Abstract
Background
Application to the Irish basic surgical training (BST) program in Ireland has decreased progressively over the past 5 years. We hypothesised that this decline was secondary to dissatisfaction with training correlated with reduced operative experience and lack of mentorship among BSTs.
Methods
An anonymous 15 question electronic survey was circulated to all BSTs appraising their impression of the operative experience available to them, their mentorship and their opinions of critical aspects of training.
Results
Fifty trainees responded to the survey. At the commencement of training 98 % (n = 43) intended to stay in surgery, decreasing to 79 % (n = 34) during the BST. Trainees who felt they had a mentor were three times more likely to be content in surgical training (OR 3.11; 95 % CI 0.94–10.25, P = 0.06). Trainees satisfied with their allocated rotation were more likely to be content in surgical training (OR 4.5; 95 % CI 1.03–19.6, P = 0.045). Individual trainee comments revealed dissatisfaction with operative exposure.
Conclusion
Mentorship and satisfaction with allocated training rotation had a positive impact on trainee satisfaction and correlated with contentedness in surgical training. Operative experience is the main element that trainees report as lacking. This highlights the need for reform of the training system to improve current levels of mentorship and increase operative exposure to enhance its attractiveness to the best quality medical graduates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
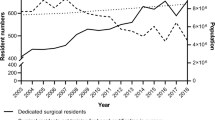
The intake of the irish basic surgical training (BST) program has declined progressively over the past 5 years, dropping by over 50 % in the past 5 years from 263 to 129 [1]. Surgical training committees perceive a decline in the quality of applicant [2]. Hitherto, the reasons forwarded for this decline include the duration of training and the lack of work-life balance thus increasing the attractiveness of ‘lifestyle specialties’ such as radiology, anaesthesia and general practice [3]. Increasingly, however, trainees are voicing concern that reduced operative exposure is having a detrimental effect on their training momentum and a demoralising effect on their career aspirations.
We hypothesised that dissatisfaction with training correlated with reduced operative experience and lack of mentorship among basic surgical trainees. The aim of this study was to evaluate the level of operative experience, mentorship and satisfaction of trainees on the basic surgical training scheme in Ireland in order to investigate the decreasing number of applicants. This data may enable us to improve basic surgical training and thus improve the attractiveness of surgery as a career for medical graduates.
Methods
Survey methods
A 15 question survey was created using Survey Monkey. This is an online tool that facilitates both survey circulation and collection of responses (http://www.surveymonkey.com). An anonymous link to the survey was circulated via email to all 170 Irish basic surgical trainees. Questions included those with binary responses and those with responses on a 5-point Likert scale, a scale from which respondents choose one option that best aligns with their view. A number of the most commonly performed training procedures were selected. The number performed by each trainee as primary operator quantified on a ranked scale.
Satisfaction with the program
Career plans prior to and during basic surgical training were assessed i.e., surgery versus another discipline. We also gave applicants the option to offer their own opinions on training.
Statistical analysis
Standard frequency analysis was used to describe the survey results. Summed operative scores were compared with the Mann–Whitney U test using contentedness as the grouping variable. Logistic regression analysis was used to identify correlations between responses and various outcomes such as whether or not trainees were content in surgical training. Data was stored using Microsoft excel version 12.3.1 (Microsoft Corporation) and analysed using Minitab version 15 (Minitab Inc.).
Results
Fifty (29.4 %) trainees responded to our survey. Three trainees entered the survey link, were registered as respondents but did not complete the survey. These were excluded from analysis. A number of trainees omitted responses to certain questions therefore not all percentages given refer to the entire quota of 50 respondents.
Satisfaction with the training scheme
Sixty-six percent (n = 33) of trainees were either dissatisfied with or indifferent to their allocated training scheme (Table 1). Of the allocated posts in 1 and 2 year, 80.2 % (n = 69) and 32.0 % (n = 16) were in general surgery in 1 and 2 year respectively. The remainder of attachments were distributed between neurosurgery, ENT, orthopaedics, paediatric surgery, cardiothoracic surgery, emergency medicine, urology and plastic surgery (Table 2).
Fifty-one percent (n = 24) of trainees are not content in surgical training (Table 3). Satisfaction with the allocated attachments correlated significantly with being content in surgical training (OR 4.5; 95 % CI 1.03–19.6, P = 0.045). There was a significant correlation between trainee dissatisfaction with allocated training scheme and those not wanting to train in Ireland again (OR 8.46; 95 % CI 1.6–44.76, P = 0.012). The majority of trainees felt that they had only received moderate support in the areas of operative surgery, clinical skills, research, exams and courses and all trainees felt that operative exposure should be increased (Tables 4, 5).
Procedures performed
The majority of trainees stated they had never performed a cholecystectomy or colonoscopy. A significant proportion (42 %, n = 19) had never performed an OGD, 42 % (n = 20) had never performed an appedicectomy (Table 6). This indicates that a significant proportion of trainees fall short of the arbitrary training targets set by the RCSI where, for example appendicectomies and five cholecystectomies are set as the minimum requirements. There was no significant correlation between operative experience and contentedness in surgical training (P = 0.1938).
Mentorship
Fifty-one percent (n = 23) of trainees report that they did not feel that they had a mentor in surgery. Trainees who felt they had a mentor were more likely to be content in surgical training (OR 3.11; 95 % CI 0.94–10.25, P = 0.06).
Career path
Ninety-eight percent (n = 46) of trainees commenced surgical training with the intention of pursuing a career in surgery (Table 3). After finishing the BST, 79 % (n = 37) intend to continue in surgery but 21 % plan to leave the training program and move to general practice, emergency medicine, radiology or have uncertain plans (Table 7). When asked to specify the reason for their career choice, the group who wished to remain in surgery (n = 37) highlighted professional interest, enthusiasm for the discipline and personal talent/flare. Those planning a change of specialty cited lifestyle, satisfaction and length of training and enthusiasm for the discipline they subsequently selected as the main reasons for their decision (Table 8).
Discussion
Over the past 5 years there has been a 51 % reduction in applicants to the BST programme and a decline in the quality of applicant [1, 2]. Whilst arguably this provides greater opportunities for higher surgical trainees to obtain experience, there is a potentially negative impact as responsibility to close the gaps in service provision will fall to them. This study casts new light on the reasons for this decline. A significant number of trainees are dissatisfied with their operative experience, dissatisfied with their allocated rotation, and feel that they lack a surgical mentor. Over 20 % expressed their intention to leave the program. This dissatisfaction mirrors the decline in applications to, and attrition from, the BST program to other disciplines. It is possible that this dissatisfaction is being communicated to more junior doctors, dissuading them from applying to the program.
Analysis of BST logbooks reveals that the majority of trainees fail to meet the modest targets for operative exposure reflecting a decline in hands-on operative experience [4]. Surgical training is complex, multifaceted and comprises largely of “hand work” [5]. It has been suggested that 20,000 h of training are required to produce a competent surgeon [6, 7]. Modern trainees face a number of challenges reducing hours of exposure and restricting training opportunities making this an unrealistic goal, unless operative exposure begins and intensifies through the BST years. The European working time directive (EWTD), introduced to enhance patient safety and protect trainees from overwork, paradoxically poses a long-term threat by reducing operative experience [8, 9]. In the UK the percentage of trainees capable of performing an appendicectomy at the end of BST has fallen from 90 to 28 %, illustrating a significant decline in surgical competence [10]. Duty hour restrictions (DHR) in the United States have reduced the number of procedures in which the trainee is competent, and residents have expressed concerns about their readiness to practice independently at the end of training [11, 12]. Concern regarding the outcome of procedures performed by trainees, often cited as a reason for restricting BST operative opportunity, has been proven to be unfounded [13–15]. The increased time required by basic surgical trainees adds to theatre costs but this is easily outweighed by the long-term benefit of a properly trained surgical workforce [14, 15].
The national treatment purchase fund (NTPF), introduced to transfer patients waiting for more than 3 months from teaching hospitals to a private facility to expedite their treatment, has removed a total of 170,000 procedures from teaching hospitals to date [4]. The bulk of these were procedures were ones in which trainees traditionally honed their skills such as skin lesions, varicose vein surgery, cholecystectomy and hernia repair [16, 17]. Concomitantly a large number of procedures have been postponed due to bed closures and budgetary constraints. While the NTPF has ceased, it is likely that bed and hospital closures will worsen over the next 10 years [18].
Fixing the current decline will require bold and comprehensive change in the organisation of training and the delivery of surgical service. Realistic operative targets should be defined to ensure adequate BST experience, which should be speciality-specific. Six-month rotations are necessary to allow trainer–trainee trust to develop. Surgeons with complex workloads can involve trainees in individual components of complex procedures, each of which should be a recognisable logbook entry. As operative experience is ultimately decided and delivered at hospital level, we suggest that a BST co-ordinator be allocated to every hospital in which trainees are located. Monitoring of operative exposure by the RCSI, through the electronic logbooks, would allow those units that fail to reach targets to be identified and to work with the training body to achieve these goals.
Our study has limitations, our population size is low and whilst a response rate of 30 % is average for online studies, it does bring a risk of reduced overall study accuracy.
Our results do confirm that mentoring has an important role within surgical training [19, 20]. In Ireland mentoring relationships are established individually, if at all, and less than half (48.9 %) of trainees currently report having a mentor. This represents a lost opportunity for most trainees, as they will forego the added support, insight, guidance, interesting debate and increased contentedness that a mentoring relationship affords [18]. A UK study concluded that an official mentoring scheme should be established to ensure that this was provided for all trainees [21]. Mentors should be selected from the ranks of those who make the most effort to provide operative experience and who might also double as hospital BST co-ordinators.
It is also essential that the organisational culture of teaching hospitals be changed. Training must be viewed of equal value to clinical work within the hospital environment to improve the trainee experience. We recommend that hospital management structures be engaged in this process as the presence of BSTs is not solely for HSE service provision but must also encompass training. Reducing the number of training posts would result in a smaller number of higher quality training posts improving the quality of basic surgical training. The posts of clinical assistant and clinical nurse specialist should be introduced to reduce administrative responsibilities on the basic surgical trainee and bridge the inevitable service gaps. We suggest that operative experience be supplemented at hospital level by simulated skills training. This translates into improved performance in theatre and reduces the resources required to complete a task [22–24]. Virtual reality training has been demonstrated to be effective, reproducible and accurate in a variety of settings and serves as an invaluable adjunct to in-theatre training [25–29]. Surgical trainees should therefore be encouraged and facilitated in supplementing theatre time with dedicated simulated skills practice and allowed full access to the extensive training facilities already in existence in the RCSI. Proper provision of these facilities locally would greatly enhance the attractiveness of surgery as a specialty and enhance the training experience.
In conclusion we have highlighted dissatisfaction with the surgical training scheme, and in particular dissatisfaction with operative exposure and the absence of mentoring as the key factors in the negative impression of the current basic surgical training programme. Our study highlights the opportunities that exist to improve basic surgical training, scheme attractiveness and high-quality graduate retention in surgical training.
Key recommendations for improvement of the BST scheme
Merging of BST/HST committees |
Determination of set operative targets per rotation |
Ongoing monitoring of training by the RCSI thus facilitating remedial activity should operative exposure be deficient |
Cessation of BST allocation to a training programme if there is failure by an institution or trainer to provide the pre-determined level of operative experience |
Division of complex operative work into smaller components suitable for trainees |
Allocatation of a BST co-ordinator per training hospital |
Six month rotation periods |
References
RCSI (2011) RCSI own data
Mulholland P (2011) Challenges of a President. Irish medical news
Yeo H, Bucholz E, Ann Sosa J, Curry L, Lewis FR Jr, Jones AT et al (2010) A national study of attrition in general surgery training: which residents leave and where do they go? Ann Surg 252(3):529–534 Discussion 34-6
Lonergan PE, Mulsow J, Tanner WA, Traynor O, Tierney S (2011) Analysing the operative experience of basic surgical trainees in Ireland using a web-based logbook. BMC Med Educ 11:70
(1875) A dictionary of Greek and Roman Antiquities. Chirurgia, London
Ericsson KA (2004) Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med 79(10 Suppl):S70–S81
Purcell Jackson G, Tarpley JL (2009) How long does it take to train a surgeon? Bmj 339:b4260
(2003) Directive 2003/88/EC of the European Parliament and of the Council of 4 November 2003 concerning certain aspects of the organisation of working time. Off J Eur Union L 299/9- L 299/19
Beasley SW, McBride C, Pearson ML (2011) Use of the operative logbook to monitor trainee progress, and evaluate operative supervision provided by accredited training posts. Surgeon 9(Suppl 1):S14–S15
Parsons BA, Blencowe NS, Hollowood AD, Grant JR (2011) Surgical training: the impact of changes in curriculum and experience. J Surg Educ 68(1):44–51
Picarella EA, Simmons JD, Borman KR, Replogle WH, Mitchell ME (2011) “Do one, teach one” the new paradigm in general surgery residency training. J Surg Educ 68(2):126–129
Thomas R, Karanjia N (2011) Operative surgical training: a comparison of logbooks across three eras of training. J Assoc Surg Great B Irel 34:12–15
Tseng WH, Jin L, Canter RJ, Martinez SR, Khatri VP, Gauvin J et al (2011) Surgical resident involvement is safe for common elective general surgery procedures. J Am Coll Surg. 213(1):19–26 discussion-8
Hwang CS, Pagano CR, Wichterman KA, Dunnington GL, Alfrey EJ (2008) Resident versus no resident: a single institutional study on operative complications, mortality, and cost. Surgery 144(2):339–344
Raval MV, Wang X, Cohen ME, Ingraham AM, Bentrem DJ, Dimick JB et al (2011) The influence of resident involvement on surgical outcomes. J Am Coll Surg 212(5):889–898
Fund NTP (2010) Patient treatment register report, Ashford House TS, Dublin 2
Fund NTP (2005) Patient treatment register report, Ashford House TS, Dublin 2
PA-Consulting (2007) Acute hospital bed capacity review: a preferred health system in Ireland to 2020. Ashford House TS, Dublin 2
Kron IL (2011) Surgical mentorship. J Thorac Cardiovasc Surg 142(3):489–492
Healy GB (2011) Role models in surgery. Surgeon 9(Suppl 1):S48–S49
Jaffer U, Pennell A, Musonda P (2010) General surgical trainee experiences of mentoring: a UK regional audit. J Surg Educ 67(1):19–24
Price J, Naik V, Boodhwani M, Brandys T, Hendry P, Lam BK (2011) A randomized evaluation of simulation training on performance of vascular anastomosis on a high-fidelity in vivo model: the role of deliberate practice. J Thorac Cardiovasc Surg 142(3):496–503
Crochet P, Aggarwal R, Dubb SS, Ziprin P, Rajaretnam N, Grantcharov T et al (2011) Deliberate practice on a virtual reality laparoscopic simulator enhances the quality of surgical technical skills. Ann Surg 253(6):1216–1222
Kurahashi AM, Harvey A, MacRae H, Moulton CA, Dubrowski A (2011) Technical skill training improves the ability to learn. Surgery 149(1):1–6
Neary PC, Boyle E, Delaney CP, Senagore AJ, Keane FB, Gallagher AG (2008) Construct validation of a novel hybrid virtual-reality simulator for training and assessing laparoscopic colectomy; results from the first course for experienced senior laparoscopic surgeons. Surg Endosc 22(10):2301–2309
Lonn L, Edmond JJ, Marco J, Kearney PP, Gallagher AG (2012) Virtual reality simulation training in a high-fidelity procedure suite: operator appraisal. J Vasc Interv Radiol 23(10):1361–1366
Cates CU, Gallagher AG (2012) The future of simulation technologies for complex cardiovascular procedures. Eur Heart J 33(17):2127–2134
Boyle E, Al-Akash M, Gallagher AG, Traynor O, Hill AD, Neary PC (2011) Optimising surgical training: use of feedback to reduce errors during a simulated surgical procedure. Postgrad Med J 87(1030):524–528
Ahlberg G, Enochsson L, Gallagher AG, Hedman L, Hogman C, 3rd McClusky DA et al (2007) Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies. Am J Surg 193(6):797–804
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O’Sullivan, K.E., Byrne, J.S. & Walsh, T.N. Basic surgical training in Ireland: the impact of operative experience, training program allocation and mentorship on trainee satisfaction. Ir J Med Sci 182, 687–692 (2013). https://doi.org/10.1007/s11845-013-0956-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-013-0956-4