Abstract
Background
The Irish childhood obesity epidemic, one of the highest ranking internationally, represents a major threat to public health. We sought to perform a retrospective observational study of a clinic based cohort of obese Irish children.
Methods
Clinical data relating to gender, age, height, weight, body mass index and blood pressure were analysed, from 206 children referred to a paediatric endocrine referral centre over a 15-year period for assessment of obesity.
Results
Younger patients tended to have a higher standardised body mass index at initial presentation; 92% of boys and 96% of girls referred were obese (age-related BMI ≥ 95th percentile). Boys (51%) and girls (49%) had initial blood pressure measurements in the hypertensive range. There was a correlation between the degree of obesity and systolic blood pressure, particularly in boys.
Conclusions
Obese Irish children present with significant long-term health risks, including hypertension at baseline.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity has become a major public health problem in Irish children. Recently, the National Survey of Children’s Dental Health found that between 4 and 11% of children aged between 4 and 16 years were obese [1]. These prevalence rates are amongst the highest in the world [2]. However, the clinical characteristics of obese Irish children are not well defined. We have recently shown that the degree of body fatness in this cohort correlates with insulin sensitivity and markers of liver steatosis [3]. Previous studies have suggested that obese children are at approximately a threefold higher risk for hypertension than non-obese children [4]. Our objective was to determine retrospectively the prevalence of high blood pressure readings within a cohort of Irish children who were referred to a paediatric endocrine clinic for evaluation of obesity. We sought to examine the relationship between the severity of obesity and the degree of blood pressure elevation. A further objective was to examine the relationship between the age of first referral to the clinic and the severity of obesity at initial presentation.
Methods
A retrospective analysis was conducted of clinical data from children who had been referred to the endocrine service of a paediatric tertiary referral centre in Dublin between 1990 and 2004, for assessment of obesity. The age at presentation, weight, height and blood pressure were recorded. All measurements were performed by one of two paediatric endocrine nurse specialists. Weight was measured using a Seca® scale, height with a Holtain® stadiometer and blood pressure was measured from the right arm with a Critikon Dynamap® oscillometric device. The departmental protocol was for three blood pressure measurements to be taken and the lowest one recorded, using an appropriate cuff size, after the child was sitting comfortably for 5 min. Growth charts published in 2000 from the Centre for Disease Control (CDC) were used to plot body mass index (BMI) against age in both sexes. Statistical software available on the CDC website was used to calculate percentile values and standard deviation scores (SDS) for BMI [5].
Standard deviation scores and percentile values for systolic and diastolic blood pressure (SBP and DBP) were derived from formulae published in the most recent report from the National High Blood Pressure Education Program Working Group [6]. Diagnostic thresholds defining elevated blood pressure were also obtained from this report. Descriptive statistics are presented as percentages and mean (with standard deviations). The relationship between age and BMI SDS was assessed using Spearman’s rank correlation. BMI SDS and SBP SDS were compared using Pearson’s correlation. Differences were considered statistically significant with P values < 0.05. The JMP® statistical package (SAS Institute, Version 5.1) was used in all statistical calculations.
This study was approved by the Ethics Committees of St James’s Hospital, Tallaght Hospital and Our Lady’s Hospital for Sick Children, Crumlin.
Results
Two hundred and six children (97 males and 109 females) between the ages of 2 and 18 years were referred to the paediatric endocrine service for evaluation of obesity between 1990 and 2004. The mean age of referral was 9.7 ± 3.7 years. Ninety-three percent of all patients referred (96% of girls and 92% of boys) were obese with a BMI ≥ 95th percentile for age and sex (or BMI SDS ≥ 1.645). The remaining patients were classified as overweight (BMI ≥ 85th percentile for age and sex or SDS ≥ 1.04). The mean BMI at referral was 29.2 ± 7.2 kg/m2 and the mean BMI SDS was 2.49 ± 0.71. Younger patients had significantly worse obesity at referral, with higher BMI SDS. Spearman’s correlation for age and BMI SDS was −0.51 in boys, −0.64 in girls and −0.59 in both groups combined (all P < 0.0001) as shown in Fig. 1.
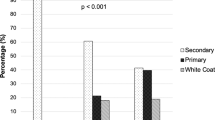
Blood pressure measurements were performed on 177 subjects at presentation (88 boys and 89 girls). Of these 51% of girls and 49% of boys had SBP readings in the hypertensive range (≥95th percentile for age, sex and height, or SDS ≥ 1.645). A further 9% of boys and 7% of girls had SBP in the pre-hypertensive range (≥90th percentile). Fewer patients had diastolic hypertension, with 8% of boys and 5% of girls exceeding the 95th percentile for DBP. A significant correlation was found between BMI SDS and SBP SDS in boys (Pearson’s correlation 0.29, P = 0.007) but not in girls (Pearson’s correlation 0.16, P = 0.13). For both groups combined, there was a Pearson’s correlation of 0.23, (P = 0.003,) as shown in Fig. 2. Diastolic blood pressure standard deviation scores did not correlate with BMI.
Discussion
The association between paediatric obesity and hypertension has been reported in numerous studies amongst a variety of ethnic and racial groups and virtually all have reported higher prevalence rates of hypertension in obese compared with lean children. In one American study, 33% of obese children were hypertensive compared with 11% of lean children [7]. In a cohort of Canadian children, BMI correlated with SBP and DBP in all age groups and systolic hypertension was prevalent in obese subjects from all age groups while diastolic hypertension was not [8].
This study in Irish children has found a very high prevalence of blood pressure measurements in the hypertensive range. These results cannot be directly translated into prevalence rates of hypertension, as this diagnosis requires elevated blood pressure readings on at least three occasions. A study of over 5,000 obese American children found that the prevalence of high-systolic blood pressure readings dropped from 38% on the first reading to 21 and 11% on the second and third readings, respectively [9]. Therefore, we expect that the rate of true hypertension in our cohort would be lower than the initial 50% measured.
Our finding that younger patients in our cohort had a significantly higher BMI SDS at the time of their initial presentation to the clinic suggests that the threshold for referral of very young children may be too high, or that obesity is under-recognised in this age group.
In conclusion, our study has demonstrated a clear and continuous increase in SBP SDS with increasing standardised BMI, particularly in boys, suggesting that obesity does not have a threshold effect on systolic blood pressure. Furthermore, a very high prevalence of hypertensive range systolic blood pressure levels were noted at presentation, which may represent a significant future cardiovascular risk burden. Prospective, repeated blood pressure measures and ambulatory haemodynamic monitoring would be useful in determining the true prevalence of hypertension in this cohort. Further studies might also be useful in clarifying the prognostic value and the optimal management of elevated blood pressure in obese children. Indeed, longitudinal studies are now confirming the association between childhood obesity and adult coronary heart disease risk [10].
References
Obesity—The policy challenges (2005) The report of the National Taskforce on Obesity: Department of Health and Children, Dublin, Ireland
Lissau I, Overpeck MD, Ruan WJ et al (2004) Body mass index and overweight in adolescents in 13 European countries, Israel, and the United States. Arch Pediatr Adolesc Med 158:27–33. doi:10.1001/archpedi.158.1.27
Finucane FM, Teong L, Pittock S et al (2008) Adverse metabolic profiles in a cohort of obese Irish children. Ann Clin Biochem 45:206–209. doi:10.1258/acb.2007.007115
Sorof J, Daniels S (2002) Obesity hypertension in children: a problem of epidemic proportions. Hypertension 40:441–447. doi:10.1161/01.HYP.0000032940.33466.12
An SAS Program for the CDC Growth Charts. URL: http://www.cdc.gov/nccdphp/dnpa/growthcharts/sas.htm. Accessed 18 Dec 2007
NHBPEP (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576. doi:10.1452/peds.114.2.S2.555
Sorof JM, Poffenbarger T, Franco K, Bernard L, Portman RJ (2002) Isolated systolic hypertension, obesity, and hyperkinetic hemodynamic states in children. J Pediatr 140:660–666. doi:10.1067/mpd.2002.125228
Paradis G, Lambert M, O’Loughlin J et al (2004) Blood pressure and adiposity in children and adolescents. Circulation 110:1832–1838. doi:10.1161/01.CIR.0000143100.31752.B7
Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ (2004) Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics 113:475–482. doi:10.1542/peds.113.3.475
Baker JL, Olsen LW, Sorensen TI (2007) Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med 357:2329–2337. doi:10.1056/NEJMoa072515
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Finucane, F.M., Pittock, S., Fallon, M. et al. Elevated blood pressure in overweight and obese Irish children. Ir J Med Sci 177, 379–381 (2008). https://doi.org/10.1007/s11845-008-0228-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-008-0228-x