Abstract
Background
Injecting drug use is associated with increased morbidity and mortality. This is the first longitudinal study of a community-based population of injecting drug users (IDUs) in the Republic of Ireland.
Aim
To establish the natural history of IDUs in a deprived Dublin community.
Methods
Eighty-two IDUs (heroin) were recruited over the summer months of 1985. The prevalence of drug use in this district electoral area was established in 1985 and followed-up over a 25-year period with two formal interviews in 1995 and 2010.
Results
It is a descriptive study of a cohort of IDUs established in 1985 prior to human immunodeficiency virus (HIV) testing being available. The majority of the cohort recruited included single, unemployed males aged 20 to 29 years, who had served a prison sentence. Fifty-one (63 %) of the cohort had died by 2010, of which 26 were attributed to HIV disease. The mean age of death was 35.9 years of age (standard deviation 4.1 years). Fifty-two (63 %) of the cohort tested positive for HIV and 58 (71 %) for hepatitis B between 1985 and 2010. The median survival time for those with a positive HIV status was 17 years (95 % CI 14.0–20.0) and for those with a positive hepatitis C status, 21 years (95 % CI 15.5–26.5).
Conclusions
The lifestyle of IDUs, as demonstrated by the experience of this cohort, has hazardous consequences resulting in high levels of morbidity and mortality. A relatively stable picture of HIV associated with IDUs is now emerging in Ireland, as is the case throughout most of the EU. HIV is a more manageable chronic disease, posing challenges for primary care in its treatment of former and existing IDUs who are ageing and now have other chronic diseases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
There are an estimated 15.9 million injecting drug users (IDUs) worldwide [1], of whom between 750,000 and 1,000,000 are within the European Union (EU) [2]. There are 20,790 users in Ireland, with nearly three-quarters living in Dublin [3]. Opiate use contributes the greatest share of morbidity and mortality related to drug use in the EU and has been associated with over 100,000 deaths over its 30-year history. This is a shared international public health problem confronting EU member states [2]. Compared with the general population, opiate users have a substantially higher risk of death and of contracting blood-borne viruses, in particular human immunodeficiency virus (HIV), hepatitis B (HBV) and hepatitis C (HCV) [4–6]. HIV infection reduces survival amongst IDUs [7, 8] and is associated with a sixfold increase in hazard of death before long-term cessation [9]. Worldwide, it is estimated that about three million IDUs are HIV-positive [1].
In 1978 it was apparent that there was, suddenly, a large quantity of good quality heroin available on the streets of Dublin. The epidemic that ensued during the 1980s took root in Dublin’s inner city flat complexes. Young people from vulnerable communities, ignorant of the effects of heroin, ‘embraced this drug rapidly and readily’ [10]. This was predominately an inner city problem, highlighted by the fact that 10 % of 15- to 24-year olds in the North Dublin inner city area in 1983 had used heroin in the previous 12 months [11]. Merchants Quay F is ranked as one of the most deprived district electoral areas in the Republic of Ireland according to deprivation scores [12]. A report published in 1983 by a local residents committee described the area in which this study was conducted at the time as bearing all the hallmarks of a deprived inner city area, with a higher rate of 15- to 24-year olds (57.7 %) than the national average, high levels of unemployment (59.2 %) and only 5 % of 15- to 24-year olds in full time education [13].
Intravenous drug use was soon recognised as a significant risk factor for the transmission of HIV. HIV testing initially became available in 1987 and highlighted the rapid increase in new diagnoses among IDUs [14]. Clarke et al. describe that mandatory case-based reporting was introduced in the Republic of Ireland in 2001 and back projections used to estimate the incidence and modes of transmission prior to this time. This estimated cumulative number of HIV-positive cases reported by the end of 1999 was 2,195, of which IDUs represented 41.6 %. From 2000 to the end of 2010, IDUs represented only 14.2 % of the cumulative figure (3,773) for this period [15]. Over this time period, the presentation of the disease has moved from infections in IDUs towards infections in men who have sex with men (MSM) and heterosexuals.
The HIV/AIDS pandemic of the 1980s was an international crisis, and intervention came by way of needle substitution programmes (NSPs) and opioid substitution programmes (OSPs). In1989, the State introduced such programmes into Ireland marking a shift in policy from drug prevention towards harm reduction initiatives. These services composed of fixed site NSPs and OSPs, as well as mobile units and specialist services for sex-workers and homeless people [16]. Recent published data showed that between 7,069 and 9,302 IDUs access NSPs, around 40 % of all IDUs in Republic of Ireland, while the number of injecting and non-IDUs receiving opiate substitution treatment is between 8,029 and 9,326 [17].
The first part of this study took place in 1985 and was the third of three community-based studies carried out under the auspices of the Medical Social Research Board, to establish the prevalence of an emerging drug use problem, in a sample of vulnerable communities in Dublin [10, 18, 19]. This is the first longitudinal study of such a population in the Republic of Ireland and the only one of the three studies to be followed-up over a 25-year period. It aims to establish the natural history of a community-based cohort of IDUs.
Methods
Subjects and setting
The study cohort was established in 1985 by identifying and interviewing all known drug users, within Merchant’s Quay F Ward, a district electoral division in Dublin’s south inner city. A total of 103 individuals, known or suspected of problem drug use, were identified from various sources and cross referenced. These sources included the author’s own clinical records, other local general practitioners, other local health and social service personnel, local community workers and the study respondents themselves. Each individual that was recruited was then asked to suggest names from within their injecting peer groups and those identified were then offered interviews. Snowball sampling is a widely accepted method of recruitment to reach such hidden populations [20, 21]. Individuals were excluded if they were not confirmed IDUs living within the target study area. Twenty-one of the target group either refused to be interviewed, or could not be traced. Eighty-two were established as the study cohort and were interviewed in 1985, giving an 80 % response rate (Fig. 1).
Contact was made through the practitioner’s clinical records, known family members and other clinicians within the area where a good rapport and trust already existed with the target group. Once contact was made, the individuals were interviewed face-to-face using a structured questionnaire, in a variety of clinical settings, in their own homes, within prisons both in Ireland and England, and two by telephone. All participants admitted to regular heroin use by injection, that is daily use for a period of at least 1 month, between 1979 and 1985. It was during 1979 that the problem involving heroin usage first became apparent to the local health and social care workers within the area. The study instrument established the basic social, medical and drug use history of the cohort.
In 1995, the study cohort was retraced and contact made using similar methods as for initial recruitment. Fifty of the remaining 55 were re-interviewed (91 % response rate). The results of this study were initially reported as part of an M.D. thesis [22]. In 2010, the surviving members of the cohort were once again retraced and 25 of a possible 31 were re-interviewed (81 % response rate) using the same study questionnaire. Official death certificates were obtained through the General Register Office (GRO), Dublin.
Comparison cohort
A comparison cohort of age-matched non-opiate users from the same community setting was retrospectively drawn from the author’s practice records in 1995. The population of Merchants Quay F Ward, between the ages of 15 and 34 years, was 984 persons in 1986, according to the census figures (CSO 1986) [23]. The comparison cohort was made up of all the non-opiate users, within the same age range as the index cohort from Merchants Quay F Ward who had attended the author’s practice in 1985. This number was 201 and represented 20 % of the Ward population between the ages of 15 and 34 years who were known to the author’s practice in 1985. The majority of both groups had an address in St. Teresa’s Gardens, the only local authority flat complex in the Ward and therefore shared the same socio-demographic profile. The comparison cohort was analysed in 1995 and 2010 for death rates and HIV status similarly to the study cohort, using the author’s clinical records, the General Register Office and the Genito-Urinary Medicine services at St. James Hospital, Dublin.
Approval
The original 1985 study was carried out under the auspices of the Medico-Social Research Board (later subsumed into the Health Research Board) and in 1995 the Research Ethics Committee of the Irish College of General Practitioners granted ethical approval for the study.
Results
Eighty-two questionnaires were completed, out of a possible 103, by face-to-face interviews in 1985. The age range of respondents was 16–37 years, with 67 (82 %) aged between 20 and 29 years. Sixty-two (76 %) of the respondents were male, 62 (76 %) were single, 55 (87 %) were unemployed and 63 (77 %) had been in prison (Table 1). Fifty-three (65 %) of the cohort had started to inject by age 19, the youngest being 10 years of age. All respondents gave a history of polydrug use. The most commonly used groups of drugs in addition to heroin were benzodiazepines and alcohol.
Seven (8.5 %) of the cohort had remained in school beyond the age of 15 years. All respondents came from large families (mean 8.2 siblings), with high levels of paternal unemployment, or from single parent households. Many also gave a history of alcohol abuse within the family. A follow-up review of non-responders showed 20 of the 21 had attended the only drug treatment centre in Dublin and are similar to those interviewed in socio-demographic characteristics, age range and drug use history. In 1985, 40 (49 %) of the 82 participants reported current injecting opiate use, that is, daily injection use in the last month, at the time of interview. In 1995, 19 of the 50 (38 %) respondents admitted current injection drug use, 8 of whom reported abstinence in 1985. A further 24 (48 %) were on a methadone programme with eight of these admitting to use of street heroin while on the methadone treatment (Table 2).
In total, 52 (63 %) of the cohort were found to have tested HIV-positive and 58 (71 %) to be hepatitis B virus (HBV) positive, over the study period. Thirty-two individuals (39 %) were diagnosed as hepatitis C (HCV) positive. However, 34 (41 %) of the original cohort was not tested, as serology testing for HCV antibodies was not routine in the Republic of Ireland, until 1992.
Mortality
Fifty-one (62 %) of the original study cohort had died by 2010. The cause of death of each individual has been transcribed from the official death record. The cause of death recorded in the earlier years often does not describe the relationship to HIV disease. It is only when read in conjunction with the known HIV sero-positivity of the individual that a link to HIV disease is recognised. The cause of death for the cohort can be summarised into four main groups: (i) HIV related (ii) opiate overdose (iii) accident or violence and (iv) medical non-HIV related.
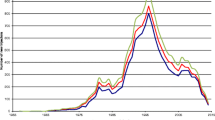
At the time of their death, 42 (82 %) were HIV sero-positive, and 26 (51 %) died as a direct result of HIV. Nine (18 %), all male, died as a consequence of opiate overdose. Five (10 %), all male, had died by accident or violent death, i.e. the result of stabbings, falling from a height or single vehicle traffic accidents (Table 3). Twenty-seven deaths occurred in the first 10-year period of the study, of which 14 were HIV related. Between 1995 and 2010 there were a further 24 deaths, of which 12 were HIV related (Fig. 2). Of the medical non-HIV deaths, most were reported as consequences of chronic liver disease, respiratory disease or cerebrovascular disease. The mean age of death was 35.9 years (standard deviation 4.1 years) and the median survival time was 17 years (95 % CI 14.0–20.0) for those cohort members with HIV-positive result (Fig. 3). At the time of their death, 82 % were HBV sero-positive and 43 % were HCV sero-positive (34 cases were never tested). The median survival time for those with a positive hepatitis C status was 21 years (95 % CI 15.5–26.5), which was significantly lower than the median survival time for drug users with a negative hepatitis C status (Fig. 4).
Year of death and HIV status of cohort (n = 51). A total of 51 deaths occurred between 1985 and 2010, these deaths were grouped in 5-year clusters (1985–1989, n = 3; 1990–1995, n = 24; 1996–2000, n = 15; 2001–2005, n = 7; and 2006–2010, n = 2). HIV status at the time of death: HIV-positive 42, HIV-negative 4 and HIV-unknown 5
HIV as a factor for survival. Participants were included in these analyses only if they were tested for HIV and the test result was known (n = 69). The median survival time for drug user with a positive HIV status was 17.0 years (95 % CI 14.0–20.0) which was significantly [log-rank (Mantel-Cox) χ2 = 14.8, df = 1, p < 0.001] lower than the median survival time for drug users with a negative HIV status
Hepatitis C as a factor for survival. Participants were included in these analyses only if they were tested for hepatitis C and the test result was known (n = 43). The median survival time for drug user with a positive hepatitis C status was 21.0 years (95 % CI 15.5–26.5) which was significantly [log-rank (Mantel-Cox) χ2 = 7.1, df = 1, p = 0.006] lower than the median survival time for drug users with a negative hepatitis C status
Surviving cohort
In 2010, 31 individuals, of the original cohort, were either known to be still alive, or did not have a death certificate in the records of the GRO. The majority of them are now aged between 45 and 54 years. Twenty-five were re-interviewed and six were not found (81 % response rate). Of the original 82 in the cohort (62 males, 20 females), 16 males and 9 females were still alive in 2010. The median survival for males was 19 years (95 % CI 15.3–22.7), and 27 years for the female cohort (Fig. 5).
Gender difference in survival time. The median survival time for male drug users was 19.0 years (95 % CI 15.3–22.7) which was lower (mean difference 2.6 years, median difference 8 years) than the median survival time for female drug users. This was a significant trend (p < 0.1): log-rank (Mantel-Cox) χ2 = 3.1, df = 1, p = 0.079
In 2010, none of the surviving cohort were currently using drugs by injection, however, 11 (44 %) were currently registered with the Central Treatment Services (Table 3) and on a methadone programme. Eight (32 %) are HIV-positive, all of whom were currently receiving anti-retroviral therapy (ART) and attending a hospital-based HIV clinic. Fifteen (60 %) of the cohort members re-interviewed were HBV positive and ten (40 %) were HCV positive. All reported regular engagement with primary and secondary care services.
Comparison cohort
Eleven persons of the comparison cohort of 201, that is 5.5 %, are known to have died. Two members of the comparison cohort are HIV-positive. These mortality rates are in line with census figures for the area [24].
Discussion
Summary of main findings
This study documents the natural history of a cohort of IDUs across a 25-year period. It confirms the findings in other studies, but over a much longer timeframe. Further, it is a community-based cohort and not a clinic, or institutional-based study, and therefore reflects this community’s experience of problem drug use more starkly. Injecting opiate use is a chronic relapsing condition with hazardous health consequences for those involved, as shown. The surviving HIV-positive patients are now an ageing population, and have evidence of other chronic viral diseases and conditions posing a further challenge for the primary care teams in the area.
Strengths and limitations of the study
This is the first community-based longitudinal study of IDUs in Ireland. Several studies have acknowledged the reliability and validity of self-reported drug use history [25–27]. This is achieved through a familiar interviewer who is knowledgeable about problem drug use. The main author of this study has been in practice in inner city Dublin since 1978 and was known to many of the recruited respondents in 1985. Respondent data were triangulated with other sources of information, including hospital-based infectious disease clinics and drug treatment centres. Furthermore, the high rate of death and infection is consistent with other studies of a similar setting and cohort demographic.
One limitation of this study is that it is a smaller cohort than in other studies. Further, the possibility of a history of abuse, sexual or physical, was not explored with respondents in the original questionnaire (1985). It has since become apparent to the principal author during consultations within his practice that this is a significant issue with some of the survivors.
Comparison with existing literature
It is well established that injecting drug use is associated with high levels of blood-borne virus infections [28–32], mostly notably HIV, hepatitis B and hepatitis C. The majority of the study cohort tested positive for HIV and HBV, with HCV levels underestimated at 39 % due to routine testing not being available until 1992. However, subsequent studies have shown that 62–81 % of IDUs attending general practice in Ireland are infected with HCV [33]. When this cohort initiated opiate use in the late 1970s and early 1980s little was known of the potential threat of infection from needle-sharing and unprotected sexual intercourse. Between 1989 and 1999, the HIV cases in Ireland were largely driven by injecting drug users. At present, there is a relatively stable HIV prevalence in Western Europe with high coverage of services for IDU populations [2]. This is reflected in the Republic of Ireland with the annual figures of HIV cases linked to IDUs accounting for only 6.6 % of newly diagnosed cases in 2010, this is in stark contrast to 61 % in 1985 [15]. This is largely due to the provision of accessible drug treatment services and better informed and educated injectors, as well as the increase in heterosexual and homosexual cases.
This study cohort shows high levels of HIV infection (63 %) and is identified as the single most common cause of death over the 25 years. HIV-related mortality peaked in this study cohort in the early to mid-1990s, showing an identical picture to that described by Copeland et al. [34], a reflection of the development of untreated HIV from the early epidemic of the 1980s. This was the time of greatest risk for acquiring blood-borne diseases. Copeland et al. also comment on reports indicating that deaths in opiate drug users are thirteen times than that of non-users, which are in keeping with our findings of injecting and non-injecting cohorts form the same electoral area. The injecting cohort had a mortality rate eleven times that of the non-using cohort (62 % compared to 5.5 %).
Much of the comparative work done to date is derived from colleagues in Edinburgh, Scotland. A study in 1994 by Robertson et al. describes a similar cohort of injecting users from a marginalised population in Edinburgh recruited between 1982 and 1985 and followed-up 10 years later. It similarly highlights the chronic relapsing nature of opiate usage, with periods of cessation followed by episodic intravenous drug use [35]. Both the Robertson study and this one demonstrate the high rates of HIV infection amongst early IDUs of the 1980s with over half the cohort populations in both studies reported as HIV sero-positive. Comparing mortality in our study for the 10-year period 1985–1995 to that of the Robertson study, the death rate amongst the Dublin cohort stood higher at 33 % with the Edinburgh cohort reporting 21 % deaths, possibly reflecting the earlier introduction of harm reduction initiatives in the UK in 1987. Through the same primary medical care facility in Edinburgh, MacLeod et al. identified and recruited drug injectors between 1980 and 2006 on a rolling basis, whereas this study captures a group of IDUs at a single point in time (1985) and follows it across a 25-year period providing information of their unique experience. MacLeod’s results reflect this combination of new, younger, IDUs alongside older generations, with almost 31 % of the follow-up population reporting current injecting drug use [36]. By comparison, our study shows that 25 years from the point of recruitment, those still alive reported no injecting drug use.
Implications for clinical practice and future research
Chronic illness and multimorbidity are common among problem drug users attending general practice [37], and those surviving members of this cohort are engaged with both primary and secondary level care for management of their health problems, most of which relate to their drug problem. The European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) 2010 report shows that Europe’s drug-using population is ageing and that “meeting the needs of older drug users is a growing issue for treatment services”, particularly so in countries that first experienced the epidemic of the early 1980s [2]. This also raises the issue of transferring much of current HIV treatment from a specialist secondary setting into primary care, given that it is now described as a manageable chronic disease. High rates of early diagnoses and intervention with an increased life expectancy have led to a growing cohort of ageing patients [38]. One-third of the surviving study cohort are HIV-positive, over 45 years of age, and are having their anti-retroviral regimen monitored locally in St James’s University Hospital, Dublin. These same patients also have a number of co-morbidities being managed in their general practice services. There is a push for greater acceptance of care in primary care of HIV-positive patients. This has been growing in recent years, with its proponents arguing that a shared care model would allow for more appropriate and accessible care for such patients [39]. For this transition to take place there needs to be focused education of all personnel in the primary care teams, in areas of high need.
Finally, this study demonstrates that general practice is well placed to conduct longitudinal studies with marginal groups in society
Conclusions
The lifestyle of IDUs as demonstrated by the experience of this cohort has hazardous consequences resulting in high levels of morbidity and mortality. A relatively stable picture of HIV associated with IDUs is now emerging in Ireland, as is the case throughout most of the EU. HIV is a more manageable chronic disease, posing challenges for primary care in its treatment of former and existing IDUs who are ageing and now have other chronic diseases.
References
Mathers BM, Degenhardt L, Phillips B, et al (2008) Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet 372(9651):1733–1745
European Monitoring Centre for Drugs and Drug Addiction (ECMDDA) 2010 Report, Chapter 6. Opioid use and drug injection, pp 71–78
Kelly A, Carvalho M, Teljeur C (2009) Prevalence of opiate use in Ireland 2006: a 3-source capture–recapture study. National Advisory Committee on Drugs, Dublin
Cornish R, Macleod J, Strang J, Vickerman P, Hickman M (2010) Risk of death during and after opiate substitution treatment in primary care: prospective observational study in UK General Practice Research Database. BMJ 341:c5475
Degenhardt L, Hall W, Warner-Smith M (2006) Using cohort studies to estimate mortality among injecting drug users that is not attributable to AIDS. Sex Transm Dis 82:56–63
Hulse GK, English DR, Milne E, Holman CD (1999) The quantification of mortality resulting from the regular use of illicit opiates. Addiction 4(2):221–229
Tyndall MW, Craib KJ, Currie S, Li K, O’Shaughnessy MV, Schechter MT (2001) Impact of HIV infection on mortality in a cohort of injection drug users. J Acquir Immune Defic Syndr 28(4):351–357
Bargagli AM, Sperati A, Davoli M, Forastiere F, Perucci CA (2001) Mortality among problem drug users in Rome: an 18-year follow-up study, 1980–97. Addiction 96:1455–1463
Kimber J, Copeland L, Hickman M (2010) Survival and cessation in injecting drug users: prospective observational study of outcomes and effect of opiate substitution treatment. BMJ 340:c3172
O’Kelly FD, Bury G, Cullen B, Dean G (1988) The rise and fall of heroin in an inner city area of Dublin. Ir J Med Sci 157(2):35–38
Dean G, Bradshaw JS, Lavelle P (1983) Drug misuse in Ireland 1982-3. The Medico-Social Research Board, Dublin
Hasse T, Pratschke J (2005) Deprivation and its spatial articulation in the Republic of Ireland. Pobal, Dublin
‘Fighting back’ (1983) The St. Teresa’s Gardens Development Committee
Clarke S, Keenan E, Bergin C, Lyons F, Hopkins S, Mulcahy F (2001) The changing epidemiology of HIV infection in injecting drug users in Dublin, Ireland. HIV Med 2:236–240
Health Protection Surveillance Centre, Annual Report 2010. HIV and AIDS, Chapter 5.3, pp 75–78
A Joint Report by the National Drugs Strategy Team and National Advisory Committee on Drugs (2008) Needle exchange provision in Ireland. Current provision of needle exchange in Ireland, Chapter 4.3, pp 26–30
Mathers BM, Degenhardt L, Ali H et al (2010) HIV prevention, treatment and care services for people who inject drugs: a systematic review of global, regional and national coverage. Lancet 375:1014–1028
Dean G, O’Hara A, O’Connor A, Kelly M, Kelly G (1988) The opiate epidemic in Dublin 1979–1983. Ir Med J 78(4):107–110
Power B (1986) Heroin use in a Dun Laoghaire Borough area 1983-4. The Medico-Social Research Board, Dublin
Griffiths P, Gossop M, Powis B, Strang J (1993) Reaching hidden populations of drug users by privileged access interviewers: methodological and practical issues. Addiction 88:1617–1626
Kaplan CD, Korf D, Sterk C (1987) Temporal and social contexts of heroin-using populations: an illustration of the snowball sampling technique. J Nerv Ment Dis 175(9):566–574
O’Kelly FD (2000) The natural history of injecting drug use in a Dublin community (1985–1995). MD Thesis, Trinity College Dublin 2000. Available online: http://www.drugsandalcohol.ie/4342. Accessed 17 Sept 2011
Central Statistics Office (1986) Small area population figures from the Central Statistics Office, Dublin
Central Statistics Office (2011) Small area population figures from the Central Statistics Office, Dublin
Ball JC (1967) The reliability and validity of interview data obtained from fifty-nine narcotic drug addicts. AM J Soc 72:650–654
Brown J, Kranzler HR, Del Boca FK (1992) Self-reports by alcohol and drug abuse in-patients: factors affecting reliability and validity. Br J Addict 87(7):1013–1024
Hyser Y, Anglen MD, Chou E (1992) Reliability of retrospective self-reported by narcotic addicts. Psychol Assess 4:207–213
Aceijas C, Stimson GV, Hickman M, Rhodes T (2004) Global overview of injecting drug use and HIV infection among injecting drug users. AIDS 18:2295–2303
UNAIDS (2010) Report on the global AIDS epidemic. http://www.unaids.org/globalreport/Global_report.htm. Accessed 11 Sept 2001
Devi K, Singh NB, Singh HL, Singh YM (2009) Co-infection by human immunodeficiency virus, hepatitis B virus and hepatitis C virus in injecting drug users. J Indian Med Assoc 107(3):144, 146–147
Strader DB (2005) Co-infection with HIV and hepatitis C virus in injection drug users and minority populations. Clin Infect Dis 41 (Suppl 1):S7–S13
Gowing L, Farrell MF, Bornemann R, Sullivan LE, Ali R (2011) Oral substitution treatment of injecting drug users for prevention of HIV infection. Cochrane Database Syst Rev (8):CD004145
Cullen W, Stanely J, Langton D, Kelly Y, Bury G (2007) Management of hepatitis C among drug users attending general practice in Ireland: baseline data from the Dublin area hepatitis C in general practice initiative. Eur J Gen Pract 13(1):5–12
Copeland L, Budd J, Robertson JR, Elton R (2004) Changing patterns in causes of death in a cohort of injecting drug users 1980–2001. Arch Intern Med 164:1214–1220
Robertson JR, Ronald PJ, Raab GM, Ross AJ, Parpia T (1994) Deaths, HIV infection, abstinence and other outcomes in a cohort of injecting drug users followed up for 10 year. BMJ 309:369–370
MacLeod J, Copeland L, Hickman M et al (2010) The Edinburgh addiction cohort: recruitment and follow-up of a primary care based sample of injection drug users and non-injecting controls. BMC Public Health 10:101
Cullen W, O’Brien S, Carroll A, O’Kelly FD, Bury G (2009) Chronic illness and multimorbidity among drug users: a comparative cross sectional pilot study in primary care. BMC Fam Pract 10:25
Health Protection Agency (2010) Largest ever annual number of new HIV diagnoses in MSM (online). http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1296683688485. Accessed 11 Sept 2011
British HIV Association (2011) Extending the role of primary and community care in HIV (online). http://www.bhiva.or/documents/Guidelines/Standards/090302%20PCBriefing. Accessed 11 Sept 2011
Acknowledgments
The authors would like to acknowledge the unrestricted grant generously provided by the Fiona Bradley Foundation to fund this study. The authors would like to thank all the participants in this study and the staff of the Department of Primary Care and Public Health, Trinity College Dublin. We would also like to acknowledge the contribution of Dr. Udo Reulbach (Dept. of Primary Care and Public Health, Trinty College Dublin), Prof. Colm Bergin (Consultant Physician in Infectious Diseases, St. James’s Hospital, Dublin) and Prof. Gerard Bury (Dept. General Practice, University College Dublin) to this study.
Conflict of interest
The authors have no competing interests and therefore have nothing to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O’Kelly, F.D., O’Kelly, C.M. The natural history of injecting drug use: a 25-year longitudinal study of a cohort of injecting drug users in inner city Dublin. Ir J Med Sci 181, 541–548 (2012). https://doi.org/10.1007/s11845-012-0814-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-012-0814-9