Abstract
Purpose
Missed Monteggia fracture dislocation in children is a serious condition. The treatment of this rare condition is controversial and reports on the long-term outcome are sparse. We present a series of patients treated with open reduction and ulnar osteotomy with a mean long-term follow-up of 8 years (range 3–17).
Methods
All 16 patients had Bado type 1 (anterior radial head) dislocation. The mean delay from injury to surgery was 17 months (range 1–83). Bilateral radiographs, Oxford Elbow Score, strength measurements, and range of motion were obtained in all patients.
Results
There were no major complications to surgery. The radiographic results showed ten patients with reduction of the radial head and with no arthrosis, four patients with arthrosis or subluxation, and two patients with a dislocated radial head. We found a significant correlation between radiographic outcome and delay to ulnar osteotomy (P = 0.03). Typical clinical findings were a small but significant extension deficit and mean loss of supination of 10° (range 0–90, P < 0.01). Ligament reconstruction or transfixation of the radial head did not influence the radiographic or clinical outcome.
Conclusions
Case reports of similar patients treated conservatively demonstrate high morbidity, and, therefore, open reduction and ulnar osteotomy seemed justified. However, this study underlines the importance of minimizing the delay between injury and ulnar osteotomy. If surgery is performed within 40 months after injury, good to fair long-term radiographic results can be obtained. Open reduction and ulnar osteotomy were performed because patients treated conservatively demonstrate high morbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The management of missed Monteggia fracture equivalent in children with radial head dislocation and ulnar bowing is controversial, and long-term results after surgical treatment are sparse [1, 2]. Also, no controlled randomized trials exist due to the rarity of the condition. Treatment options are many, ranging from nonsurgical treatment [3] to ligament reconstruction and osteotomies [1, 2, 4–14]. Most commonly, a proximal ulnar osteotomy, as first described by Bouyala et al. [15, 16] is performed in order to correct the angulation of the ulna, but some authors recommend osteotomy at the site of the deformity of the ulna [2, 6, 7]. Ulnar elongation [1, 10] or shortening of the radius [4, 7] is advocated if overgrowth of the radius is present because of long-term dislocation.
If this condition is left untreated, the function of the elbow may be impaired. A few cases of untreated dislocations have been published [11, 17–19], and many of these patients experience pain, instability, deformity, and loss of strength and range of motion in adult life. Moreover, neuropathy of the ulnar or radial nerve seems to be a frequent late complication [17].
The current opinion is that these lesions should be surgically treated because of the poor long-term outcome of conservative treatment and because many children have pain or other problems at the time of diagnosis. In recent study by Nakamura et al. [1], as many as 60% of patients complained of pain preoperatively and 50% had decreased range of motion.
However, several factors influence the outcome after surgery, and all patients may not benefit from surgical treatment because surgery has many potential complications [4]. If the radial head remains dislocated, it gradually becomes hypertrophic, and the concavity of the head is lost [20]. Therefore, delay to surgery seems to influence the outcome because the joint becomes incongruent, and there is lengthening of the radius. The incongruent joint may remodel as the joint surfaces adapt to each other during growth after reduction. Surgery in the adolescent with a hypertrophic radial head may, therefore, carry a poor prognosis because the potential for remodeling is small [11].
Since 1989, we have used open reduction with ulnar proximal osteotomy as the treatment for missed Monteggia equivalents. Surgery was performed by only two surgeons. The treatment algorithm did not change, but there were some differences in the surgical technique between surgeons. We present our experience after open reduction and proximal ulnar osteotomy in a consecutive series of 16 patients evaluated retrospectively, with a mean follow-up of 8 years. To our knowledge, this is the longest clinical and radiographic follow-up yet published.
Patients and methods
All skeletally immature patients treated at our hospital with missed Monteggia fracture dislocation since 1989 were selected for follow-up. All patients were referred from other hospitals for treatment at our department and had a plastic deformation of the ulna and an anterior dislocation of the radius (Bado type 1) [21]. Patients with congenital dislocation, multiple exostoses, or Marfan syndrome were excluded. This left us with 17 patients who were offered a follow-up clinical examination, strength measurement, and radiographic examination. In addition, an Oxford Elbow Score was obtained. One patient was abroad and did not wish to participate in the study. She had had a 12-month delay before surgery. At the age of 10 years, she had a severe valgus deformity and a hypertrophic radial head, and proximal ulnar osteotomy was performed with pinning of the radial head. At follow-up 3 years postoperatively, she had mild pain and a radiographic subluxation of the radial head.
Preoperative data on the 16 patients who participated in the follow-up are shown in Table 1.
Clinical examination included measurement of the range of motion and carrying angle with a handheld goniometer. The maximal circumferences of the forearm and the humerus were also measured.
Strength measurement was performed with an Isobex apparatus (Medical Device Solutions AG, Oberburg, Switzerland), which is a validated [22], handheld dynamometer designed for the measurement of muscular strength. Static strength was recorded in extension, flexion, supination, and pronation. The sampling interval was 3 s and measurements were repeated three times at short intervals in each direction. Only the maximal strength was recorded. Both the injured and the healthy arm were tested for comparison.
Radiographic examination in the anterior–posterior and lateral planes was performed at follow-up. Subluxation was present if there was contact between joint surfaces without complete reduction. Complete reduction was present if a line drawn through the center of the radius passed through the middle third of the capitellum on the lateral projection [1]. The radiographs were scored according to Nakamura et al. [1]. Good results were complete reduction of the radial head without osteoarthritic changes and fair results were radial subluxation or osteoarthritic changes. A poor result was dislocation of the radial head. Radiographs were evaluated by three of the authors independently, and there were no disagreements as to scores. We defined radial head hypertrophy according to the method of Kim et al. [20]. Hypertrophy was present if the diameter of the widest portion of the proximal metaphysis was 1.5 times greater than the diameter of the narrowest portion of the neck just proximal to the bicipital tuberosity in either the lateral or the anterior–posterior projection.
The Oxford Elbow Score was used to assess the patient-reported outcome and is based on a questionnaire with 12 items with five response options. Items are divided into three domains: “elbow function”, “pain”, and “social-psychological” [23, 24]. Each domain ranges from 0 to 100, where 100 is the best outcome.
Surgery was performed by one of two surgeons. Open reduction and ulnar osteotomy were done in all cases with an open-wedge technique through a Boyd incision. In all cases, remnants of the annular ligament and fibrous tissue were removed from the joint in order to facilitate reduction. The osteotomy was performed at the level of the ulnar tuberosity. The ulna was flexed until reduction of the radiocapitellar joint was obtained. The osteotomy was not bone grafted. A stability test was performed by a simple pronation of the forearm in a 90° flexed elbow. If the radial head dislocated during this pronation test, it was judged to be unstable and a further opening of the osteotomy was done until a stable position was present in both full supination and pronation. We did not find the need for notchplasty in any patient [20]. One of the treating surgeons preferred to use the remnants of the annular ligament for ligament reconstruction, while the other surgeon chose to remove the remnants. The osteotomy was fixed with either a Steinmann pin or a plate. A supplementary transfixation of the radius was performed with a K-wire through the capitellum if, during surgery, the surgeon judged that the reduction was unstable. In one case, transfixation was performed because post-operative radiographs revealed subluxation in the radiocapitellar joint. The arm was immobilized with a cast for 6 weeks after surgery.
Ethical considerations
All patients were informed that the follow-up was performed with the intention of publication, and all patients gave consent prior to the examination. The Local Ethics Committee was informed about the project, but the study was regarded as a quality control investigation and approval was not needed.
Statistics
Interquartile ranges are given in brackets if the median values are used, and if the mean values are used, standard deviations (SDs) are given. Means were compared by an unpaired t-test if the test for normality was passed. If not, then the Mann–Whitney rank sum test was applied. For paired data, a paired t-test or the Wilcoxon signed-rank test was used. Spearman’s rank order correlation was used for correlations.
Results
There were no infections, nerve palsies, or other complications after surgery according to the patient records. Two patients had subluxation of the radial head on the postoperative radiograph. One patient (Case 1) was treated with a closed reduction and percutaneous transarticular pinning of the radial head. Closed reduction was not successful in Case 3. An open reduction was performed 3 days after surgery, and interposed soft tissue was removed from the joint (Table 2). Hereafter, stable reduction was obtained. The mean follow-up was 8 years, ranging from 3 to 17.5 years, and the outcomes at follow-up are summarized in Table 3.
Oxford Elbow Score
The mean function score was 92 (SD 9), the mean social/psychological score 83 (SD 14), and the mean pain score was 88 (SD 15). There was no significant correlation between the Oxford Elbow Score and delay to ulnar osteotomy or age at surgery.
Radiology
The mean radiographic score was 1.5, ranging from 1 to 3. Seven patients had radial head hypertrophy. These patients had a radiographic score of more than 1, except for one case. Even though this patient (Case 4) had a radiographic score of 1, the general outcome was good. Two patients (Cases 5 and 7) had redislocation of the radial head and severe radial head hypertrophy. Four patients (Cases 11, 12, 13, and 15) had, in addition to the hypertrophy, slight to moderate osteoarthritic changes in the elbow joint. One of these patients (Case 12) also had a radial head subluxation. Hourglass constriction of the radial neck as described by Rodgers et al. [4] was not seen.
Age at surgery and delay from injury seemed to influence the radiographic outcome (Fig. 1). We found a significant correlation between radiographic outcome and delay to ulnar osteotomy (P = 0.03), and the radiographic score was good in all patients treated before the age of 8 years. There was no significant correlation between age at surgery and radiographic outcome or the Oxford Elbow Score.
Scatterplot showing the relationships between the radiographic score at the time of follow-up, interval between injury and the ulnar osteotomy, and the age at the time of operation. A good radiographic result was a complete reduction and no osteoarthritic changes, and a fair result was a radial head subluxation or osteoarthritic changes. Radial head dislocation was considered a poor result
Clinical examination
On clinical examination, the most prevalent finding was a significant decrease in supination and extension compared with the contralateral arm (Table 3). Flexion and supination strength were significantly decreased in the affected arm. In none of the patients with a fully reduced radial head was there an increase in valgus. In contrast, the two patients with secondary dislocation of the radial head had an increase in the carrying angle of 25° (Case 7) and 5° (Case 5) compared with the contralateral elbow.
Two additional patients (Cases 12 and 11) had more than 5° excessive valgus at follow-up. Case 13 had 12 ° of excessive valgus and a subluxation of the radial head. Case 11 is described in detail below.
The maximum circumference of the brachium of the affected arm was 0.4 cm less (P = 0.07) than that of the contralateral arm and 0.2 cm less than that of the antebrachium (P = 0.29).
Effect of the surgical technique
Ligament reconstruction was performed in 10 of 16 patients. The primary operation was open reduction and ligament reconstruction without osteotomy in two patients (Cases 15 and 16). This was done 7 and 3 months after the initial injury (Table 2) and ulnar osteotomy was done 5 and 15 months later because of subluxation after the primary procedure, respectively. The radiographic score was 1 (1–2) in patients with ligament reconstruction and 1.5 in those without (1–2) (P = 0.55). Pain scores were 95 (80–100) and 90 (85–100) (P = 0.78), respectively. Thus, ligament reconstruction did not markedly affect the radiographic or pain score.
Ulnar osteotomy was fixed with either a Steinmann pin at the osteotomy site or a small fragment plate. All osteotomies healed uneventfully regardless of the choice of fixation and had signs of radiographic healing 6 weeks after surgery.
Transarticular fixation of the radial head was performed in 7 of 16 patients, but did not seem to affect the outcome. No complications, such as the breakage of K-wires, were recorded. The radiographic score in these patients was 1 (1–1.75) compared with 1 (1–2.25) in the group without a transarticular K-wire (P = 0.50), and the pain scores were 100 (86–100) and 90 (80–95), respectively (P = 0.29).
Case 11
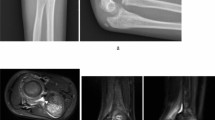
This patient had a proximal ulnar osteotomy in her left arm at the age of 11 years, with a delay of 4 years since the initial injury. Her complaints before surgery were intermittent pain and decreased range of motion. Her carrying angle was 15° before osteotomy. The proximal ulnar osteotomy was fixed by a Steinmann pin, which was removed along with the cast after 6 weeks. Ligament reconstruction was not performed. At the age of 20 years, she had a resection of the radial head because of pain due to osteoarthritic changes in the radiohumeral joint (Fig. 2a–f). She was seen at follow-up 1 year after radial head resection (Fig. 3). She had a slight increase in valgus compared with the contralateral arm, a normal range of movement, and an excellent Oxford Elbow Score (Table 2).
Selected radiographs of Case 11. a Anterior–posterior (AP) projection of the elbow 6 weeks after ulnar osteotomy with good placement of the Steinmann pin and with reduction of the radial head. b Lateral projection of the elbow 6 weeks after ulnar osteotomy with good placement of the Steinmann pin and with reduction of radial head. There is callus formation around the osteotomy. c AP projection 8 years after proximal ulnar osteotomy with arthritic changes in the joint. d Lateral projection 8 years after proximal ulnar osteotomy with arthritic changes in the joint and radial head hypertrophy. e AP projection of the elbow at follow-up 10 years after proximal ulnar osteotomy and 1 year after redial head resection. Bone anchors were inserted after radial resection due to ligament reconstruction. f Lateral projection 1 year after radial head resection
Case 11. Range of motion at follow-up. This patient had a an ulnar osteotomy at the age of 11 years after a delay of 4 years since the initial injury. At the age of 20 years, she had a resection of the radial head because of arthritic pain (see Fig. 2). At follow-up 1 year after radial head resection, she had a slight valgus of her left elbow, but an excellent range of motion
Discussion
We present a consecutive series of traumatic Bado type 1 lesions, with a mean follow-up of 8 years. To our knowledge, this is the longest reported follow-up of a series of this kind [1, 2, 5–14, 25–28]. Only two other studies exist with a follow-up of more than 6 years [1, 2]. In our series, proximal ulnar osteotomy was performed in all cases, and two surgeons performed all of the operations. Follow-up was not complete because 1 of the 17 patients operated on during the 16-year study period was not available.
The conclusions that can be drawn from the study are limited because it was a retrospective study in a small group of patients (due to the rarity of the condition), and information regarding the preoperative status of patients was not systematically collected. In that respect, this study resembles other published studies in this field. To date, only one prospective study has been published [1].
Multiple treatment strategies have been proposed for this demanding condition. Resection of the radial head in children has been tried but abandoned because it carries a poor prognosis, with valgus instability, proximal migration of radius, and wrist pain [12, 25]. Most authors recognize that the deformity of the ulna should be addressed before a durable reduction of the radial head can be obtained because dislocation is associated with deformity of the ulna or rupture of the interosseous membrane. However, cases have been reported in which open reduction of the radial head with ligament reconstruction and K-wire transfixation provided good results [9]. In our experience, ligament reconstruction alone cannot suffice. We report two patients treated with ligament reconstruction as the initial treatment, but, in both cases, we had to perform a proximal ulna osteotomy as a later procedure due to redislocation. This is in agreement with the findings of Horii et al. [26], who found redislocations after ligament reconstruction only in patients without ulnar osteotomy.
We used the remnants of the annular ligament for reconstruction; however, the Bell Tawse procedure [29], later modified by Lloyd-Roberts and Bucknill [11], is the one which is most often mentioned in the literature [6, 9, 12, 26, 30]. In this procedure, the ligament is reconstructed by a lateral strip from the triceps tendon [31]. Other surgeons have used a palmaris longus tendon graft [1], fascia strips [1, 2, 14], or remnants of the original ligament for reconstruction, as in the present study [13]. Published studies give no evidence that one technique is superior to another; however, Nakamura et al. [1] reported that radial notching could be avoided if remnants of the annular ligament for reconstruction are used instead of the pedicled forearm fascia. This is in accordance with our findings because we did not see radial notching in our patients.
It is open to discussion whether ligament reconstruction is mandatory, and adverse effects of reconstruction, such as hourglass constriction of the radial neck and ossification of the ligament, have been published [4]. Several authors argue that reconstruction is not necessary if the radial head is fully reduced by the ulnar osteotomy [8, 10], whereas others find that reconstruction is crucial for the stability of the radial head and for normal elbow function [6, 9, 14, 30]. In our series, ligament reconstruction did not have a significant influence on outcome. We recognize that we have only a few patients in each group and a statistical type 2 error [32] could be present. Yet, judging from the data set, we do not believe that ligament reconstruction had a major effect on the outcome after surgery. The reason for this could be that, if the radial head is perfectly reduced during surgery and tested dynamically in both supination and pronation, then there are no displacing forces acting on the joint. Scar tissue developing around the joint may further stabilize the joint.
An alternative or supplementary approach for the stabilization of the radiocapitellar joint is temporary K-wire fixation. This approach carries the risk of breakage of the wire and damage to the joint surfaces. We did not experience these complications. We found the procedure to be helpful in cases with persistent instability of the radiocapitellar joint. It can be argued that perfect reduction of the radiocapitellar joint by elongation and angulation at the ulnar osteotomy should supersede the need for K-wire transfixation. For these reasons, Hasler et al. [28] advocate external fixation of the ulnar osteotomy. They argue that transfixation of the radiocapitellar joint and ligament reconstruction can be avoided because the elongation and angulation can be adjusted without the need for general anesthesia if subluxation occurs in the postoperative period. With this method, they obtained reduction in 15 of 15 patients with no signs of arthrosis after a mean follow-up of 2 years. This technique was, however, complicated by two delayed healings that had to be bone-grafted. In our study, the radiographic outcome was not worse in the group that had been transfixated. As previously mentioned, the results should be interpreted cautiously; however, our data suggests that K-wire transfixation can be used if indicated without increased risk of osteoarthritic changes. Despite these findings, we advocate that K-wire fixation is to be avoided if possible because of the risk of complications. Instability of the radiohumeral joint, determined intraoperatively with the pronation test, should make the surgeon reconsider the angulation and elongation of the ulnar osteotomy.
There have been many suggestions regarding fixation of the ulnar osteotomy. Kalamchi [13] recommends that the osteotomy should be left unfixed because the periosteum provides sufficient fixation of the fragments. However, he advocated against this approach in cases with radial overgrowth of the radius or other significant adaptive changes. Best [6] treated even late cases with unfixed osteotomies because they believed that this method reduced the deforming forces threatening the radial head. The radial head was kept reduced by a modified Bell Tawse procedure and a transarticular K-wire.
Contrary to the findings of Kalamchi are those of Gyr et al. [30] Although they used modified Bell Tawse procedures and K-wire transfixations in their patients, they obtained the best results when ulnar osteotomy was rigidly fixed with a plate. The concept of rigid fixation is also supported Horii et al. [26], who found that rigid fixation of the ulna was mandatory and that ligament reconstruction alone was not sufficient.
We performed the osteotomy at the level of the ulnar tuberosity because we expected better healing of the metaphyseal bone than more distally. Other authors [2, 6–8] have advocated that the osteotomy should be done at the deformity of the bone. We found, along with others [1, 5, 10, 27], that a proximal osteotomy has a good healing potential and correct of alignment of the radius can be obtained by this method. In our series, two modes of fixation were employed based on surgeon preferences. Fixation was performed either rigidly with a plate or with a bi-cortical Steinmann pin with less stability. We did not find that the outcome was influenced by the fixation method, and all osteotomies healed without complications. Therefore, we believe that Steinmann pin fixation could be further evaluated because it is easier and less complicated to remove than a plate. Steinmann pins may not be useful if a more distal osteotomy is chosen.
It is obvious that Monteggia lesions should be managed in the acute setting. Treatment is, in most cases, closed reduction and the outcome is good [33, 34]. Therefore, the prevention of late cases is of utmost importance, and radiographs should always be evaluated by experienced radiologists. Late cases are a challenge to the surgeon, and the question is whether all cases should be surgically treated. Outcome seems to depend on the magnitude of the hypertrophic changes and the remodeling potential of the bone. These parameters, then again, depend on the delay from injury and the age of the patient. Some authors do not recommend surgery in patients with radial overgrowth [13, 27], whereas others suggest surgery in these patients, even if they only have a small potential for remodeling [1].
At our institution, the approach has been to suggest surgery even in patients over 10 years of age and regardless of the time elapsed since injury in order to avoid late complications like neuropathy and cubitus valgus and to treat complaints such as pain, deformity, and limitations in the range of motion. Our finding is that if surgery is performed less than 40 months after injury, good to fair long-term radiographic results can be obtained. If more than 40 months have elapsed, there is a high risk of recurrent dislocation of the radial head. If surgery is performed before the age of 6 years, the radiographic outcome is good, and if surgery is performed before 10 years of age, the results are fair or good.
Patients should be informed that, even if surgery is performed, they should expect some limitation in the range of motion and strength. Typically, there will be less range of motion and strength in supination.
None of the patients with fully reduced radial head showed an increase in excessive valgus. In contrast, 1 of 2 patients with postoperative secondary dislocation of the radial head had an increase in the carrying angle of 25° compared with the contralateral elbow. This underlines the importance of reducing the radial head in the growing child and argues against conservative treatment or radial head resection during childhood. Radial head resection is a treatment option once there is growth arrest and the elbow is painful. We present the case (Case 11) of a girl who had surgery at the age of 11 years, with a delay of 4 years since the initial injury. At the age of 20 years, she had a resection of the radial head because of pain. The radial head had remained reduced, but there were arthritic changes in the radiohumeral joint. She was seen at follow-up 1 year after radial head resection and showed good objective and self-reported outcomes.
In conclusion, we find that open reduction and proximal ulnar osteotomy are justified, given the fair to good long-term outcomes in the present study. Our findings underline the importance of minimizing the delay between injury and ulnar osteotomy because the outcome depends on it. Until 40 months after injury, good to fair long-term radiographic results can be obtained. After 40 months, there is a high risk of recurrent dislocation of the radial head. We advocate that surgery is offered to patients even at the age of 11 years or with delays of more than 40 months, although there is a risk of pain, secondary dislocation, and further surgery. The patient and parents should be informed about these risks. The elbow must be kept realigned during growth in order to prevent cubitus valgus and neuropathies. We present such a case with long delay and high age at ulnar osteotomy with good functional results at follow-up, even though radial resection was performed at the age of 20 years.
We did not find any evidence that ligament reconstruction and plate fixation provided a more stable reduction than Steinmann pin fixation. Transarticular fixation of the radial head may be used for supplementary fixation because we did not find any complications to this procedure, and it did not seem to influence the radiographic outcome. However, we recognize that breakage of the K-wire is a potential complication and do not recommend its routine use.
References
Nakamura K, Hirachi K, Uchiyama S, Takahara M, Minami A, Imaeda T, Kato H (2009) Long-term clinical and radiographic outcomes after open reduction for missed Monteggia fracture-dislocations in children. J Bone Joint Surg Am 91:1394–1404
Wang MN, Chang WN (2006) Chronic posttraumatic anterior dislocation of the radial head in children: thirteen cases treated by open reduction, ulnar osteotomy, and annular ligament reconstruction through a Boyd incision. J Orthop Trauma 20:1–5
Stelling FH, Cote RH (1956) Traumatic dislocation of head of radius in children. J Am Med Assoc 160:732–736
Rodgers WB, Waters PM, Hall JE (1996) Chronic Monteggia lesions in children. Complications and results of reconstruction. J Bone Joint Surg Am 78:1322–1329
Degreef I, de Smet L (2004) Missed radial head dislocations in children associated with ulnar deformation: treatment by open reduction and ulnar osteotomy. J Orthop Trauma 18:375–378
Best TN (1994) Management of old unreduced Monteggia fracture dislocations of the elbow in children. J Pediatr Orthop 14:193–199
Kim HT, Park BG, Suh JT, Yoo CI (2002) Chronic radial head dislocation in children, Part 2: results of open treatment and factors affecting final outcome. J Pediatr Orthop 22:591–597
Devnani AS (1997) Missed Monteggia fracture dislocation in children. Injury 28:131–133
Cappellino A, Wolfe SW, Marsh JS (1998) Use of a modified Bell Tawse procedure for chronic acquired dislocation of the radial head. J Pediatr Orthop 18:410–414
Lädermann A, Ceroni D, Lefèvre Y, De Rosa V, De Coulon G, Kaelin A (2007) Surgical treatment of missed Monteggia lesions in children. J Child Orthop 1:237–242
Lloyd-Roberts GC, Bucknill TM (1977) Anterior dislocation of the radial head in children: aetiology, natural history and management. J Bone Joint Surg Br 59-B:402–407
Stoll TM, Willis RB, Paterson DC (1992) Treatment of the missed Monteggia fracture in the child. J Bone Joint Surg Br 74:436–440
Kalamchi A (1986) Monteggia fracture-dislocation in children. Late treatment in two cases. J Bone Joint Surg Am 68:615–619
Hui JH, Sulaiman AR, Lee HC, Lam KS, Lee EH (2005) Open reduction and annular ligament reconstruction with fascia of the forearm in chronic monteggia lesions in children. J Pediatr Orthop 25:501–506
Bouyala JM, Chrestian P, Ramaherison P (1978) High osteotomy of the ulna in the treatment of residual anterior dislocation following Monteggia fracture (author’s transl). Chir Pediatr 19:201–203
Bouyala JM, Bollini G, Jacquemier M, Chrestian P, Tallet JM, Tisserand P, Mouttet A (1988) The treatment of old dislocations of the radial head in children by osteotomy of the upper end of the ulna. Apropos of 15 cases. Rev Chir Orthop Reparatrice Appar Mot 74:173–182
Chen WS (1992) Late neuropathy in chronic dislocation of the radial head. Report of two cases. Acta Orthop Scand 63:343–344
Kadic MA, Bloem RM (1991) Traumatic isolated anterior dislocation of the radial head. A case with a 32-year follow-up. Acta Orthop Scand 62:288–289
Jacobsen K, Holm O (1998) Chronic Monteggia injury in a child. Ugeskr Laeger 160:4222–4223
Kim HT, Conjares JN, Suh JT, Yoo CI (2002) Chronic radial head dislocation in children, Part 1: pathologic changes preventing stable reduction and surgical correction. J Pediatr Orthop 22:583–590
Bado JL (1967) The Monteggia lesion. Clin Orthop Relat Res 50:71–86
Leggin BG, Neuman RM, Iannotti JP, Williams GR, Thompson EC (1996) Intrarater and interrater reliability of three isometric dynamometers in assessing shoulder strength. J Shoulder Elbow Surg 5:18–24
Dawson J, Doll H, Boller I, Fitzpatrick R, Little C, Rees J, Jenkinson C, Carr AJ (2008) The development and validation of a patient-reported questionnaire to assess outcomes of elbow surgery. J Bone Joint Surg Br 90:466–473
Dawson J, Doll H, Boller I, Fitzpatrick R, Little C, Rees J, Carr A (2008) Comparative responsiveness and minimal change for the Oxford Elbow Score following surgery. Qual Life Res 17:1257–1267
Tajima T, Yoshizu T (1995) Treatment of long-standing dislocation of the radial head in neglected Monteggia fractures. J Hand Surg Am 20:S91–S94
Horii E, Nakamura R, Koh S, Inagaki H, Yajima H, Nakao E (2002) Surgical treatment for chronic radial head dislocation. J Bone Joint Surg Am 84-A:1183–1188
Hirayama T, Takemitsu Y, Yagihara K, Mikita A (1987) Operation for chronic dislocation of the radial head in children. Reduction by osteotomy of the ulna. J Bone Joint Surg Br 69:639–642
Hasler CC, Von Laer L, Hell AK (2005) Open reduction, ulnar osteotomy and external fixation for chronic anterior dislocation of the head of the radius. J Bone Joint Surg Br 87:88–94
Bell Tawse AJ (1965) The treatment of malunited anterior Monteggia fractures in children. J Bone Joint Surg Br 47:718–723
Gyr BM, Stevens PM, Smith JT (2004) Chronic Monteggia fractures in children: outcome after treatment with the Bell–Tawse procedure. J Pediatr Orthop B 13:402–406
Olsen BS, Søjbjerg JO (2003) The treatment of recurrent posterolateral instability of the elbow. J Bone Joint Surg Br 85:342–346
Altman DG (1991) Practical statistics for medical research. Chapman & Hall, London
Letts M, Locht R, Wiens J (1985) Monteggia fracture-dislocations in children. J Bone Joint Surg Br 67:724–727
Wiley JJ, Galey JP (1985) Monteggia injuries in children. J Bone Joint Surg Br 67:728–731
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Rahbek, O., Deutch, S.R., Kold, S. et al. Long-term outcome after ulnar osteotomy for missed Monteggia fracture dislocation in children. J Child Orthop 5, 449–457 (2011). https://doi.org/10.1007/s11832-011-0372-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-011-0372-0