Opinion statement
Over the recent years, there has been an increasing recognition that triple-negative breast cancer constitutes a separate, albeit heterogeneous, entity arising from distinct oncogenic pathways. Despite its aggressive clinical behavior, triple-negative disease responds favorably to cytotoxic chemotherapy resulting in high response rates. Nonetheless, the relapse rates are high and, in the absence of targeted therapies to significantly alter its natural history, the prognosis can be poor. Most of the trials conducted in the past that led to the formulation of the current guidelines have indiscriminately lumped triple-negative disease with receptor-positive subtypes. Therefore, there are relatively scant data regarding how standard approaches specifically apply for triple-negative disease. By virtue of its chemosensitive nature and high probability of achieving a complete pathologic response, neoadjuvant chemotherapy in early-stage/operable and locally-advanced/inoperable triple-negative disease is highly recommended. The indications for adjuvant chemotherapy are the same as in receptor-positive tumors, although endocrine therapies or agents targeting Her2 signaling have no established role in triple-negative disease. The optimal chemotherapy is not entirely clear; however, by virtue of their efficacy in breast cancer in general, anthracycline-containing regimens are the most widely used. The incorporation of taxanes in the regimen is supported by retrospective analyses. There is scant evidence to recommend any particular agent in the metastatic setting, although the combination of ixabepilone with capecitabine was shown to be active specifically in triple-negative disease. Given the uncertainty in the optimal management of triple-negative disease, the shortcomings of contemporary regimens, and the strong rationale of novel therapies, participation in clinical trials should be strongly considered at any stage of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer constitutes the most common malignancy in women in developed countries. In 2010, in the United States, an estimated 208,000 women were diagnosed with breast cancer with an estimated 40,000 deaths attributed to the disease [1]. Gene expression analysis of primary breast tumors has led to the recognition of five distinct subtypes: the estrogen receptor (ER) positive luminal A and B, the human epidermal growth factor receptor 2 (HER2)-overexpressing/enriched, the normal breast tissue-like, and the basal-like subtype [2–4]. Recently, another subtype has been described, “claudin-low”, which appears to be enriched for stem cell markers [5].
Triple-negative breast cancer is characterized by the lack of expression of ER, progesterone receptor (PR), and HER2. It represents approximately 12–17% of all breast cancers [6] and encompasses a heterogeneous group of tumors including, but not limited to, those classified as basal-like. It expresses cytokeratins 5/6/17 and has upregulation of epidermal growth factor receptor (EGFR). As ER, PR, and HER2 represent known targets in breast cancer therapeutics, patients with triple-negative disease do not derive any benefit from endocrine therapies or agents targeting HER2 signaling, a fact that may in part account for the unfavorable clinical outcomes in this subgroup of patients. However, over the recent years, there has been a considerable effort to elucidate the molecular underpinnings of triple-negative disease, identify new treatment targets, and refine the therapeutic approaches.
Definitions
The identification of a triple-negative phenotype has important clinical implications. In an attempt to overcome the variability in reporting and interpretation of the receptor status of a tumor, the American Society of Clinical Oncology jointly with the College of American Pathologists have proposed guidelines for testing and interpretation [7, 8]. In triple-negative disease, less than 1% of tumor cells stain positive for ER and PR by immunohistochemistry [7]. These cells also stain ≤2+ on immunohistochemistry for HER2 or carry fewer than 6 HER2 gene copies per nucleus or have a fluorescence in situ hybridization ratio of less than 2.2 (HER2 signals to chromosome 17 signals) [8]. We recommend abiding by the ASCO/CAP recommendations as even low levels of receptor expression are associated with clinical benefit from targeted therapies.
Basal-like breast cancer is a classification based on gene expression profile and not on immunohistochemistry. Triple-negative and basal-like breast cancer are not synonymous despite the significant overlap. Under the immunohistochemical definition of “triple-negative disease” other intrinsic subtypes, such as Her2-enriched, may be represented as well [9].
Epidemiology
Premenopausal and African-American women seem to be disproportionately afflicted by the disease [10] which is clinically associated with an unfavorable prognosis [10, 11]. Nonetheless, the disease-related mortality seems to be higher among white premenopausal and particularly postmenopausal women compared with their African-American counterparts [12].
Deleterious BRCA1 mutations are associated with an exceptionally high risk for developing triple-negative/basal-like breast cancer [4, 13, 14]. Single-nucleotide polymorphisms specific for triple-negative disease have been identified in a locus on 19p13 and their association with triple-negative disease was shown to be particularly strong in the context of germline BRCA1 mutations [15•].
Pathologic and molecular characteristics
Pathologically, triple-negative tumors are usually high-grade invasive ductal carcinomas of no special type with high mitotic indices [16]. Pushing borders, central necrotic areas, lymphocytic infiltration, medullary and metaplastic differentiation constitute other histologic hallmarks of triple-negative disease.
At the molecular level, gene-expression studies have unveiled the significant heterogeneity within the triple-negative disease. This was illustrated in a recent analysis that identified six distinct subtypes within triple-negative disease with unique gene-expression patterns and distinct “driver” signaling pathways [17••]. On cell line models, these subtypes showed differential sensitivities to cisplatin, bicalutamide (an androgen receptor antagonist used in prostate cancer), and PI3K/mTOR inhibition [17••].
Clinical characteristics
Triple-negative tumors are usually larger at diagnosis and more likely to be detected on physical examination [18] compared with the other subtypes. Basal-like breast cancers also constitute the majority of cancers detected in the interval between screening mammograms [19]. Although studies have shown that basal-like breast cancer tends to be node-negative at presentation [20], its risk for nodal and regional recurrence is high and appears to be similar to the other subtypes [21].
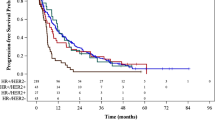
Another distinctive feature of triple-negative disease is its metastatic pattern in terms of location and time. Compared with the other subtypes, basal-like breast cancer has a high risk of visceral and central nervous involvement; skeleton is frequently spared [22]. The risk for distant recurrence was shown to peak at approximately 2 to 3 years after diagnosis and to remain high for the first 5 years, whereas the risk among patients with other subtypes remains constant throughout the years of follow-up [18]. Upon metastatic recurrence, the median survival in triple-negative disease is significantly shorter compared with the other subtypes [23].
Treatment
-
In deciding the optimal approach to treat triple-negative disease, the general principles of breast cancer therapeutics still apply. Distinct differences, however, when compared to the management of other subtypes, are the absence of response to endocrine therapies and HER2 targeted agents, and the high chemosensitivity especially in the neoadjuvant setting. Despite the high response rates, the risk of relapse in triple-negative disease remains high, especially if residual tumor is present resulting in inferior clinical outcomes (hence the term “triple-negative paradox”) [24].
-
The clinical trials conducted over the years that led to the formulation of the current guidelines have indiscriminately lumped triple-negative disease with receptor-positive subtypes. Therefore, there are relatively scant data regarding how standard approaches specifically apply for triple-negative disease. Given the uncertainty in the optimal management of triple-negative disease, the shortcomings of contemporary regimens, and the strong rationale of novel therapies, participation in clinical trials should be highly preferred at any stage of the disease.
Surgery
Surgery for local disease
-
Surgery represents the optimal modality for local control of triple-negative disease. Large randomized trials have demonstrated the equivalent outcomes between mastectomy and breast conserving surgery followed by moderate-dose radiation therapy in early breast cancer [25]. [Class I] Triple-negative disease is usually unifocal with smooth radiographic margins, and, hence, a good candidate for breast conserving surgery with negative resection margins.
-
Although not uniformly shown in studies, triple-negative disease and basal-like breast cancer in particular, have been associated with high rates of locoregional recurrence [21]. However, locoregional relapse-free survival rates among women who underwent mastectomy and those who underwent breast-conserving surgery were overlapping [21], advocating in favor of less invasive interventions in early breast cancer. [Class III]
-
Positive or indeterminate resection margins should prompt reexcision, as these patients have a high risk of local recurrence even with adjuvant radiation therapy. The importance of achieving negative margins in triple-negative disease is underscored by the high frequency of residual tumors identified in the reexcision specimens [26], which in the context of neoadjuvant chemotherapy, may represent chemoresistant disease responsible for early relapse. [Class I]
-
There is no consensus definition for “close margins”; however, in most studies the latter was defined as ≤2 mm. Although the clinical implications of lumpectomy in close margins are not clear-cut, we recommend reexcision following the same rationale as in excisions performed in positive margins. If reexcision in negative margins cannot be performed, radiation boost of 16 Gray to the primary tumor bed, in addition to the usual postoperative radiation treatment, should be considered [27]. [Class II]
Surgery for metastatic disease
-
Surgery in the metastatic setting is recommended for palliation of symptoms or impending complications. In view of the aggressive nature of triple-negative disease, surgery can be undertaken only if complete resection of the tumor is anticipated. Otherwise, radiation therapy constitutes a reasonable alternative. Also, as the patient will not be eligible for chemotherapy in the perioperative period, other sites of disease should not pose a threat for growth.
-
Although there is evidence to recommend excision of the primary tumor in the metastatic setting [28], this evidence comes from retrospective studies and this recommendation should be applied with caution in triple-negative disease. [Class IV] A protocol of the Translational Breast Cancer Research Consortium (TBCRC) is exploring prospectively the role of mastectomy in the metastatic setting.
Pharmacologic treatments
Neoadjuvant chemotherapy
-
The primary rationale of neoadjuvant chemotherapy is to downstage inoperable, locally advanced tumors so as to facilitate locoregional control by means of surgery and/or radiation therapy. In this setting, a significant benefit in progression-free and overall survival has been shown among patients who achieve a pathologic complete response (pCR) [29]. [Class I] In operable, early stage breast cancer, neoadjuvant chemotherapy has resulted in a higher rate of successful breast-conserving surgeries among women who would otherwise require mastectomy; no benefit in overall survival, disease progression, and distant disease recurrence was seen in the clinical trials comparing identical regimens in the adjuvant versus neoadjuvant setting [30]. [Class I]
-
Triple-negative disease constitutes a particularly chemosensitive entity, especially in the neoadjuvant setting. This has been illustrated in 2 studies conducted on prospectively collected clinical databases where patients with triple-negative disease achieved significantly higher response rates compared with their counterparts with other subtypes [23, 24]. These high response rates, however, did not translate into better clinical outcomes, primarily due to the high recurrence rates among patients with residual disease [23, 24]. The importance of achieving pCR in triple-negative disease with neoadjuvant chemotherapy was underscored by the significantly better outcomes among patients who achieved pCR; their prognosis was similar to that of patients with other subtypes who achieved pCR. [23] Improving the pCR rates in triple-negative disease appears to be an important stepping stone in improving the overall clinical outcomes. The TBCRC012 study is addressing if exercise, diet, metronomic chemotherapy and bevacizumab can improve the prognosis of patients with less than a pCR in the neoadjuvant setting [31].
-
Support regarding the importance of achieving pCR is also provided by insightful research that showed the selective survival of resistant clones after the administration of chemotherapy [32, 33•]. Overcoming the intrinsic resistance of these cells by identifying the most relevant therapeutic targets is anticipated to bend the high recurrence rate in triple-negative disease.
-
Anthracycline- and taxane-based regimens have been extensively evaluated in clinical trials and constitute the most widely used regimens in the neoadjuvant setting. Multiple trials have shown the improvement in the response rate conferred by adding a taxane concurrently or sequentially to an anthracycline-based regimen, although the benefit in overall survival has been less clear. [Class I] In the largest trial of neoadjuvant chemotherapy in breast cancer conducted by the National Surgical Adjuvant Breast and Bowel Project, the sequential addition of docetaxel improved the overall response rate and, most importantly, the pCR rate over adriamycin and cyclophosphamide alone [34]. Although no differences in disease-free and overall survival were seen, the clinical outcomes among patients who achieved a pCR were significantly superior [34].
-
Dose-dense chemotherapy constitutes an appealing option and has been made possible with the concurrent administration of hematopoietic growth factors. Its clinical benefit was clearly shown in the adjuvant setting [35]. Although many neoadjuvant trials have included a dose-dense arm, differences in the regimens between arms besides intervals of administration, preclude clear conclusions. In fact, in a clinical trial that compared identical regimens administered in a standard versus dose-dense fashion, no differences in the response rates and clinical outcomes were seen [36]. Nonetheless, dose-dense chemotherapy remains a promising option as illustrated by the higher (but not statistically significant) pCR rates in triple-negative disease in a recent neoadjuvant trial comparing similar regimens [37•]. [Class II]
-
Clinical trials have shown that changing regimen in the neoadjuvant setting based on response did not confer any benefit [38]; however, it is unclear whether this applies to triple-negative disease as these trials did not discriminate for receptor status. In the absence of clinical response, we recommend transition to locoregional treatments and systemic therapies under clinical trials.
-
The optimal length of neoadjuvant chemotherapy has not been clearly established. Although prolonging neoadjuvant chemotherapy from 3 to 6 cycles improved significantly the pCR rate [39], no further improvement was seen by prolonging chemotherapy to 8 cycles [40]. In a pooled analysis of neoadjuvant trials, adding more cycles of chemotherapy did not confer a clear benefit in triple- negative disease [41]. In the same analysis, higher response rates in triple-negative disease were associated with higher cumulative doses of anthracyclines and taxanes and the administration of capecitabine [41]. Most experts would recommend, in the absence of progressive disease, the administration of four to six cycles of neoadjuvant chemotherapy. [Class II]
-
By virtue of its high chemosensitivity, and consequently the high probability of achieving favorable long-term outcomes, we recommend neoadjuvant chemotherapy in early-stage/operable and locally-advanced/inoperable triple-negative disease. An anthracycline-containing regimen should generally be preferred as there is scant data with nonanthracycline-containing regimens. Taxanes improve significantly the response rate and therefore should be incorporated in the regimen. It is unclear whether a dose-dense schedule is superior to a conventional one.
Adjuvant chemotherapy
-
The principal rationale of adjuvant chemotherapy is the elimination of clinically inapparent micrometastases that are thought to give rise to recurrent disease after locoregional treatment. Multiple trials have demonstrated the benefit of adjuvant chemotherapy in recurrence rate and disease-specific mortality [42] but most of them did not prospectively stratify for receptor status. Nonetheless, retrospective analyses of those studies have shown that patients with receptor-negative disease have derived the most benefit from adjuvant chemotherapy [43, 44]. [Class III]
-
Overall, the regimens and the indications for adjuvant cytotoxic chemotherapy in triple-negative disease are the same as in receptor-positive tumors with poor prognostic features. Although tumors >1 cm and/or metastatic to the lymph nodes require adjuvant chemotherapy, the recommendations for smaller tumors with or without micrometastases to the lymph nodes are unclear. In a retrospective analysis of 965 patients with T1a/bN0M0 tumors who did not receive cytotoxic chemotherapy, the 5-year survival and recurrence rates in triple-negative disease were statistically worse compared to hormone-receptor positive disease [45]. Another retrospective study that included T1c tumors, showed a higher recurrence rate and an inferior disease-free survival among patients with T1N0 triple-negative disease compared to hormone-receptor positive counterparts, even with adjuvant chemotherapy [46]. As the benefit of adjuvant chemotherapy in this subgroup is unclear, we recommend an individualized approach weighing the potential benefit against the anticipated toxicities [47]. [Class III]
-
Numerous regimens have been investigated in phase III clinical trials and can be considered in the adjuvant setting. Anthracycline- containing regimens were shown to achieve better reductions in the recurrence rates compared to cyclophosphamide plus methotrexate plus 5-fluorouracil although the benefit in the mortality was marginal [48]. Moreover, it has been suggested that the superiority of anthracycline-containing regimens may be limited to Her2-positive disease [49] rendering their use in other subtypes, including triple-negative disease, controversial. The benefit of incorporating a taxane to the regimen specifically in triple-negative disease was shown in retrospective analyses of adjuvant trials with docetaxel, paclitaxel, and weekly paclitaxel, respectively [50–52]. As the superiority of anthracycline- and taxane-based regimens in triple-negative disease [53] has been challenged, participation in clinical trials is highly recommended to identify the optimal regimens. [Class III]
-
The benefit of incorporating capecitabine in an anthracycline-taxane containing regimen in triple-negative disease was shown in an exploratory subgroup analysis of a prospective clinical trial [54]. The incorporation of capecitabine resulted in a significant improvement in relapse-free and overall survival after 5 years [54]. [Class III]
-
The clinical benefit of dose-dense chemotherapy in the adjuvant setting was shown in a prospective clinical trial that compared identical chemotherapies administered in a conventional versus dose-dense schedule [35]. The preference for a dose-dense schedule in triple-negative disease is supported by a retrospective analysis where, compared to other subtypes, triple-negative disease was shown to derive the most benefit from a dose-dense regimen [55]. [Class II]
-
In the absence of adjuvant trials specifically for triple-negative disease, we recommend participation in clinical trials for eligible patients. If none available or the patient declines participation, an anthracycline-taxane containing regimen, preferably administered in a dose-dense schedule should be considered. We also favor weekly paclitaxel given the benefit in disease-free and overall survival with the weekly regimen [52, 56]. Extension of chemotherapy beyond 6 months has been associated with a nonsignificant benefit in recurrence rate without reflection on overall survival, and, therefore is not recommended [48].
Chemotherapy in metastatic disease
-
In the metastatic setting, chemotherapy constitutes the primary therapeutic modality. As its principal goals are palliation of symptoms and prolongation of life, efficacy and toxicity should be equally considered. Selection of the optimal regimen should be individualized considering performance status, prior treatments, extent of disease, presence of disease-related symptoms, toxicity profile, and goals of care.
-
Although combination chemotherapy has shown superior response rates and progression-free intervals compared to single-agent regimens, the benefit in overall survival has been modest [57] and inconsistent [58]. [Class II] As combination chemotherapy comes with the cost of significant toxicities, it is generally reserved for cases where rapid control of the disease is required. Otherwise, sequential single-agent regimens are preferred.
-
There is scant evidence to recommend any particular regimen in triple-negative disease. The use of anthracyclines and taxanes is generally limited by prior exposure to these agents. Ixabepilone plus capecitabine represents one of the few combinations shown to be active specifically in triple-negative disease with an improvement of progression-free and overall survival compared to capecitabine alone [59]. [Class III]
Emerging therapies
Multiple pathways amenable to therapeutic targeting (Fig. 1) have been shown to be operational in triple-negative disease providing a strong rationale for investigational therapies and supporting the preference for participation in clinical trials.
Illustration of selected pathways found to be operational in triple-negative disease. a. As BRCA-deficient tumor cells cannot repair double-strand DNA breaks by homologous recombination, they rely heavily on PARP to maintain the integrity of DNA by engaging the mechanism of base-excision repair. In the setting of PARP inhibition, an overwhelming accumulation of double-strand breaks during replication occurs selectively in BRCA-deficient tumor cells, leading to death, whereas normal tissues are spared. In sporadic triple-negative tumors, BRCA1 may be epigenetically silenced, or downregulated by means of microRNA-182 overexpression. Abbreviations: BRCA, breast cancer 1 early onset; PARP, PolyADP-ribose Polymerase. b. Under normal conditions, p53 binds with mdm2 and is shuttled out of the nucleus where is undergoes degradation by ubiquitination. In response to stimuli such as DNA damage, p53 and mdm2 are phosphorylated by the ATM and ATR serine/threonine kinases, and the immediate downstream checkpoint kinases, CHK1 and CHK2. As a result, p53 dissociates from mdm2, forms tetramers, and leads to upregulation of genes involved in cell cycle arrest and apoptosis. p53 is also activated by oncogenes such as Myc, which promote aberrant G1/S transition. Under these conditions, p14ARF is upregulated, binds to mdm2, and rescues p53 from degradation. p53 is mutated in 44% of triple-negative breast cancers [14] leading to aberrant cell cycle progression. Tumors with mutated p53 may be amenable to a “synthetic lethality” approach, as different molecular pathways may be operational in cells with mutated p53 compared to normal tissues. Abbreviations: ATM, ataxia-telangiectasia mutated; ATR, ataxia telangiectasia and Rad3 related; CHK1, checkpoint 1; CHK2, checkpoint 2; mdm2, murine double minute 2; P, phosphoryl group; p14ARF, p14 alternate open reading frame; U, ubiquitine. c. Receptor tyrosine kinases and downstream signaling pathways in triple-negative disease. Receptor tyrosine kinases such as EGFR, ckit, Insulin-like Growth Factor 1 Receptor (IGF1R), and Fibroblast Growth Factor Receptor 2 (FGFR2) activate downstream signaling pathways by phosphorylation of specific tyrosine residues in their intracellular domains. One pathway involves the protooncogene RAS which is activated by the Grb2/mSOS guanine nucleotide exchange factor as it cycles between the inactive GDP- and active GTP-bound state. RAS-GTP recruits and activates RAF leading to subsequent activation of MEK and ERK. Another pathway involves the kinase PI3K which phosphorylates the membrane lipid PIP2 to PIP3. PIP3 in turn acts as a docking site for serine/threonine kinases PDK1 and AKT1 which have numerous downstream cellular targets, including mTOR. The end effect of the activation of these pathways is upregulation of protein synthesis and upregulation of genes involved in cell survival, growth, and proliferation. A small subgroup of triple-negative breast tumors have a Her2-enriched molecular signature. Abbreviations: AKT1, protein kinase B; ckit, stem cell factor receptor; EGFR, epidermal growth factor receptor; ERK, mitogen-activated protein kinase 1; GDP/GTP, guanosine diphosphate/ triphosphate; GRB2, growth factor receptor-bound protein 2; Her2/neu, epidermal growth factor receptor 2; MEK, mitogen-activated protein kinase kinase 1; mTOR, mammalian target of rapamycin; mSOS, son of sevenless homolog 1; P, phosphoryl group; p85 and p110, p85 [regulatory] and p110[catalytic] subunits of the PI3K, respectively; PDK1, 3- phosphoinositide-dependent protein kinase 1; PI3K, phosphatidyl inositol-3 kinase; PIP2, phosphatidyl inositol 4, 5 diphosphate; PIP3, phosphatidyl inositol 3,4,5 triphosphate; PTEN, phosphatase and tensin homolog ; RAF, Raf-1 serine/threonine kinase ; RAS, rat sarcoma viral oncogene homolog. d. The Wnt/β-Catenin pathway. In the absence of Wnt, cytoplasmic β-catenin forms a complex with Axin, adenomatous polyposis coli gene product (APC), casein kinase 1 (CK1), and glycogen synthase kinase 3 beta (GSK3β). In this complex, β-catenin undergoes phosphorylation followed by proteasomal degradation. The Wnt-ligand is a secreted glycolipoprotein that binds to Frizzled receptor and LRP leading to the recruitment of Dishevelled to the Frizzled receptor. Disheveled in turn, recruits axin and GSK3β away from the β-catenin degradation complex, thereby leading to the stabilization of β-catenin. β-catenin translocates to the nucleus and associates with LEF/ TCF DNA-binding factors where it acts as an activator of transcription. GSK3β phosphorylates critical sites on LRP which serve as docking sites for axin allowing for the stabilization of β-catenin. Abbreviations: Dvl, Dishevelled; GSK3β, glycogen synthase kinase 3 beta; LRP, low-density lipoprotein receptor related protein; MMP7, matrix metallopeptidase 7; PPAR-δ, peroxisome proliferator-activated receptor delta; TCF/LEF, T cell factor/lymphoid enhancer factor; Wnt, Wnt ligand. e. The hedgehog signaling pathway may be operational in cancer stem cells. In normal cells, the PTCH1 receptor binds to the SMO receptor, blocking hedgehog signaling. In the absence of ligand, the GLI family zinc finger transcription factors GLI2 and GLI3, are bound by the SUFU and undergo proteasomal cleavage into the repressor forms, GLI2R and GLI3R. In cancer cells, the binding of hedgehog ligands, such as SHH, to PTCH1 releases SMO, whereby GLI2 and GLI3 evade proteasomal degradation, translocate to the nucleus and act as activating transcription factors (GLI2A and GLI3A) for genes such as BCL2 and Cyclin D1. (Abbreviations: GLI1/2, glioma-associated oncogene homolog 1 and 2; PTCH1, patched; SHH, Sonic hedgehog homolog; SMO, smoothened; SUFU, suppressor of fused). f. The Death Receptor 5 is the target of the agonistic monoclonal antibody, tigatuzumab. An antiapoptotic protein complex consisting of GSK3, DDX3, and cIAP-1 is associated with death receptors. Normal cells overcome the antiapoptotic complex upon stimulation of the death receptors by causing GSK3 inactivation and cleavage of DDX3 and cIAP-1. The antiapoptotic complex, however, remains functional in cancer cells rendering them resistant to death receptor stimulation. Triple-negative breast cancer cell lines were shown to contain low levels of DR5-associated DDX3 and cIAP-1 rendering them susceptible to DR5-mediated cytotoxicity. (Abbreviations: cIAP-1, cellular inhibitor of apoptosis protein-1; DDX3, DEAD {Asp-Glu-Ala-Asp} box polypeptide 3; DR5, TNT-related apoptosis-inducing ligand receptor-2; GSK3; glycogen synthase kinase-3; TRAIL, TNF-related apoptosis-inducing ligand).
Platinum agents
-
There has been a renewed interest in platinum compounds, partly because of improvements in the management of their toxicities as well as preclinical evidence of increased sensitivity to cisplatin of BRCA1-deficient cell lines [60].
-
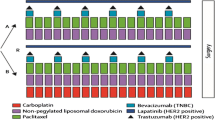
In early-phase clinical trials, platinum compounds have shown variable activity depending on the setting, population, and use in combination or alone (Table 1). The results of two trials are anticipated to clarify the role of the platinum compounds in triple- negative disease: a randomized phase II trial investigating the benefit of incorporating carboplatin and/or bevacizumab in the neoadjuvant setting (Cancer and Leukemia Group B 40603) [61] and a randomized trial comparing the efficacy of cisplatin or carboplatin in the metastatic setting (TBCRC009) [62].
Table 1 Selected clinical studies in triple-negative disease with novel regimens
Antiangiogenic agents
-
Preclinical data has shown significantly higher intra-tumoral vascular endothelial growth factor (VEGF) levels in triple-negative [63] and basal-like breast cancers [64] compared to other subgroups rendering VEGF signaling a rational therapeutic target in triple-negative disease [63].
-
Despite the significant improvements in the response rate and progression-free survival with bevacizumab, no significant improvements in overall survival were achieved [65, 66, 67•]. A recent combined analysis of three major randomized trials with bevacizumab showed a significant increase in progression-free survival in patients with triple-negative disease receiving anti-angiogenic therapy but no improvement in overall survival [68]. Thus, the clinical utility of bevacizumab remains undefined.
-
Tyrosine kinase inhibitors targeting angiogenesis have also been clinically investigated. One such inhibitor, sunitinib, has been evaluated alone or in combination with chemotherapy but the results have been disappointing [69–71]. Subset analyses of patients with triple-negative disease in these studies suggested a benefit and led to trials of sunitinib in combination with chemotherapy in the neoadjuvant setting [72].
PolyADP-ribose Polymerase (PARP) inhibitors
-
As BRCA-deficient tumor cells cannot repair double-strand DNA breaks by homologous recombination, they rely heavily on PARP to maintain the integrity of DNA by engaging the mechanism of base-excision repair [73]. In the setting of PARP inhibition, an overwhelming accumulation of double-strand breaks during replication occurs selectively in BRCA-deficient tumor cells, leading to death, whereas normal tissues are spared [73]. This concept of synthetic lethality has borne out nicely in early-phase clinical trials (Table 1, Fig. 1a) especially among patients with germline BRCA mutations.
-
Based on the observation that sporadic triple-negative tumors have impaired DNA repair capabilities similar to BRCA1-deficient tumors, O’Shaughnessy et al. have conducted clinical trials evaluating whether the addition of the PARP inhibitor iniparib, to DNA- damaging chemotherapy could improve outcomes in triple- negative disease. Although the randomized phase II study showed that iniparib added to carboplatin and gemcitabine conferred a significant benefit in response rate, progression-free and overall survival [74], preliminary negative results from the phase III confirmatory trial [75] imply that the benefit may not be uniform in sporadic triple-negative disease.
-
Other PARP inhibitors such as veliparib [76] and PF-01367338 [77] are currently evaluated in clinical trials with patients with BRCA-mutated or sporadic triple-negative breast cancer. Results of these trials will further clarify the role of PARP inhibition in triple-negative disease.
Targeting the epidermal growth factor receptor
-
Preclinical studies have shown that basal-like breast cancer depends on the EGFR pathway for proliferation, rendering EGFR a rational target (Fig. 1c) [78, 79]. Two classes of agents target EGFR signaling: monoclonal antibodies, such as cetuximab and panitumumab; and small molecule tyrosine kinase inhibitors, such as gefitinib and erlotinib.
-
Carey et al. conducted a clinical trial of cetuximab with or without carboplatin in patients with metastatic triple-negative disease (TBCRC001) [80]. Patients who received cetuximab alone had a clinical benefit ratio of 10%. Although this ratio was raised to 31% when cetuximab was combined with carboplatin, the progression-free survival was only 2 months in both arms [80].
-
Clinical trials with gefitinib and erlotinib alone or in combination with chemotherapy have been conducted in breast cancer but the results were not encouraging [81–83].
Targeting Death-Receptor 5 (DR5)
-
Targeting death receptors on cancer cells with agonistic monoclonal antibodies (Fig. 1f) may represent a new generation of targeted therapy as these antibodies can directly induce apoptosis of malignant cells [84]. Monoclonal antibodies may be superior to the natural ligand (tumor necrosis factor-related apoptosis inducing ligand; TRAIL) as TRAIL targets multiple receptors including functional and decoy receptors as well as has a shorter plasma half-life affecting dose and schedule parameters. Daiichi Sankyo has developed an agonistic humanized monoclonal antibody (Tigatuzumab) specific for the human DR5 receptor. Unlike cell lines of other subtypes, basal-like breast cancer cell lines were sensitive to agonistic DR5 targeting and, when the anti-DR5 antibody was combined with chemotherapy, an additive or synergistic effect was seen. The in vivo efficacy of the anti-DR5 antibody plus Abraxane (or doxorubicin) exceeded the efficacy of either agent alone [85, 86]. A protocol involving treatment with Abraxane ± Tigatuzumab will be activated in 2011 (TBCRC019).
Several other potential therapeutic targets have been identified and are currently clinically investigated. Given the strong rationale and promising activity of new agents in triple-negative disease, participation in clinical trials is strongly encouraged at any stage of the disease. Studies have indicated that in order to optimize the benefit from novel agents, a refined patient selection based on genomic profiling of the tumor may be necessary, as different ”driver” pathways may be activated among the triple-negative subsets [17••].
Abbreviations
- ASCO:
-
American Society of Clinical Oncology
- BRCA1 :
-
Breast cancer 1 early onset
- BRCA2 :
-
Breast cancer 2 early onset
- CAP:
-
College of American Pathologists
- DNA:
-
Deoxyribonucleic acid
- EGFR:
-
Epidermal growth factor receptor
- ER:
-
Estrogen receptor
- Her2 (ERBB2):
-
Epidermal growth factor receptor 2
- mTOR:
-
Mammalian target of rapamycin
- PARP:
-
Poly (Adenosine Diphosphate–Ribose) Polymerase
- pCR:
-
Pathologic complete response
- PI3K:
-
Phosphatidylinositol 3-kinase
- PR:
-
Progesterone receptor
- RNA:
-
Ribonucleic acid
- TBCRC:
-
Translational Breast Cancer Research Consortium
- TRAIL:
-
Tumor necrosis factor-related apoptosis inducing ligand
- VEGF:
-
Vascular endothelial growth factor
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA: a cancer journal for clinicians. 2010;60(5):277–300.
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, et al. Molecular portraits of human breast tumours. Nature. 2000;406(6797):747–52.
Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(19):10869–74.
Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(14):8418–23.
Hennessy BT, Gonzalez-Angulo AM, Stemke-Hale K, Gilcrease MZ, Krishnamurthy S, et al. Characterization of a naturally occurring breast cancer subset enriched in epithelial-to-mesenchymal transition and stem cell characteristics. Cancer Research. 2009;69(10):4116–24.
Foulkes WD, Smith IE, Reis-Filho JS. Triple-negative breast cancer. The New England Journal of Medicine. 2010;363(20):1938–48.
Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, et al. American Society of Clinical Oncology/College Of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol. 2010;28(16):2784–95.
Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25(1):118–45.
Perou CM. Molecular stratification of triple-negative breast cancers. Oncologist. 2010;15 Suppl 5:39–48.
Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V. Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer Registry. Cancer. 2007;109(9):1721–8.
Morris GJ, Naidu S, Topham AK, Guiles F, Xu Y, et al. Differences in breast carcinoma characteristics in newly diagnosed African-American and Caucasian patients: a single-institution compilation compared with the National Cancer Institute's Surveillance, Epidemiology, and End Results database. Cancer. 2007;110(4):876–84.
O'Brien KM, Cole SR, Tse CK, Perou CM, Carey LA, et al. Intrinsic breast tumor subtypes, race, and long-term survival in the Carolina Breast Cancer Study. Clin Cancer Res. 2010;16(24):6100–10.
Ford D, Easton DF, Bishop DT, Narod SA, Goldgar DE. Risks of cancer in BRCA1-mutation carriers. Breast Cancer Linkage Consortium. Lancet. 1994;343(8899):692–5.
Schneider BP, Winer EP, Foulkes WD, Garber J, Perou CM, et al. Triple-negative breast cancer: risk factors to potential targets. Clin Cancer Res. 2008;14(24):8010–8.
Antoniou AC, Wang X, Fredericksen ZS, McGuffog L, Tarrell R, et al. A locus on 19p13 modifies risk of breast cancer in BRCA1 mutation carriers and is associated with hormone receptor-negative breast cancer in the general population. Nat Genet. 2010;42(10):885–92.
Badve S, Dabbs DJ, Schnitt SJ, Baehner FL, Decker T, et al. Basal-like and triple-negative breast cancers: a critical review with an emphasis on the implications for pathologists and oncologists. Mod Pathol. 2011;24(2):157–67.
Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, et al. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. Journal Clinical Investigation. 2011;121(7):2750–67. This genome profiling study sheds light onto the molecular heterogeneity of triple-negative disease. Cell lines representative of the triple-negative subtypes were shown to be differentially susceptible to platinum compounds, tyrosine kinase inhibitors, and androgen receptor antagonists. This study may explain the discrepant results seen in early-phase clinical trials with novel agents in triple-negative disease.
Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007;13(15 Pt 1):4429–34.
Collett K, Stefansson IM, Eide J, Braaten A, Wang H, et al. A basal epithelial phenotype is more frequent in interval breast cancers compared with screen detected tumors. Cancer Epidemiol Biomarkers Prev. 2005;14(5):1108–12.
Crabb SJ, Cheang MC, Leung S, Immonen T, Nielsen TO, et al. Basal breast cancer molecular subtype predicts for lower incidence of axillary lymph node metastases in primary breast cancer. Clinical Breast Cancer. 2008;8(3):249–56.
Voduc KD, Cheang MC, Tyldesley S, Gelmon K, Nielsen TO, et al. Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol. 2010;28(10):1684–91.
Kennecke H, Yerushalmi R, Woods R, Cheang MC, Voduc D, et al. Metastatic behavior of breast cancer subtypes. J Clin Oncol. 2010;28(20):3271–7.
Liedtke C, Mazouni C, Hess KR, Andre F, Tordai A, et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008;26(8):1275–81.
Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, et al. The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res. 2007;13(8):2329–34.
Early Breast Cancer Trialists' Collaborative Group. Effects of radiotherapy and surgery in early breast cancer. An overview of the randomized trials. New England Journal Medicine. 1995;333(22):1444–55.
Gwin JL, Eisenberg BL, Hoffman JP, Ottery FD, Boraas M, et al. Incidence of gross and microscopic carcinoma in specimens from patients with breast cancer after re-excision lumpectomy. Ann Surg. 1993;218(6):729–34.
Jones HA, Antonini N, Hart AA, Peterse JL, Horiot JC, et al. Impact of pathological characteristics on local relapse after breast-conserving therapy: a subgroup analysis of the EORTC boost versus no boost trial. J Clin Oncol. 2009;27(30):4939–47.
Rapiti E, Verkooijen HM, Vlastos G, Fioretta G, Neyroud-Caspar I, et al. Complete excision of primary breast tumor improves survival of patients with metastatic breast cancer at diagnosis. J Clin Oncol. 2006;24(18):2743–9.
Kuerer HM, Newman LA, Smith TL, Ames FC, Hunt KK, et al. Clinical course of breast cancer patients with complete pathologic primary tumor and axillary lymph node response to doxorubicin-based neoadjuvant chemotherapy. J Clin Oncol. 1999;17(2):460–9.
Mauri D, Pavlidis N, Ioannidis JP. Neoadjuvant versus adjuvant systemic treatment in breast cancer: a meta-analysis. Journal National Cancer Institute. 2005;97(3):188–94.
Bevacizumab, Metronomic Chemotherapy (CM), Diet and Exercise After Preoperative Chemotherapy for Breast Cancer (ABCDE), NCT00925652, accessed on July 20, 2011. Available from: http://clinicaltrials.gov/ct2/show/NCT00925652.
Li X, Lewis MT, Huang J, Gutierrez C, Osborne CK, et al. Intrinsic resistance of tumorigenic breast cancer cells to chemotherapy. Journal National Cancer Institute. 2008;100(9):672–9.
Creighton CJ, Li X, Landis M, Dixon JM, Neumeister VM, et al. Residual breast cancers after conventional therapy display mesenchymal as well as tumor-initiating features. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(33):13820–5.
Rastogi P, Anderson SJ, Bear HD, Geyer CE, Kahlenberg MS, et al. Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol. 2008;26(5):778–85.
Citron ML, Berry DA, Cirrincione C, Hudis C, Winer EP, et al. Randomized trial of dose-dense versus conventionally scheduled and sequential versus concurrent combination chemotherapy as postoperative adjuvant treatment of node-positive primary breast cancer: first report of Intergroup Trial C9741/Cancer and Leukemia Group B Trial 9741. J Clin Oncol. 2003;21(8):1431–9.
Baldini E, Gardin G, Giannessi PG, Evangelista G, Roncella M, et al. Accelerated versus standard cyclophosphamide, epirubicin and 5-fluorouracil or cyclophosphamide, methotrexate and 5-fluorouracil: a randomized phase III trial in locally advanced breast cancer. Ann Oncol. 2003;14(2):227–32.
Untch M, Fasching PA, Konecny GE, von Koch F, Conrad U, et al. PREPARE trial: a randomized phase III trial comparing preoperative, dose-dense, dose-intensified chemotherapy with epirubicin, paclitaxel and CMF versus a standard-dosed epirubicin/cyclophosphamide followed by paclitaxel {+/−} darbepoetin alfa in primary breast cancer--results at the time of surgery. Ann Oncol. 2011 Mar 23 (in press). This study is the first one to show a benefit in complete pathologic response rate with neoadjuvant dose-dense chemotherapy in triple-negative disease. Nonetheless, the benefit did not reach statistical significance, the regimens were similar but not identical, and pCR rate in triple-negative disease was not the primary endpoint.
von Minckwitz G, Kummel S, Vogel P, Hanusch C, Eidtmann H, et al. Neoadjuvant vinorelbine-capecitabine versus docetaxel-doxorubicin-cyclophosphamide in early nonresponsive breast cancer: phase III randomized GeparTrio trial. Journal National Cancer Institute. 2008;100(8):542–51.
Steger GG, Galid A, Gnant M, Mlineritsch B, Lang A, et al. Pathologic complete response with six compared with three cycles of neoadjuvant epirubicin plus docetaxel and granulocyte colony-stimulating factor in operable breast cancer: results of ABCSG-14. J Clin Oncol. 2007;25(15):2012–8.
von Minckwitz G, Kummel S, Vogel P, Hanusch C, Eidtmann H, et al. Intensified neoadjuvant chemotherapy in early-responding breast cancer: phase III randomized GeparTrio study. Journal National Cancer Institute. 2008;100(8):552–62.
von Minckwitz G, Untch M, Nuesch E, Loibl S, Kaufmann M, et al. Impact of treatment characteristics on response of different breast cancer phenotypes: pooled analysis of the German neo-adjuvant chemotherapy trials. Breast Cancer Research Treatment. 2011;125(1):145–56.
Early Breast Cancer Trialists' Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365(9472):1687–717.
Berry DA, Cirrincione C, Henderson IC, Citron ML, Budman DR, et al. Estrogen-receptor status and outcomes of modern chemotherapy for patients with node-positive breast cancer. JAMA. 2006;295(14):1658–67.
Colleoni M, Cole BF, Viale G, Regan MM, Price KN, et al. Classical cyclophosphamide, methotrexate, and fluorouracil chemotherapy is more effective in triple-negative, node-negative breast cancer: results from two randomized trials of adjuvant chemoendocrine therapy for node-negative breast cancer. J Clin Oncol. 2010;28(18):2966–73.
Gonzalez-Angulo AM, Litton JK, Broglio KR, Meric-Bernstam F, Rakkhit R, et al. High risk of recurrence for patients with breast cancer who have human epidermal growth factor receptor 2-positive, node-negative tumors 1 cm or smaller. J Clin Oncol. 2009;27(34):5700–6.
Kaplan HG, Malmgren JA, Atwood M. T1N0 triple negative breast cancer: risk of recurrence and adjuvant chemotherapy. Breast Journal. 2009;15(5):454–60.
National Comprehensive Cancer Network. Breast Cancer, Version 2.2011. National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology version 2.2011.[accessed on July 17, 2011]; Available from: www.nccn.org.
Early Breast Cancer Trialists' Collaborative Group. Polychemotherapy for early breast cancer: an overview of the randomised trials. Early Breast Cancer Trialists' Collaborative Group. Lancet. 1998;352(9132):930–42.
Pritchard KI, Shepherd LE, O'Malley FP, Andrulis IL, Tu D, et al. HER2 and responsiveness of breast cancer to adjuvant chemotherapy. New England Journal Medicine. 2006;354(20):2103–11.
Hugh J, Hanson J, Cheang MC, Nielsen TO, Perou CM, et al. Breast cancer subtypes and response to docetaxel in node-positive breast cancer: use of an immunohistochemical definition in the BCIRG 001 trial. J Clin Oncol. 2009;27(8):1168–76.
Hayes DF, Thor AD, Dressler LG, Weaver D, Edgerton S, et al. HER2 and response to paclitaxel in node-positive breast cancer. New England Journal Medicine. 2007;357(15):1496–506.
Martin M, Rodriguez-Lescure A, Ruiz A, Alba E, Calvo L, et al. Molecular predictors of efficacy of adjuvant weekly paclitaxel in early breast cancer. Breast Cancer Research Treatment. 2010;123(1):149–57.
Wang S, Shi Y, Yuan Z, Wang X, Liu D, et al. Classical CMF regimen as adjuvant chemotherapy for triple-negative breast cancer may be more effective compared with anthracycline or taxane-based regimens. Medical Oncology 2011 Apr 29 (in press).
Lindman H, Kellokumpu-Lehtinen PL, Huovinen R, Jukkola-Vuorinen A, Tanner M, et al. Integration of capecitabine into anthracycline- and taxane-based adjuvant therapy for triple-negative early breast cancer: Final Subgroup Analysis of the FinXX Study. American Association for Cancer Research, 33rd Annual San Antonio Breast Cancer Symposium, December 8–12; 2010; San Antonio, TX.
Gluz O, Nitz UA, Harbeck N, Ting E, Kates R, et al. Triple-negative high-risk breast cancer derives particular benefit from dose intensification of adjuvant chemotherapy: results of WSG AM-01 trial. Ann Oncol. 2008;19(5):861–70.
Sparano JA, Wang M, Martino S, Jones V, Perez EA, et al. Weekly paclitaxel in the adjuvant treatment of breast cancer. New England Journal Medicine. 2008;358(16):1663–71.
Carrick S, Parker S, Thornton CE, Ghersi D, Simes J, et al. Single agent versus combination chemotherapy for metastatic breast cancer. Cochrane database of systematic reviews (Online). 2009(2):CD003372.
Sledge GW, Neuberg D, Bernardo P, Ingle JN, Martino S, et al. Phase III trial of doxorubicin, paclitaxel, and the combination of doxorubicin and paclitaxel as front-line chemotherapy for metastatic breast cancer: an intergroup trial (E1193). J Clin Oncol. 2003;21(4):588–92.
Thomas ES, Gomez HL, Li RK, Chung HC, Fein LE, et al. Ixabepilone plus capecitabine for metastatic breast cancer progressing after anthracycline and taxane treatment. J Clin Oncol. 2007;25(33):5210–7.
Bhattacharyya A, Ear US, Koller BH, Weichselbaum RR, Bishop DK. The breast cancer susceptibility gene BRCA1 is required for subnuclear assembly of Rad51 and survival following treatment with the DNA cross-linking agent cisplatin. J Biol Chem. 2000;275(31):23899–903.
Cancer and Leukemia Group B. Randomized Phase II 2 × 2 Factorial Trial of the Addition of Carboplatin +/− Bevacizumab to Neoadjuvant Weekly Paclitaxel Followed by Dose- Dense AC in Hormone Receptor-Poor/HER2-Negative Resectable Breast Cancer. 2011 June 9, 2011 (NCT00861705) accessed on June 9, 2011. Available from: http://www.clinicaltrials.gov/ct2/show/NCT00861705.
A Phase II Study of Cisplatin or Carboplatin for Triple-Negative Metastatic Breast Cancer and Evaluation of p63/p73 as a Biomarker of Response (NCT00483223), accessed on July 20, 2011. Available from: http://clinicaltrials.gov/ct2/show/NCT00483223.
Linderholm BK, Hellborg H, Johansson U, Elmberger G, Skoog L, et al. Significantly higher levels of vascular endothelial growth factor (VEGF) and shorter survival times for patients with primary operable triple-negative breast cancer. Ann Oncol. 2009;20(10):1639–46.
Linderholm BK, Lindahl T, Holmberg L, Klaar S, Lennerstrand J, et al. The expression of vascular endothelial growth factor correlates with mutant p53 and poor prognosis in human breast cancer. Cancer Research. 2001;61(5):2256–60.
Miles DW, Chan A, Dirix LY, Cortes J, Pivot X, et al. Phase III study of bevacizumab plus docetaxel compared with placebo plus docetaxel for the first-line treatment of human epidermal growth factor receptor 2-negative metastatic breast cancer. J Clin Oncol. 2010;28(20):3239–47.
Miller K, Wang M, Gralow J, Dickler M, Cobleigh M, et al. Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. New England Journal Medicine. 2007;357(26):2666–76.
Robert NJ, Dieras V, Glaspy J, Brufsky AM, Bondarenko I, et al. RIBBON-1: randomized, double-blind, placebo-controlled, phase III trial of chemotherapy with or without bevacizumab for first-line treatment of human epidermal growth factor receptor 2-negative, locally recurrent or metastatic breast cancer. J Clin Oncol. 2011;29(10):1252–60.
O'Shaughnessy J, Miles D, Gray RJ, Dieras V, Perez EA, et al. A meta-analysis of overall survival data from three randomized trials of bevacizumab (BV) and first-line chemotherapy as treatment for patients with metastatic breast cancer (MBC). 2010 American Society of Clinical Oncology Annual Meeting, Chicago, IL; J Clin Oncol 28:15s, 2010 (suppl; abstr 1005).
Burstein HJ, Elias AD, Rugo HS, Cobleigh MA, Wolff AC, et al. Phase II study of sunitinib malate, an oral multitargeted tyrosine kinase inhibitor, in patients with metastatic breast cancer previously treated with an anthracycline and a taxane. J Clin Oncol. 2008;26(11):1810–6.
Crown J, Dieras V, Staroslawska E, Yardley DA, Davidson N, et al. Phase III trial of sunitinib (SU) in combination with capecitabine (C) versus C in previously treated advanced breast cancer (ABC). 2010 American Society of Clinical Oncology Annual Meeting, Chicago, IL: Journal of Clinical Oncology, 28:18s (suppl; abstr LBA1011).
Bergh J, Greil R, Voytko N, Makhson A, Cortes J, et al. Sunitinib (SU) in combination with docetaxel (D) versus D alone for the first-line treatment of advanced breast cancer (ABC). 2010 American Society of Clinical Oncology Annual Meeting, Chicago, IL; J Clin Oncol 28:18s, 2010 (suppl; abstr LBA1010).
Phase I/II Trial of Neoadjuvant Sunitinib Administered With Weekly Paclitaxel/Carboplatin in Patients With Locally Advanced Triple-Negative Breast Cancer (NCT00887575). Accessed on July 19, 2011. Available from: http://www.clinicaltrials.gov/ct2/show/NCT00887575.
Hoeijmakers JH. DNA damage, aging, and cancer. New England Journal Medicine. 2009;361(15):1475–85.
O'Shaughnessy J, Osborne C, Pippen JE, et al. Iniparib plus chemotherapy in metastatic triple-negative breast cancer. New England Journal Medicine. 2011;364(3):205–14.
O'Shaughnessy J, Schwartzberg LS, Danso MA, Rugo HS, Miller K, et al. A randomized phase III study of iniparib (BSI-201) in combination with gemcitabine/carboplatin (G/C) in metastatic triple-negative breast cancer (TNBC). 2011 American Society of Clinical Oncology Annual Meeting, Chicago, IL: J Clin Oncol 29: 2011 (suppl; abstr 1007).
Isakoff SJ, Overmoyer B, Tung NM, Gelman RS, Giranda VL, et al. A phase II trial of the PARP inhibitor veliparib (ABT888) and temozolomide for metastatic breast cancer. 2010 American Society of Clinical Oncology Annual Meeting, Chicago, IL; Journal of Clinical Oncology 28:15s. 2010 (suppl; abstr 1019).
PARP inhibition after preoperative chemotherapy in patients with triple negative breast cancer or ER/PR +, HER2 negative with known BRCA1/2 mutations: Hoosier Oncology Group BRE09-146 (NCT01074970). Accessed on July 19, 2011. Available from: http://clinicaltrials.gov/ct2/show/NCT01074970.
Turner NC, Reis-Filho JS. Basal-like breast cancer and the BRCA1 phenotype. Oncogene. 2006;25(43):5846–53.
Hoadley KA, Weigman VJ, Fan C, Sawyer LR, He X, et al. EGFR associated expression profiles vary with breast tumor subtype. BMC Genomics. 2007;8:258.
Carey LA, Irvin W, Rugo H, Mayer E, Marcom PK, et al. TBCRC 001: EGFR inhibition with cetuximab added to carboplatin in metastatic triple-negative (basal-like) breast cancer 2008 American Society of Clinical Oncology Annual Meeting, Chicago, IL; Journal of Clinical Oncology 26:15s 2008 (suppl; abstr 1009).
Green MD, Francis PA, Gebski V, Harvey V, Karapetis C, et al. Gefitinib treatment in hormone-resistant and hormone receptor-negative advanced breast cancer. Ann Oncol. 2009;20(11):1813–7.
Gutteridge E, Agrawal A, Nicholson R, Leung Cheung K, Robertson J, et al. The effects of gefitinib in tamoxifen-resistant and hormone-insensitive breast cancer: a phase II study. International Journal Cancer. 2010;126(8):1806–16.
Dickler MN, Cobleigh MA, Miller KD, Klein PM, Winer EP. Efficacy and safety of erlotinib in patients with locally advanced or metastatic breast cancer. Breast Cancer Research Treatment. 2009;115(1):115–21.
Ichikawa K, Liu W, Zhao L, Wang Z, Liu D, et al. Tumoricidal activity of a novel anti-human DR5 monoclonal antibody without hepatocyte cytotoxicity. Nature Medicine. 2001;7(8):954–60.
Buchsbaum DJ, Zhou T, Grizzle WE, Oliver PG, Hammond CJ, et al. Antitumor efficacy of TRA-8 anti-DR5 monoclonal antibody alone or in combination with chemotherapy and/or radiation therapy in a human breast cancer model. Clin Cancer Res. 2003;9(10 Pt 1):3731–41.
Ohtsuka T, Buchsbaum D, Oliver P, Makhija S, Kimberly R, et al. Synergistic induction of tumor cell apoptosis by death receptor antibody and chemotherapy agent through JNK/p38 and mitochondrial death pathway. Oncogene. 2003;22(13):2034–44.
Silver DP, Richardson AL, Eklund AC, Wang ZC, Szallasi Z, et al. Efficacy of neoadjuvant Cisplatin in triple-negative breast cancer. J Clin Oncol. 2010;28(7):1145–53.
Ogston KN, Miller ID, Payne S, Hutcheon AW, Sarkar TK, et al. A new histological grading system to assess response of breast cancers to primary chemotherapy: prognostic significance and survival. Breast (Edinburgh, Scotland). 2003;12(5):320–7.
Ryan PD, Tung NM, Isakoff SJ, Golshan M, Richardson A, et al. Neoadjuvant cisplatin and bevacizumab in triple negative breast cancer (TNBC): safety and efficacy. 2009 American Society of Clinical Oncology Annual Meeting, Chicago, IL; Journal of Clinical Oncology, 27:15S 2009 (suppl; abstr 551).
Frasci G, Comella P, Rinaldo M, Iodice G, Di Bonito M, et al. Preoperative weekly cisplatin-epirubicin-paclitaxel with G-CSF support in triple-negative large operable breast cancer. Ann Oncol. 2009;20(7):1185–92.
Torrisi R, Balduzzi A, Ghisini R, Rocca A, Bottiglieri L, et al. Tailored preoperative treatment of locally advanced triple negative (hormone receptor negative and HER2 negative) breast cancer with epirubicin, cisplatin, and infusional fluorouracil followed by weekly paclitaxel. Cancer Chemotherapy Pharmacology. 2008;62(4):667–72.
Byrski T, Huzarski T, Dent R, Gronwald J, Zuziak D, et al. Response to neoadjuvant therapy with cisplatin in BRCA1-positive breast cancer patients. Breast Cancer Research Treatment. 2009;115(2):359–63.
Baselga J, Stemmer S, Pego A, Chan A, Goeminne JC, et al. Cetuximab + cisplatin in estrogen receptor-negative, progesterone receptor-negative, Her2-negative (triple-negative) metastatic breast cancer: results of the randomized phase II BALI-1 trial. American Association for Cancer Research 2010. 33rd Annual San Antonio Breast Cancer Symposium, December 8–12; 2010; San Antonio, TX.
Maisano R, Zavettieri M, Azzarello D, Raffaele M, Maisano M, et al. Carboplatin and gemcitabine combination in metastatic triple-negative anthracycline- and taxane-pretreated breast cancer patients: a phase II study. Journal Chemotherapy (Florence, Italy). 2011;23(1):40–3.
Staudacher L, Cottu PH, Dieras V, Vincent-Salomon A, Guilhaume MN, et al. Platinum-based chemotherapy in metastatic triple-negative breast cancer: the Institut Curie experience. Ann Oncol. 2011;22(4):848–56.
Sirohi B, Arnedos M, Popat S, Ashley S, Nerurkar A, et al. Platinum-based chemotherapy in triple-negative breast cancer. Ann Oncol. 2008;19(11):1847–52.
Byrski T, Gronwald J, Huzarski T, Grzybowska E, Budryk M, et al. Pathologic complete response rates in young women with BRCA1-positive breast cancers after neoadjuvant chemotherapy. J Clin Oncol. 2010;28(3):375–9.
Tutt A, Robson M, Garber JE, Domchek SM, Audeh MW, et al. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and advanced breast cancer: a proof-of-concept trial. Lancet. 2010;376(9737):235–44.
Disclosure
The authors have no conflicts of interest relevant to this manuscript to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Level of Evidence
I: Evidence comes from multiple well-designed clinical trials conducted in representative populations with consistent results.
II: Evidence comes from at least one well-designed clinical study. Strength of evidence limited by the number, quality, or consistency of the individual studies.
III: Evidence comes from well-designed nonrandomized single-group or single-cohort studies or case–control studies. Evidence also comes from retrospective analyses of prospective clinical trials.
IV: Evidence comes from well-designed nonexperimental studies such as comparative correlational, and descriptive studies.
V: Evidence comes from case reports or case series and therefore, is insufficient for recommendations.
Rights and permissions
About this article
Cite this article
Vaklavas, C., Forero-Torres, A. How do I Treat “Triple-Negative” Disease. Curr. Treat. Options in Oncol. 12, 369–388 (2011). https://doi.org/10.1007/s11864-011-0168-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11864-011-0168-y