulfates and nitrates), and other biogenic components (Samet et al. 2006).
Stratified analysis of exposure based on sex showed that the effect of PM2.5 on pneumonia admissions was evident both in males and in females, but was stronger in males. The effect of PM10 on hospitalization for pneumonia was statistically significant only in males. Our data appear to be in line with those of previous studies. For example, Zanobetti et al. (Zanobetti et al. 2000) showed that the effect of PM10 on pneumonia admissions tended to be higher for males, while Santus et al. (Santus et al. 2012) reported larger effects of PM2.5 on hospitalization for pneumonia in males. The reasons for the higher risk of PM2.5-associated hospitalization for pneumonia in males may be related to higher smoking rates in males, although the mechanisms are not yet fully understood.
In the present study, stratified analysis based on age showed that the effects of PM2.5 on hospitalization for pneumonia were more important for people younger than 60 years. This finding differs from those of Zanobetti et al. (Santus et al. 2012; Zanobetti et al. 2000). who reported a stronger association between PM2.5 and hospital admission for pneumonia in an elderly population. The elderly may be more susceptible to pollution (Neupane et al. 2010). although our data appears contradictory to this. One possible explanation for our finding is that the elderly population may have a tendency to spend more time indoors at home, thereby reducing outdoor exposure. Indeed, a recent study in China showed that indoor PM levels were lower during the cold season compared with outdoor PM levels, but that the levels were similar during the warm season, probably because people open their windows (Zhang et al. 2015). If so, the actual level of exposure of the elderly to PM2.5 would have been below the monitored concentrations of PM2.5, leading to bias in the results (Katsouyanni et al. 1997; Zeger et al. 2000).
When the data were analyzed by season, effects of PM2.5 on hospitalization for pneumonia were evident on both warm and cold days, but were stronger on warm days. These findings appear to be in agreement with those of previous studies (Santus et al. 2012; Medina-Ramon et al. 2006). The concentrations of PM10 and PM2.5 during the warm season (243.6 ± 96.1 μmol/l and 104.2 ± 56.1 μmol/l, respectively) tended to be lower than those during the cold season (376.2 ± 184.1 μmol/l and 209.0 ± 140.0 μmol/l, respectively). Thus, the stronger effect during the warm season may be related to an increase in individual exposure rather than to an overall increase in the outdoor ambient concentration of pollutant, since people are more likely to go outdoors and open windows in the warm season than in the cold season. Thus, the monitored PM2.5 concentrations may be closer to the actual levels of personal exposure in the warm season than in the cold season (Tsai et al. 2013; Xu et al. 2011).
The stratified analysis also examined whether the effect of PM2.5 on the risk of hospitalization for pneumonia differed depending on the presence of comorbidities (such as heart disease, diabetes mellitus, asthma, and chronic obstructive pulmonary disease). We found that the effects of PM2.5 on hospital admissions for pneumonia were more important for people without comorbidities. Our results differ from the study by Zanobetti et al. (Zanobetti et al. 2000) which showed that people with heart diseases appeared to be at higher risk of a PM10-associated admission for pneumonia, and that people with asthma had twice the risk of hospitalization for PM10-induced pneumonia as people without asthma. Animal studies (Costa and Dreher 1997) have demonstrated that animals with cardiopulmonary diseases have an increased vulnerability to PM10. There are several possible explanations for the apparent difference between our study and that of Zanobetti et al. One relevant factor may be variation in exposure patterns, since people with comorbidities tend to adopt a more indoor lifestyle because of poor cardiorespiratory functions. In addition, the level of exposure to a pollutant is dependent not only on the environmental concentration of PM2.5 and the exposure time but also on the pulmonary ventilation of the individual. People with chronic lung disease often have ventilation defects that could reduce the total load of PM2.5, resulting in the level of exposure of a patient with lung disease being lower than that expected from the monitored PM2.5 concentration. Differences in healthcare systems between countries might also be responsible for the differences in the impact of comorbidities on the effects of PM.
One limitation of the present study is exposure measurement error, which is a common concern in environmental epidemiology. PM2.5 levels were determined from fixed, outdoor monitoring stations, and these values were extrapolated to estimate exposure in individuals. The PM2.5 concentrations were treated as homogenous throughout the city, and variations between locations were not considered. Furthermore, an individual’s exposure to PM2.5 is influenced by a variety of factors including the time he/she spends outdoors and his/her pulmonary ventilation. These types of exposure measurement error would likely lead to underestimation of pollutant effects (Zeger et al. 2000). Another limitation may result from cases of pneumonia treated in outpatient clinics, which did not lead to hospitalization and were not included in the study. Such under-reporting of the occurrence of the disease would also be expected to result in an underestimation of pollutant effects. Finally, the exact composition of the PM was not analyzed. It is possible that the chemicals adsorbed onto PM might have a greater influence on CAP than PM levels. However, further studies are necessary to address this issue.
In conclusion, this study provided evidence that short-term exposure to PM2.5 is associated with increased hospitalization for pneumonia in Shijiazhuang, China.
References
Analitis A, Katsouyanni K, Dimakopoulou K, Samoli E, Nikoloulopoulos AK, Petasakis Y, Touloumi G, Schwartz J, Anderson HR, Cambra K, Forastiere F, Zmirou D, Vonk JM, Clancy L, Kriz B, Bobvos J, Pekkanen J (2006) Short-term effects of ambient particles on cardiovascular and respiratory mortality. Epidemiology 17(2):230–233. doi:10.1097/01.ede.0000199439.57655.6b
Chinese Medical Association of Respiratory Diseases (2006) Guidelines for the diagnosis and management of community-acquired pneumonia. Zhonghua Jie He He Hu Xi Za Zhi 29(10):651–655
Chiu HF, Cheng MH, Yang CY (2009) Air pollution and hospital admissions for pneumonia in a subtropical city: Taipei, Taiwan. Inhal Toxicol 21(1):32–37. doi:10.1080/08958370802441198
Cifuentes LA, Vega J, Kopfer K, Lave LB (2000) Effect of the fine fraction of particulate matter versus the coarse mass and other pollutants on daily mortality in Santiago, Chile. J Air Waste Manag Assoc 50(8):1287–1298
Clarke RW, Antonini JM, Hemenway DR, Frank R, Kleeberger SR, Jakab GJ (2000) Inhaled particle-bound sulfate: effects on pulmonary inflammatory responses and alveolar macrophage function. Inhal Toxicol 12(3):169–186. doi:10.1080/089583700196220
Costa DL, Dreher KL (1997) Bioavailable transition metals in particulate matter mediate cardiopulmonary injury in healthy and compromised animal models. Environ Health Perspect 105(Suppl 5):1053–1060
Duan Z, Du FY, Yuan YD, Zhang YP, Yang HS, Pan WS (2013) Effects of PM2.5 exposure on Klebsiella pneumoniae clearance in the lungs of rats. Zhonghua Jie He He Hu Xi Za Zhi 36(11):836–840
Ferreira-Ceccato AD, Ramos EM, de Carvalho LC Jr, Xavier RF, Teixeira MF, Raymundo-Pereira PA, Proenca Cdos A, de Toledo AC, Ramos D (2011) Short-term effects of air pollution from biomass burning in mucociliary clearance of Brazilian sugarcane cutters. Respir Med 105(11):1766–1768. doi:10.1016/j.rmed.2011.08.003
Ghio AJ, Carraway MS, Madden MC (2012) Composition of air pollution particles and oxidative stress in cells, tissues, and living systems. J Toxicol Environ Health B Crit Rev 15(1):1–21. doi:10.1080/10937404.2012.632359
Gouveia N, de Freitas CU, Martins LC, Marcilio IO (2006) Respiratory and cardiovascular hospitalizations associated with air pollution in the city of Sao Paulo, Brazil. Cad Saude Publica 22(12):2669–2677
Katsouyanni K, Touloumi G, Spix C, Schwartz J, Balducci F, Medina S, Rossi G, Wojtyniak B, Sunyer J, Bacharova L, Schouten JP, Ponka A, Anderson HR (1997) Short-term effects of ambient sulphur dioxide and particulate matter on mortality in 12 European cities: results from time series data from the APHEA project. Air Pollution and Health: a European Approach. BMJ 314(7095):1658–1663
Knox EG (2008) Atmospheric pollutants and mortalities in English local authority areas. J Epidemiol Community Health 62(5):442–447. doi:10.1136/jech.2007.065862
Le Tertre A, Medina S, Samoli E, Forsberg B, Michelozzi P, Boumghar A, Vonk JM, Bellini A, Atkinson R, Ayres JG, Sunyer J, Schwartz J, Katsouyanni K (2002) Short-term effects of particulate air pollution on cardiovascular diseases in eight European cities. J Epidemiol Community Health 56(10):773–779
Leonardi GS, Houthuijs D, Steerenberg PA, Fletcher T, Armstrong B, Antova T, Lochman I, Lochmanova A, Rudnai P, Erdei E, Musial J, Jazwiec-Kanyion B, Niciu EM, Durbaca S, Fabianova E, Koppova K, Lebret E, Brunekreef B, van Loveren H (2000) Immune biomarkers in relation to exposure to particulate matter: a cross-sectional survey in 17 cities of Central Europe. Inhal Toxicol 12(Suppl 4):1–14
Liao D, Shaffer ML, He F, Rodriguez-Colon S, Wu R, Whitsel EA, Bixler EO, Cascio WE (2011) Fine particulate air pollution is associated with higher vulnerability to atrial fibrillation—the APACR study. J Toxicol Environ Health A 74(11):693–705. doi:10.1080/15287394.2011.556056
Lundborg M, Johard U, Lastbom L, Gerde P, Camner P (2001) Human alveolar macrophage phagocytic function is impaired by aggregates of ultrafine carbon particles. Environ Res 86(3):244–253. doi:10.1006/enrs.2001.4269
Maclure M (1991) The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol 133(2):144–153
Medina-Ramon M, Zanobetti A, Schwartz J (2006) The effect of ozone and PM10 on hospital admissions for pneumonia and chronic obstructive pulmonary disease: a national multicity study. Am J Epidemiol 163(6):579–588. doi:10.1093/aje/kwj078
Ministry of Environmental Protection of the People’s Republic of China. The State of China’s Environment 2013. http://jcs.mep.gov.cn/hjzl/zkgb/2013zkgb
Nascimento LF, Pereira LA, Braga AL, Modolo MC, Carvalho JA Jr (2006) Effects of air pollution on children’s health in a city in Southeastern Brazil. Rev Saude Publica 40(1):77–82
Negrisoli J, Nascimento LF (2013) Atmospheric pollutants and hospital admissions due to pneumonia in children. Rev Paul Pediatr 31(4):501–506. doi:10.1590/S0103-05822013000400013
Neupane B, Jerrett M, Burnett RT, Marrie T, Arain A, Loeb M (2010) Long-term exposure to ambient air pollution and risk of hospitalization with community-acquired pneumonia in older adults. Am J Respir Crit Care Med 181(1):47–53. doi:10.1164/rccm.200901-0160OC
Peel JL, Tolbert PE, Klein M, Metzger KB, Flanders WD, Todd K, Mulholland JA, Ryan PB, Frumkin H (2005) Ambient air pollution and respiratory emergency department visits. Epidemiology 16(2):164–174
Phipps JC, Aronoff DM, Curtis JL, Goel D, O'Brien E, Mancuso P (2010) Cigarette smoke exposure impairs pulmonary bacterial clearance and alveolar macrophage complement-mediated phagocytosis of Streptococcus pneumoniae. Infect Immun 78(3):1214–1220. doi:10.1128/IAI.00963-09
Pope CA 3rd, Dockery DW (2006) Health effects of fine particulate air pollution: lines that connect. J Air Waste Manag Assoc 56(6):709–742
Pope CA 3rd, Burnett RT, Thurston GD, Thun MJ, Calle EE, Krewski D, Godleski JJ (2004) Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation 109(1):71–77. doi:10.1161/01.CIR.0000108927.80044.7F
Samet J, Krewski D (2007) Health effects associated with exposure to ambient air pollution. J Toxicol Environ Health A 70(3–4):227–242. doi:10.1080/15287390600884644
Samet JM, Brauer M, Schlesinger R (2006) Particulate matter. In: Word Health Organization, editor. Air quality guidelines: global update 2005. Copenhagen: WHO 217–305
Santus P, Russo A, Madonini E, Allegra L, Blasi F, Centanni S, Miadonna A, Schiraldi G, Amaducci S (2012) How air pollution influences clinical management of respiratory diseases. A case-crossover study in Milan. Respir Res 13:95. doi:10.1186/1465-9921-13-95
Schwartz J (2004) The effects of particulate air pollution on daily deaths: a multi-city case crossover analysis. Occup Environ Med 61(12):956–961. doi:10.1136/oem.2003.008250
Schwartz J, Dockery DW, Neas LM (1996) Is daily mortality associated specifically with fine particles? J Air Waste Manag Assoc 46(10):927–939
Suh HH, Zanobetti A, Schwartz J, Coull BA (2011) Chemical properties of air pollutants and cause-specific hospital admissions among the elderly in Atlanta, Georgia. Environ Health Perspect 119(10):1421–1428. doi:10.1289/ehp.1002646
Tsai SS, Yang CY (2014) Fine particulate air pollution and hospital admissions for pneumonia in a subtropical city: Taipei, Taiwan. J Toxicol Environ Health A 77(4):192–201
Tsai SS, Chang CC, Yang CY (2013) Fine particulate air pollution and hospital admissions for chronic obstructive pulmonary disease: a case-crossover study in Taipei. Int J Environ Res Public Health 10(11):6015–6026. doi:10.3390/ijerph10116015
Wilson WE, Suh HH (1997) Fine particles and coarse particles: concentration relationships relevant to epidemiologic studies. J Air Waste Manag Assoc 47(12):1238–1249
Xu MM, Jia Y, Li GX, Pan XC (2011) Evaluation of personal integrated exposure to fine particle in a community in Beijing. J Environ Health 28(11):941–943
Zanobetti A, Schwartz J (2006) Air pollution and emergency admissions in Boston, MA. J Epidemiol Community Health 60(10):890–895. doi:10.1136/jech.2005.039834
Zanobetti A, Schwartz J, Gold D (2000) Are there sensitive subgroups for the effects of airborne particles? Environ Health Perspect 108(9):841–845
Zanobetti A, Franklin M, Koutrakis P, Schwartz J (2009) Fine particulate air pollution and its components in association with cause-specific emergency admissions. Environ Health 8:58. doi:10.1186/1476-069X-8-58
Zeger SL, Thomas D, Dominici F, Samet JM, Schwartz J, Dockery D, Cohen A (2000) Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Perspect 108(5):419–426
Zelikoff J, Nadziejko C, Fang T, Gordon C, Premdass C, Cohen M (1999) Short-term, low-dose inhalation of ambient particulate matter exacerbates ongoing pneumococcal infections in Streptococcus pneumoniae-infected rats. In: Proceedings of the Third Colloquium on Particulate Air Pollution and Human Health pp 94–101
Zhang Y, He M, Wu S, Zhu Y, Wang S, Shima M, Tamura K, Ma L (2015) Short-term effects of fine particulate matter and temperature on lung function among healthy college students in Wuhan, China. Int J Environ Res Public Health 12(7):7777–7793. doi:10.3390/ijerph120707777
Zhou H, Kobzik L (2007) Effect of concentrated ambient particles on macrophage phagocytosis and killing of Streptococcus pneumoniae. Am J Respir Cell Mol Biol 36(4):460–465. doi:10.1165/rcmb.2006-0293OC
Acknowledgments
This study was supported by the Hebei provincial science and technology plan projects (No. 1527701D).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with ethical standards
This study was approved by the Ethics Committee of The Second Hospital of Hebei Medical University. Written informed consent was obtained from all participants.
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Duan, Z., Han, X., Bai, Z. et al. Fine particulate air pollution and hospitalization for pneumonia: a case-crossover study in Shijiazhuang, China. Air Qual Atmos Health 9, 723–733 (2016). https://doi.org/10.1007/s11869-015-0383-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11869-015-0383-y