Abstract
Background
Esophagectomy through cervico-thoraco-abdominal approach is a useful surgical technique in treating patients with esophageal cancer. However, the cervical reconstruction is also known to have a high rate of anastomotic leakage, as well as anastomotic stricture, intrathoracic stomach syndrome, reflux esophagitis and other complications, thereby influencing postoperative recovery and quality of life.
Aims
The objective of this study was to investigate whether tubular stomach is superior to whole stomach in reducing anastomotic leakage for esophageal reconstruction through the cervico-thoraco-abdominal (3-field) approach.
Methods
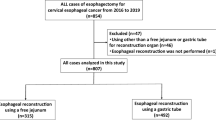
A total of 850 patients undergoing the 3-field esophagectomy were retrospectively included in this study and divided into a tubular stomach reconstruction group (Group A, n = 453) and a whole stomach reconstruction group (Group B, n = 397). All patients underwent esophagectomy through right thorax, left cervical part, abdominal triple incisions and done in esophageal reconstruction by hand-sewn two-layer anastomosis.
Results
Results revealed that in comparison with whole stomach, esophageal reconstruction with tubular stomach had a lower incidence of anastomotic leakage (5.5 vs. 9.3 %, P < 0.05), less manifestation of intrathoracic syndrome (3.3 vs. 9.8 %, P < 0.001) and less occurence of reflux esophagitis (5.1 vs. 11.1 %, P < 0.01). However, for the incidence of anastomotic stricture, there was no significant difference between the two groups (9.3 vs. 9.8 %).
Conclusions
This observation study suggests that for esophageal cancer patients undergoing the 3-field esophagectomy tubular stomach is better than whole stomach for esophageal reconstruction as reflected by a reduced postoperative anastomotic leakage, intrathoracic syndrome and reflux esophagitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophagectomy through cervico-thoraco-abdominal approach is a useful surgical technique in treating patients with esophageal cancer. This approach facilitates the three-field lymph node dissection, leading to a high feasibility of complete resection of primary tumor and removal of metastatic nodes [1–3]. However, the cervical reconstruction is also known to have a high rate of anastomotic leakage, as well as anastomotic stricture, intrathoracic stomach syndrome, reflux esophagitis and other complications, thereby influencing postoperative recovery and quality of life [4–6].
Currently, both the tubular stomach and whole stomach are utilized for esophagectomy through cervico-thoraco-abdominal approach in patients with esophageal cancer. Theoretically, the use of whole stomach for reconstruction after esophagectomy interferes with physiological structure of the patient which seriously affects the quality of postoperative life. Thoracic surgeons have performed such operations with tubular stomach gradually, and this mode of operation is more consistent with the physiological condition of the patients, which significantly improve the quality of postoperative life. Although there have been several reports comparing tubular stomach with whole stomach for cervical reconstruction on blood flow and quality of postoperative life [7, 8], little is known about the clinical comparison of these two operation methods with regard to the relative incidence of postoperative anastomotic leakage, anastomotic stricture, intrathoracic stomach syndrome and reflux esophagitis.
This study aimed to compare the tubular stomach with whole stomach for cervical reconstruction focusing on the incidence of anastomotic leakage, anastomotic stricture, intrathoracic stomach syndrome and reflux esophagitis in esophageal cancer patients who underwent esophagectomy through the cervico-thoraco-abdominal approach.
Materials and methods
Clinical data
From January 2007 to January 2011, 850 esophageal cancer patients undergoing esophagectomy through the cervico-thoraco-abdominal (3-field) approach in the Northern Jiangsu people’s Hospital were retrospectively analysed. Patients were divided into two groups. Group A included a total of 453 cases who underwent esophagectomy using tubular stomach, whereas Group B included a total of 397 cases done with whole stomach. The demographic information of the two patient groups is listed in Table 1. Patients included in this study received neither preoperative radiotherapy nor chemotherapy before operation. Diagnosis of esophageal cancer was made by upper gastrointestinal Barium meal and gastroscopy.
Operative methods
All patients underwent esophagectomy through right thorax, left cervical part, abdominal triple incisions and done in esophageal reconstruction by hand-sewn two-layer anastomosis. All operations followed the principles of radical resection of esophagus: stumping from esophageal tumor edge is greater than 5 cm, at the same time wild lymph nodes dissection is performed. The patients in Group A used tubular stomach. The tubular stomach was formed from the distal aspect of the lesser curvature of the stomach with application of linear staplers. It was created by resection of the lesser curvature of the stomach The formation of the gastric conduit (4–6 cm in diameter) was based on the preservation of the gastroepiploic vessels of the greater curvature of the stomach. And then, the tubular stomach was pulled upward to the left cervical part through the posterior mediastinal route and performed hand-sewn two-layer anastomosis. The patients in Group B used full stomach, which was pulled to the left cervical part through the posterior mediastinal route and performed hand-sewn two-layer anastomosis.
Postoperative determination of anastomotic leakage, anastomotic stricture, intrathoracic stomach syndrome and reflux esophagitis
Cervical wound drainage was the most common presenting symptom of anastomotic leakage, and screening barium swallow also identified the occurrence of anastomotic leakage.
Six months after operation, we assessed reflux symptoms such as pharyngeal regurgitation, cervical heartburn, pain, throat disturbance, or nocturnal cough and the symptoms of stricture such as dysphagia and the symptom of intrathoracic stomach syndrome such as palpitations and chest discomfort after eating [9]. All information was obtained from the patients’ medical records. Upper gastrointestinal endoscopy was performed after the esophagectomy. Anastomotic stricture was diagnosed in patients who required anastomotic dilatation.
Statistical analysis
Normally distributed continuous data such as age are presented as the mean and standard deviation and compared with the Student’s t test. Differences between proportions such as disease staging, tumor location and the incidence of anastomotic leakage were compared with Chi-squared test. A P value of less than 0.05 or smaller was considered statistically significant. The statistical software package SPSS 16.0 was used for all calculations using a standard personal computer.
Results
All patients in two groups were recovered with no operative death. The difference between patients of the two groups in general was not statistically significant (P > 0.05). The incidence of anastomotic leakage was 5.5 % (25/453) in the tubular stomach group and 9.3 % (37/397) in the whole stomach group, the difference was significant (P = 0.033). The incidence of intrathoracic stomach syndrome was 3.3 % (15/453) in the tubular stomach group and 9.3 % (39/397) in the whole stomach group, the difference was significant (P = 0.000). And the incidence of reflux esophagitis was 5.1 % (23/453) in the tubular stomach group and 11.1 % (44/397) in the whole stomach group, the difference was significant (P = 0.001). Follow-up endoscopy showed that the incidence of anastomotic stricture was 9.3 % (42/453) in the tubular stomach group and 9.8 % (39/397) in the whole stomach group, the difference between the two groups was not statistically significant (P = 0.784) (Table 2).
Discussion
In this observational study, we found that in patients undergoing esophagectomy through cervico-thoraco-abdominal approach esophageal reconstruction with tubular stomach is associated with less anastomotic leakage, less intrathoracic stomach syndrome and less reflux esophagitis than those with whole stomach. However, the incidence of anastomotic stricture is similar in both groups.
Anastomotic leakage is one of the most frequently encountered postoperative complications following esophagectomy that is known to have a significantly higher incidence occurring in cervical reconstruction than in thoracic reconstruction [4–6, 10]. The literature reported the incidence of cervical anastomotic leakage with a range between 11.9 ~ 25 % [11–13]. Several factors may have contributed to the high incidence of cervical anastomotic leakage: (1) with high position in cervical reconstruction, anastomotic tension is higher and (2) blood circulation of stoma in cervical reconstruction is poorer than in thoracic reconstruction. Zhang et al. [14] used Doppler laser detection instrument for determination of the gastric tissue’s blood flow of esophagogastric anastomosis and found the blood flow could increase 41 % with tubular stomach. Arcus minor ventriculi is cut away in tubular stomach, which can extend the stomach 5–10 cm. Proper construction of the tubular stomach should afford ample length for a tension-free anastomosis [15]. The cause of anastomotic stricture is more complex, due to the limited diameter of the esophagus, use of stapler, stoma sutured too tight, scar hyperplasia postoperative, local infection and other factors [16]. The key cause is its diameter of esophagus and surgical technique. This study showed that there was no significant correlation in the incidence of anastomotic stenosis between tubular stomach and whole stomach.
This study showed that the incidence of intrathoracic stomach syndrome and reflux esophagitis with tubular stomach was significantly lower than that of the whole stomach. In traditional operations of esophagectomy with whole stomach, gastric peristalsis decreases after being placed in thoracic cavity, which can induce gastric dilation, and it can produce intrathoracic stomach syndrome. Zhang et al. [17] study finds the use of tubular stomach can decrease the incidence of intrathoracic stomach syndrome; meanwhile, it is equivalent in food intake and digestive function between the patients using tubular stomach and the patients using whole stomach. The following is reasons we analyzed: (1) The volume of the stomach is reduced by a range of 21.4–47.2 % after tubulization [18], and theoretically, gastric tubulization should reduce the parietal cell mass, further reducing the acid secretion capacity. (2) Tubular stomach is laid in posterior mediastinum. There is no room for expansion so that the volume occupied by intrathoracic stomach is lesser and it is light in interfering with the heart and lung system. (3) The diameter of tubular stomach and esophagus is close. It is equivalent to the normal physiological channel and can decrease the thoracic gastric retention time of food, make food creeping speed up, which is not easy to cause gastric retention [19]. (4) Tubular gastric volume is small and the gastric wall compliance is low. When stomach is full of food, gastric wall’s expansion is limited and gastric pressure is increased [20]. It is easy to produce gastric emptying function, which can effectively prevent gastric retention, bile reflux and reflux esophagitis. (5) postoperative thoracic gastric volume is reduced, which alleviates the squeeze by lung when patients are in deep inspiration or coughing. And it reduces the symptom and duration of reflux.
This study reveals that tubular stomach is better than whole stomach for esophagectomy through cervico-thoraco-abdominal approach. It can decrease the incidence of anastomotic leakage, intrathoracic stomach syndrome and reflux esophagitis. This surgical technique merits wider application and greater refinement.
References
Udagawa H, Akiyama H (2001) Surgical treatment of esophageal cancer: Tokyo experience of the three-field technique. Dis Esophagus 14(2):110–114
Altorki N, Kent M, Ferrara C et al (2002) Three-field lymph node dissection for squamous cell and adenocarcinoma of the esophagus. Ann Surg 236(2):177–183
Lerut T, Coosemans W, Decker G et al (2004) Extended surgery for cancer of the esophagus and gastroesophageal junction. J Surg Res 117(1):58–63
Orringer MB, Marshall B, Iannettoni MD (2000) Eliminating the cervical esophagogastric anastomotic leak with a side-to-side stapled anastomosis. J Thorac Cardiovasc Surg 119(2):277–288
Cooke DT, Lin GC, Lau CL et al (2009) Analysis of cervical esophagogastric anastomotic leaks after transhiatal esophagectomy: risk factors, presentation, and detection. Ann Thorac Surg 88(1):177–184 (discussion 184-185)
Biere SS, Maas KW, Cuesta MA et al (2011) Cervical or thoracic anastomosis after esophagectomy for cancer: a systematic review and meta-analysis. Dig Surg 28(1):29–35
Ndoye JM, Dia A, Ndiaye A et al (2006) Arteriography of three models of gastric oesophagoplasty: the whole stomach, a wide gastric tube and a narrow gastric tube. Surg Radiol Anat 28(5):429–437
Poghosyan T, Gaujoux S, Chirica M et al (2011) Functional disorders and quality of life after esophagectomy and gastric tube reconstruction for cancer. J Visc Surg 148(5):e327–e335
Kim HK, Choi YH, Shim JH et al (2008) Endoscopic evaluation of the quality of the anastomosis after esophagectomy with gastric tube reconstruction. World J Surg 32(9):2010–2014
Urschel JD (1995) Esophagogastrostomy anastomotic leaks complicating esophagectomy: a review. Am J Surg 169(6):634–640
Fang W, Kato H, Chen W et al (2001) Comparison of surgical management of thoracic esophageal carcinoma between two referral centers in Japan and China. Jpn J Clin Oncol 31(5):203–208
Orringer MB, Marshall B, Chang AC et al (2007) Two thousand transhiatal esophagectomies: changing trends, lessons learned. Ann Surg 246(3):363–374
Nigro JJ, Hagen JA, DeMeester TR et al (1999) Prevalence and location of nodal metastasis in distal esophageal adenocarcinoma confined to the wall: implication for therapy. J Thorac Cardiovasc Surg 117(1):16–25
Zhang CB, Li J, Zheng J et al (2005) Feasible study for construction of gastric tube in easophageal reconstruction. J Henan Med Univ 2(3):175–179
Liebermann-Meffert DM, Meier R, Siewert JR (1992) Vascular anatomy of the gastric tube used for esophageal reconstruction. Ann Thorac Surg 54(6):1110–1115
Lerut TE, van Lanschot JJ (2004) Chronic symptoms after subtotal or partial oesophagectomy: diagnosis and treatment. Best Pract Res Clin Gastroenterol 18(5):901–915
Zhang C, Wu QC, Hou PY et al (2011) Impact of the method of reconstruction after oncologic oesophagectomy on quality of life—a prospective, randomised study. Eur J Cardiothorac Surg 39(1):109–114
D’Journo XB, Martin J, Ferraro P et al (2008) The esophageal remnant after gastric interposition. Dis Esophagus 21(5):377–388
Barbera L, Kemen M, Wegener M et al (1994) Effect of site and width of stomach tube after esophageal resection on gastric emptying. Zentralbl Chir 119:240–244
Bemelman WA, Taat CW, Slors JF et al (1995) Delayed postoperative emptying after esophageal resection is dependent on the size of the gastric substitute. J Am Coll Surg 180(4):461–464
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shu, YS., Sun, C., Shi, WP. et al. Tubular stomach or whole stomach for esophagectomy through cervico-thoraco-abdominal approach: a comparative clinical study on anastomotic leakage. Ir J Med Sci 182, 477–480 (2013). https://doi.org/10.1007/s11845-013-0917-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-013-0917-y