Abstract
Background
Multiple sclerosis (MS) is a chronic, progressive, and neurodegenerative central nervous system disorder. MS usually causes disability, cognitive deficiency, fatigue, and depression symptoms.
Objectives
To assess cognitive functions of people with MS (pwMS) and investigate the impact of depression, fatigue, and disability on cognitive functions.
Methods
We administered the Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS) battery to assess 200 pwMS. The Expanded Disability Status Scale (EDSS) was used to evaluate disability levels. Fatigue Severity Scale (FSS) and the Beck Depression Inventory (BDI) were used, respectively, for fatigue and depression levels.
Results
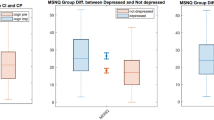
EDSS and FSS scores were significantly higher in those with a disease duration of 5 years or more. Those with the EDSS ≥ 4 were found to have lower BICAMS performances and higher FSS scores. There was a significant difference in Symbol Digit Modalities Test (SDMT) performances between the groups with and without fatigue (FSS ≥ 4 and FSS < 4, respectively). When depression and fatigue symptoms concur or in the existence of just one of them or none of them, significant differences in terms of SDMT performances have been shown.
Conclusion
The level of disability and fatigue adversely affects the cognitive functions of pwMS; depression has no significant effect. BICAMS that is specific for MS can be beneficial to assess the cognitive state of pwMS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is a chronic, progressive, autoimmune, neurodegenerative disorder that occupies the central nervous system (CNS); its pathogenesis includes axon loss and demyelination [1]. MS causes brain atrophy and widespread lesions or plaques in the brain and spinal cord [2]. These involvements in the CNS may result in disability in various areas, including motor, sensory, visual, balance-coordination, and cognitive impairment (CI) [3]. Different studies have reported the prevalence of cognitive decline in MS as 43–73% [4]. Cognitive areas affected are information processing speed, complex attention, visual learning, episodic memory, delayed recall, and executive functions [5, 6]. CI is a frequent symptom is explained by the existence of a significant number of separate lesions, diffuse axonal injury [7], and white and gray matter damages [8].
The diagnostic ratio of lifelong major depression in people with MS (pwMS) is approximately 50% [9]. Moreover, the prevalence of fatigue, which is considered closely related to depression, is 50–90% [10]. The composite effect of CI, depression, and fatigue affects the decision-making processes of pwMS, limiting their mental flexibility capacities; therefore, they can take a toll on daily activities, quality of life, and mental health [11]. Apart from the objective neurological status, evaluation of cognitive function, fatigue, and depression in pwMS is essential in terms of adherence to treatment, benefit from treatment, and planning of individual rehabilitation programs in order to improve the disability of pwMS. This study aimed to evaluate the cognitive functions of pwMS and investigate the relationship between depression, fatigue, disability, and cognitive functions.
Materials and methods
Participants
We interviewed 203 pwMS, who were followed by the MS Clinic of the Dokuz Eylul University (DEU) Hospital. Patients who applied to our clinic were invited to this study according to the order of application. It was informed that their participation in the study would not provide interest for them, but cognitive involvement would be determined. We could not complete tests in three pwMS because they had to back to work. The criteria for patient inclusion were (a) aged 18–55 years, (b) diagnosed with MS according to the “McDonald 2010 criteria”, and (c) signed the informed consent form. The exclusion criteria were (a) absence or non-completion of the data form, (b) having additional neurological and/or psychological disorders that could influence the clinical evaluation and cognitive tests, (c) antipsychotic drug use, severe head trauma history, (d) having a learning disability or mental retardation, (e) being a pregnant or lactating woman, (f) prior or current history of substance or alcohol dependence, (g) MS relapse and/or taking corticosteroid treatment within four weeks of the assessment.
Cognitive assessment
Brief International Cognitive Assessment for MS (BICAMS) is a test battery with robust psychometric features [12]; it consists of the Symbol Digit Modalities Test (SDMT) [13], initial learning trials of the California Verbal Learning Test–second edition (CVLT-II) [14], and Brief Visuospatial Memory Test–Revised (BVMT-R) [15]. A Turkish validity study for BICAMS was conducted by Ozakbas et al. [16] in Turkey. As no validated threshold of CI for BICAMS was available, CI for a single test was defined as 1.5 standard deviations (SD) below the control group mean in the validity study [17].
The SDMT primarily measures visuospatial scanning, constant attention and concentration, information processing speed, and narrowly, working memory [13]. In this study, the Rao (oral version) adaptation of the SDMT was individually used. On top of the test page, there is a key in divided blocks that matches nine numbers and symbols. The participant is asked to pair the pseudo-randomized digits with each symbol as quickly as possible over 90 s. The oral version of the task was selected, and the number of correct answers was recorded (highest score, 110).
The CVLT-II is the standard scale for auditory/verbal learning and memory in clinical neuropsychology [18]. It consists of 16 words divided into four categories (four tools, fruits, and animals, and furniture). In this study, the application covered the first five trials of the test, which assesses verbal memory. The total learning score indicates the total number of words recalled (highest score, 80).
The BVMT-R includes three recall trials for visuospatial learning and memory [15]. Participants are shown a stimulus card for 10 s on which six geometric shapes are printed in a 2 × 3 pattern. They are asked to draw as many symbols as they can remember. These symbols are scored from 0 to 2 based on accuracy and location. The total score consists of the sum of scores across the three trials (highest score, 36).
Other measurements
The Fatigue Severity Scale (FSS) consists of nine statements on a 7-point scale. The patient is asked to mark the level of fatigue in the last week, including the day the test was applied. The result is calculated by dividing the total score by the number of items [19]. The cutoff value of fatigue was defined as four and above in this study [20].
The Beck Depression Inventory (BDI) is administered to evaluate the degree of self-reported depression, with 21 items rated on a scale of 0–3. If the total score is 17 or above, it indicates depression [21] (highest score, 63).
Functional systems are evaluated based on the clinician’s interview and neurological examination, then the Expanded Disability Status Scale (EDSS) score is obtained. In this scale, consisting of 20 steps with 0.5 intervals, 0 indicates a normal neurological exam, while 10 refers to death due to MS [22].
Procedures
These procedures were approved by the Non-Invasive Research Ethics Committee of DEU. All pwMS provided written informed consent to participate in the study (code: 2016/12-21). First, they completed the demographics questionnaire, and then the medical history was obtained; this was followed by administered of the FSS and BDI. BICAMS neuropsychological battery was administered by a board-certified psychologist (SDMT, CVLT-II, BVMT-R respectively), and a neurologist evaluated the Expanded Disability Status Scale (EDSS) scores.
Statistical analysis
Data analysis was conducted using the SPSS Statistics Version 20.0 software package. Descriptive statistics were shown as means and SD for numerical variables and numbers with percentages for categorical variables. Two group comparisons were obtained by t tests in the individual groups. A composite effect of depression and fatigue was expressed by a one-way analysis of variance (ANOVA). The Pearson correlation coefficient r was used to determine the relationship between the numerical variables. CI for a single test was defined as 1.5 SD below the control group mean in the Turkish validity study [16], we carried out a risk analysis of our study group (mean age 36.5 vs 37.5, mean education level 11.9 vs 13.9). To examine independent predictors of CI, binary logistic regression analysis was used to evaluate associations among all three BICAMS raw scores (SDMT, BVMT-R, and CVLT-II total learning), age, gender, education level, disease duration, fatigue, depression, and disability level (A predictor assessed was not examined while controlling for another predictor). As p value ≤ 0.05 was considered statistically significant.
Results
Demographic and clinical characteristics
One hundred and forty females (70%) and 60 males (30%) diagnosed with MS were included in the study. Of the 200 pwMS, 191 had relapsing remitting-MS (RRMS) (95%), 6 secondary progressive-MS (SPMS) (6%), and 3 primary progressive-MS (PPMS) (2%). The sample included pwMS receiving immunomodulation therapy (oral: 38%; injectable: 56%) and who had stopped treatment for a while (6%; due to pregnancy plan, stable PPMS). The mean age of pwMS was 36.53 ± 9.73 years, and the mean length of education was 11.98 ± 3.55 years. The sociodemographic characteristics are shown in Table 1.
The average depression score of the group was 9.93 ± 9.06, fatigue score was 3.15 ± 1.84, and EDSS score was 1.78 ± 1.58; the average disease duration was 6.17 ± 4.85 years. 124 pwMS did not suffer from depression or fatigue (62.0%), while 22 pwMS have both depression and fatigue (11%). The clinical characteristics are shown in Table 2.
Cognitive outcome and correlation analyses
The mean scale scores for pwMS were as follows: SDMT, 47.99 ± 12.15; CVLT-II, 52.87 ± 11.13; and BVMT-R, 25.10 ± 6.53. CI was identified in 66 pwMS (33%) in one or more BICAMS sub-tests. The raw BICAMS values of pwMS with and without CI are shown in Table 3.
A moderate association was found between BICAMS and both the age and years of education (Table 4). Age, education years, disease duration, EDSS, BDI, occupation/employment status (females employed 31.4%, males 41.7%), and monthly income did not differ significantly between female and male pwMS. However, it was observed that the CVLT-II scores of females were significantly higher than those of males (r = 2.95, P < 0.05) (Table 5). The FSS scores of females were significantly higher than those of males (M = 3.33 versus 2.73, P = 0.031). A weak negative correlation between the FSS and both SDMT and BVMT-R (respectively, r = − 0.24, P = 0.001, r = − 0.14, P = 0.04), but not between the BDI and BICAMS, was found. The relationship among sociodemographic, clinical features, and BICAMS scores were shown in Table 4.
Between-group analyses
The disease duration was categorized as ≤ 5 years or > 5 years [23], and disability was categorized as EDSS < 4 or ≥ 4 [24, 25]. Furthermore, it was found that the BICAMS scores of the group with EDSS < 4 were significantly higher than those of pwMS with EDSS ≥ 4 (SDMT r = 5.60, CVLT-II r = 5.36, BVMT-R r = 4.42, P < 0.001). SDMT scores of pwMS without fatigue (FSS < 4) were significantly higher than those of pwMS with fatigue (FSS ≥ 4) (r = 2.99, P = 0.003). The cognitive functions of the pwMS according to their sociodemographic and clinical characteristics are shown in Table 5.
Disability and fatigue levels for pwMS with a disease duration of ≥ 5 years (long-term group) were significantly higher than those in the group with < 5 years since diagnosis (short-term group) (χ2 = 11.853, P < 0.001 for EDSS, χ2 = 1,021, P = 0.034 for FSS). Depression scores were found to be higher for the short-term than the long-term group (χ2 = 0.821, P > 0.05). Education years, occupation/employment status, and monthly income did not differ significantly between the short- and long-term groups. When the composite effect of depression and fatigue was examined, a significant difference was found between the groups in terms of SDMT scores (F = 3.771, P = 0.025).
Binary regression analyses
Gender was not significantly predictive in the binary regression analysis, so it was dropped from further analysis. The disease duration, FSS, and BDI scores were not significantly predictive either. When the education level was increased by 1 year, the SDMT scores increased by 0.8 points (P < 0.001 Exp(B): 0.827, 95% C.I. 0.744–0.919) and the CVLT-II scores by 0.9 points (P < 0.001 Exp(B): 0.869, 95% C.I. 0.777–0.972). When age was increased by 1 year, the SDMT scores decreased by 1.1 points (P = 0.009 Exp(B): 1.062, 95% C.I.1.015–1.111) (Table 6). When the EDSS increased by 1 point, the SDMT scores decreased by 1.4 points (P = 0.019 Exp(B): 1.366, 95% C.I. 1.053–1.772), and CVLT-II scores by 1.5 points (P < 0.001 Exp(B): 1.507, 95% C.I. 1.173–1.937) (Table 6).
Discussion
The present study examined that the relationship between cognitive functions and demographic-clinical features with 200 pwMS. Our findings revealed that pwMS with higher fatigue level have lower information-processing speeds, and all BICAMS scores of those with higher disability were significantly lower; nevertheless, there were no significant differences between the groups with/without depression in cognitive performance. Importantly, considering the cognitive effects of depression and fatigue symptoms coupling, the only significant difference was seen related to the information-processing speed.
Several studies have noted that age and education level are related to BICAMS performance, and substantive predictors of employment status at an early stage of disease [26, 27]. In the current study, the correlation results among age, education, and BICAMS supported the idea of taking into consideration the demographic characteristics, as well as clinical variables. Interestingly, verbal memory scores of women were higher than those of men in our study, although there were no sex differences found in any demographic or clinical characteristics, except fatigue level. Previous studies have suggested that females establish strategies for organization and spatial memory tasks via verbal memory [28, 29], and women performed significantly better than men on the verbal memory test [30].
We have determined the CI group according to the average BICAMS data of our previous study [16]. In line with the literature, age was negatively related to SDMT, and education was positively related to SDMT and CVLT-II in our study [31, 32]. With cognitive impairment defined as at least one or more abnormal tests [33, 34], it was 33% of pwMS with CI in one or more BICAMS subtests. The lower frequency of CI in our study group may be explained by the lower disability level and shorter disease duration.
Fatigue is the most frequently seen complaint in pwMS [3]. PwMS have to cope with the difficulties caused by the disability, which increases both psychological, physical, and cognitive fatigue. Our results revealed that those with higher disability (EDSS ≥ 4) and longer disease duration (> 5 years) had significantly higher fatigue scores. In contrast, depression scores were higher in the short-term group (≤ 5 years). It is possible that pwMS may face difficulties in coping with cognitive, emotional, behavioral, social, and physical factors affecting the adaptation of the individual to the disease in the early stages. Furthermore, the information-processing speeds of the group with fatigue were significantly worse than that of the group without fatigue, using a similar cut-off in a previous study [20]. Although it is possible to presumptively claim that fatigue may have adverse effects on the cognitive skills of pwMS, recent studies indicate that the relationship with cognitive status and subjective fatigue may not be as significant as expected [35,35,37].
Some researchers define primary fatigue as the absence of other indications (pain, depression, poor sleep, life quality, etc.) related to this condition and secondary fatigue as when such symptoms are present [20]. Considering the cognitive effects of depression and fatigue symptoms coupling, the only significant difference found related to the SDMT. This analysis is necessary because fatigue and depression are frequently intertwined. They may not be differentiated, or one may obscure the other. This difference is observed in SDMT because the test requires high-level working memory as Paced Auditory Serial Addition Test, with the information processing speed measuring primarily as a strong predictor of functional regression [27], suggesting the significant effect of fatigue on information processing speeds. These results demonstrated that SDMT denoted as a sentinel test [38] should be prioritized to identify the relationship between cognitive deterioration and disease-related factors in clinical practice.
Our results are consistent with the findings that pwMS with higher disability level is lower in cognitive performance [24, 31]. A previous study reported that SDMT, CVLT-II, and BVMT-R (5.9, 3.7, and 2.3 points, respectively) scores decreased when the EDSS was increased by 1 point [31]. We carried out a risk analysis of our study group using the BICAMS average of the control group in our study [16]. Finally, the disability was negatively related to SDMT (1.4 points), and CVLT-II (1.5 points) scores also parallel with the literature. Based on these results, attention should be paid to the importance of evaluating cognitive changes, for example, when assessing disease progression and severity [39].
The finding that no significant difference was found between the groups with/without depression in terms of BICAMS is unexpected in the current study. Also, there were no differences in pwMS with/without depression on any demographic or clinical characteristics. These results supported the findings of previous studies that used the same neuropsychological assessment [26, 34, 37]. Even if depression does not influence the objective neuropsychological performance of pwMS, some evidence suggests that it affects their subjective perception of CI and emphasizes to focus on patient-informant discrepancies in need of further multifaceted treatments [40, 41].
Research has shown disease duration to be predictive of SDMT [42] or both SDMT and CVLT-II [43]. As stated in the results, a significant difference could not be identified in BICAMS subtests between the short- and long-term groups by the fifth year from disease onset [44]. This difference stems from the heterogeneity of the characteristics of the sample (age, disability level, medications taken) and differences in evaluation tools. In several studies with larger samples, more extensive and detailed cognitive batteries, or longitudinal design, the relationship between the disease duration and cognitive functions was demonstrated [23, 33, 45]. Thus, cross-sectional or longitudinal studies in pwMS with longer disease duration are needed.
The current study had several limitations. First, we could not obtain distinct and robust data about whether demographic and clinical variables may lead to the probability of increasing CI during the disease course due to the low representation of people with SPMS and PPMS. A second limitation of our study is a lack of cognitive measures related to the effect of depression and fatigue on delayed verbal recall. In addition to this limitation, our findings regarding depression and fatigue frequency probably reflect the low disability level and short disease duration of the study group. The identification of fatigue and depression may also have been lower because the adaptation of pwMS to their continuing treatment was high, the medical team gave them adequate information, and they participated in activities that could increase their life quality. It can be considered that the individual differences between the cognitive profiles of pwMS complicate the act of reaching a definitive conclusion. Thus, pwMS should be matched in terms of age, gender, education, and premorbid intellectual functioning (cognitive reserve) [46]; the collective effects of factors affecting the cognitive functions should also be examined in detail in longitudinal studies.
In conclusion, the existence of depression and fatigue symptoms concur is devastating consequences on information processing speed, and the increasing severity of fatigue and disability makes it difficult to cope with the already present cognitive insufficiency. There is a clear need for research toward the psychological resilience of pwMS in the early stages for developing the ability to cope with MS-related problems. Additionally, this study encourages using BICAMS evaluating cognitive functions quickly, in routine neuropsychological assessment in MS since it is a predictor of disability. Here, BICAMS was applied in a broader MS population when compared with similar studies conducted in Turkey. These data are supportive that early detection of CI and determining those who carry risk factors early for boosting the value of neurorehabilitation can facilitate benefit from early intervention and improve pwMS’s quality of life.
References
Merritt HH (2010) Merritt’s neurology, 12th edn. Lippincott Williams & Wilkins
Kutzelnigg A, Lucchinetti CF, Stadelmann C et al (2005) Cortical demyelination and diffuse white matter injury in multiple sclerosis. Brain 128(11):2705–2712. https://doi.org/10.1093/brain/awh641
Chiaravalloti ND, DeLuca J (2008) Cognitive impairment in multiple sclerosis. Lancet Neurol 7:1139–1151. https://doi.org/10.1016/S1474-4422(08)70259-X
Wallin MT, Wilken JA, Kane R (2006) Cognitive dysfunction in multiple sclerosis: assessment, imaging, and risk factors. J Rehabil Res Dev 43(1):63. https://doi.org/10.1682/jrrd.2004.09.0120
Benedict RHB, Cookfair D, Gavett R et al (2006) Validity of the minimal assessment of cognitive function in multiple sclerosis (MACFIMS). J Int Neuropsychol Soc 12:549–558. https://doi.org/10.1017/S1355617706060723
Langdon DW (2011) Cognition in multiple sclerosis. Curr Opin Neurol 24(3):244–249. https://doi.org/10.1097/WCO.0b013e328346a43b
Compston A, Coles A (2008) Multiple sclerosis. Lancet 372(9648):1502–1517. https://doi.org/10.1016/S0140-6736(08)61620-7
Calabrese M, Gajofatto A, Gobbin F et al (2015) Late-onset multiple sclerosis presenting with cognitive dysfunction and severe cortical/infratentorial atrophy. Mult Scler 21(5):580–589. https://doi.org/10.1177/1352458514542363
Feinstein A (2004) The neuropsychiatry of multiple sclerosis. Can J Psychiatry 49(3):157–163. https://doi.org/10.1177/070674370404900302
Flachenecker P, Kümpfel T, Kallmann B et al (2002) Fatigue in multiple sclerosis: a comparison of different rating scales and correlation to clinical parameters. Mult Scler 8(6):523–526. https://doi.org/10.1191/1352458502ms839oa
Glanz BI, Healy BC, Rintell DJ et al (2010) The association between cognitive impairment and quality of life in patients with early multiple sclerosis. J Neurol Sci 290(1-2):75–79. https://doi.org/10.1016/j.jns.2009.11.004
Langdon DW, Amato MP, Boringa J et al (2012) Recommendations for a brief international cognitive assessment for multiple sclerosis (BICAMS). Mult Scler 18(6):891–898. https://doi.org/10.1177/1352458511431076
Smith A (1982) Symbol digit modalities test: manual. Western Psychological Services, Los Angeles
Delis DC, Kramer JH, Kaplan E (2000) California verbal learning test, 2nd edn. Psychological Corporation, San Antonio, Texas
Benedict RHB (1997) Brief visuospatial memory test—revised professional manual. Psychological Assessment Resources, Odessa
Ozakbas S, Yigit P, Cinar BP et al (2017) The Turkish validation of the brief international cognitive assessment for multiple sclerosis (BICAMS) battery. BMC Neurol 17(1):208. https://doi.org/10.1186/s12883-017-0993-0
Parmenter BA, Testa SM, Schretlen DJ (2010) The utility of regression-based norms in interpreting the minimal assessment of cognitive function in multiple sclerosis (MACFIMS). J Int Neuropsychol Soc 16(1):6–16. https://doi.org/10.1017/S1355617709990750
Woods SP, Delis DC, Scott JC et al (2006) The California Verbal Learning Test–second edition: test-retest reliability, practice effects, and reliable change indices for the standard and alternate forms. Arch Clin Neuropsychol 21(5):413–420. https://doi.org/10.1016/j.acn.2006.06.002
Krupp LB, LaRocca NG, Muir-Nash J et al (1989) The fatigue severity scale. Arch Neurol 46:1121–1123
Andreasen AK, Spliid PE, Andersen H, Jakobsen J (2010) Fatigue and processing speed are related in multiple sclerosis. Eur J Neurol 17(2):212–218. https://doi.org/10.1111/j.1468-1331.2009.02776.x
Beck AT, Steer RA, Brown GK (1996) Beck depression inventory-second edition manual. The Psychological Corporation, San Antonio
Kurtzke JF (1983) Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDgiedSS). Neurology 33(11):1444. https://doi.org/10.1212/wnl.33.11.1444
Achiron A, Polliack M, Rao SM et al (2005) Cognitive patterns and progression in multiple sclerosis: construction and validation of percentile curves. J Neurol Neurosurg Psychiatr 76(5):744–749. https://doi.org/10.1136/jnnp.2004.045518
Patti F, Amato MP, Trojano M et al (2009) Cognitive impairment and its relation with disease measures in mildly disabled patients with relapsing–remitting multiple sclerosis: baseline results from the Cognitive Impairment in Multiple Sclerosis (COGIMUS) study. Mult Scler 15(7):779–788. https://doi.org/10.1177/1352458509105544
Prakash RS, Snook EM, Lewis JM et al (2008) Cognitive impairments in relapsing-remitting multiple sclerosis: a meta-analysis. Mult Scler 14(9):1250–1261. https://doi.org/10.1177/1352458508095004
Skorve E, Lundervold AJ, Torkildsen Ø, Myhr KM (2019) The Norwegian translation of the brief international cognitive assessment for multiple sclerosis (BICAMS). Mult Scler Relat Disord 36:101408. https://doi.org/10.1016/j.msard.2019.101408
Vanotti S, Smerbeck A, Benedict RH et al (2016) A new assessment tool for patients with multiple sclerosis from Spanish-speaking countries: validation of the Brief International Cognitive Assessment for MS (BICAMS) in Argentina. Clin Neuropsychol 30(7):1023–1031. https://doi.org/10.1080/13854046.2016.1184317
Frings L, Wagner K, Unterrainer J et al (2006) Gender-related differences in lateralization of hippocampal activation and cognitive strategy. Neuroreport 17(4):417–421. https://doi.org/10.1097/01.wnr.0000203623.02082.e3
Sunderaraman P, Blumen HM, DeMatteo D et al (2013) Task demand influences relationships among sex, clustering strategy, and recall: 16-word versus 9-word list learning tests. Cogn Behav Neurol 26(2):78–84. https://doi.org/10.1097/WNN.0b013e31829de450
Donaldson E, Patel VP, Shammi P, Feinstein A (2019) Why sex matters: a cognitive study of people with multiple sclerosis. Cogn Behav Neurol 32(1):39–45. https://doi.org/10.1097/WNN.0000000000000188
Giedraitienė N, Kizlaitienė R, Kaubrys G (2015) The BICAMS battery for assessment of lithuanian-speaking multiple sclerosis patients: relationship with age, education, disease disability, and duration. Med Sci Monit 21:3853. https://doi.org/10.12659/MSM.896571
Smerbeck A, Benedict RH, Eshaghi A et al (2018) Influence of nationality on the Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS). Clin Neuropsychol 32(1):54–62. https://doi.org/10.1080/13854046.2017.1354071
Dusankova JB, Kalincik T, Havrdova E, Benedict RHB (2012) Cross cultural validation of the minimal assessment of cognitive function in multiple sclerosis (MACFIMS) and the brief international cognitive assessment for multiple sclerosis (BICAMS). Clin Neuropsychol 26(7):1186–1200. https://doi.org/10.1080/13854046.2012.725101
O’Connell K, Langdon D, Tubridy N et al (2015) A preliminary validation of the brief international cognitive assessment for multiple sclerosis (BICAMS) tool in an Irish population with multiple sclerosis (MS). Mult Scler Relat Disord 4(6):521–525. https://doi.org/10.1016/j.msard.2015.07.012
Morrow SA, Rosehart H, Johnson AM (2015) Diagnosis and quantification of cognitive fatigue in multiple sclerosis. Cogn Behav Neurol 28(1):27–32. https://doi.org/10.1097/WNN.0000000000000050
Sandi D, Rudisch T, Füvesi J et al (2015) The Hungarian validation of the Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS) battery and the correlation of cognitive impairment with fatigue and quality of life. Mult Scler Relat Disord 4(6):499–504. https://doi.org/10.1016/j.msard.2015.07.006
Walker LA, Osman L, Berard JA et al (2016) Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS): Canadian contribution to the international validation project. J Neurol Sci 362:147–152. https://doi.org/10.1016/j.jns.2016.01.040
Van Schependom J, D'hooghe MB, Cleynhens K et al (2014) The Symbol Digit Modalities Test as sentinel test for cognitive impairment in multiple sclerosis. Eur J Neurol 21(9):1219–1e72. https://doi.org/10.1111/ene.12463
Costa SL, DeLuca J, Sandroff BM et al (2018) Role of demographic and clinical factors in cognitive functioning of persons with relapsing-remitting and progressive multiple sclerosis. J Int Neuropsychol Socb 24(2):139–146. https://doi.org/10.1017/S1355617717000777
Kinsinger SW, Lattie E, Mohr DC (2010) Relationship between depression, fatigue, subjective cognitive impairment, and objective neuropsychological functioning in patients with multiple sclerosis. Neuropsychology 24(5):573. https://doi.org/10.1037/a0019222
Van der Hiele K, Spliethoff-Kamminga NGA, Ruimschotel RP et al (2012) The relationship between self-reported executive performance and psychological characteristics in multiple sclerosis. Eur J Neurol 19(4):562–569. https://doi.org/10.1111/j.1468-1331.2011.03538.x
Niino M, Mifune N, Kohriyama T et al (2014) Apathy/depression, but not subjective fatigue, is related with cognitive dysfunction in patients with multiple sclerosis. BMC Neurol 14(1):3. https://doi.org/10.1186/1471-2377-14-3
Vanotti S, Smerbeck A, Eizaguirre MB et al (2018) BICAMS in the Argentine population: relationship with clinical and sociodemographic variables. Appl Neuropsychol Adult 25(5):424–433. https://doi.org/10.1080/23279095.2017.1323751
Achiron A, Chapman J, Magalashvili D et al (2013) Modeling of cognitive impairment by disease duration in multiple sclerosis: a cross-sectional study. PLoS One 8(8):e71058. https://doi.org/10.1371/journal.pone.0071058
Amato MP, Ponziani G, Siracusa G, Sorbi S (2001) Cognitive dysfunction in early-onset multiple sclerosis: a reappraisal after 10 years. Arch Neurol 58(10):1602–1606
Sumowski JF, Wylie GR, Gonnella A et al (2010) Premorbid cognitive leisure independently contributes to cognitive reserve in multiple sclerosis. Neurology 75(16):1428–1431. https://doi.org/10.1212/WNL.0b013e3181f881a6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yigit, P., Acikgoz, A., Mehdiyev, Z. et al. The relationship between cognition, depression, fatigue, and disability in patients with multiple sclerosis. Ir J Med Sci 190, 1129–1136 (2021). https://doi.org/10.1007/s11845-020-02377-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-020-02377-2