Opinion statement
The advances made in the therapeutic management of colorectal cancer (CRC) over recent years with the addition of therapies targeting angiogenesis or cell proliferation have positioned bevacizumab, cetuximab, and panitumumab as accepted first-line treatments when combined with FOLFOX or FOLFIRI for RAS wild-type (WT) metastatic CRC. The question has been raised as to the choice of targeted therapy to maximize chances of an optimal outcome. Three studies, the phase III FIRE-3 (AIO KRK-0306), the phase II PEAK, and the recently presented phase III CALGB/SWOG 80405 trial, have addressed this issue face-on, directly comparing the addition of bevacizumab versus cetuximab or panitumumab to FOLFOX/FOLFIRI in terms of efficacy outcomes. None of these studies met their primary endpoint (response rate, progression-free survival or overall survival respectively), meaning we are no closer to being able to categorically define an optimal targeted treatment in the first-line setting for patients with advanced CRC. This led to reflection over study design and further analyses, raising a number of important issues. High-sensitivity analysis of the mutational status of exons identified a population with a “pure” non-RAS-mutated profile showing benefit with anti-epidermal growth factor receptor (anti-EGFR) combinations, particularly in the context of early and greater depth of response. Coherent with a personalized therapeutic approach, the importance of performing individual high-sensitivity extended RAS testing is unequivocal and is currently a requirement in many countries to identify this all-RAS WT population, thus limiting unnecessary exposure and expense in patients unlikely to respond. These three studies, particularly the CALGB/SWOG 80405 trial, mark an important milestone in the roadmap of metastatic CRC treatment, highlighting the need for close analysis to fully exploit the available data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
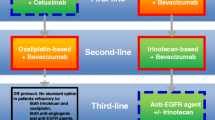
Colorectal cancer (CRC) is one of the leading causes of cancer deaths worldwide (1). Although advances in diagnosis and surgical and systemic therapeutic approaches have ensured major improvements in managing this disease, prognosis remains poor for patients with advanced disease. More recently, a better understanding of the biological hallmarks of CRC has led to the widespread incorporation of targeted therapies designed to specifically interfere with angiogenesis or proliferation pathways, changing the paradigm of metastatic CRC (mCRC). Bevacizumab, a monoclonal antibody directed against vascular endothelial growth factor A (VEGF-A) was approved as a front-line therapy for advanced disease when combined with irinotecan- or oxaliplatin- and fluoropyrimidine-based regimens (2, 3). Cetuximab and panitumumab are anti-epidermal growth factor receptor (anti-EGFR) monoclonal antibodies whose efficacy is dependent on the mutational status of exons 2, 3, and 4 of the KRAS and NRAS oncogenes, with a wild-type (WT) status being mandatory for prescription by regulatory authorities with FOLFOX/FOLFIRI regimens (4•, 5•). In this WT population, irinotecan with infusional 5-fluorouracil (5-FU) was established as the chemotherapy regimen of choice for combination with cetuximab as front-line therapy, whereas oxaliplatin and infusional 5-FU is considered the optimal partner for panitumumab (6), this preference based on the availability of phase III study results.
The value of these targeted agents is not limited to the first-line setting. Favorable efficacy data have been published for bevacizumab in combination with oxaliplatin and infusional 5-FU in the second-line setting after fluoropyrimidine/irinotecan-based chemotherapy, and similar success was reported for bevacizumab administered in combination with chemotherapy as a maintenance strategy after progression under a first-line combination with bevacizumab (7). This concept has been extended even further in the context of anti-EGFR agents, which have been shown to improve clinical outcomes not only in the first- and second-line setting but also in refractory patients (8–14).
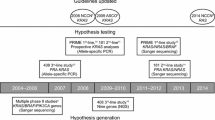
A crucial issue has emerged on the basis of the therapeutic success of these two types of targeted therapies, with the potential for a “preferable choice” between antiangiogenic drugs and anti-EGFR agents in the RAS WT population. Three studies have directly addressed the optimal strategy for managing the KRAS exon 2 WT population by comparing head-to-head bevacizumab versus cetuximab or panitumumab combined with either FOLFIRI or FOLFOX in the first-line setting: the FIRE-3 (AIO KRK-0306) study, the PEAK trial, and the recently presented CALGB/SWOG 80405 (15). We present here the outcomes of these studies including the latest publications/presentations of further analyses driving the identification of patient populations with the greatest potential to benefit from these targeted combination therapies and discuss the potential therapeutic implications for routine patients’ care and challenges to be addressed in new clinical studies.
Treatment
FIRE-3 (AIO KRK-0306)
FOLFOX or FOLFIRI combined with cetuximab or bevacizumab are considered standard first-line treatments for RAS WT mCRC; however, the optimal antibody combination out of the two is unknown. The FIRE-3 trial (also known as AIO KRK-0306) was one of the first studies to shed light to this question (16). FIRE-3 was a randomized phase III trial comparing the efficacy of FOLFIRI in combination with cetuximab or bevacizumab in mCRC patients not pretreated for metastatic disease. The trial was amended after nearly 2 years to restrict inclusion to patients with KRAS exon 2 WT tumors. The primary endpoint of the study was the objective response rate (ORR) as per investigator assessment. Secondary endpoints included progression-free survival (PFS), overall survival (OS), depth of response (DpR), secondary resection of liver metastasis, as well as safety and tolerability.
An intention-to-treat (ITT) analysis was performed in the 592 KRAS exon 2 WT patients included in the study, 297 of whom received FOLFIRI plus cetuximab and 295 who were treated with the bevacizumab combination. The results published after a median of 33 and 39 months of follow-up for each arm, respectively, showed no differences regarding ORR or PFS. Nevertheless, an unexpected statistically significant difference in OS of 3.7 months was reported, favoring cetuximab (28.7 months with cetuximab versus 25.0 months with bevacizumab; HR = 0.77, p = 0.017). Subsequent treatment after progression was equivalent in the two arms, with 78 % of patients in the cetuximab arm and 76 % in the bevacizumab arm receiving second-line therapy, and there were no significant differences regarding biological maintenance or crossover nor the chemotherapy backbone used. The discordance between the lack of significant differences with ORR and PFS versus the significant difference in OS thus cannot be explained by a difference in second-line and further treatments. Nor is it explained by an imbalance in the rate of conversion to resectability since the rate of liver metastasis resections with curative intent was similar in the two groups (12 % with cetuximab and 14 % with bevacizumab).
An expanded RAS analysis was performed in 82.4 % of the ITT population with exon 2 WT, assessing KRAS and NRAS exons 2, 3, and 4 by pyro-sequencing. Efficacy outcomes did not differ for the 342 all-RAS WT population (i.e., WT for exons 2, 3, and 4 of KRAS and NRAS), with no difference in ORR or PFS and confirmation of the OS advantage for the cetuximab-treated population (33.1 months compared to 25.6 months with bevacizumab; HR = 0.70, p = 0.011).
In light of the fact that most published studies show a strong correlation between ORR, PFS, and OS in these parameters for mCRC (17–20), a number of alternative explanations have been proposed to justify this intriguing misalignment between ORR, PFS, and OS in this particular study. Further assessment of efficacy readouts such as independent reviews of ORR, early tumor shrinkage (ETS), or DpR has provided added value in this context. An independent radiological review (IRR) was performed by participating investigators to evaluate tumor response according to RECIST 1.1 (21) and ETS defined as a reduction in tumor diameter of more than 20 % at first tumor assessment after baseline, and DpR considered as the maximal tumor shrinkage compared with baseline (22••). To maximize accuracy, reviewers were blinded to patient data and the analysis was performed in the ITT populations. The IRR in the KRAS exon 2 WT population reported an ORR of 66.5 versus 55.6 % in favor of cetuximab-treated patients. When analyzing the total RAS WT population, ORRs were 72.1 and 56.1 % for the cetuximab- and bevacizumab-containing arms, respectively. The OS benefit was confirmed, again favoring cetuximab (33.1 versus 25.0 months; HR = 0.697, p = 0.0059).
In a further effort to explain these results, the authors correlated ETS and DpR with PFS and OS. Patients with ETS treated with cetuximab achieved a PFS of 9.7 months compared with 5.8 months in patients without ETS. In the bevacizumab arm, PFS was 11.7 and 8.3 months for the ETS and no-ETS groups, respectively. Of note, higher DpR also correlated with improved OS and PFS. The authors concluded that FOLFIRI/cetuximab-treated patients had a significantly higher ORR compared with the FOLFIRI/bevacizumab combination and that both ETS and DpR were associated with prolonged OS and that this effect was more exaggerated with the cetuximab combination.
FIRE-3 provides evidence that front-line therapy based on a combination of FOLFIRI and cetuximab can translate into an OS benefit in the all-RAS WT population, with a more pronounced effect in patients with greater ETS and/or DpR. This study also established the importance of performing expanded RAS testing to ensure optimal patient selection for further studies and to identify patients most likely to benefit from this treatment.
PEAK
While the FIRE-3 study was ongoing, the PEAK trial was initiated comparing panitumumab with bevacizumab using FOLFOX as the backbone chemotherapy in first-line treatment of mCRC patients. This randomized phase II study recruited a KRAS exon 2 WT population, with a primary endpoint of PFS, while secondary objectives included OS, ORR, and outcomes in pre-specified WT RAS patients determined by pyro-sequencing. A total of 285 patients were enrolled, 142 of whom were assigned to the panitumumab-containing regimen and 143 to the bevacizumab combination. The ITT analysis did not show significant differences in terms of PFS, OS, or ORR in the KRAS exon 2 WT population. When considering the all-RAS WT population, an improvement in PFS favoring panitumumab was observed (13.0 months with panitumumab, 9.5 months with bevacizumab; HR = 0.65, p = 0.029). Likewise, a non-significant trend towards better OS was observed in patients treated with panitumumab, with a median OS of 41.3 months in panitumumab-treated patients and 28.9 months in the bevacizumab arm (HR = 0.63, p = 0.058). However, no clinically relevant differences in ORR were observed.
As performed in the FIRE-3 study, an analysis on the impact of ETS and DpR on other efficacy outcomes was conducted. These data were recently presented, and the results were consistent with those of the FIRE-3 study (23). A total of 169 patients with RAS WT mCRC were included in the ORR analysis, and 154 were evaluable for tumor shrinkage. As expected, more patients treated with panitumumab achieved ETS at week 8 compared with the bevacizumab arm (HR = 0.46, p = 0.0259). Tumor shrinkage of 30 % or more was associated with longer median PFS compared to when patients had tumor shrinkage below 30 % (HR = 0.52; 95 % CI 0.29–0.92 versus HR = 0.65; 95 % CI 0.38–1.13, respectively). Similar effects were observed for median OS giving HRs of 0.44; (95 % CI 0.15–1.32) and 0.23 (95 % CI 0.08–0.66) favoring the panitumumab arm. However, it should also be noted that resection rates and outcomes in this subset of patients achieving ETS were similar in the two treatment arms, although the sample size is very small (N = 20). For accurate interpretation of the data, it is important to consider subsequent therapies administered after progression. As it could be anticipated, patients included in the panitumumab arm received further treatment with an anti-EGFR agent in 21 % of cases whereas this was almost double (38 %) in the bevacizumab arm, while conversely, subsequent anti-VEGF-based treatments were 40 and 24 % for the panitumumab and bevacizumab groups, respectively. The use of chemotherapy as well as anti-VEGF agents was also slightly higher in patients treated with panitumumab, and it could be speculated whether this translated into an improved OS.
Thus, the PEAK trial also suggests that RAS WT patients may benefit from an anti-EGFR combination as a first-line therapy relative to anti-VEGF approaches, particularly when an early and deep response is achieved. Strengthening this, these data are consistent with those obtained from the AIO KRK-0306 study. Nonetheless, as a phase II study, PEAK data must be interpreted with caution.
The trial supports for the approach that extensive mutation profiling is mandatory in patients who are candidates for anti-EGFR therapies, although large prospective studies testing formal hypotheses regarding treatment sequences are needed. The results obtained from this study do not call for a change to current clinical practice; however, the fact that outcomes are largely consistent with the FIRE-3 data will ensure that further investigations to address the issue of mutational profiling will be initiated.
CALGB/SWOG 80405
Taken together, the FIRE-3 and PEAK trials suggest that an anti-EGFR-based front-line combination in the all-RAS WT mCRC population could positively impact OS. However, the failed primary endpoint of the phase III FIRE-3 and the phase II design of the PEAK study are major limitations for establishing a formal recommendation. The CALGB/SWOG 80405 trial, performed concurrently with the other two studies, addressed both these issues (19). This academic study is the result of an effort from different cooperative groups: Cancer and Leukemia Group B (CALGB), the Alliance for Clinical Trials in Oncology, and Southwest Oncology Group (SWOG) representing 3,100 institutions and 14,000 investigators across USA and Canada.
This randomized phase III study was designed to demonstrate a benefit in terms of OS for a cetuximab-containing regimen compared with a bevacizumab combination. Patients with mCRC were randomly assigned to receive first-line chemotherapy (FOLFIRI or FOLFOX as per patient and investigator choice) combined with cetuximab, bevacizumab, or both biologicals. The initial design included unselected mCRC patients but was amended after 1420 patients were accrued, to include only KRAS exon 2 WT tumors. The cetuximab/bevacizumab combination arm was also closed given reports of unsatisfactory results for dual VEGF-A and EGFR inhibition (24, 25). Treatment was continued until progression, death, unacceptable toxicity, or curative surgery. A total of 3058 mCRC patients without any molecular selection were included. Among them, 2334 KRAS exon 2 WT patients were randomized and a final sample size amenable for analysis of 1137 was identified. Among the patients with KRAS exon 2 WT tumors, 73 % were treated with FOLFOX and the other 27 % with FOLFIRI.
The primary endpoint of OS was equivalent in the two arms, at 29.0 months (95 % CI 25.7–31.2 months) with bevacizumab/chemotherapy and 29.9 months (95 % CI 27.6–31.2 months) in the cetuximab/chemotherapy arm (HR = 0.92, p = 0.34). Likewise, PFS did not differ between treatments (10.8 months for bevacizumab and 10.4 months for cetuximab; HR = 1.04, 95 % CI [0.91–1.17]; p = 0.55). Analysis according to the chemotherapy backbone also failed to show any substantial differences. For patients treated with FOLFOX, median OS was 26.9 months with bevacizumab (HR = 0.9, 95 % CI [0.7–1.0]; p = 0.09) and 30.1 months when combined with cetuximab. Among patients treated with FOLFIRI, median OS was 33.4 months in patients treated with the antiangiogenic agent and 28.9 months in the cetuximab-treated patients (HR = 1.2, 95 % CI [0.9–1.6]; p = 0.28). It is important to note, however, that the FOLFIRI sample size precluded any firm conclusion from being drawn. An analysis of the ORR assessed by investigators was presented in 733 KRAS exon 2 WT patients (26••), demonstrating a 57 % rate for the bevacizumab-treated population and 66 % in the cetuximab-treated patients.
Resection was possible in 180 KRAS exon 2 WT patients as part of the treatment strategy (26••). Among them, 132 patients achieved non-evidence of disease after chemotherapy and surgery, 82 patients (30 %) in the cetuximab arm and 50 patients (15 %) in the bevacizumab arm. Median OS of these patients was 64.7 months (95 % CI 59.8–78.9) and was not significantly different between arms (67.4 and 64.1 months for cetuximab- and bevacizumab-treated patients, respectively (HR = 1.2). Among the 132 patients, 111 were evaluable for response, 66 with cetuximab and 45 with bevacizumab suggesting that cetuximab-treated patients were more likely to undergo resection.
Extended RAS was tested in RAS exon 2 WT patients using BEAMing magnetic technology with a detection sensitivity of 0.01 % (27••). Among 1137 KRAS exon 2 WT (codons 12 and 13) patients, 621 patients (55 %) could be analyzed for this molecular exploratory objective. The authors found additional 95 patients (15.3 %) with a previously unidentified RAS mutation. The updated results of outcomes based on this analysis showed a median OS beyond 30 months; however, there was still no significant difference between the cetuximab and bevacizumab combinations with chemotherapy (32.0 and 31.2 months, respectively, HR = 0.9, 95 % CI 0.7–1.1; p = 0.40). PFS also did not differ, with 11.4 and 11.3 months for cetuximab and bevacizumab (HR = 1.1, 95 % CI 0.9–1.3; p = 0.31). A higher ORR was achieved in the cetuximab arm in the extended RAS population (68.6 versus 53.6 %; p < 0.01). Analysis of the expanded RAS population among resected patients who achieved no evidence of disease was possible in 82 patients, with new mutations identified in 11 patients (13.4 %) (26). Interestingly, in this subgroup, OS for the all-RAS WT patients was 78.8 months compared with 11.0 months for patients with mutated RAS (HR = 0.52, 95 % CI [0.2–1.4; p = 0.2). The disease-free survival rate was also better, albeit non-significantly, for the all-RAS WT population with 16.1 versus 9.5 months in patients harboring a mutation (HR = 0.84, 95 %; p = 0.60) (15). These data highlight the fact that expanded RAS analysis may identify patients with particularly good prognosis who could benefit from this strategy.
Toxicity profiles were as expected with the most frequent grade 3 or higher toxicities associated with bevacizumab included hypertension (7 %) and gastrointestinal events (2 %), while for cetuximab toxicities included diarrhea (11 %) and acne-like rash (7 %). This toxicity profiles did not translate in major differences in terms of quality of life (QoL) when patients were assessed by the European Organisation for Research and Treatment of Cancer (EORTC) global QoL measure. While the skin rash associated with cetuximab had an effect on a skin satisfaction measure, this did not translate into a significant difference in QoL (15).
Discussion
Taking into account the design and results of these three critical studies, it would appear that we are still far from establishing with any degree of clarity any guidelines for choosing an antiangiogenic over an anti-EGFR treatment or vice versa for combination with the commonly used chemotherapy regimens in the first-line setting in patients with mCRC. The long-awaited results of the CALGB/SWOG trial did not provide a clear answer regarding an optimal treatment strategy. This situation merits further reflection to ensure that any caveats justifying these outcomes are uncovered and exploited where possible.
As a starting point, it should be taken into consideration that the chemotherapy backbones used in the CALGB/SWOG study correspond to the most widely used schedules in mCRC worldwide. The intergroup N9741 study demonstrated that infusional 5-FU plus oxaliplatin (FOLFOX) offered an advantage over irinotecan with bolus fluorouracil and leucovorin (IFL) in terms of both safety and efficacy in this population (28), while a GERCOR study showed that the FOLFOX and FOLFIRI schemas were comparable for efficacy (29). Although the triple FOLFOXIRI regimen developed by the Italian GONO group appeared to give a better outcome compared to FOLFIRI, this has not been widely incorporated into routine clinical practice (30).
A degree of controversy exists regarding the combination of a biologic agent with FOLFOX. The NO16966C phase III trial showed that bevacizumab combined with FOLFOX or XELOX increased PFS with a non-significant improvement in OS (3). The FOLFIRI/bevacizumab combination has not been extensively evaluated with the only direct comparative data coming from the phase III AVF2107 trial clearly showing the superiority of bevacizumab when added to IFL (2). Although the combination of bevacizumab with FOLFIRI has been widely implemented, some doubts exist within the oncology community as to its true benefit. For cetuximab, when combined with FOLFOX, while a statistically significant increase was seen in the ORR and PFS with a trend for OS in the randomized phase II OPUS study (28), the British phase III COIN study did not reproduce these results, showing only a modest increase in ORR (29). Other studies, such as the NORDIC-VII and the recent EPOC trial, have confirmed these conflicting data (30, 31). This initially led to a strong current of questioning as to the clinical value of combining FOLFOX and cetuximab, and this combination was initially excluded from treatment recommendations in some countries. However, when added to FOLFIRI in the CRYSTAL study, cetuximab showed an advantage in all terms of efficacy parameters including OS (4•, 32). The CALGB/SWOG trial had a superiority design for the cetuximab combination, with the primary endpoint being OS. It is important to consider this in context of the time the study was designed (2004), when median OS in academic trials was typically between 21 and 23 months, with the exception of the COIN study (17 months in the cetuximab-treated population) (29). From a statistical standpoint, it could be argued that non-inferiority or an equivalence design would have been a more “pure” approach; however, the large sample size implied by this approach made it unrealistic. The study did not meet its primary endpoint of superiority, with assumptions that there were considered in the target population of patients with KRAS exon 2 WT tumors. There were no differences in either the HR or in the median OS and PFS. Although the sample size was limited, a higher ORR was achieved in the cetuximab arm in the expanded RAS population. However, data regarding DpR and ETS are yet to be presented and are essential for obtaining accurate knowledge about the initial effects of the treatment on tumor burden. When examining the effect of the addition of a biological agent to the different chemotherapy backbones, the results are consistent with the FOLFOX regimen. FOLFOX-cetuximab and FOLFOX-bevacizumab are comparable in this setting although a slight trend favoring the cetuximab arm may be discerned in the second part of the curves. The FOLFIRI results may be less robust as this treatment group only accounts for a quarter of the total population, but nonetheless, FOLFIRI-cetuximab and FOLFIRI-bevacizumab appear comparable.
All combination treatments were well tolerated with some differences in the arms related to class effect toxicities. As expected, patients in the cetuximab arm presented grade 3 skin rash and a higher incidence of diarrhea; nonetheless, the reported rates were lower than in the literature. More patients in the bevacizumab arm presented grade 3 hypertension and venous thromboembolisms. The QoL evaluations showed that although patients treated with cetuximab had a higher degree of dissatisfaction with skin appearance in the first 3 months, this effect did not translate into a significant difference in the global QoL. It is possible the widespread knowledge that patients with higher skin rash rate may have a better outcome could have contributed to this outcome. The 30 % rate of patients discontinued the treatment due to disease progression was surprisingly low given that the trial was implemented in countries where there is a high tendency to treat patients until disease progression. It will be important to review these data in more detail as well as all parameters concerning treatment disposition and exposure to fully understand trial results.
Putting the CALGB/SWOG results into context with other studies, there has been a major increase in the median OS from approximately 20 months in trials of chemotherapy without biological agents to the impressive results of the present study reaching the bar of 30 months of survival with both targeted agents. This increase may be explained by several factors including a slightly more favorable population, the academic collaborative group environment, the percentage of secondary liver resections, and the fact that a large proportion of patients in the study received post-progression treatment with chemotherapy and biologics. Some differences are observed regarding the treatment population when comparing the CALGB/SWOG and FIRE-3 studies (Table 1). Although highly comparable, it is possible that more patients in the CALGB/SWOG study had primary tumors in place, while the FIRE-3 study included a slightly older population and patients were treated with FOLFIRI only. In addition, more patients in the CALGB/SWOG study received second-line and later treatments than in the FIRE-3 trial (88 and 67 %, respectively). Finally, more mature data regarding relevant points of discussion such as ORR, DpR, and ETS are available for the FIRE-3 trial, but are awaited for CALGB/SWOG. The choice of an anti-EGFR combination in the first-line setting may thus be preferable when the therapeutic goal is tumor shrinkage in patients who could achieve a conversion to surgical resection or in cases of symptomatic disease.
After the initial studies showing the negative predictive value of the KRAS exon 2 codon 12 and 13 mutations, it has been demonstrated that other KRAS mutations in exons 3 and 4 and NRAS mutations also harbor predictive information (Table 2). By applying this critical molecular knowledge, we have been able to narrow the target population benefiting from EGFR monoclonal antibodies from the initial population by approximately 60 % with the exclusion of the KRAS exon 2 mutant population to around 45 % if we exclude all-RAS mutations. The all-RAS test is now mandatory in many countries, minimizing unnecessary exposure in patients whose tumors harbor any of the RAS mutations, which would dramatically lower chances of a successful outcome. Ultimately, this extended RAS analyses has unveiled the stronger real benefit in patients with all-RAS WT tumors when treated with EGFR inhibitors. The latest results presented of the CALGB/SWOG trial focused on the all-RAS testing suggest that benefit is greater in RAS WT patients using anti-EGFR therapies at least in terms of ORR. Hence, the extended RAS testing is the first step in selecting patients whose tumors may be dependent on EGFR signaling and must be performed up front to ensure they are offered optimal therapeutic options.
The results of the CALGB/SWOG study mark an important milestone in the therapeutic landscape of mCRC treatment. More mature efficacy data including DpR, ETS, and treatment disposition along with epidemiological and translational sub-studies will shed light on important questions that remain unanswered and will permit a better comparison between trials. The CALGB/SWOG study should be considered a reference study for the integration of different disciplines to allow recommendation to patients of the best treatment options. Several conceptual questions remain to be addressed with further preclinical and clinical evaluations, notably evaluating specific interactions of biological agents with chemotherapy, treatment sequence, as well as correlations with key clinical and molecular characteristics relating to primary tumor location and molecular subtypes.
Taken together, for the time being, the three studies do not allow a conclusion to be reached in support of selecting an optimal regimen sequence for the whole RAS WT population, although there is emerging data that treatment can be used on an individual basis. The treatment choice for each patient must consider efficacy, tolerability profile, cost, drug availability, and other important parameters for the specific aim of the treatment in each patient. Nonetheless, median survival of mCRC patients has reached a new benchmark of over 30 months, which has been the result of considerable efforts of years of research into a better understanding of tumor biology in order to find the most suitable approach for each individual patient.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance, •• Of major importance
Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, et al. Cancer treatment and survivorship statistics, 2012. CA: Cancer J Clin. 2012;62(4):220–41.
Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350(23):2335–42.
Saltz LB, Clarke S, Diaz-Rubio E, Scheithauer W, Figer A, Wong R, et al. Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol : Off J Am Soc Clin Oncol. 2008;26(12):2013–9.
Van Cutsem E, Kohne CH, Lang I, Folprecht G, Nowacki MP, Cascinu S, et al. Cetuximab plus irinotecan, fluorouracil, and leucovorin as first-line treatment for metastatic colorectal cancer: updated analysis of overall survival according to tumor KRAS and BRAF mutation status. J Clin Oncol : Off J Am Soc Clin Oncol. 2011;29(15):2011–9. The CRYSTAL trial granted the approval for prescribing FOLFIRI plus cetuximab in first metastatic chemotherapy line in RAS WT CRC.
Douillard JY, Oliner KS, Siena S, Tabernero J, Burkes R, Barugel M, et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med. 2013;369(11):1023–34. The PRIME study constructed the necessary evidence for using FOLFOX plus panitumumab in first metastatic line in RAS WT patient. This trail was the first in considering as a pre-specified end point the analysis according KRAS exon 2 status.
Douillard JY, Siena S, Cassidy J, Tabernero J, Burkes R, Barugel M, et al. Randomized, phase III trial of panitumumab with infusional fluorouracil, leucovorin, and oxaliplatin (FOLFOX4) versus FOLFOX4 alone as first-line treatment in patients with previously untreated metastatic colorectal cancer: the PRIME study. J Clin Oncol : Off J Am Soc Clin Oncol. 2010;28(31):4697–705.
Bennouna J, Sastre J, Arnold D, Osterlund P, Greil R, Van Cutsem E, et al. Continuation of bevacizumab after first progression in metastatic colorectal cancer (ML18147): a randomised phase 3 trial. Lancet Oncol. 2013;14(1):29–37.
Van Cutsem E, Peeters M, Siena S, Humblet Y, Hendlisz A, Neyns B, et al. Open-label phase III trial of panitumumab plus best supportive care compared with best supportive care alone in patients with chemotherapy-refractory metastatic colorectal cancer. J Clin Oncol : Off J Am Soc Clin Oncol. 2007;25(13):1658–64.
Amado RG, Wolf M, Peeters M, Van Cutsem E, Siena S, Freeman DJ, et al. Wild-type KRAS is required for panitumumab efficacy in patients with metastatic colorectal cancer. J Clin Oncol : Off J Am Soc Clin Oncol. 2008;26(10):1626–34.
Cunningham D, Humblet Y, Siena S, Khayat D, Bleiberg H, Santoro A, et al. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med. 2004;351(4):337–45.
Jonker DJ, O’Callaghan CJ, Karapetis CS, Zalcberg JR, Tu D, Au HJ, et al. Cetuximab for the treatment of colorectal cancer. N Engl J Med. 2007;357(20):2040–8.
Karapetis CS, Khambata-Ford S, Jonker DJ, O’Callaghan CJ, Tu D, Tebbutt NC, et al. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008;359(17):1757–65.
Sobrero AF, Maurel J, Fehrenbacher L, Scheithauer W, Abubakr YA, Lutz MP, et al. EPIC: phase III trial of cetuximab plus irinotecan after fluoropyrimidine and oxaliplatin failure in patients with metastatic colorectal cancer. J Clin Oncol : Off J Am Soc Clin Oncol. 2008;26(14):2311–9.
Peeters M, Price TJ, Cervantes A, Sobrero AF, Ducreux M, Hotko Y, et al. Randomized phase III study of panitumumab with fluorouracil, leucovorin, and irinotecan (FOLFIRI) compared with FOLFIRI alone as second-line treatment in patients with metastatic colorectal cancer. J Clin Oncol : Off J Am Soc Clin Oncol. 2010;28(31):4706–13.
Venook AND, Lenz HJ, et al. CALGB/SWOG 80405: phase III trial of irinotecan/5-FU/leucovorin (FOLFIRI) or oxaliplatin/5-FU/leucovorin (mFOLFOX6) with bevacizumab (BV) or cetuximab (CET) for patients (pts) with KRAS wild-type (wt) untreated metastatic adenocarcinoma of the colon or rectum (MCRC). J Clin Oncol. 2015;32:5s. 2014 (suppl; abstr LBA3).
Heinemann V, Stintzing S. FOLFIRI with cetuximab or bevacizumab: FIRE-3-authors’ reply. Lancet Oncol. 2014;15(13):e583–4.
Tang PA, Bentzen SM, Chen EX, Siu LL. Surrogate end points for median overall survival in metastatic colorectal cancer: literature-based analysis from 39 randomized controlled trials of first-line chemotherapy. J Clin Oncol : Off J Am Soc Clin Oncol. 2007;25(29):4562–8.
Buyse M, Burzykowski T, Carroll K, Michiels S, Sargent DJ, Miller LL, et al. Progression-free survival is a surrogate for survival in advanced colorectal cancer. J Clin Oncol : Off J Am Soc Clin Oncol. 2007;25(33):5218–24.
Shi Q, de Gramont A, Grothey A, Zalcberg J, Chibaudel B, Schmoll HJ, et al. Individual patient data analysis of progression-free survival versus overall survival as a first-line end point for metastatic colorectal cancer in modern randomized trials: findings from the analysis and research in cancers of the digestive system database. J Clin Oncol : Off J Am Soc Clin Oncol. 2015;33(1):22–8.
Venook AP, Tabernero J. Progression-free survival: helpful biomarker or clinically meaningless end point? J Clin Oncol : Off J Am Soc Clin Oncol. 2015;33(1):4–6.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Stintzing SMD, Fischer von Weikerstha L, et al. Independent radiological evaluation of objective response rate, early tumor shrinkage, and depth of response in FIRE-3 (AIO KRK-0306) in the final RAS evaluable population. Ann Oncol. 2014;2014:ii112–3. (suppl 2;abstr LBA O-0019). This is the FIRE-3 trial reference corresponding to the an oral presentation at the European Society of Medical Oncology congress on 2014.
Rivera FKM, Hecht R, et al. First-line treatment with modified FOLFOX6 (mFOLFOX6) + panitumumab (pmab) or bevacizumab (bev) in wild-type (WT) RAS metastatic colorectal carcinoma (mCRC): tumor response outcomes beyond RECIST. p. J Clin Oncol. 2015;33 suppl 3:abstr 660.
Hecht JR, Mitchell E, Chidiac T, Scroggin C, Hagenstad C, Spigel D, et al. A randomized phase IIIB trial of chemotherapy, bevacizumab, and panitumumab compared with chemotherapy and bevacizumab alone for metastatic colorectal cancer. J Clin Oncol : Off J Am Soc Clin Oncol. 2009;27(5):672–80.
Tol J, Koopman M, Cats A, Rodenburg CJ, Creemers GJ, Schrama JG, et al. Chemotherapy, bevacizumab, and cetuximab in metastatic colorectal cancer. N Engl J Med. 2009;360(6):563–72.
Venook AND, Lenz HJ, et al. CALGB/SWOG 80405: analysis of patients undergoing surgery as part of treatment strategy. Ann Oncol. 2014;25(5):1–41. This is the CALGB/SWOG 80405 trial reference corresponding to an oral presentation at the European Society of Medical Oncology congress on 2014.
Lenz HND, Innocenti F, et al. CALGB/SWOG 80405: phase III trial of irinotecan/5-FU/leucovorin (FOLFIRI) or oxaliplatin/5-FU/leucovorin (mFOLFOX6) with bevacizumab (BV) or cetuximab (CET) for patients (pts) with expanded RAS analyses untreated metastatic adenocarcinoma of the colon or rectum (mCRC). Ann Oncol. 2014;25(Supplement 5):v1–v41. This is the CALGB/SWOG 80405 trial reference corresponding to an oral presentation at the European Society of Medical Oncology congress on 2014.
Bokemeyer C, Bondarenko I, Makhson A, Hartmann JT, Aparicio J, de Braud F, et al. Fluorouracil, leucovorin, and oxaliplatin with and without cetuximab in the first-line treatment of metastatic colorectal cancer. J Clin Oncol : Off J Am Soc Clin Oncol. 2009;27(5):663–71.
Maughan TS, Adams RA, Smith CG, Meade AM, Seymour MT, Wilson RH, et al. Addition of cetuximab to oxaliplatin-based first-line combination chemotherapy for treatment of advanced colorectal cancer: results of the randomised phase 3 MRC COIN trial. Lancet. 2011;377(9783):2103–14.
Tveit KM, Guren T, Glimelius B, Pfeiffer P, Sorbye H, Pyrhonen S, et al. Phase III trial of cetuximab with continuous or intermittent fluorouracil, leucovorin, and oxaliplatin (Nordic FLOX) versus FLOX alone in first-line treatment of metastatic colorectal cancer: the NORDIC-VII study. J Clin Oncol : Off J Am Soc Clin Oncol. 2012;30(15):1755–62.
Primrose J, Falk S, Finch-Jones M, Valle J, O’Reilly D, Siriwardena A, et al. Systemic chemotherapy with or without cetuximab in patients with resectable colorectal liver metastasis: the New EPOC randomised controlled trial. Lancet Oncol. 2014;15(6):601–11.
Van Cutsem E, Kohne CH, Hitre E, Zaluski J, Chang Chien CR, Makhson A, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009;360(14):1408–17.
Compliance with Ethics Guidelines
Conflict of Interest
Elena Elez, Guillem Argilés, and Josep Tabernero declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Lower Gastrointestinal Cancers
Rights and permissions
About this article
Cite this article
Elez, E., Argilés, G. & Tabernero, J. First-Line Treatment of Metastatic Colorectal Cancer: Interpreting FIRE-3, PEAK, and CALGB/SWOG 80405. Curr. Treat. Options in Oncol. 16, 52 (2015). https://doi.org/10.1007/s11864-015-0369-x
Published:
DOI: https://doi.org/10.1007/s11864-015-0369-x