Abstract
Objective
To report the pregnancy outcomes in Irish female renal transplant recipients on modern maintenance immunosuppression.
Methods
The Republic of Ireland transplant database was accessed to identify the patient cohort in question. All female renal transplant recipients whose transplantation was in Ireland before or during their reproductive years were included. A questionnaire was sent to the identified women. A chart review was performed for those women who reported a pregnancy following renal transplantation.
Results
Two hundred and ten women met the inclusion criteria. There was a response rate of 70% (n = 148). Eighteen women reported 29 pregnancies. The live birth rate was 76%. The mean gestation of the live births was 36.2 weeks with a mean birth weight of 3.0 kg. There were six cases of pre-eclampsia. Twin pregnancies and those entering pregnancy with a creatinine greater than 135 µmol/l had particularly complicated clinical courses. Four women had not conceived post transplant despite actively trying for over 1 year. Two women utilised assisted fertility methods (in vitro fertilisation), one of whom became pregnant.
Conclusions
A significant proportion of women who attempt to conceive following renal transplantation are successful, without the use of assisted fertility. Pregnancy in this setting warrants meticulous multidisciplinary care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
End-stage kidney disease is associated with subfertility and poor pregnancy outcomes. Endocrine and gonadal dysfunction experienced in end-stage renal disease is thought to be rapidly reversed after successful renal transplantation, with restoration of reproductive health in female renal transplant recipients of child-bearing age [1].
The first successful pregnancy in a renal transplant recipient occurred in 1958 [2]. Since then, thousands of pregnancies in renal transplant recipients have been reported by means of national and international registry reports and single centre reports [3]. This has led to an improved understanding of the risks and interactions involved.
The transplant recipient mentioned above was not receiving any immunosuppression as her donor was her identical twin sister. However, the vast majority of renal transplant recipients require maintenance immunosuppression, the regimes of which are continuously evolving. As immunosuppressive regimen evolve; so too must our research and understanding of this complex patient group.
Maintenance immunosuppression after kidney transplant usually consists of a calcineurin inhibitor, an anti-metabolite, and steroids in low dose. In the last decade, tacrolimus has replaced cyclosporine as the calcineurin inhibitor of choice, and mycophenolate mofetil has replaced azathioprine as the anti-metabolite of choice in renal transplant immunosuppression [4].
There is accumulating evidence that mycophenolate mofetil is teratogenic and so, when pregnancy is planned, a switch is made to azathioprine several months pre-conception [5]. If an unplanned pregnancy occurs whilst taking mycophenolate mofetil, the switch is made as soon as the pregnancy is discovered.
The literature regarding pregnancy outcomes for those receiving tacrolimus is smaller than for older immunosuppressive regimes. We aimed to prepare a national report documenting the pregnancy outcomes in Irish female renal transplant recipients since the introduction of tacrolimus.
Little is known about the rate of infertility in this patient group. Our secondary aim was to determine the uptake rate of assisted fertility methods and use this as a gauge for infertility rates.
Methods
Ethical approval was obtained from the Beaumont Hospital Research and Ethics Committee based in the Republic of Ireland Renal Transplant Centre in Beaumont Hospital.
The Republic of Ireland renal transplant database was accessed. All female kidney and simultaneous pancreas-kidney (SPK) transplant recipients who were transplanted prior to 2009 in Ireland were identified. Patients were included if they were over the age of 18 at the time of the study and had been transplanted at the age of 45 or younger.
A postal questionnaire was sent to the identified females. The questionnaire was divided into two sections: one regarding fertility issues and the other regarding pregnancy outcomes. A follow-up phone call was made to those who did not reply within a 4-week period. A detailed medical and obstetric chart review was performed for all reported pregnancies.
Results
Of the 210 women who were eligible for inclusion, 148 (70%) responded to the questionnaire. Sixteen renal transplant recipients reported 27 pregnancies, two of which were twin pregnancies. One further pregnancy was ongoing at the time of analysis and so was not included in the analysis. Two SPK recipients reported one singleton pregnancy each. The baseline maternal demographics are outlined in Table 1.
All women were receiving tacrolimus, an anti-metabolite and prednisolone as standard immunosuppression. In the cases of planned pregnancies, mycophenolate mofetil had been switched to azathioprine 3–6 months pre-pregnancy. If unplanned, the switch was made when pregnancy was confirmed. There were no reported pregnancies in women receiving sirolimus.
Fetal outcomes
There were four miscarriages (<24 weeks gestation). One set of twins miscarried at 10 weeks gestation. One single twin miscarried at 14 weeks (the second twin was live-born at 30 weeks). One singleton baby was lost at 23 weeks following a protracted period of maternal illness and transplant kidney failure.
There were four singleton stillbirths (≥24 weeks gestation). Three were lost due to utero-placental insufficiency. The fourth was entirely unexpected at 36 weeks gestation. The post-mortem showed confluent haemorrhage of the vital organs with severe fetal maceration. The exact cause for this was not identified.
Of the 23 live births, there was one neonatal death. The baby in question was born at 24 weeks gestation as a result of cervical incompetence. In total, seven babies (30%) spent time in the neonatal intensive care unit.
The mean gestation of the 23 live births was 36.2 weeks (range 24–40 weeks). Eight (34%) of the live births were premature (<37 weeks gestation). The mean birth weight was 3.0 kg (range 1.0–4.5 kg); nine (39%) were of low birth weight (<2.5 kg). Four (17%) were of very low birth weight (<1.5 kg). Of the live births, there were four spontaneous vaginal deliveries, eight induced vaginal deliveries, three planned caesarean sections and eight emergency caesarean sections. The most common indication for emergency caesarean section was pre-eclampsia (n = 6). Fetal outcomes are summarised in Table 2.
None of the mothers breast-fed. The majority chose not to because of the risk of passage of medications into breast milk. One reported that she was too ill herself to breast-feed. No congenital abnormalities were reported. No childhood medical, immunological or neuro-developmental problems were reported.
Maternal outcomes
The mean age at the time of delivery was 33.4 years (range 24–39 years). One mother had pre-existing diabetes, eight had pre-existing medicated hypertension. The most frequently encountered maternal complications are summarised in Table 3.
The diagnosis of pre-eclampsia can be difficult in renal transplant recipients as many have baseline proteinuria and hypertension. It can also be particularly devastating in this setting. Of the six cases of pre-eclampsia, all ended in emergency caesarean section. Both baby and transplant kidney were lost in two cases. There were no cases of HELLP (haemolysis; elevated liver enzymes; low platelets) syndrome.
Renal transplant outcomes
The mean time from transplant to conception was 4.5 years (range 2–9 years). New or progressive proteinuria developed in 15 pregnancies, 6 of whom later developed the full syndrome of pre-eclampsia.
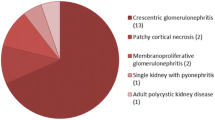
Mean creatinine at the time of conception was 100 µmol/l (range 60–205 µmol/l). Renal dysfunction (defined for the purposes of this study, as in other international studies, as 20% rise in serum creatinine during the pregnancy) developed in 12 pregnancies. Six cases were in the setting of pre-eclampsia; two of whom lost graft function and required dialysis. One was due to biopsy-proven acute rejection, which was successfully managed with intravenous steroids.
All patients with significant allograft dysfunction at the time of conception (baseline creatinine > 135 µmol/l; n = 3) had complicated clinical courses, which involved severe pre-eclampsia, loss of baby, or loss of transplant kidney.
Of the 12 cases of renal dysfunction, 9 largely settled over time following delivery. Two patients started dialysis as a result of acute kidney injury in the setting of pre-eclampsia. One has since been re-transplanted. A third patient, who also had severe pre-eclampsia and acute renal dysfunction during pregnancy, now has severe chronic transplant dysfunction, and is approaching dialysis 2 years post-delivery. Mean serum creatinine 3 months post-partum (excluding the two patients on dialysis) was 127 µmol/l.
Two simultaneous pancreas-kidney recipients reported one pregnancy each. Both had complicated pregnancies resulting in a stillbirth at 36 weeks in one case and a premature (30 weeks) delivery in the other.
In terms of medications, one unplanned pregnancy occurred while the mother was receiving mycophenolate mofetil. This was switched to azathioprine at 3 weeks gestation with no reported adverse outcomes. One pregnancy occurred while the mother was receiving an angiotensin converting enzyme (ACE) inhibitor. Again, it was discontinued early in pregnancy (9 weeks gestation) and no adverse outcomes were reported. There were no pregnancies whilst receiving a statin.
Fertility issues
Of the 148 women who responded to the questionnaire, 130 did not become pregnant following renal transplantation. Of these, four had been actively trying for over 1 year to become pregnant. One had used assisted fertility methods (in vitro fertilisation) once without success.
One SPK recipient who went on to have a pregnancy conceived with the aid of in vitro fertilisation. She delivered a live born baby at 30 weeks.
Discussion
Tacrolimus is the current calcineurin inhibitor of choice in renal transplant medicine in Ireland and most western countries. It has led to improved renal transplant survival and lower rates of rejection since its introduction over 10 years ago [6]. It is important to establish whether immunosuppression regimes incorporating tacrolimus are favourable to women of reproductive age.
The outcomes described above compare favourably with previously published Irish data in the setting of older immunosuppressive regimes [7, 8]. The Irish report on pregnancy outcomes in patients receiving a cyclosporine-based regimen described a similar number of live births (23/29) but higher rates of fetal complications including prematurity (73.9%), low birth weight (65.2%), neonatal intensive care (61%) and neonatal death (8.7) [7].
This analysis also compares favourably with various international reports in terms of live birth rate, rate of premature delivery, maternal complications and renal transplant outcomes [9, 10]. For example, the UK Transplant Pregnancy Registry reported live births in 79% of renal transplant recipients with pre-term delivery in 50%.
The American Society of Transplantation consensus opinion recently set out guidelines for the management of pregnancy in renal transplant recipients [11]. These guidelines outline optimal pre-pregnancy conditions including no rejection in the last year, no potentially teratogenic infections, stable dosing of maintenance immunosuppression and stable adequate renal function (creatinine < 135 µmol/l). Several other studies have found an increase in maternal, graft and fetal complications with increasing pre-pregnancy creatinine value [9]. Indeed in our study, those (n = 3) that entered pregnancy with a creatinine greater than 135 µmol/l had particularly complicated courses as outlined above.
The large number of reported pregnancies in the international literature suggests that many females enjoy full reproductive health after transplantation. However, the number of females who remain infertile is unknown. The precise uptake of IVF and other assisted fertility methods, which can be used as a gauge for infertility rates, is also unknown.
There are case reports documenting pregnancy following in vitro fertilisation (IVF) [12, 13] and, indeed, one of the women in our analysis had a successful pregnancy following IVF. Our findings suggest that the number of women who are unable to conceive despite trying for over 1 year is small. The reported uptake of IVF was also small (n = 2). Neither of the two women experienced adverse outcomes as a direct result of IVF, although it was successful for one woman only.
The above data analysis from the national transplant registry is encouraging. The majority (75%) of renal transplant recipients receiving tacrolimus based immunosuppression deliver a live-born baby. However, the risks and complications are not insignificant and therefore detailed pre-pregnancy counselling is crucial. Specific sub-groups such as SPK recipients, those with creatinine > 135 µmol/l, those with a twin pregnancy and those utilising assisted fertility methods are at a particularly high risk of complications.
Our study has a number of important strengths. There was a good response rate to the questionnaire. This patient group is tightly followed by both medical and obstetric teams and so patient records were very informative.
There were also a number of weaknesses in our study. The outcomes of the non-responders are unknown. A significant proportion of the data collected relied on patient self-reporting. Proteinuria measurement was inconsistent between patients and centres and so it was difficult to draw any conclusions from this data.
We conclude that meticulous multi-disciplinary care prior to conception, during pregnancy and in the post-partum period is essential to ensure optimal outcomes for this complicated patient cohort.
Ethics approval: Ethics approval was sought and granted by the Ethical (Medical Research) Committee, Beaumont Hospital, Dublin, Ireland. REC reference 09/96. Final approval date 3/12/09.
References
Saha MT, Saha HH, Niskanen LK et al (2002) Time course of serum prolactin and sex hormones following successful renal transplantation. Nephron 92:735–737
Murray JE, Reid DE, Harrison JH et al (1963) Successful pregnancies after human renal transplantation. N Eng J Med 269:341–343
Davison JM, Baylis C (2002) Renal disease. In: De Swiet M (ed) Medical disorders in medical practice, 4th Edn edn. Blackwell Publishing, Malden, pp 198–266
Meier-Kriesche HU, Li S, Gruessner RW et al (2006) Immunosuppression: evolution in practice and trends, 1994–2004. Am J Transplant 6(5 Pt 2):1111–1131
Anderka MT, Lin AE, Abuelo DN et al (2009) Reviewing the evidence for mycophenolate mofetil as a new teratogen: case report and review of the literature. Am J Med Genet A 149A(6):1241–1248
Tang IY, Meier-Kriesche HU, Kaplan B (2007) Immunosuppressive strategies to improve outcomes of kidney transplantation. Semin Nephrol 27(4):377–392
Little MA, Abraham KA, Kavanagh J et al (2000) Pregnancy in Irish renal transplant recipients in the cyclosporine era. Ir J Med Sci 169(1):19–21
Mulcahy D, Garrett P, Hanson S et al (1986) Pregnancy following renal transplantation. Ir Med J 79(3):67–70
Sibanda N, Briggs JD, Davison JM et al (2007) Pregnancy after organ transplantation: a report from the UK transplant pregnancy registry. Transplant 83(10):1301–1307
Coscia LA, Constantinescu S, Moritz MJ, et al (2009) Report from the National Transplantation Pregnancy Registry: outcomes of pregnancy after transplantation. Clin Transpl. 2009:103-22
McKay DB, Josephson MA, Armenti VT et al (2005) Reproduction and transplantation: report on the AST consensus conference on reproductive issues and transplantation. Am J Transplant 5(7):1592–1599
Fichez A, Labrousse C, Fromajoux C et al (2008) Successful pregnancy outcome after in vitro fertilization in a pancreas-kidney recipient. Fertil Steril 90(3):849
Coscia LA, Cardonick EH, Moritz MJ et al (2003) Multiple gestations in female kidney transplant recipients maintained on calcineurin inhibitors. Am J Transplant 3(Suppl 5):1603–1663
Acknowledgments
Many thanks to all the women who participated in the study.
Conflict of interest
There are no conflicts of interests to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kennedy, C., Hussein, W., Spencer, S. et al. Reproductive health in Irish female renal transplant recipients. Ir J Med Sci 181, 59–63 (2012). https://doi.org/10.1007/s11845-011-0767-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-011-0767-4