Abstract
Introduction
Fractured neck of femur in osteogenesis imperfecta is rarely reported. Its management is always difficult because of bone fragility and the outcome is not well known. We, therefore, aimed to study the management pitfalls in this group of patients.
Methods
We retrospectively reviewed five cases of fractured neck of femur in four patients treated in our hospital between 2006 and 2009. The demographic data, mode of injury, fracture configuration, treatment, complications, clinical and radiological outcome were reviewed.
Results
According to the Sillence classification, one patient was type I, two were type III and one was type IV. There were two children (aged 8 and 15 years) and two adults (aged 21 and 22 years), with the 8 year-old girl suffering from hip fracture on different sides in two accidents. All five hip fractures were the result of low-energy injury and were associated with other fractures. Two undisplaced fractures required intra-operative fluoroscopic confirmation to demonstrate movement at the fracture site. The interval between the injury and fixation ranged from 6 h to 3 days. One hip required secondary surgery to openly reduce the fracture due to inadequate primary fixation and reduction. Two hips were fixed with paediatric dynamic hip screws and three hips were fixed with cannulated screws. All patients were immobilised in hip spica for 6 weeks. The average follow-up was 4 years (3–5 years). All patients had satisfactory union and none of them developed radiological evidence of avascular necrosis at the latest follow-up. All patients returned to their pre-injury functional level.
Conclusion
Fractured neck of femur is rare given the high prevalence of long bone fractures in osteogenesis imperfecta. They all have characteristic associated fractures of the extremity at the time of injury and neck of femur fractures could be easily missed. Fracture fixation is a great challenge to the orthopaedic surgeons because of the small size of the patients, poor bone quality with suboptimal imaging intra-operatively and compromised purchase of fixation devices. The choice of implants should be determined by the size of the patients and the presence of prior instrumentation close to the hip joint.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteogenesis imperfecta (OI) is a life-long genetic disorder characterised by fractures after minimal or absent trauma, dentinogenesis imperfecta and, in adult years, hearing loss. The clinical features of OI span a spectrum of disease from the most severe form with perinatal lethality, severe skeletal deformities, mobility impairments and very short stature to nearly asymptomatic individuals with a mild predisposition to fractures, normal stature and normal life span. Either end of the spectrum (types I and II) requires minimal treatment, while those who fall in the middle (types III and IV) require the most medical attention [1]. These patients may develop repeated fractures very early in life as a result of poor bone quality. The bone quality is compromised due to thin shelled-out cortices, osteoporosis and poor regeneration after fractures. Medical management using bisphosphonates have certainly decreased the fracture risk of long bones [2, 3] and, thereby, reducing outpatient department consultations and operative interventions [4]. However, the number of fractures per child is still very high.
The femur is the most common bone that requires surgical correction in OI as a result of fractures and progressive deformities [5, 6]. The femoral midshaft appears to be the most common site [7]. However, fractures of the neck of femur are relatively uncommon, and the reason for this is still unknown. Fixation of these fractures is made difficult either by hardware from previous fracture fixations or by the presence of an intra-medullary (IM) rod used for stabilisation of the femoral shaft. Very few cases have been reported in the literature concerning fractures of the neck of femur in OI patients in the presence of previously inserted implants and their long-term outcome. We would like to highlight the surgical challenges in managing this life-long brittle bone disease.
Materials and methods
We retrospectively reviewed five fractures of the neck of femur in four patients treated in our hospital between the years 2006 and 2009. All of the patients had been diagnosed with OI since childhood and had been classified according to the Sillence classification. A summary of all cases can be found in Table 1.
Case 1
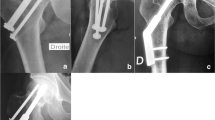
An 8-year-old girl with type IV OI sustained a fracture in the inter-trochanteric region of the left femur following a fall at home. Intra-operatively, a subcapital fracture of the neck of the same femur was noted during X-ray screening of the hip joint (Fig. 1a). A decision to fix both the neck and inter-trochanteric fractures with a paediatric dynamic hip screw (DHS) was made. Placement of the DHS was technically difficult due to a short and narrow neck of femur. She was placed in a hip spica post-operatively for 6 weeks.
a Patient 1 with both fracture of the neck of the left femur and inter-trochanteric fracture of the left femur. b The fractures at the left femur were treated by a dynamic hip screw (DHS) but then the patient suffered from a fracture in the neck of the right femur after another trivial fall. The fracture was not obvious but was confirmed by intra-operative X-ray examination. c The fracture of the neck of right femur was fixed by a DHS. An anti-rotation K-wire was inserted proximally to prevent rotation of the head of femur during the insertion of the hip screw
Unfortunately, she had another injury 3 months after the first fracture. This time, she sustained a fracture in the supracondylar region of the right distal femur after a trivial fall. During pre-operative assessment, she complained of having concomitant pain in the right groin. Initial X-rays did not show any fracture in the neck of femur (Fig. 1b). However, on intra-operative X-ray screening, a fracture of the neck of the right femur was found. This fracture was fixed by a paediatric DHS (Fig. 1c) and was protected by a hip spica cast for 6 weeks. Both fractures healed uneventfully at 10 weeks. She was then protected further with a hip spica brace.
Case 2
A 22-year-old female, with type III OI, injured herself after falling from her wheelchair. She sustained a trans-cervical fracture of the right femur and a supracondylar fracture of the left distal femur. She had been previously treated with a valgus osteotomy of the right hip for coxa vara at the age of 12 years, which was fixed with a paediatric DHS. This trans-cervical fracture occurred at the tip of the DHS lag screw (Fig. 2a). The fracture was first stabilised prior to removal of the DHS by placing one cannulated cancellous screw proximal to the DHS lag screw. Another cancellous screw was then inserted after the DHS screw was removed to ensure good stability, despite the large void remaining after removal of the DHS (Fig. 2b). The supracondylar fracture of the left femur was treated with cross K-wire fixation. She was immobilised in a hip spica for 6 weeks and both fractures united in 8 weeks. In her third-year follow-up, she was found to have persistent right hip abductor weakness. We want to ensure that there is no avascular necrosis (AVN) of the femoral head by serial radiographs before planning future corrective osteotomy.
Case 3
A 15-year-old boy with type I OI came to the casualty department after sustaining a fracture of the neck of the right femur and a fracture of the right humerus after a trivial fall (Fig. 3a). He had previous lower limb fracture requiring deformity correction with a modified Sofield–Millar operation and fixation by IM Rush pin in his femurs. The displaced subcapital fracture was treated promptly within 6 h of injury with closed reduction and fixation with two 4.5-mm cannulated cancellous screws. The hip was immobilised in a hip spica cast for 6 weeks. The reduction was satisfactory intra-operatively and during the early post-operative period. However, the reduction was lost at about week 3 after injury, resulting in coxa vara (Fig. 3b). The humerus fracture was treated with IM K-wire fixation.
a Displaced fracture of the neck of the right femur. b The fracture was fixed with two 4.5-mm cancellous screws and further immobilised in hip spica. The pre-existing intra-medullary (IM) rod and narrow shaft of the femur made insertion of the additional screw difficult. Further insertion of a third screw might compromise the cortical stability, since all screws would be inserted very close together. The intra-operative radiograph showed satisfactory alignment (left). However, the alignment was lost despite being immobilised in a hip spica cast, resulting in coxa vara (right)
Due to the very narrow proximal femur in the lateral view with much of the space being occupied by the IM Rush pin, both screws were inserted from the anterior surface of the proximal femur. An additional screw to be inserted posterior to the IM nail was considered too dangerous, as it may have weakened the already narrowed neck, resulting in fracture through the implants. The fixation with the two anterior screws proved to be suboptimal and coxa vara subsequently developed. Both fractures united at the end of 3 months.
Case 4
A 21-year-old lady with type III OI sustained an undisplaced trans-cervical fracture of the left neck of femur and a supracondylar fracture of both femurs after a fall at home (Fig. 4a). She had previous lower limb fracture requiring deformity correction with a modified Sofield–Millar operation and fixation by IM Rush pin in her left femur. She was treated on the same day by in situ fixation of the fractured neck of femur by cannulated cancellous screws (Fig. 4b) and the supracondylar fracture by crossed K-wires. She was subsequently immobilised in a hip spica cast. Problems were encountered intra-operatively due to suboptimal positioning of the patient due to an ipsilateral fracture of the distal femur and difficulty in the assessment of the screw due to poor bone quality.
a Fracture of the neck of the left femur (arrow). b The fracture was fixed with two cancellous screws, but the position was difficult to be confirmed intra-operatively due to limitations in the positioning of the hip joint. c The screw fixation was lost and the femoral head was displaced anteriorly (left). The fracture was revised by open reduction followed by additional screw fixation (middle). There was no sign of avascular necrosis (AVN) 4 years after the injury (right)
Unfortunately, subsequent X-rays taken after 3 days revealed displacement of the fracture in the left hip. The patient was treated with open reduction and additional screw fixation, followed by hip spica immobilisation (Fig. 4c). Her fracture ultimately united at 3 months without any deformity.
Results
All of the fractures occurred after trivial injuries in the form of slips and falls on level ground or falls from a wheelchair. All patients had OI and were subdivided according to the Sillence classification; one patient was type I OI, two were type III and one was type IV. Out of the four cases, two cases fractured the neck of femur during adulthood and the other two happened during childhood; three were females and one was male. All had undisplaced fractures of the neck of femur, except one patient who had a displaced fracture. Of the total of five hips with fractures of the neck of femur, two fractures were trans-cervical, while three were subcapital. The time from admission to surgery ranged from 6 h to 3 days.
All of the fractures were treated by the same surgeon. All fractures were treated by closed reduction, as they were all undisplaced. Case 4 required open reduction after the fracture was found to have displaced. Fractures were fixed by DHS or cannulated cancellous screws. All cases had associated fractures elsewhere, which required fixation by K-wires. Post-operative immobilisation was achieved by hip spica casts for 5–6 weeks. Similar to other series in the literature, the time required for union of the fractures was an average of 3 months. All four patients required further protection afterwards with night time bracing. By 2 years follow-up, all had regained their pre-operative ambulatory status (Table 1). There was no obvious radiological evidence of AVN in any of the femoral heads and all joints remained congruent at the latest follow-up radiographs. Only case 3 had significant coxa vara at the latest follow-up. There was no infection, non-union or neurovascular injury in any of the patients. The average follow-up was 4 years, ranging from 3 to 5 years.
A summary of the results can be found in Table 1.
Discussion
OI, a disorder causing increased bone fragility, is a common cause of pathological fracture and long bone deformity. Pathological fractures have, subsequently, become one of the most common reasons for disability and impairment of function in these patients. IM rodding has been proven to be safe and effective in fracture fixation and deformity correction in patients with OI [8–10]. Fractures of the neck of femur are very rare in OI and are seldom reported in the literature. Therefore, the exact incidence of these fractures is unknown. Not to mention, there is little information on its management and the long-term outcome. We have performed an English literature search from 1980 to 2012 using the PubMed database in our review. We first used the keywords of osteogenesis imperfecta, fracture neck of femur/hip for the search. We found only five papers. We then searched using the keywords of pathological fracture of neck of femur/hip. We found only one related article. We have summarised all the six English literatures [11–16] available regarding fractures of the neck of femur in patients with OI (Table 2). Furthermore, only a few studies had detailed documentation of the treatment methods and outcome. The reason for the difference in fracture rates in the femoral neck compared to other parts of the femur is unclear.
Fractures of the neck of femur in healthy children are also rare [17]. They are usually caused by high-energy trauma and are highly associated with complications, e.g. AVN, coxa vara, premature physeal closure, limb length discrepancy and non-union. The incidence of AVN varies from 13 to 45 % [11, 18–20]. All hip joints from our series remained congruent post-operatively and none of the fractures developed AVN. This finding is consistent with other cases reported in the literature. We believe that none of our patients developed AVN because all of them sustained relatively low-energy trauma, which managed to preserve the soft tissues and, thus, the blood supply around the neck of femur. This probably explained why patient 2 did not develop any AVN despite being treated 3 days after the injury. Furthermore, in our series, all fractures were undisplaced, except for case 3, who was treated promptly within 6 h of injury. Unfortunately, case 3 developed subsequent coxa vara after fixation. Increased coxa vara after fractures of the neck of femur in normal children is associated with poor functional outcome [21]. The prevalence of coxa vara was reported to be about 20–30 % [18, 19, 22, 23]. The possible causes of his coxa vara will be explored later in the discussion.
Our series, with a total of five hips with fractures of the neck of femur, is the largest series of patients with OI reported so far in the literature with detailed documentation. From our series, several common diagnostic pitfalls and therapeutic challenges can be identified.
Diagnostic difficulties
Fractures may not be obvious on pre-operative X-rays. Clinical suspicion must remain high in any patient with OI complaining of groin or hip pain after a trivial injury. In cases 1 and 2, fractures through the neck of femur were not readily seen on plain X-rays and were only discovered clearly during intra-operative X-ray screening.
To make things more complicated, these patients often present with multiple sites of injury. More attention will naturally be paid to those fractures with obvious displacement or those which can be easily seen on plain X-rays. In our series, all patients had associated injuries to either the same bone or other bones. Fractures on the ipsilateral bone may also limit proper positioning of the patient intra-operatively. This was seen in case 4, where the loss of reduction may have been caused by suboptimal internal fixation as a result of poor bone quality combined with compromised radiological assessment intra-operatively due to an ipsilateral distal femur fracture.
Pre-existing implants
As seen in all of our cases, the femoral neck fractures consistently occurred just proximal to any pre-existing IM rods or DHSs. The insertion of the implants increases the stiffness of the shaft of femur [24], hence, producing areas of high stress concentration at the neck of femur, leading to insufficiency fractures [25–27]. This is consistent in nearly all existing cases found in the literature. In a case report by Chung et al. [13], the authors found a fracture in the neck of femur in an adult female who already had an IM nail in situ. The fracture was fixed with cannulated cancellous screws, with the aid of a navigation system to guide the entry point. Another case series reported by Tsang and Adedapo [12] presented two cases with fractured neck of femur in patients with OI. In both cases, difficulty was encountered during fixation of the fractures due to the presence of pre-existing IM rods. This problem was seen in case 3 of our series, where additional screws could not be inserted due to a pre-existing IM Rush pin. This suboptimal fixation, combined with poor bone quality, subsequently led to coxa vara when the fracture healed. In retrospect, a larger lag screw should also have been inserted if possible, but the screw entry sites would have to be placed medial to the IM Rush pin. This would potentially create a stress riser at the space between the IM Rush pin and the screw entry sites. The surgical correction of the coxa vara is very challenging using the commonly used plating system because of the stress riser’s effect on the fragile bone. To overcome this problem, Fassier et al. [28] used Kirschner wires to supplement the IM nail after the valgus osteotomy in correcting the coxa vara in patients with OI.
While statistics show that femoral fractures most commonly occur in the shaft, one must be vigilant in screening for fractures through the neck of femur, especially in patients who have had previous internal fixation devices inserted into the shaft of the femur.
Structural abnormalities and distortion
Pre-existing anatomical abnormalities in OI patients, including the presence of short and narrow necks, create challenges in the imaging and management of these fractures. Even seemingly simple tasks of determining the orientation of the fracture line and confirming fracture reduction on X-rays can be very difficult in such distorted anatomy with severe osteopaenia. We agree with Tsang and Adedapo [12] that the surgery needs to be done by freehand without traction. In all of our cases in this series, we did not use a traction table because of bone fragility, concomitant fractures and relatively small body size. As a result, we rely on the cross-table lateral fluoroscopy in assessing the lateral position of the hip. Unfortunately, the overlapping soft tissue shadow and osteopaenia make the images very hard to interpret. The frog lateral position is not an option in our patients because of the fracture and pre-existing hip deformities that have already limited motion. The suboptimal fixation also limits the use of frog lateral radiography to assess the screw position after implant insertion.
Another observation from our cases is that, apart from case 1, all patients had deformities in the hips even before the fracture, e.g. acetabular protrusio and coxa vara. Whether or not these have compromised the range of motion of the hips and contributed to the fractures after the fall have yet to be proven.
Bone fragility and implant fixation
Finally, there are the challenges of providing adequate fixation to fractures in bones that are brittle, thin and may already have implants that may require removal. On one hand, there are the challenges of circumventing previous implants if one decides to retain them. This can be seen in cases 2 and 3, in which screws had to be passed around IM devices. Naturally, the margin of error for the entry site of such screws is very narrow in such fragile bone.
On the other hand, there are the challenges of removing existing implants and then trying to provide stable fixation in the remaining porotic bone. In case 2, the large void from the DHS lag screw left little bone to provide good purchase of the cancellous screws. One trick devised to prevent collapse of the fracture upon removal of the DHS was to first insert a screw just proximal to the lag screw to stabilise the fracture. However, one must always be wary of the poor bone quality, even if there are no pre-existing implants in the bone. Case 4 demonstrated the hazards of early implant failure even after seemingly adequate stability achieved during the first operation. Care must also be taken when attempting to revise the screws, as repeated screw insertion would further compromise the bone stock.
Bone plating in patients with OI has been shown to have many complications [29] because it can act as a stress riser in osteopaenic bone. In general, we try to avoid plating in treating fractures in OI. We also do not routinely remove the implants since the bone defects, after the removal of the implants, will act as stress risers, leading to fracture. Immobilisation of the bones after the removal of implants will weaken the already osteopaenic bone further.
Conclusion
Fractures in the neck of femur in patients with osteogenesis imperfecta (OI) are relatively rare given the high prevalence of long bone fractures. Most of our patients have pre-existing implants and they likely act as stress risers to the neck of femur at the time of injury. Furthermore, all of them have associated fractures of the lower extremity at the time of injury, so the femoral neck fracture may be easily missed. As more patients are now rodded, their effects on the neck of femur should not be under-estimated, even they have reached skeletal maturity. Lastly, fracture fixation is a great challenge to the orthopaedic surgeon due to poor bone quality, suboptimal imaging pre- and post-operatively, pre-existing implants and compromised purchase of fixation devices. The importance of pre-operative planning cannot be understated.
References
Sillence DO, Senn A, Danks DM (1979) Genetic heterogeneity in osteogenesis imperfecta. J Med Genet 16(2):101–116
Sakkers R, Kok D, Engelbert R, van Dongen A, Jansen M, Pruijs H et al (2004) Skeletal effects and functional outcome with olpadronate in children with osteogenesis imperfecta: a 2-year randomised placebo-controlled study. Lancet 363(9419):1427–1431
DiMeglio LA, Ford L, McClintock C, Peacock M (2004) Intravenous pamidronate treatment of children under 36 months of age with osteogenesis imperfecta. Bone 35(5):1038–1045
de Graaff F, Verra W, Pruijs JE, Sakkers RJ (2011) Decrease in outpatient department visits and operative interventions due to bisphosphonates in children with osteogenesis imperfecta. J Child Orthop 5(2):121–125
Mulpuri K, Joseph B (2000) Intramedullary rodding in osteogenesis imperfecta. J Pediatr Orthop 20(2):267–273
Karbowski A, Schwitalle M, Brenner R, Lehmann H, Pontz B, Wörsdörfer O (2000) Experience with Bailey–Dubow rodding in children with osteogenesis imperfecta. Eur J Pediatr Surg 10(2):119–124
Wolf H, Sarahrudi K, Vécsei V (2009) Intramedullary osteosynthesis for fracture associated with osteogenesis imperfecta. Injury 40(3):315–320
Ruck J, Dahan-Oliel N, Montpetit K, Rauch F, Fassier F (2011) Fassier–Duval femoral rodding in children with osteogenesis imperfecta receiving bisphosphonates: functional outcomes at one year. J Child Orthop 5(3):217–224
Li YH, Chow W, Leong JC (2000) The Sofield–Millar operation in osteogenesis imperfecta. A modified technique. J Bone Joint Surg Br 82(1):11–16
Pichard CP, Robinson RE, Skolasky RL, Fedarko NS, Leet AI (2009) Surgical blood loss during femoral rodding in children with osteogenesis imperfecta. J Child Orthop 3(4):301–305
Azouz EM, Karamitsos C, Reed MH, Baker L, Kozlowski K, Hoeffel JC (1993) Types and complications of femoral neck fractures in children. Pediatr Radiol 23(6):415–420
Tsang KS, Adedapo A (2011) Cannulated screw fixation of fracture neck of femur in children with osteogenesis imperfecta. J Pediatr Orthop B 20(5):287–290
Chung FC, Wai CK, Koon WM (2008) A case of screw fixation of femur neck fracture with the use of computer navigation in a woman with osteogenesis imperfecta. J Trauma 65(5):1168–1170
Livesley PJ, McAllister JC, Catterrall A (1994) The treatment of progressive coxa vara in children with bone softening disorders. Int Orthop 18(5):310–312
Shrader MW, Schwab JH, Shaughnessy WJ, Jacofsky DJ (2009) Pathologic femoral neck fractures in children. Am J Orthop (Belle Mead NJ) 38(2):83–86; discussion 86
Nayeemuddin M, Higgins GA, Bache E, O’Hara J, Glitheroe P (2009) Complication rate after operative treatment of paediatric femoral neck fractures. J Pediatr Orthop B 18(6):314–319
Ratliff AH (1962) Fractures of the neck of the femur in children. J Bone Joint Surg Br 44-B:528–542
Canale ST, Bourland WL (1977) Fracture of the neck and intertrochanteric region of the femur in children. J Bone Joint Surg Am 59(4):431–443
Morsy HA (2001) Complications of fracture of the neck of the femur in children. A long-term follow-up study. Injury 32(1):45–51
Kay SP, Hall JE (1971) Fracture of the femoral neck in children and its complications. Clin Orthop Relat Res 80:53–71
Eberl R, Singer G, Ferlic P, Weinberg AM, Hoellwarth ME (2010) Post-traumatic coxa vara in children following screw fixation of the femoral neck. Acta Orthop 81(4):442–445
Lam SF (1971) Fractures of the neck of the femur in children. J Bone Joint Surg Am 53(6):1165–1179
Hughes LO, Beaty JH (1994) Fractures of the head and neck of the femur in children. J Bone Joint Surg Am 76(2):283–292
Kiely N (2002) Mechanical properties of different combinations of flexible nails in a model of a pediatric femoral fracture. J Pediatr Orthop 22(4):424–427
Kitajima I, Tachibana S, Mikami Y, Mori T, Hirota Y, Nakamichi K (1999) Insufficiency fracture of the femoral neck after intramedullary nailing. J Orthop Sci 4(4):304–306
Patton JT, Cook RE, Adams CI, Robinson CM (2000) Late fracture of the hip after reamed intramedullary nailing of the femur. J Bone Joint Surg Br 82(7):967–971
Evans A, Gabbar OA, Furlong AJ (2007) Fractured neck of femur in a child after femoral fracture fixation by intramedullary flexible nails: a case report. J Pediatr Orthop B 16(1):53–55
Fassier F, Sardar Z, Aarabi M, Odent T, Haque T, Hamdy R (2008) Results and complications of a surgical technique for correction of coxa vara in children with osteopenic bones. J Pediatr Orthop 28(8):799–805
Enright WJ, Noonan KJ (2006) Bone plating in patients with type III osteogenesis imperfecta: results and complications. Iowa Orthop J 26:37–40
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Chow, W., Negandhi, R., Kuong, E. et al. Management pitfalls of fractured neck of femur in osteogenesis imperfecta. J Child Orthop 7, 195–203 (2013). https://doi.org/10.1007/s11832-013-0495-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-013-0495-6