Abstract
Purpose
The aim of this study was to investigate the relation between the physical problems of children with CP and caregiving burden and the emotional expression characteristics of caregivers.
Methods
The study included 144 caregivers of child with cerebral palsy and Zarit Burden Interview (ZBI) and Expressed Emotion Scale (EES) will be applied to the caregivers who will participate in the study. Disease severity of children with cerebral palsy will be evaluated by the Gross Motor Function Classification System (GMFCS) and Manual Ability Classification System (MACS) in children with cerebral palsy. Communication Function Classification System (CFCS) will be used to examine the communication of children with their families.
Results
Accordingly, a positive, statistically significant, moderate correlation was found between the GMFCS, MACS, and CFCS scores and ZBI scores in patients with cerebral palsy (r ~ 0.50; p < 0.01). In this study, a positive, statistically significant but weak correlation was found between GMFCS, MACS, and CFCS scores and EES scores in patients with cerebral palsy (r ~ 0.30; p < 0.01). A statistically significant, moderate correlation was found between ZBI and EES (r ~ 0.50; p < 0.01).
Conclusion
According to the results of our study, as motor skills and communication skills decrease, especially the burden of caregivers increases and the family’s emotional expression processes are related to these variables. We think that in the long-term follow-up of children with CP, it may be useful to provide appropriate psychiatric support by evaluating caregivers appropriately.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization reports that there are a total of 650 million disabled individuals in the world, of which 200 million are children [1]. Cerebral palsy is defined as a group of disorders that occur as a result of permanent, non-progressive damage in the developing fetal or infant brain, causing movement and posture disorder and limited activity. It often affects sensation, perception, cognitive status, communication, and behavior. Further, it is accompanied with epilepsy and secondary musculoskeletal problems. Cerebral palsy (CP) is a description of a combination of symptoms that indicate chronic, non-progressive central nervous system dysfunction, manifested by abnormal muscle tone, abnormal posture and motor, and coordination disorder such as abnormal movement [2]. In Turkey, this rate was reported at 4.4 per 1000 live births in a study conducted in children 2–16 years of age [3].
At every development stage of a child with CP, new problems arise in the family. A child, who does not develop according to his chronological age, causes negative effects in the family. The presence of a child with CP affects especially the primary caregiver, mostly the mother [4]. Since the diagnosis is made, frequent visits to the hospital and caring for the child due to the disease and secondary complications associated with it, cause the mother to be unable to devote time to herself and her environment, economic problems, and deterioration of quality of life [5].
A person taking care of an individual who is incapable of performing daily life activities due to a physical or mental disorder is defined as a “caregiver” [6]. The prolongation of the average human life expectancy and the survival of diseases have led to an increase in the number of individuals in need of care [7, 8]. As a result of these developments, the concept of “caregiving” gained importance [7, 8].
The concept of burden in researches on caregiving is a subject that has been emphasized in recent years. caregiver burden (CB), related to caregiving, refers to multidimensional responses to caregivers such as physical, social, psychological, emotional, and economic problems [9]. Studies have shown that after a long-term of caregiving, CB can cause severe depression, anxiety, and decrease in physical health, social isolation, and burnout [10, 11].
Emotional expression (EE) is basically a way of communicating the needs and expectations of individuals to others. One of the environments in which interpersonal communication is intense is family. Emotional expression is accepted as an indicator of the emotional quality of family life, and it is stated that the individual exposed to uncontrolled and intense emotional expression will experience intense distress [12]. Studies have acknowledged that EE can represent complex interactions between patients and family caregivers, and that patients’ illness and behavior are an important part of the process that contributes to the origins and changes of EE in a family [13]. Studies have shown that patient criticism/hostility and excessive interest/interventionism are the main components of EE [14].
Criticism/hostility levels are related to families’ perceptions that patients’ problems/behaviors can be controlled by themselves. Excessive interest/interventionism tends to be more intrusive within family members. In addition, patients may experience more frustration when interacting with caregivers in families because of their high level of emotional intervention, intrusive and emotional exposure to them.
Family members who expect a healthy child and make all their plans for the future in this direction face many difficulties with a disabled child in various areas of life (social, work, financial). For this reason, caregivers struggle with many problems and uncertainties.
The aim of this study was to investigate the relation between the physical problems of children with CP and caregiving burden and the emotional expression characteristics of caregivers.
For this purpose, answers to the following questions were sought in this study:
-
1.
Is there a relation between caregiver burden and development levels of children with CP?
-
2.
Is there a relation between the emotional expression of caregivers and the development levels of children with CP?
Method
Sampling and data collection
The study included 144 caregivers of child with cerebral palsy who were admitted to the Physical Therapy and Rehabilitation Outpatient Clinic of Dışkapı Yıldırım Beyazıt Training and Research Hospital between May 2019 and September 2019. After the self-report scales were applied to the families who brought their children with cerebral palsy to the physical therapy and rehabilitation outpatient clinic, the examinations of the children were performed by 2 different physical medicine doctors and their psychiatric evaluations were performed by a psychiatrist. Caregivers with the need and demand of psychiatric support were included in the follow-up and treatment process. Twenty-one out of 165 people who participated in the study were not included due to different reasons (discontinuation of the study, random marking of scales); eventually the research was completed with 144 people. Informed consent was obtained from the participants for the study. This study was conducted by S.B.Ü. Ankara Dışkapı Yıldırım Beyazıt Training and Research Hospital Ethics Committee. It was carried out in accordance with the ethical standards set out in the 2013 Helsinki Declaration.
Patients with psychotic disorder, bipolar disorder, major depression, dementia, and organic mental disorder and patients with mental retardation and illiterate caregivers were excluded from the study. Zarit Burden Interview (ZBI) and Expressed Emotion Scale (EES) were applied to the caregivers who participated in the study. Disease severity of children with cerebral palsy was evaluated by the Gross Motor Function Classification System (GMFCS) and Manual Ability Classification System (MACS) in Children with Cerebral Palsy. Communication Function Classification System (CFCS) was used to examine the communication of children with their families. The data of the caregivers will be examined and evaluated together with the disease severity of children with cerebral palsy.
Data collection tools
Zarit Burden Interview
It was developed by Zarit et al. [15] in order to reveal caregiving burden, while the Turkish validity study was conducted by Özlü et al. [8]. It is a Likert-type scale, consisting of 22 questions featuring “never”, “rarely”, “sometimes”, “often”, or “almost always” and has ratings ranging from “1” to “5”. The total score ranges between 22 and 110 points. Although there is no data on the cut-off point of the scale, the scores obtained are considered as mild between 22 and 46, moderate between 47 and 55 and severe load of burden over 56 and above. The items taking part in the scale are generally social and emotional oriented, and the higher the scale score, the higher the caregiving burden.
Emotion Expression Scale
It was developed by Cole and Kazarian (1988). The validity and reliability study was conducted by Berksun (1992), and the scale was given to relatives of schizophrenia patients [16]. The scale consists of 41 questions and has the subscales of criticism/hostility (EES criticism) and excessive interest/protection-interventionism (EES excessive interest). High scores indicate high emotional expression. The total score reliability coefficient of the scale was 0.93.
Gross Motor Function Classification System
It is a standard classification system developed by Palisano [17]. GMFCS objectively divides the child’s existing gross motor functions into levels. It evaluates basic functions such as sitting and walking by focusing on movements that the child can initiate on his/her own. It consists of five levels; level 1 represents children who are more independent in terms of motor function, while level 5 represents the most dependent children. The child’s assistive technology supports and wheelchair requirements are taken into account. It does not include the motor function quality of the child and does not indicate the potential for progress. [18].
The Manual Ability Classification System for Children with Cerebral Palsy
A questionnaire developed to evaluate how children use their hands in object-handling activities in daily life activities to reflect the manual performance of children with CP between the ages of 4 and 18 [19]. It evaluates the common use of both hands; it does not evaluate hand functions separately. Levels are determined by children’s ability to hold the object, whether it needs support or adaptation. It consists of 5 levels. A Turkish validity and reliability study was conducted [20].
Communication Functions Classification System
CFCS classifies the daily communication performance of individuals with cerebral palsy between 1 and 5 levels. CFCS focuses on the levels of activity and participation as mentioned in the international classification of function, disability, and health defined by the World Health Organization [21].
If the communication performance fits more than one level, the level that describes the overall performance of this child the best is chosen. The distinctions between levels are based on the performance of the sender and receiver roles, the communication course, and the communication type of partner [22].
Statistical procedures
SPSS 22.0 for Windows Evaluation Version (statistical package for the social sciences) was used to evaluate data with the statistical package program. Sociodemographic data of patients and caregivers with nominal characteristics are shown as a percentage. Numerical variables are shown with mean and standard deviation, while categorical variables are represented by numbers and percentages. The homogeneity of the variances of the compared groups was evaluated with the Levene test. Since parametric assumptions were met for the relation between numerical variables, the Pearson correlation was used. Multiple regression analysis was used to investigate the connections between scales. A p value of < 0.05 was considered statistically significant.
Results
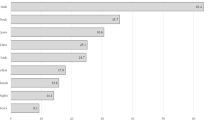
The distribution of some sociodemographic and clinical characteristics of the participants is given in Table 1. Accordingly, 78.5% (n = 113) of the participants were women, and the mean age was 33 ± 8 years. 90.3% (n = 130) of the parents are married, 31.3% (n = 45) of them work, and half of them have at least 2 children. The mean ZBI of the caregivers was 49.77 (SD ± 10.20), the total scores of the EES were 14.71 (SD ± 3.64), the EES criticism points were 10.51 (SD ± 3.19), and the EES extreme interest scores were 4.20 (SD ± 1.10).
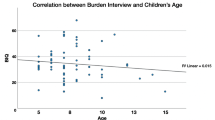
Table 2 shows the distribution of some sociodemographic and clinical characteristics of patients with cerebral palsy. Accordingly, 59.7% (n = 86) of the patients were male, with a mean age of 7 ± 4 years and delivery of half of the patients is over 36 weeks. 70.1% (n = 101) of the patients were diagnosed with CP at birth and 72.9% (n = 97) required intensive care.
Correlation of ZBI, EES, and subdimensions of GMFCS, MACS, and CFCS scores of patients with cerebral palsy is given in Table 3. Accordingly, a positive, statistically significant, moderate correlation was found between the GMFCS, MACS, and CFCS scores and ZBI scores in patients with cerebral palsy (r ~ 0.50; p < 0.01). In this study, a positive, statistically significant but weak correlation was found between GMFCS, MACS, and CFCS scores and EES scores in patients with cerebral palsy (r ~ 0.30; p < 0.01). In the study, a positive, statistically significant but weak (GMFCS) and negligible (MACS, CFCS) correlation was found between the GMFCS, MACS, and CFCS scores and the EES criticism scores in patients with cerebral palsy (p < 0.05). In the study, a positive, statistically significant, weak (GMFCS) and moderate (MACS, CFCS) correlation was found between the GMFCS, MACS, and CFCS scores and the EES excessive interest scores in patients with cerebral palsy (r > 0.39; p < 0, 05). A statistically significant, moderate correlation was found between ZBI and EES (r ~ 0.50; p < 0.01).
Table 4 shows the relationship between GMFCS, MACS, and CFCS scores in patients with cerebral palsy. Accordingly, no statistically significant relationship was found between GMFCS, MACS, and CFCS scores and ZBI scores in the multivariate model (p > 0.05).
The relationship between GMFCS, MACS, and CFCS scores in the patients with cerebral palsy is given in Table 5. Accordingly, no statistically significant relationship was found between GMFCS, MACS, and CFCS scores and EES scores in the multivariate model (p > 0.05).
Discussion
In children with cerebral palsy, usually accompanied by posture and movement disorders, problems such as developmental disabilities, malnutrition such as chewing-swallowing problems, intellectual disability, mental problems (depression, anxiety, etc.), behavioral disorders (attention deficit, hyperactivity, aggression, etc.), communication difficulties, hearing and vision problems, epilepsy, sleep disorders, lung infections, pain and sphincter control disorders may occur [23].
In our study, 40.3% of children with CP were girls, and 59.7% were boys. Many studies in the literature show that the number of boys is high [24]. In our study, the number of boys was high in accordance with many studies in the literature.
78.5% of the caregivers of our patients were women. In a study by Raina et al. [25] on 486 children with CP, 94.4% of caregivers were women, and 89.7% of caregivers were mothers of children. It is known that mothers in our community play a much higher role in the care of disabled children than fathers [10].
Emotional expression (EE) was initially evaluated in families of individuals diagnosed with schizophrenia; EE has proved to be a reliable and robust predictor of symptom relapse [26]. More recently, it has been applied to a number of other diseases, including depression, bipolar disorder, and eating disorders [14]. Recently, an increasing number of studies have identified families’ EE as important factors affecting family relationships and dysfunction [27], and close relationships have been established between EE and family functioning and distress. Raune et al. have suggested that, for family parental caregivers, not the disease factors of the patients but their psychological evaluation is effective in determining high EE and high subjective burden [27]. In our study, a statistically significant, moderate correlation was found between ZBI and EES. In addition, it was observed that EE criticism subscale had higher correlation with GMFCS and EE excessive interest subscale had higher correlation with CFCS compared with other evaluations. Again, the correlation between EE criticism and ZBI scale was more significant than the correlation between EE excessive interest and ZBI. It can be said that developmental retardation in gross motor skills has a higher relationship with EE criticism and family burden. Developmental delay in communication is more closely related to the family’s EE excessive interest/interventionism.
Children with CP are in constant need of special attention and care because of inadequacies or problems caused by the disease. These special needs of the child with CP often overburden the parents. While this burden creates physical and psychological effects on parents, it may negatively affect their social, cultural, and professional lives and may decrease the quality of life [28]. In our study, when the average Zarit scores of the caregivers were examined, it was found to be in moderate load range. Studies have also shown that the presence of a disabled child increases the family burden [29].
In our study, there was a positive and moderate correlation between GMFCS, MACS, and CFCS scores and ZBI scores in patients with cerebral palsy; On the other hand, there was a statistically significant but weak correlation between the EES scores of the participants. One of the most important factors that increase caregiving is the deterioration in the patient’s physical abilities. In particular, physical and psychological complications of the disease and intensive treatment regimens are long sources of stress for patients and caring family members [30, 31].
However, there are some different studies on caregivers. In some studies, no correlation was found between GMFCS level of children with CP and depression and quality of life of mothers [32]; otherwise in some other studies, it has been shown that GMFCS levels of children are correlated with depression, anxiety [33], and mothers’ quality of life [34].
Multiple regression analysis was performed in order to understand the relationship between GMFCS, MACS, and CFCS scores in patients with cerebral palsy. Along with the correlation results, it is possible to mention the existence of a relationship between scales. However, it is not possible to interpret ZBI and EES scores directly on the developmental processes of children with cerebral palsy. Both family burden and the fact that emotional expression processes are multidimensional variables could have caused this situation.
Among the limitations of our study, gender differences between children and caregivers with CP, family burden, and emotional expression scales are self-report scale, as in all self-report scales can be counted in the sense that cognitive avoidance processes can be effective. At the same time, as we mentioned earlier, it is not easy to interpret the ZBI and EES scores directly in the developmental processes of children with cerebral palsy. It is also difficult to control all other factors related to the child’s health (such as complications, treatment, and follow-up processes), caregiver health and socioeconomic status. There is also a need for studies with more participants from more different age groups.
Conclusion
As far as we know, this study is the first to evaluate the care burden and emotional expression in families, focusing directly on CP. According to our findings, it can be said that evaluation together with family and caregiver is important in the evaluation of children with CP. According to the results of our study, as motor skills and communication skills decrease, especially the burden of caregivers increases and the family’s emotional expression processes are related to these variables. In the long-term follow-up of children with CP, we think that it may be useful to evaluate the caregivers from these aspects and to provide the necessary psychiatric support.
References
Organization WH. World report on disability 2011: World Health Organization; 2011
Richards CL, Malouin F (2013) Cerebral palsy: definition, assessment and rehabilitation. Handb Clin Neurol 111:183–195
Serdaroǧlu A, Cansu A, Özkan S, Tezcan S (2006) Prevalence of cerebral palsy in Turkish children between the ages of 2 and 16 years. Dev Med Child Neurol 48(6):413–416
Ström H, Kreuter M, Rosberg S (2011) Quality of life in parents/caretakers of children with cerebral palsy in Kampong Cham, Cambodia. J Trop Pediatr 58(4):303–306
Khanna AK, Prabhakaran A, Patel P, Ganjiwale JD, Nimbalkar SM (2015) Social, psychological and financial burden on caregivers of children with chronic illness: a cross-sectional study. Indian J Pediatr 82(11):1006–1011
Zarit SH (2004) Family care and burden at the end of life. Cmaj 170(12):1811–1812
Atagün Mİ, Balaban ÖD, Atagün Z, Elagöz M, Özpolat AY (2011) Kronik hastalıklarda bakım veren yükü. Psikiyatride Güncel Yaklaşımlar 3(3):513–552
Ozlu A, Yildiz M, Aker T. (2009).Zarit Bakıcı Yük Ölçeğinin Şizofreni Hasta Yakınlarında Geçerlilik ve Güvenilirlik Çalışması. Archives of Neuropsychiatry/Noropsikiatri Arsivi;46
Kasuya RT, Polgar-Bailey MP, MPH Robbyn Takeuchi M. (2000) Caregiver burden and burnout a guide for primary care physicians. Postgraduate Med 108(7):119
Sarı HY. (2007).Zihinsel engelli çocuğu olan ailelerde aile yüklenmesi
Dokmen ZY. (2017).Yakınlarına bakım verenlerin ruh sağlıkları ile sosyal destek algıları arasındaki ilişkiler. Ankara Üniversitesi Sosyal Bilimler Dergisi;3(1)
Dattilio FM, Epstein NB (2015) Cognitive-behavioral couple and family therapy. Handbook of family therapy, Routledge, pp 103–133
Barrowclough C, Parle M (1997) Appraisal, psychological adjustment and expressed emotion in relatives of patients suffering from schizophrenia. Br J Psychiatry 171(1):26–30
Butzlaff RL, Hooley JM (1998) Expressed emotion and psychiatric relapse: a meta-analysis. Arch Gen Psychiatry 55(6):547–552
Zarit SH, Reever KE, Bach-Peterson J (1980) Relatives of the impaired elderly: correlates of feelings of burden. The Gerontologist 20(6):649–655
Cole JD, Kazarian SS (1988) The level of Expressed Emotion Scale: a new measure of expressed emotion. J Clin Psychol 44(3):392–397
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B (1997) Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 39(4):214–223
Wood E, Rosenbaum P (2000) The Gross Motor Function Classification System for cerebral palsy: a study of reliability and stability over time. Dev Med Child Neurol 42(5):292–296
Eliasson A-C, Krumlinde-Sundholm L, Rösblad B, Beckung E, Arner M, Ohrvall AM, Rosenbaum P (2006) The Manual Ability Classification System (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol 48(7):549–554
Akpinar P, Tezel CG, Eliasson A-C, Icagasioglu A (2010) Reliability and cross-cultural validation of the Turkish version of Manual Ability Classification System (MACS) for children with cerebral palsy. Disabil Rehabil 32(23):1910–1916
Hidecker MJC, Paneth N, Rosenbaum PL, Kent RD, Lillie J, Eulenberg JB, Chester K Jr, Johnson B, Michalsen L, Evatt M, Taylor K (2011) Developing and validating the communication function classification system for individuals with cerebral palsy. Dev Med Child Neurol 53(8):704–710
Mutlu A, Kaya-Kara O, Kerem-Gunel M, Livanelioglu A, Karahan S, Hidecker M (2013) Agreement between parents and clinicians for the communication function classification system (cfcs) of children with cerebral palsy: sp53. Dev Med Child Neurol 55:76
Sewell MD, Eastwood DM, Wimalasundera N (2014) Managing common symptoms of cerebral palsy in children. bmj 349:g5474
Yuan J, Wang J, Jieqiong M, Zhu D, Zhang Z, Jianan L (2019) Paediatric cerebral palsy prevalence and high-risk factors in Henan Province, Central China. J Rehabil Med 51(1):47–53
Raina P, O’Donnell M, Rosenbaum P et al (2005) The health and well-being of caregivers of children with cerebral palsy. Pediatrics 115(6):e626–ee36
Leff J, Vaughn C (1984) Expressed emotion in families: its significance for mental illness. Guilford press
Raune D, Kuipers E, Bebbington P (2004) Expressed emotion at first-episode psychosis: investigating a carer appraisal model. Br J Psychiatry 184(4):321–326
Guillamón N, Nieto R, Pousada M, Redolar D, Muñoz E, Hernández E, Boixadós M, Gómez-Zúñiga B (2013) Quality of life and mental health among parents of children with cerebral palsy: the influence of self-efficacy and coping strategies. J Clin Nurs 22(11–12):1579–1590
Hodge D, Hoffman CD, Sweeney DP (2011) Increased psychopathology in parents of children with autism: genetic liability or burden of caregiving? J Dev Phys Disabil 23(3):227–239
Can T. (2010).Bakas Caregiving Outcomes Scale'in (Bakas Bakım Verme Etki Ölçeği) Türkçe'ye uyarlanması, geçerlilik ve güvenirliliği
Stetz KM, Brown MA (1997) Taking care: caregiving to persons with cancer and AIDS. Cancer Nurs 20(1):12–22
Ones K, Yilmaz E, Cetinkaya B, Caglar N (2005) Assessment of the quality of life of mothers of children with cerebral palsy (primary caregivers). Neurorehabil Neural Repair 19(3):232–237
Yilmaz H, Erkin G, Nalbant L (2013) Depression and anxiety levels in mothers of children with cerebral palsy: a controlled study. Eur J Phys Rehabil Med 49(6):823–827
Eker L, Tüzün EH (2004) An evaluation of quality of life of mothers of children with cerebral palsy. Disabil Rehabil 26(23):1354–1359
Acknowledgements
The authors thank all the study participants and clinical staff who helped with this article.
Author information
Authors and Affiliations
Contributions
FY, ZAY, and EUA took part in the study design, conduct of the study, literature review and preparation of the article and conduct of the study. All authors have seen and approved the final draft. FY will act as guarantor for this post.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yığman, F., Aykın Yığman, Z. & Ünlü Akyüz, E. Investigation of the relationship between disease severity, caregiver burden and emotional expression in caregivers of children with cerebral palsy. Ir J Med Sci 189, 1413–1419 (2020). https://doi.org/10.1007/s11845-020-02214-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-020-02214-6