Abstract
Background
Various biomarkers and clinical variables are used to determine the probability risk, diagnosis, and the prognosis of acute ischemic stroke, but effective markers are still warranted.
Aim
We aimed to determine the effectiveness of Hs-cTnI levels to predict the prognosis of AIS.
Methods
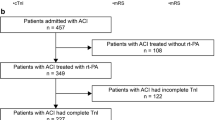
This study was planned as a retrospective observational study. Patients with available data and over 18 years old were included in the study. Diffusion magnetic resonance images were evaluated by a senior radiologist and the infarct size was calculated.
Results
We included 110 (54.2%) males and 93 (45.8%) females; a total of 203 patients with a mean age of 68.9 were included in the present study. Patients were divided into two groups according to the cut-off level of Hs-troponin-I (group I: lower than 8.5 mg/dL; group 2: higher than 8.5 mg/dL). These two groups were compared for mortality and infarct volume. Infarct volume and the mortality ratio of the group 2 was significantly higher [p = 0.041, U = 4294.5, LV = 6.5 (IQR = 1.8–25.4)].
Conclusions
Hs-troponin I may be an effective biomarker in predicting the prognosis of patients with acute ischemic stroke. Multicenter comprehensive prospective studies are warranted to obtain stronger results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute stroke is the second death reason with a ratio of 11% on earth [1]. Besides this high mortality ratio, it causes chronic sequel in survivors and a common cause of disability [1,2,3]. An immediate diagnosis and treatment should be administered when this high mortality and disability ratio is considered. It is also important to predict the prognosis to determine the requirement of aggressive treatment in selected patients.
Troponin protein complex is consisted of troponin C, I, and T subunits and contributes to striated muscle contraction modulation. Cardiac troponin C is similar to skeletal muscle isoform but troponin I and T are defined as cardiac specific isoforms. Recently, new generation high sensitive troponin (hs-cTns) provides measuring 5–10 times lower concentrations than conventional troponins and also provides to detect smaller ischemic areas of heart muscle [4]. By this way, besides the routinely use of cardiac troponins (cTns) in the diagnosis of acute myocardial infarction (AMI), they also show an increment in cardiac muscle diseases such as rapid response ventricular atrial fibrillation, congestive heart failure, cardiomyopathy and pulmonary embolism, severe sepsis, acute ischemic stroke (AIS), and chronic renal failure (CRF) [5, 6].
Nowadays, various biomarkers and clinical variables (elder age, AF existence, severity of the symptoms etc.) are used to determine the probability risk, diagnosis, and the prognosis of AIS, but effective markers are still warranted. In this study, we aimed to determine the effectiveness of Hs-cTnI levels to predict the prognosis of AIS.
Materials and methods
Study design
After the ethics committee approval (Health Science University, Adana City Research and Training Hospital, Ethics Committee, Meeting Number: 80, Decision Number: 1395, Date: 06/May/2021), we included patients diagnosed with AIS in the emergency department (ED) between 1 Jan 2020 and 31 Dec 2020 in this retrospective observational study. Patient data was obtained from hospital automation system.
Diffusion magnetic resonance images were evaluated by a senior radiologist and the infarct size was calculated. Demographic data, Glasgow Coma Scale (GCS), CBC, AST, ALT, BUN, Cr, coagulation parameters, BNP, CK-MB, and Hs-cTn-I levels were noted.
Patients with available data and over 18 years old were included in the study. Patients with hemorrhagic stroke, mass, and lesions apart from AIS were excluded. We also excluded patients under 18 years old, patients with missed data, patients diagnosed with acute coronary syndrome, cardiac arrest patients (inhospital-out of hospital) who were not return to spontaneous circulation, patients with rheumatologic and oncologic diagnosis, and patients who underwent chemotherapy/radiotherapy.
Laboratory analyses
WBC, Hb, Hct, platelet, monocyte count, neutrophil count, BUN, Cr, AST, ALT PTZ, INR, Aptt, CK-MB, and Hs-troponin I levels were noted. CBC was analyzed via Sysmex XN 10 (Automated Hematology Analyzer XN series, Sysmex Corporation, 1–5-1 Wakinnohama-Kaigandori, Chuo-ku, Kobe 651–0073, Japan) and biochemical parameters were measured with Beucher Coulter AU5800 (Beckman Coulter GmbH, Europark Fichtenhain B 13, 47,807 Krefeld, Germany) device.
Calculation of infarct volume
The brain diffusion MR images of the patients were screened via 1.5 T and 3 T Philips Ingenia. Acute infarct volume was measured with tumor tracking method via Philips İntelliSpace Workstation (Fig. 1). Apparent diffusion coefficient (ADC) mapping was used in the diffusion weighted images. Diffusion limited areas were manually drawn with 3D-ROI (region-of-interest). The volume of diffusion limitation signals was noted as cm3.
Statistical analyses
Statistical comparisons were performed using the statistical software package SPSS 25.0 (SPSS Inc., Chicago, IL, USA). The Shapiro–Wilk test was used to control for normal distribution. The normally distributed variables were evaluated with independent sample t-test and for three or more groups we used one-way ANOVA test. Non-normally distributed variables were analyzed using the Mann–Whitney U test and Kruskal–Wallis. Post hoc tests (Bonferroni for normally distributed groups and Tamhane’s T2 test for non-normally distributed groups) were used to determine the source of the difference between groups. The categorical variables are expressed in frequencies and percentages. Chi-square test was used to compare the categorical data. Definitive statistics were expressed as mean ± SD and median (interquartile range, IQR). A p value < 0.05 was considered significant. Cut-off values were determined via ROC curve.
Results
We included 110 (54.2%) males and 93 (45.8%) females; a total of 203 patients with a mean age of 68.9 were included in the present study. Demographic data, presentation symptoms, comorbidities, GCS, and Hs-Trop-I levels are given in Table 1.
According to categorical variable analyses, mortality ratio of the patients with diabetes mellitus is significantly higher both in survivor and the non-survivor group (Table 2).
When we considered the patients according to the outcome (discharged/ex), mortality increased with age and high hs-troponin I level; similarly, GSC was negatively related with mortality (Table 3).
Cut-off level of Hs-troponin-I level for mortality prediction was 8.5 mg/dL according to ROC curve (Fig. 2, Table 4).
Patients were divided into two groups according to the cut-off level of Hs-troponin-I (group I: lower than 8.5 mg/dL; group 2: higher than 8.5 mg/dL). These two groups were compared for mortality and infarct volume (Table 6). Infarct volume and the mortality ratio of the group 2 was significantly higher [p = 0.041, U = 4294.5, LV = 6.5 (IQR = 1.8–25.4)] (Tables 5 and 6).
Patients were categorized according to GCS (mild-GCS: 13–15, moderate-GCS: 9–12, and severe-GCS: 3–8) and these groups were compared for mortality and infarct volume. Hs-troponin-I levels and infarct volume increased with low GCS. Hs-troponin-I levels were higher in moderate GCS than mild GCS. Infarct volume was higher in severe GCS than mild GCS (Fig. 3).
Discussion
Cardiac complication risk of ischemic stroke patients are correlated with severity of the stroke and neurologic dysfunction [7]. So, besides the administration of immediate and appropriate treatment of stroke patients in the ED, we also carefully observe the cardiac biomarkers [8]. Troponin levels were high in 48 (23.26%) patients in our study. Hs-trop levels higher than 8.5 mg/dL were 68% sensitive and 54% specific. Mortality ratios were significantly higher in patients whose Hs-troponin levels higher than 8.5 mg/dL. Infarct volume and GCS which are very important for prognosis in stroke were significantly correlated with hs-trop I level.
Although the etiology of high troponin levels in stroke patients is not clear, various theories have been suggested. The first one is the incidental existence of acute coronary syndrome [9]. The second and the commonly accepted theory includes activation of sympathoadrenal system with increased intracranial pressure due to acute cerebral lesions. Serum troponin level increase with the activation of this system and myocyte degeneration (myocytolysis) because of high catecholamine secretion. Recently, incidence of high hs-trop levels is common in AIS because of usual measurement of hs-trop levels. According to a systemic review published in 2009, this high ratio of hs-trop is 5–34% [10]. In Scheitz et al.’s study [11], this ratio was 50%. In our study, 23.6% patients’ hs-trop levels were high and this ratio was 41.17% among non-survivors.
Infarct area size is an important parameter to determine the severity, ability after recovery, and the prediction of prognosis in AIS [12]. Kimura et al. suggested that wide lesion volume in diffusion weighted screening was associated with poor clinical outcome [13]. Similarly, Pop et al. showed that the poor prognosis was related with lesion volume and hs-trop was correlated with lesion volume [14]. In our study, lesion volume and mortality were not directly correlated but mean lesion volume was larger in non-survivors. Besides, hs-trop levels increased with the increment in lesion volume. This correlation made us think that increased intracranial pressure caused a sympathoadrenal discharge and myocyte damage.
Hypertension is a potential risk factor for AIS with a ratio of 54% [15, 16]. Similarly, DM is also an important risk factor for AIS. According to literature, existence of DM in the patient with AIS is related with rehospitalization, poor prognosis, and high mortality rates (including all reasons) within next 3 years [17]. The prognosis of AIS patients with DM was poor when compared with non-diabetics in Pop et al.’s study [14]. In our study, 58.1% of the patients had DM and hypertension and mortality ratio was higher in patients with DM.
Limitations
This retrospective study was a single-center study and included limited count of patients. And our patient group was not constituted of follow-up study population. One of the limitations of our study is that the duration of symptoms could not be determined exactly. For this reason, the relationship between the hs-troponin I levels studied from the blood sample taken at the time of admission to the emergency department could not be examined.
Conclusion
Clinicians have been struggling to determine a biomarker for diagnosis and prediction of prognosis in AIS. Among these biomarkers, Hs-Trop-I may be an effective biomarker in predicting the prognosis of these patients. Multicenter comprehensive prospective studies are warranted to obtain stronger results.
Availability of data and materials
Data and materials are reachable from hospital automation information systems.
References
WHO (2020) The top 10 causes of death. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
Katan M, Luft A (2018) Global burden of stroke. Semin Neurol 38(2):208–211. https://doi.org/10.1055/s-0038-1649503
Donkor ES (2018) Stroke in the 21st century: a snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat 2018:3238165. Published 2018 Nov 27. https://doi.org/10.1155/2018/3238165
Giannitsis E, Kurz K, Hallermayer K, Jarausch J, Jaffe AS, Katus HA (2010) Analytical validation of a high-sensitivity cardiac troponin T assay. Clin Chem 56(2):254–261. https://doi.org/10.1373/clinchem.2009.132654
Latini R, Masson S, Anand IS et al (2007) Prognostic value of very low plasma concentrations of troponin T in patients with stable chronic heart failure. Circulation 116(11):1242–1249. https://doi.org/10.1161/CIRCULATIONAHA.106.655076
Røsjø H, Varpula M, Hagve TA et al (2011) Circulating high sensitivity troponin T in severe sepsis and septic shock: distribution, associated factors, and relation to outcome. Intensive Care Med 37(1):77–85. https://doi.org/10.1007/s00134-010-2051-x
Chen Z, Venkat P, Seyfried D, Chopp M, Yan T, Chen J (2017) Brain-Heart Interaction: Cardiac Complications After Stroke. Circ Res 121(4):451–468. https://doi.org/10.1161/CIRCRESAHA.117.311170
Xu C, Zheng A, He T, Cao Z (2020) Brain-heart axis and biomarkers of cardiac damage and dysfunction after stroke: a systematic review and meta-analysis. Int J Mol Sci 21(7):2347. Published 2020 Mar 28. https://doi.org/10.3390/ijms21072347
Jensen JK, Atar D, Mickley H (2007) Mechanism of troponin elevations in patients with acute ischemic stroke. Am J Cardiol 99(6):867–870. https://doi.org/10.1016/j.amjcard.2006.10.052
Kerr G, Ray G, Wu O, Stott DJ, Langhorne P (2009) Elevated troponin after stroke: a systematic review. Cerebrovasc Dis 28(3):220–226. https://doi.org/10.1159/000226773
Scheitz JF, Lim J, Broersen LHA et al (2021) High-sensitivity cardiac troponin T and recurrent vascular events after first ischemic stroke. J Am Heart Assoc 10(10):e018326. https://doi.org/10.1161/JAHA.120.018326
Saunders DE, Clifton AG, Brown MM (1995) Measurement of infarct size using MRI predicts prognosis in middle cerebral artery infarction. Stroke 26(12):2272–2276. https://doi.org/10.1161/01.str.26.12.2272
Kimura K, Iguchi Y, Shibazaki K et al (2008) Large ischemic lesions on diffusion-weighted imaging done before intravenous tissue plasminogen activator thrombolysis predicts a poor outcome in patients with acute stroke. Stroke 39(8):2388–2391. https://doi.org/10.1161/STROKEAHA.107.510917
Pop NO, Tit DM, Diaconu CC et al (2021) The Alberta Stroke Program Early CT score (ASPECTS): a predictor of mortality in acute ischemic stroke. Exp Ther Med 22(6):1371. https://doi.org/10.3892/etm.2021.10805
Benjamin EJ, Muntner P, Alonso A et al (2019) Heart disease and stroke statistics-2019 update: a report from the American Heart Association [published correction appears in Circulation. 2020 Jan 14;141(2):e33]. Circulation 2019;139(10):e56-e528. https://doi.org/10.1161/CIR.0000000000000659
Boehme AK, Esenwa C, Elkind MS (2017) Stroke risk factors, genetics, and prevention. Circ Res 120(3):472–495. https://doi.org/10.1161/CIRCRESAHA.116.308398
Echouffo-Tcheugui JB, Xu H, Matsouaka RA et al (2018) Diabetes and long-term outcomes of ischaemic stroke: findings from Get With The Guidelines-Stroke. Eur Heart J 39(25):2376–2386. https://doi.org/10.1093/eurheartj/ehy036
Author information
Authors and Affiliations
Contributions
Dr. Aksu Arif, Dr. Icme Ferhat, Dr. Avci Akkan, Dr. Yolcu Sadiye, Dr. Sumbul Hilmi Erdem, Dr. Kaya Adem, and Dr. Avci Begum Seyda: conceptualization, methodology, investigation, and writing—original draft. Dr. Tugcan Mustafa Oguz, Dr. Demir Ozan, Dr. Arici Fatih Necip, Dr. Ozturk Huseyin Ali, and Dr. Dilek Okan: resources, formal analysis, and writing—review and editing. Dr. Sumbul, Dr. Avci A, and Dr. Yolcu: conceptualization, methodology, and writing—review and editing. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The ethics committee of Health Science University, Adana City Research and Training Hospital approved the study. The study was performed according to the recommendations set by the Declaration of Helsinki on medical research involving human subjects.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Any part of this paper is not under consideration for publishing or published in anywhere else.
Rights and permissions
About this article
Cite this article
Aksu, A., Avci, A., Yolcu, S. et al. The relationship between infarct volume and high sensitivity troponin I level in patients diagnosed with ischemic stroke. Ir J Med Sci 192, 901–906 (2023). https://doi.org/10.1007/s11845-022-03048-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-022-03048-0