Abstract
Background
The purpose of this study was to analyze whether hips treated for developmental dysplasia of the hip (DDH) during infancy, which were clinically and radiologically fully normalized by walking age, may become dysplastic again during later growth.
Materials and methods
A total of 150 patients were randomly selected out of a collective of 386 patients treated for DDH at the Department of Orthopaedics at the University of Zurich between 1993 and 2004. Treatment was started at birth and continued for 6 months. All patients had clinically and radiographically normal hips by walking age. The patients did not suffer from other diseases, in particular, neurological or neuromuscular diseases.
Results
We detected four female subjects among the 150 patients who had been successfully treated for DDH, who had developed dysplastic hips in early adolescence, necessitating acetabular surgery.
Conclusion
The successful treatment of DDH in infancy does not ensure normal hip development; therefore, follow up into maturity may be recommended.
Level of evidence
Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Screening for hip dysplasia and early treatment has significantly reduced the rate of later hip disease [1]. Normal hips at birth, without any concomitant neurologic disease, are thought to continue to develop normally [2]. However, as the hips develop throughout growth, secondary abnormal development can occur [3] and of particular importance is secondary dysplastic hip development, which is associated with breech presentation during birth [4]. The question of how long children with normal hips at birth, but with a family history of developmental dysplasia of the hip (DDH), should be followed has been addressed by Osarumwense et al. [5], who concluded that follow up to 1 year is sufficient. However, Cashman et al. [6] argued that follow up until the patients turn 5 years old is needed, as some hips become deteriorated again. Recently, it has been reported that a late dislocation of the hip was observed at the age of 30 months, while initial normal neonatal development was observed by clinical and ultrasound examination [7].
In our institution, the policy is to examine children treated for DDH until skeletal maturity. We have now raised the question as to whether this is needed.
Methods
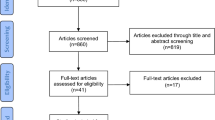
At the Department of Orthopaedics at the University of Zurich, between 1993 and 2004, 386 children were treated for DDH type IIc or worse, according to Graf [8], before 6 months of age. Out of this collective, 150 patients were randomly selected for analysis of their treatment data and their final examination.
The mean age at the last examination was 11.8 years (range 10–16 years).
All patients had had treatment until normal hips were confirmed sonographically or radiographically. Following normalization, they were observed by ultrasound at 9 months and X-rays were taken when the children had been freely walking for 3 months. Most of the children were re-examined when they turned 4 years old with a standard pelvic X-ray.
X-rays were evaluated for the osseous development of the anterior and posterior wall and the center edge (CE) angle compared to the normal data as described by Tönnis [9].
Our institutional review board does not require approval or informed consent for the retrospective review of patient records or images. However, patients’ rights are protected by a law which requires that they must be informed that their charts and images might be reviewed for scientific purposes and which grants patients the opportunity to forbid such use of their data.
Results
All children had normal pelvic X-rays when they started walking. At the follow up examination at puberty, we discovered four females who were treated for DDH as infants had developed significant dysplasia of the hip at puberty. These patients did not have neurologic disorders or other medical conditions.
Details of these patients are discussed as follows.
Patient G.M. *3.12.1993 (Fig. 1)
This patient was delivered by C-section because of breech presentation. She underwent a closed reduction for bilateral hip dislocation at 1 month and retention in a spica cast for 1 month, followed by retention in a Pavlik harness until the age of 8 months.
a This girl showed a good reduction with symmetrical centred hips at the age of 4 years. b At the age of eight on the x-ray symmetrical centred hips could be confirmed. c At the age of 14 she complaint about pain during exercise and in the x-rays a dysplasia of the right hip could be confirmed, with a CE angle of 25°. On the left side a minor dysplasia could be observed. d When she turned 15, a bernese pelvis osteotomy was performed, the left hip is currently still asymptomatic
Pelvic X-Rays at 4 years (Fig. 1a) as well as at 8 years of age (Fig. 1b) were normal. She was re-examined as planned at 14 years; she then complained of right hip pain during physical activity. Clinically, she showed a decreased range of motion (flexion–extension 90°–5°–0°) and apprehension in flexion. The X-ray showed severely dysplastic hips bilaterally (Fig. 1c). The CE angle was measured to be 15° (three standard deviations below the mean normal value [9]). She was treated with a Bernese periacetabular osteotomy [10].
Patient F.N. *13.04.1993 (Fig. 2)
Ultrasound screening at birth showed hips bilaterally type IIc according to Graf. Initially, she was treated for 5 months with broad diapering. Because of insufficient improvement, treatment was changed to a Pavlik harness until 8 months of age. X-rays were normal at the age of 4 years (Fig. 2a), as well as at 8 years (Fig. 2b). She presented herself for the planned consultation at the age of 13 years, at which time she admitted to experiencing groin pain during physical activity. Radiologically (Fig. 2c), she showed insufficient anterior and posterior acetabular coverage on the right side, less pronounced on the left side. The CE angle was measured to be 6° (four standard deviations below the mean normal value [9]). At the age of 14 years, she was treated with a Bernese pelvic osteotomy.
a In this patient at the age of 4 years normal appearing hips could be observed by x-ray. b Also at the age of 8 years the x-ray showed normal hips. c At the age of 13 radiologically an acetabular dysplasia could be confirmed at the right side while a borderline dysplasia on the left side, with a CE angle of 21°. d At the age of 14 also in this patient a bernese pelvic osteotomy was performed
Patient L.M. *18.10.1996 (Fig. 3)
At birth, an ultrasound examination detected hip dysplasia type IIIa on the right side and type IId on the left. Treatment with a Pavlik harness continued until 5 months of age. The X-ray at 14 months of age was normal (Fig. 3a). She was seen again for a consultation at the age of 10 years, without hip disturbances. The pelvic X-ray was normal (Fig. 3b). However, at the age of 12 years, she developed increasing hip pain more pronounced in her left hip than the right, mainly occuring during gymnastics (Fig. 3c). The CE angle is 26° (one standard deviation below the mean normal value [9]), but there is a significant retroversion of the acetabulum with a positive crossover sign (Fig. 3c). She is scheduled for a periacetabular osteotomy in 1 year, when bone growth arrest is expected to be reached.
a The third girl showed a normal x-ray when she was 14 months old with symmetrical hips. b At the age of 10 years she did not complain about any hip problems, and the x-ray of her hips was interpreted as being normal. c At the age of 12 radiologically an acetabular retrovsion could be observed, causing painful impingement symptoms. The CE angle was measured with 15°. Due to the fact that bone growth arrest was not reached until now, we plan to perfom acetabular surgery next year
Patient B.G. *07.11.1988 (Fig. 4)
An ultrasound examination 6 weeks after birth detected hip dysplasia type IIc on the right side and type IIc on the left. Treatment with a Pavlik harness was followed for 12 weeks. The ultrasound at the age of 12 weeks was normal. The X-ray at 18 months of age was normal. At 6 years of age, the pelvic X-ray was normal. She came for the planned check-up at the age of 12 years; she did not have pain or other clinical symptoms. After radiographic analysis, hip dysplasia presented on the right side. The CE angle is 5° (four standard deviations below the mean normal value [9]), but there is a significant retroversion of the acetabulum with a positive crossover sign. She is scheduled for a triple pelvic osteotomy.
a The x-ray at 18 months of age was normal. b She was seen again for a consultation when she was 6 years old, without hip disturbances; pelvic x-ray was normal. c At the age of 12 she developed a hip dysplasia on the right side. The CE angle is 5° (four standard deviation below the mean normal value) but there is significant retroversion of the acetabulum with positive cross over sign. She is scheduled for a triple pelvic osteotomy
Discussion
The hips of four of 150 children who had appeared to be treated successfully for DDH in early infancy with normal X-rays at walking age became dysplastic again at puberty to a degree which required acetabular reorientation. These patients account for about 3% of the randomly selected patient population. Only one of the children came for the proposed control examination at puberty because of a complaint of groin pain. The others—though admitting to having some hip symptoms—presented for check-up because of our recommendation for such a control.
Unfortunately, there are no statistical data available for the development of children born with normal hips and their developmental profile. However, we know from occasional observations that some individuals who initially appear normal may develop dysplasia with later growth [3, 4, 7].
Kobayashi et al. [11] recently reported data about the development of the unaffected hip in children treated for unilateral hip dysplasia. The initial normal/healthy interpreted side later appeared to be dysplastic in 13.6% of the patient population. These are very surprising data; however, they also support the need for long-term follow up.
The question remains open if our observations of secondary dysplastic development following the normalization of hips treated for DDH reflects the ‘normal natural’ statistical development or are related to the primary causes of DDH.
Though the long-term follow up data for acetabular reorientation are still limited, pain relief following acetabular reorientation in symptomatic patients is highly suggestive of its value to prevent early degenerative arthritis. Our data add to the data arguing for a longer follow up until maturity [6].
Conclusion
The result of treatment for developmental dysplasia of the hip (DDH) is definitive only at skeletal maturity. Follow up into maturity should, therefore, be considered. As only one of the patients presented a complaint because of hip symptoms, while the other three stated their hip problems only when specifically asked, we suggest re-examination at puberty for children treated for DDH. Whether asymptomatic adolescents should have an X-ray is debatable. However, patients may develop clinical symptoms from significant hip dysplasia much later in development, as well as joint damage, and, therefore, would benefit from an earlier acetabular re-orientation.
References
Graf R (2007) Hip sonography: 20 years experience and results. Hip Int 17(Suppl 5):S8–S14
Graf R (2002) Ultrasound examination of the hip. An update. Orthopade 31(2):181–189
Exner GU, Kern SM (1994) Natural course of mild hip dysplasia from young childhood into adulthood. Orthopade 23(3):181–184
Exner GU, Schams M (1999) Later development of hip dysplasia after breech presentation with normal hips at birth in otherwise healthy children. Abstract, EPOS, Göteborg
Osarumwense D, Popple D, Kershaw IF, Kershaw CJ, Furlong AJ (2007) What follow-up is required for children with a family history of developmental dysplasia of the hip? J Pediatr Orthop B 16(6):399–402
Cashman JP, Round J, Taylor G, Clarke NM (2002) The natural history of developmental dysplasia of the hip after early supervised treatment in the Pavlik harness. A prospective, longitudinal follow-up. J Bone Joint Surg Br 84(3):418–425
Jaiswal A, Starks I, Kiely NT (2010) Late dislocation of the hip following normal neonatal clinical and ultrasound examination. J Bone Joint Surg Br 92(10):1449–1451
Graf R (1984) Classification of hip joint dysplasia by means of sonography. Arch Orthop Trauma Surg 102(4):248–255
Tönnis D (1976) Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res (119):39–47
Ganz R, Klaue K, Vinh TS, Mast JW (1988) A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res (232):26–36
Kobayashi D, Satsuma S, Kuroda R, Kurosaka M (2010) Acetabular development in the contralateral hip in patients with unilateral developmental dysplasia of the hip. J Bone Joint Surg Am 92(6):1390–1397
Acknowledgments
We would like to thank Sophia Savage for carefully proofreading the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
About this article
Cite this article
Modaressi, K., Erschbamer, M. & Exner, G.U. Dysplasia of the hip in adolescent patients successfully treated for developmental dysplasia of the hip. J Child Orthop 5, 261–266 (2011). https://doi.org/10.1007/s11832-011-0356-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-011-0356-0