Abstract
Background
There have been many changes in number and place of trocars that have been described, since the first laparoscopic cholecystectomy (LC), but, in fact, all authors agree that laparoscopic procedure is accepted as gold standard. However, four trocars use in standard laparoscopic cholecystectomy, it has been argued that the fourth port is not necessary for grasping fundus of gallbladder so as to expose Calot’s triangle. The aim of this study is to establish the safety of three-trocar LC in symptomatic gallbladder disease and also to determine the ratio of technical requirements of the fourth trocar.
Methods
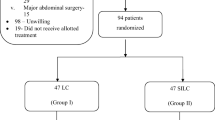
Between August 2010 and January 2016, 291 cases were operated in Kocaeli Derince Education and Research Hospital, department of general surgery for symptomatic gallbladder disease with three-port LC, and their records were examined retrospectively.
Results
Two hundred and twenty patients were female (75.6 %) and seventy one (24.4 %) were male. Two hundred and eighteen of two hundred and ninety-one cases (74.92 %) were operated with three- port LC in a secure way. In seventy-three cases (25.08 %), one more port was needed to use. Mean operative time was 33.76 ± 11:18 min. (15–90 min). In these cases, major complications, such as main bile duct injury or bile leakage, that may increase the mortality and morbidity, did not occur. Only in one case (0.34 %) postoperative bleeding was seen from the liver bed, which was required exploration.
Conclusion
We concluded that in experienced hand, LC with three ports is safe and feasible technique if it is not endanger the course of the surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The first cholecystectomy was performed in 1882 by Carl Langenbuch [1]. Until 1987, open cholecystectomy for symptomatic gall bladder disease has been performed for Phillipe Mouret who performed first LC (LC) later established by Dubois and Perissat in 1990. It has met with wide-spread acceptance as a gold standard procedure all over the world [2, 3]. The laparoscopic approach has almost become synonymous with LC. The traditional LC is usually performed using four ports [4]. With increasing surgeon experience, it has been argued that the fourth trocar for hanging fundus of the gallbladder so as to expose Calot’s triangle may not be necessary and LC can be performed safely with three ports [5–8].
The aim of this study is to determine the reliability of three-port LC and to determine the rate of fourth trocar need.
Materials and methods
The medical records of 291 cases who had undergone three-port LC for symptomatic gallbladder disease in the Department of Surgery of Kocaeli Derince Education and Research Hospital, Turkey, between August 2010 and January 2016, were included in this study. The reason and rate of four-port requirement, operating time, complication rates, average length of hospital stay, and return to work have been viewed from the records of patients. For this purpose, cases of one surgeon who had an experience in LC over 500 cases and assistant surgeon cases performed under the supervision of the same surgeon were examined retrospectively.
Operative technique
All the patients were operated under general anesthesia. After preparation of patient with betadine scrub and dressing the operation field, a Veress’ needle inserted into the abdomen with closed technique to create pneumoperitoneum with approximately 3–4 L of CO2 gas. After than a 10 mm trocar inserted from the same incision at the umbilicus, through which the 30° viewing videoscope was introduced. Another 10 mm trocar was inserted 3 cm below the xyphoid, and then, a 5 mm trocar was inserted in the right hypochondrium on anterior axillary line ~2–3 cm below the costal margin. Patients were placed supine in reverse Trendelenburg position and 30° to left. The operating surgeon and assistant (videoscope holder) stood on the left of the patient with the nurse on the right. A TV monitor was placed to the right of the patient’s head, across the surgeon. The surgeon operated via two ports, while the assistant manipulated the camera. A grasper was inserted via the 5 mm port to dissect the inferior and posterior aspects of the cystic duct, a grasper was inserted via the midclavicular port to grip the infundibulum and retracted downward to expose Calot’s triangle, and the anterior and superior portions of cystic duct were dissected. First cystic duct and then cystic artery were clipped and divided. The grasper was used to hold the gallbladder in various positions, so that it could be dissected from the liver bed. The gallbladder was put into an endobag and then extracted through the epigastric port. A drain was inserted from 5 mm port through foramen Winslow in all cases and postoperative first day taken off, and in cases where a large, soft liver overhangs Calot’s triangle or the operative field is obscure due to hypertrophy of segment IV of liver a fourth trocar (5 mm) from the middle point of right hypochondrium to epigastric trocar may be added to insert a retractor. No suspending suture was used in any of our cases. Preoperative prophylactic antibiotic (i.v) was given to all patients.
Results
The demographic data (age, sex, weight) for the two groups were written in Table 1. Two hundred and ninety-one cases were included in this study. Two hundred and twenty of 291 were female (75.6 %), while 71 of all cases were male (24.4 %) (Table 1). Two hundred and eighteen of 291 cases were operated with three-trocar safely (74.92 %). Fourth trocar was needed in 73 (25.08 %) of all cases. Forty-eight of two hundred and seventeen of cases who were operated by a single surgeon (22.12 %), and 25 of 74 (33.78 %) cases who were operated by an assistant surgeon under the supervision of same surgeon fourth port need occurred. In twenty-eight cases (9.62 %), anatomical variations and difficulties, such as buried gallbladder or anatomical variations, which prevents discovery of the triangle of calotte, were observed. However, in 45 cases (15.46 %), fourth trocar was needed, because of Mirizzi’s syndrome, thickening of gallbladder wall that caused insufficient traction of gallbladder, or Hartmann pouch adhesions that caused dissection difficulty. All the cases were finish laparoscopic and there was no conversion to open cholecystectomy. Major complications, such as bile duct injury and bile leakage that cause mortality and morbidity, were not occurred (Table 2). Intraoperatively, bleeding from the liver bed was seen in 17 (7.8 %) of all cases. In these cases, hemostasis was achieved by monopolar cautery. Mean operative time was 33.76 ± 11:18 min (15–90 min) (Table 3). In the postoperative period, port-site hematoma in two cases (0.92 %), and intraabdominal hemorrhage in three patients (1.37 %). were observed. Postoperative exploration was needed only one of three cases (0.34 %) (Table 4). The average hospitalization period and time to return to work were 1.10 day (1–3 days) and 7.2 days (7–10 days), respectively.
Discussion
The first LC was performed in 1987 by Phillipe Mouret. In 1990, the development of the method by Dubois and Perissat, LC has revolutionized the surgical treatment of symptomatic gallbladder disease [1–3]. Traditionally, LC is performed using the four-port technique all over the world [4]. However, the gained experience and development of laparoscopic tools have prompted the surgeons to modify the technique, for instance, reducing number or placing site of trocars, to improve postoperative outcomes and cosmetic results. For this purpose, some surgeons used suture for retracting the gall bladder by that way they reduced the port number; on the other hand, some surgeons argued that LC can be done safety with three ports [5–8]. The surgeons who believe in every surgical incision cause trauma for patient, so that they tried to reduce port number first to second, then to three ports from single incision over time [9, 10]. Several studies have reported that postoperative pain increased in direct proportion to the ports numbers and length of the incision [11–13]. Although there are published reports about the port number and different incision methods, four-port LC is still widely used all over the world. However, three-port LC well accepted and continues to be done in various centers [4–6]. In our clinic, some surgeons prefer to do four-port LC, while some of us prefer to do three-port LC.
The publications related to three-port LC emphasize that this technique can be applied by experienced surgeons [4–6]. In our study, 217 of 291 cases were operated by single surgeon who has an experienced more than 500 cases of LC, 74 of them were operated by assistant surgeons under the supervision of the same surgeon. The fourth port was needed in 48 of 217 (22.12 %), 25 of 74 (33.78 %), and total of 73 (33.78 %) cases. The difference between the rates of fourth port that need show us with the increasing experience three-port LC can be done safety as noted in literature. The most common intraoperative complication of three-port cholecystectomy is gallbladder perforation. Gallbladder perforation rate reported in the literature for standard four ports is 16 and 33 % in three-port LC [14]. In our series, this rate is 11.93 % and consistent with the literature. The most serious complication of LC may lead to morbidity and mortality is the main bile duct injury [15]. The consensus of surgeons who reject to used three ports; the third port which was placed from right hypocondirum cannot provide adequate traction of gallbladder so exposing and dissection could not be done safety, so that it caused a major risk for surgeon [16]. However, 218 of our 291 cases were finished with three ports. In seventy-three cases, fourth port is needed to ensure the safety of surgery. We have no main bile duct injury either in three- or four-port LC.
Bleeding complications of LC can be occurred from aorta, vena cava, portal vein, cystic artery, port site, and liver bed bleeding [17]. In our study, 17 (7.8 %) patients had bleeding from the liver bed in the intraoperative period. Hemostasis was achieved with monopolar cautery in all cases. We did not use vascular clips in any of cases for no vascular injuries were seen in our cases. Port-site hematoma and intraabdominal hemorrhage were seen in second (0.92 %) and third (1.37 %) cases, respectively, in postoperative period. Postoperative exploration was need only in one (0.34 %) of the three intraabdominal hemorrhage cases. The bleeding as a leakage from the liver bed was control by cauterization. Port-site hematomas were locally hemostasis after sutures were taken off.
In studies comparing three-port and four-port LC is emphasized that the average operating time, length of hospitalization, and return to normal activities are all similar [4, 6, 8, 18]. Our results were consistent with the literature (Table 2).
As a result, we believe that three-port LC is a safe and favorable technique and can be performed by experienced surgeons if it is not jeopardize the progress of the surgery for it is more economical than four-port.
References
Hardy KJ (1993) Carl Langenbuch and the Lazarus Hospital: events and circumstances surrounding the first cholecystectomy. Aust N Z J Surg 63:56–64. doi:10.1111/j.1445-2197.1993.tb00035.x
Dubois F, Icard P, Berthelot G et al (1990) Coelioscopic cholecystectomy: premilary report of 36 cases. Ann Surg 211:60–62. doi:10.1097/00000658-199001000-00010
Mouret P (1996) How i developed laparoscopic cholecystectomy. Ann Acad Med Singap 25:744–747
Trichak S (2003) Three-port vs standard four-port laparoscopic cholecystectomy. Surg Endosc 17:1434–1436. doi:10.1007/s00464-002-8713-1
Chalkoo M, Ahangar S, Durrani AM (2010) Is fourth port really required in laparoscopic cholecystectomy? Indian J Surg 72:373–376. doi:10.1007/s12262-010-0154-9
Al-Azawi D, Houssein N, Rayis AB et al (2007) Three-port versus four-port laparoscopic cholecystectomy in acute and chronic cholecystitis. BMC Surg. doi:10.1186/1471-2482-7-8
Kumar M, Agrawal CS, Gupta RK (2007) Three-port versus standard four-port laparoscopic cholecystectomy: a randomized controlled clinical trial in a community-based teaching hospital in eastern Nepal. JSLS 11:358–362
Sun S, Yang K, Gao M et al (2009) Three-port versus four-port laparoscopic cholecystectomy: meta-analysis of randomized clinical trials. World J Surg 33:1904–1908. doi:10.1007/s00268-009-0108-1
Sulu B, Diken T, Altun H et al (2014) A comparison of single-port laparoscopic cholecystectomy and an alternative technique without a suspension suture. Ulus Cer Derg 30:192–196. doi:10.5152/UCD.2014.2717
Justo-Janeiro J, Vincent GT, Lara FV et al (2014) One, two, or three ports in laparoscopic cholecystectomy? Int Surg 99:739–744. doi:10.9738/INTSURG-D-13-00234.1
Harsha HS, Gunjiganvi M, Singh C et al (2013) A study of three-port versus four-port laparoscopic cholecystectomy. J Med Soc 27:208–211. doi:10.4103/0972-4958.127395
Sakran N, Goitein D, Raziel A et al (2014) Advantages of minimal incision laparoscopic cholecystectomy. IMAJ 16:363–366
Gurusamy KS, Vaughan J, Rossi M et al (2014) Fewer-than-four ports versus four ports for laparoscopic cholecystectomy. Cochrane Database of Syst Rev. doi:10.1002/14651858.CD007109.pub2 (Art. No.: CD007109)
Gurusamy KS, Samraj K, Ramamoorthy R et al (2010) Miniport versus standard ports for laparoscopic cholecystectomy. Cochrane Database Syst Rev. doi:10.1002/14651858.CD006804.pub3
Frilling A, Li J, Weber F et al (2004) Major bile duct injuries after laparoscopic cholecystectomy: a tertiary center experience. J Gastrointest Surg 8:679–685. doi:10.1016/j.gassur.2004.04.005
Haribhakti SP, Mistry JH (2015) Techniques of laparoscopic cholecystectomy: nomenclature and selection. J Min Access Surg 11:113–118. doi:10.4103/0972-9941.140220
Kaushik R (2010) Bleeding complications in laparoscopic cholecystectomy: incidence, mechanisms, prevention and management. J Minim Access Surg 6:59–65. doi:10.4103/0972-9941.68579
Cerci C, Tarhan OR, Barut I et al (2007) Three-port versus four-port laparoscopic cholecystectomy. Hepatogastroenterology 54:15–16
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest. This study was designed as retrospective research, so that informed consent was obtained from all individual participants included in the study, but we have no ethical approval for this article. However, this article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Ciftci, A., Yazicioglu, M.B., Tiryaki, C. et al. Is the fourth port routinely required for laparoscopic cholecystectomy? Our three-port laparoscopic cholecystectomy experience. Ir J Med Sci 185, 909–912 (2016). https://doi.org/10.1007/s11845-016-1493-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-016-1493-8