Abstract
Purpose
This study compared measured physical performance, health-related quality of life (HRQOL), and social role attainment between extremity sarcoma survivors and controls, and evaluated associations between disease and treatment exposures, health conditions, and performance measures.
Methods
Survivors of extremity sarcoma from the St. Jude Lifetime cohort and controls frequency matched by age-, sex-, and race completed physical performance testing and questionnaires. Survivors with Z-scores on outcome measures ≤ −2.0 SD (compared to controls) were categorized with severe impairment/limitation.
Results
Among 206 survivors (52.4 % male median age 36 years (range 19–65)), 37 % had low relative lean mass, 9.7 % had an ejection fraction <50 %, 51.5 % had diffusion capacity for carbon monoxide <75 %, 27.7 % had sensory and 25.2 % motor neuropathy, and 78.2 % had musculoskeletal complications. Severe impairments/limitations were present among ≥25 % of survivors on fitness, balance, and physical HRQOL measures, and among ≥15 % on strength and activity of daily living measures. Lower extremity tumor location (OR 8.23, 95 % CI 2.54–26.67, P value 0.0004) and amputation (OR 8.07, 95 % CI 3.06–21.27, P value <0.0001) were associated with poor fitness. Poor fitness was associated with increased odds of scoring <40 on the SF-36 physical component summary (OR 4.83, 95 % CI 1.95–11.99, P value 0.001) and role-physical subscale (OR 3.34, 95 % CI 1.33–8.43, P value 0.01). Survivors and controls had similar rates of marriage, independent living, employment, and college attendance.
Conclusions
Extremity sarcoma survivors experience high rates of physical impairment and report lower than expected physical HRQOL. However, they are as likely as peers to be married, live independently, be employed, and attend college.
Implications for Cancer Survivors
Follow-up for extremity sarcoma survivors should include assessment of need for further orthopedic care and rehabilitation to address cardiopulmonary and musculoskeletal health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Musculoskeletal sarcomas in children and adolescents are a group of rare malignant tumors involving bone and soft tissue, accounting for 4–13 % of all malignant neoplasms in these age groups. Survival has improved over the last decades due to advances in treatment, including adjuvant chemotherapy [1, 2]. Estimates indicate there are nearly 50,000 survivors of pediatric bone and soft tissue sarcoma in the USA; 36,723 are younger than age 50 years [3]. Because curative treatment requires a multimodal approach involving surgery, radiation, and chemotherapy, sarcoma survivors are at risk for therapy-related complications [4, 5]. Medical late effects, including infertility, gonadal hormone deficiency, second malignant neoplasms, cardiomyopathy, pulmonary dysfunction, and renal insufficiency have been documented [4, 6–11]. Self-report data from the Childhood Cancer Survivor Study (CCSS) also indicate that adult survivors of childhood bone and soft tissue sarcoma are vulnerable to adverse physical performance outcomes that increase with age and are associated with poor health-related quality of life (HRQOL), lower educational attainment, and unemployment [12].
Previous studies provide insight regarding functional loss and broadly identify those at risk for a poor outcome. However, because this information is based on self-report, it does not provide details about physical performance needed to guide development of interventions tailored to this population. In addition, identification of disease-specific and demographic variables, treatment modalities, medical complications, and lifestyle factors that influence physical performance would provide information for survivors currently receiving treatment to identify those in need of rehabilitation and follow-up.
The aims of this study were to (1) compare measured physical performance, HRQOL, and social attainment between survivors of childhood musculoskeletal sarcomas of the extremities to healthy controls, frequency matched by age, sex, and race and (2) evaluate associations between disease and treatment variables, health conditions, and physical performance measures in this population.
Materials and methods
Study participants
Participants were members of the St. Jude Lifetime cohort (SJLIFE), treated for musculoskeletal sarcomas of the extremities during childhood, who completed physical performance assessments and questionnaires that included the Medical Outcomes Survey Short-Form 36 (SF-36) and items related to social role attainment. Sarcoma of the extremity was defined as a malignant tumor derived from mesenchymal bone or soft tissue. Pelvic tumors were excluded. Eligibility criteria for inclusion in the SJLIFE cohort include the following: (1) diagnosis of childhood malignancy treated at St. Jude Children’s Research Hospital (SJCRH); (2) survival of >10 years from diagnosis; and (3) current age ≥18 years. Three levels of participation are offered in the SJLIFE study: (1) comprehensive evaluation on the SJCRH campus; (2) limited local evaluation by Examination Management Services, Inc. (EMSI) for survivors who decline to return to SJCRH; or (3) completion of health surveys by mail or phone interview for those survivors who decline to return to SJCRH or undergo a local evaluation [13, 14]. Briefly, participants were at least ten-year survivors of childhood cancer, treated between 1962 and 2004, and 18 years of age or older. As of October 2013, this included 328 survivors of an extremity sarcoma, 206 (62.8 %) of whom completed a functional assessment. A comparison group of adults without previous cancer diagnoses, recruited from among parents, friends, and relatives of current St. Jude patients, and frequency matched by 5-year age group, sex, and race, completed the same assessments. Study documents were approved by the institutional review board. Participants provided written informed consent prior to assessment.
Variable definitions
Physical performance
Physical performance measures included flexibility, balance, muscle strength, general fitness, and overall physical performance. Results are presented as means and standard deviations (SD) and percentages to indicate the proportion of survivors whose scores were 1.5 and 2.0 SD below the means of age-, sex-, and race-matched peers. Low back and hamstring flexibility were assessed by having the participants complete the sit-and-reach test [15]. Ankle passive and active ranges of motion were measured in sitting with the hips and knees in 90° of flexion with a goniometer [16, 17]. Balance was evaluated with the Sensory Organization Test (Neurocom Smart Equitest, Natus Medical, Clackamas, OR). Participants maintained an upright posture during six sensory conditions while standing in a visual surround on a force plate that measured time spent inside a 12° sway envelope. Overall composite and vestibular scores (percentages) were used for analysis [18].
Hand grip strength was measured with a dynamometer (Jamar, Lafayette Instrument Company, Lafayette, IN) with the participant sitting, the shoulder in 0°–10° of flexion/abduction, the elbow in 90° of flexion, and the forearm in neutral [19, 20]. Isokinetic knee extension, dorsiflexion, and plantar flexion were assessed with an isokinetic dynamometer (Biodex System 3.0, Biodex Medical Systems, Shirley, NY). Measurements of peak torque (Newton meters (Nm)) per kilogram (kg) of body weight were made at speeds of 60°, 180°, and 300°/s for the quadriceps, and 60° and 90°/s for ankle motions [21, 22]. For bilateral measures, the average of the maximum value from each side was used for analysis. For those with amputation, the maximum value from the intact extremity was used.
Fitness was evaluated with the six-minute-walk test [23]. Participants wore a heart rate monitor and walked in a level corridor. Encouragement was given every minute, and heart rate recorded at rest, 2, 4, and 6 min and 2 min after test completion. Distance in meters and physiologic cost index (maximum heart rate – resting heart rate / gait speed) were calculated. Overall physical performance was evaluated with the 7-item physical performance test (PPT), [24] where a score of 28/28 indicates no deficit.
Health-related quality of life
HRQOL was measured using the Medical Outcomes Survey 36-Item Short Form Health Survey (SF-36) [25]. This widely used generic health profile provides subscale scores for 8 domains of HRQOL: general health, role physical, physical function, bodily pain, vitality, mental health, social function, and role emotional, and mental and physical health composite scores. The SF-36 provides age- and sex-specific norms. T-scores ≤40 were classified as poor HRQOL.
Social role attainment
Social attainment was assessed using indicators of adult achievement including marital status, independent living, employment, and educational attainment.
Independent variables
Participant characteristics, age, sex, and race, were obtained by questionnaire. Diagnosis and treatment data were obtained from medical records by trained abstractors and included diagnosis, metastatic status, relapse status, age at diagnosis, length of follow-up, tumor location(s), chemotherapy exposures and doses, radiation exposures and doses and surgery for local control, metastatic disease, relapse, and complications. Musculoskeletal complications from diagnosis through follow-up were obtained from extensive review of medical records and images by a surgeon (IFP) and by interview and examination during medical and functional evaluations. Participants were also screened for body composition abnormalities, cardiac impairment, pulmonary dysfunction, and neuropathy. Those with age-, race-, and sex-specific relative lean muscle mass for height Z-scores < −1.5 SD were classified with low lean mass [26], those with ejection fraction (EF) < 50 % with cardiac impairment [27], those with diffusing capacity of the lungs for carbon monoxide (DLCOcorr) <75 % with abnormal pulmonary function [28], and those with Common Terminology Criteria for Adverse Events (CTCAE) grades 2–4 peripheral sensory or motor dysfunction with neuropathy [29].
Statistical analyses
The means for demographic and functional measures were compared between survivors and controls with two-sample t tests or non-parametric equivalents. The percentages of survivors who performed below −1.5 and −2 SD of expected (compared to controls) were calculated to illustrate the magnitude of functional loss.
The means for composite and subscale scores on the SF-36 were compared between survivors and controls with two-sample t tests. Percentages of survivors in social attainment categories were contrasted to controls with Chi-square statistics. Associations between disease (tumor type, location, bone involvement) and treatment variables, health conditions, and impaired performance (−1.5 SD) on physical measures were evaluated with multivariable logistic regression among survivors. Associations between impaired performance on physical measures and poor HRQOL were also evaluated with logistic regression. Variables with P values ≤0.10 in preliminary univariable models were retained for inclusion in multivariate models. Multicollinearity was evaluated to avoid over fitting. SAS version 9.3 (SAS Institute, Cary, NC) was used for analysis.
Results
Characteristics of study participants
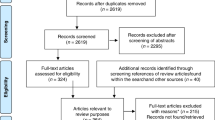
Of 328 extremity sarcoma survivors potentially eligible, 20 were elected to complete a survey only, 13 were lost to follow-up, 25 were interested but had not yet completed a campus visit at the time of this analysis, and 61 declined participation. This report summarizes results of 209 (63.7 %) participants with a campus visit, 206 of whom completed a functional assessment. Participants did not differ from non-participants by sex, race, diagnosis, or age at diagnosis. The characteristics of the study population are shown in Table 1. Median ages at evaluation were bone sarcoma (BS), 38 years (range, 21–65), soft tissue sarcoma (STS), 33 years (range, 19–61) , and controls, 33 years (range, 19–51). BS survivors were more likely to be male and STS survivors more likely to be female. The most frequent BS histology was osteosarcoma; the most frequent STS histology was non-rhabdomyosarcoma soft tissue sarcoma. The most frequent tumor site was the lower extremity (81 %).
Surgery was the primary method of local control for 84 % of survivors; 43.9 % with BS and 32.7 % with STS had amputation for local control. Amputation was required as the result of local complication/relapse for an additional 13.4 % of BS and 6.1 % of STS survivors. Pulmonary metastases at diagnosis resulted in thoracotomies among 12 BS and 4 STS patients. An additional 27 participants had thoracotomy for relapsed pulmonary disease. Overall, the 206 participants had 783 surgical procedures, with mean per patient of 3.8 (95 % CI 3.4–4.3). Chest radiation was received by 5.8 % and limb radiation by 22.3 % of patients. Nearly all BS, but less than half of STS, were treated with anthracycline- and alkylating-containing regimens. Platinum was received by 46.5 % of BS and 10.2 % of STS survivors.
Health outcome data with potential impact on physical function are also shown in Table 1. Relative lean mass < −1.5 SD was observed in approximately 36 % of BS and 43 % of STS survivors. EF <50 % was present in 12 % of BS and 2 % of STS survivors. DLCOcorr <75 % was present in 57 % of BS and 33 % of STS survivors. Over 25 % of survivors had sensory and 25.2 % had motor neuropathy. Musculoskeletal complications were experienced by 78.2 % of patients (mean rate per patient 1.9 (range 0–8)). The most common long-term musculoskeletal complication was fracture associated with traumatic injury (28.8 %), followed by prosthetic malfunction/complication (8.3 %).
Physical performance, HRQOL, social roles
Table 2 demonstrates mean values (survivors and controls) and percentages of survivors with values 1.5 and 2.0 SD below age- and sex-specific expected values (using our control population) for physical performance and HRQOL. Severe deficits in performance on the six-minute-walk test, balance measures, and physical component summary and physical function subscale of the SF-36 were observed in over 25 % of survivors. A substantial number of survivors (>15 % when the expected rate is only 6.7 %) also had severe limitations in strength, social functioning, and activities of daily living. Survivors and controls had similar percentages for marriage (60.2 vs. 60.9 %, P = 0.79), independent living (75.7 vs. 72.8 %, P = 0.99), employment (70.9 vs. 75.7 %, P = 0.14), and college attendance (63.6 vs. 68.5 %, P = 0.06).
Treatment and physical performance
Table 3 shows the results of multivariable models examining associations between treatment and poor physical performance among survivors. After adjusting for other treatment exposures, tumor location in the lower extremity and amputation were the only factors associated with any performance outcomes, impacting balance and cardiopulmonary fitness.
Chronic conditions and physical performance
Table 4 shows the results of multivariable models examining associations between specific chronic conditions, number of musculoskeletal complications, and poor physical performance among survivors. Relative low lean muscle mass was associated with quadriceps and ankle weakness and with balance impairment. EF <50 % was associated with impaired balance and quadriceps weakness; DLCOcorr <75 % was associated with impaired flexibility. Motor neuropathy was associated with impaired flexibility, quadriceps and ankle weakness, impaired fitness, and limited activities of daily living. The presence of two or more musculoskeletal complications was associated with impaired balance, and amputation was associated with impaired balance and impaired fitness. Sensory neuropathy was not associated with any of the physical performance outcomes.
Physical performance and HRQOL
Table 5 shows the results of multivariable models examining associations between physical performance measures and scoring <40 on the summary and subscales of the SF-36. Impaired fitness and limited activities of daily living were associated with a suboptimal outcome on the physical component summary of the SF-36; fitness impairment was also associated with scoring <40 on the role physical subscale of the SF-36. Social functioning was not impacted by any of the physical performance impairments.
Discussion
Prior investigations have relied on self-report or clinician-based observations to describe long-term functional outcomes and HRQOL in adult survivors of childhood extremity sarcomas [6, 11, 30, 31]. In this study, we provide results of an extensive clinical assessment of long-term musculoskeletal sarcomas of the extremities among survivors evaluated decades following treatment. Nearly 80 % of extremity sarcoma survivors in this cohort treated 1962–2004 experienced musculoskeletal complications after initial local control. These complications required subsequent surgical intervention, including eventual amputation among some initially treated with limb-sparing surgery. We also document significant rates of other adverse health outcomes in this population, including impaired cardiac and pulmonary function, low lean mass, peripheral neuropathy, muscle weakness, poor balance, impaired fitness, and limitations in activities of daily living. In addition, we observed that performance limitations are associated with reduced HRQOL in physical domains. Despite these impairments, survivors were as likely as controls to be married, live independently, be employed, and attend college.
Our study indicates a higher prevalence of musculoskeletal complications among extremity sarcoma survivors than previously reported. For example, Hamilton et al. [32] reviewed progress notes of pediatric Ewing sarcoma survivors (median follow-up 13.5 years) treated 1960–2005 and reported that 50 % of 64 patients who survived at least 5 years had long-term musculoskeletal abnormalities. Tan et al. [33] reported post-operative complications in 35 % of 120 patients with osteosarcoma (mean follow-up 56.8 months) treated 1998–2008. These included infection, prosthetic loosening, fracture, and patellar tendon rupture. Mavrogenis et al. [34] evaluated outcomes (median follow-up 67 months) among 42 patients with osteosarcoma in the distal tibia treated 1985–2010, reporting complications among 26 % with limb-sparing procedures and 5 % with amputation. Our prevalence is more consistent with data from CCSS that reported a hazard ratio of 2.8 (95 % CI 1.3 to 5.9) for grades 3–5 musculoskeletal chronic conditions when comparing survivors (total N = 5604, sarcoma N = 1342) 35+ years of age to siblings [35]. Like CCSS, our study included survivors with longer follow-up (median 25 years) and some survivors treated before 1980. Results emphasize the need for continuing orthopedic follow-up among extremity sarcoma survivors as they age.
Increased risk for cardiac and pulmonary conditions [7, 8, 11, 36], neuropathy [37], and low lean muscle mass [38] in long-term pediatric extremity sarcoma survivors have been previously reported in large cohorts. However, only small studies have reported specific, objectively measured physical performance, and few report associations between chronic health conditions and physical performance, or between physical performance and HRQOL. In a study that included 30 sarcoma survivors aged 35 ± 10 years, Gerber et al. [39] documented impaired range of motion in 67 %, reduced gait velocity in 42 %, and substantial problems with activities of daily living in 44 %. As in our study, these authors observed that lower extremity tumor location was associated with impaired physical performance and that suboptimal performance on a walking test was associated with worse scores on both measured and self-report of daily activity. Data from a younger cohort (N = 68, ages 6–26 years) of patients with sarcoma at least 1 year post-limb-sparing surgery also described problems with joint range of motion and mobility (walking, stair climbing) [40].
Our data extends the results of these studies by identifying apparent musculoskeletal and other specific chronic health conditions that could be addressed as part of clinical/rehabilitative care to improve physical performance. Data suggests that structured exercise for pediatric sarcoma survivors with subclinical cardiomyopathy is feasible and safe [41] and that intense exercise post-pneumonectomy improves lung function, strength, and fitness [42]. Evidence also exists to support resistance training to improve lean muscle mass [43] and vestibular rehabilitation to improve balance [44].
Our finding that survivors of childhood musculoskeletal sarcomas of the extremities report poor HRQOL in physical but not mental or emotional domains is consistent with the others [45]. Although some attribute this to potential alteration in expectations among individuals who have become accustomed to disability over time, in a much younger cohort (N = 82, ages 8–25 years) of bone sarcoma survivors, Bekkering et al. [45] reported impaired HRQOL only in physical domains when comparing survivors to controls. Importantly, survivors of sarcoma who participated in our study have neither social outcomes different from controls nor indicate that physical performance impacted their social function.
There are limitations that should be considered when evaluating results. First, the therapy for extremity musculoskeletal sarcomas has changed from 1962 to 2004, the period of diagnosis for our participants. Data from older survivors may not apply to children treated today with fewer amputations, improved surgical techniques, and better hospital care. Second, this was a cross-sectional analysis, concomitant evaluation of physical performance measures, and HRQOL does not allow interpretation of a temporal association between these outcomes. Although we found no differences among survivors by diagnosis, sex, race/ethnicity, or age, it is possible that survivors with more or less disability, either unable to travel, or more likely to be too busy to return to the institution, were less likely to participate, which would bias our results. Finally, although our population is large and well characterized, it is heterogeneous in terms of tumor type and location, making it difficult to draw conclusions about specific sub-populations.
Conclusions
Long-term survivors of extremity sarcomas experience complications and have low scores on physical performance measures. Low lean muscle mass, impaired cardiac and pulmonary function, and neuropathy contribute to their poor performance. Follow-up for extremity sarcoma survivors should include assessment of need for further orthopedic care and rehabilitation to address cardiopulmonary and musculoskeletal health.
References
Mirabello L, Troisi RJ, Savage SA. Osteosarcoma incidence and survival rates from 1973 to 2004: data from the Surveillance, Epidemiology, and End Results Program. Cancer. 2009;115:1531–43.
Pappo AS, Pratt CB. Soft tissue sarcomas in children. Cancer Treat Res. 1997;91:205–22.
Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF et al. SEER cancer statistics review, 1975–2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.
Denbo JW, Zhu L, Srivastava D, Stokes DC, Srinivasan S, Hudson MM, et al. Long-term pulmonary function after metastasectomy for childhood osteosarcoma: a report from the St Jude lifetime cohort study. J Am Coll Surg. 2014;219:265–71.
Green DM, Kun LE, Matthay KK, Meadows AT, Meyer WH, Meyers PA, et al. Relevance of historical therapeutic approaches to the contemporary treatment of pediatric solid tumors. Pediatr Blood Cancer. 2013;60:1083–94.
Punyko JA, Mertens AC, Gurney JG, Yasui Y, Donaldson SS, Rodeberg DA, et al. Long-term medical effects of childhood and adolescent rhabdomyosarcoma: a report from the childhood cancer survivor study. Pediatr Blood Cancer. 2005;44:643–53.
Nagarajan R, Kamruzzaman A, Ness KK, Marchese VG, Sklar C, Mertens A, et al. Twenty years of follow-up of survivors of childhood osteosarcoma: a report from the Childhood Cancer Survivor Study. Cancer. 2011;117:625–34.
Mertens AC, Yasui Y, Liu Y, Stovall M, Hutchinson R, Ginsberg J, et al. Pulmonary complications in survivors of childhood and adolescent cancer. A report from the Childhood Cancer Survivor Study. Cancer. 2002;95:2431–41.
Green DM, Kawashima T, Stovall M, Leisenring W, Sklar CA, Mertens AC, et al. Fertility of male survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2010;28:332–9.
Green DM, Kawashima T, Stovall M, Leisenring W, Sklar CA, Mertens AC, et al. Fertility of female survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol. 2009;27:2677–85.
Ginsberg JP, Goodman P, Leisenring W, Ness KK, Meyers PA, Wolden SL, et al. Long-term survivors of childhood Ewing sarcoma: report from the childhood cancer survivor study. J Natl Cancer Inst. 2010;102:1272–83.
Marina N, Hudson MM, Jones KE, Mulrooney DA, Avedian R, Donaldson SS, et al. Changes in health status among aging survivors of pediatric upper and lower extremity sarcoma: a report from the childhood cancer survivor study. Arch Phys Med Rehabil. 2013;94:1062–73.
Hudson MM, Ness KK, Nolan VG, Armstrong GT, Green DM, Morris EB, et al. Prospective medical assessment of adults surviving childhood cancer: study design, cohort characteristics, and feasibility of the St Jude Lifetime Cohort Study. Pediatr Blood Cancer. 2011;56:825–36.
Ojha RP, Oancea SC, Ness KK, et al. Assessment of potential bias from non-participation in a dynamic clinical cohort of long-term childhood cancer survivors: results from the St Jude Lifetime Cohort Study. Pediatr Blood Cancer. 2013;60:856–64.
Mayorga-Vega D, Merino-Marban R, Viciana J. Criterion-related validity of Sit-and-reach tests for estimating hamstring and lumbar extensibility: a meta-analysis. J Sports Sci Med. 2014;13:1–14.
Baggett BD, Young G. Ankle joint dorsiflexion. Establishment of a normal range. J Am Podiatr Med Assoc. 1993;83:251–4.
Moseley AM, Crosbie J, Adams R. Normative data for passive ankle plantarflexion–dorsiflexion flexibility. Clin Biomech (Bristol, Avon). 2001;16:514–21.
Cohen H, Heaton LG, Congdon SL, Jenkins HA. Changes in sensory organization test scores with age. Age Ageing. 1996;25:39–44.
Mathiowetz V, Weber K, Volland G, Kashman N. Reliability and validity of grip and pinch strength evaluations. J Hand Surg [Am]. 1984;9:222–6.
Mathiowetz V, Kashman N, Volland G, Weber K, Dowe M, Rogers S. Grip and pinch strength: normative data for adults. Arch Phys Med Rehabil. 1985;66:69–74.
Danneskiold-Samsoe B, Bartels EM, Bulow PM, Lund H, Stockmarr A, Holm CC, et al. Isokinetic and isometric muscle strength in a healthy population with special reference to age and gender. Acta Physiol (Oxf). 2009;197(673 Suppl):1–68.
Drouin JM, Valovich McLeod TC, Shultz SJ, Gansneder BM, Perrin DH. Reliability and validity of the Biodex system 3 pro isokinetic dynamometer velocity, torque and position measurements. Eur J Appl Physiol. 2004;91:22–9.
Laboratories ATSCoPSfCPF. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7.
Reuben DB, Siu AL. An objective measure of physical function of elderly outpatients. The physical performance test. J Am Geriatr Soc. 1990;38:1105–12.
Ware Jr JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Kelly TL, Wilson KE, Heymsfield SB. Dual energy X-Ray absorptiometry body composition reference values from NHANES. PLoS One. 2009;4:e7038.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey Jr DE, Drazner MH, et al. ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147–239.
Neas LM, Schwartz J. The determinants of pulmonary diffusing capacity in a national sample of U.S. adults. Am J Respir Crit Care Med. 1996;153:656–64.
U.S. Department of Health and Human Services-National Institutes of Health-National Cancer Institute: Common Terminology Criteria for Adverse Events (CTCAE) version 4.0, 2010.
Nagarajan R, Clohisy DR, Neglia JP, Yasui Y, Mitby PA, Sklar C, et al. Function and quality-of-life of survivors of pelvic and lower extremity osteosarcoma and Ewing’s sarcoma: the Childhood Cancer Survivor Study. Br J Cancer. 2004;91:1858–65.
Stish BJ, Ahmed SK, Rose PS, Arndt CA, Laack NN. Patient-reported functional and quality of life outcomes in a large cohort of long-term survivors of Ewing sarcoma. Pediatr Blood Cancer. 2015;62:2189–96.
Hamilton SN, Carlson R, Hasan H, Rassekh SR, Goddard K. Long-term outcomes and complications in pediatric Ewing sarcoma. Am J Clin Oncol 2015; Jan 16.
Tan PX, Yong BC, Wang J, Huang G, Yin JQ, Zou CY, et al. Analysis of the efficacy and prognosis of limb-salvage surgery for osteosarcoma around the knee. Eur J Surg Oncol. 2012;38:1171–7.
Mavrogenis AF, Abati CN, Romagnoli C, Ruggieri P. Similar survival but better function for patients after limb salvage versus amputation for distal tibia osteosarcoma. Clin Orthop Relat Res. 2012;470:1735–48.
Armstrong GT, Kawashima T, Leisenring W, Stratton K, Stovall M, Hudson MM, et al. Aging and risk of severe, disabling, life-threatening, and fatal events in the childhood cancer survivor study. J Clin Oncol. 2014;32:1218–27.
Mulrooney DA, Yeazel MW, Kawashima T, Mertens AC, Mitby P, Stovall M, et al. Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: retrospective analysis of the Childhood Cancer Survivor Study cohort. BMJ. 2009;339:b4606.
Ness KK, Jones KE, Smith WA, Spunt SL, Wilson CL, Armstrong GT, et al. Chemotherapy-related neuropathic symptoms and functional impairment in adult survivors of extracranial solid tumors of childhood: results from the St. Jude Lifetime Cohort Study. Arch Phys Med Rehabil. 2013;94:1451–7.
Ness KK, Krull KR, Jones KE, Mulrooney DA, Armstrong GT, Green DM, et al. Physiologic frailty as a sign of accelerated aging among adult survivors of childhood cancer: a report from the St Jude Lifetime cohort study. J Clin Oncol. 2013;31:4496–503.
Gerber LH, Hoffman K, Chaudhry U, Augustine E, Parks R, Bernad M, et al. Functional outcomes and life satisfaction in long-term survivors of pediatric sarcomas. Arch Phys Med Rehabil. 2006;87:1611–7.
Marchese VG, Spearing E, Callaway L, Rai SN, Zhang L, Hinds PS, et al. Relationships among range of motion, functional mobility, and quality of life in children and adolescents after limb-sparing surgery for lower-extremity sarcoma. Pediatr Phys Ther. 2006;18:238–44.
Smith WA, Ness KK, Joshi V, Hudson MM, Robison LL, Green DM. Exercise training in childhood cancer survivors with subclinical cardiomyopathy who were treated with anthracyclines. Pediatr Blood Cancer. 2013. doi:10.1002/pbc.24850.
Edvardsen E, Skjønsberg OH, Holme I, Nordsletten L, Borchsenius F, Anderssen SA. High-intensity training following lung cancer surgery: a randomised controlled trial. Thorax. 2015;70:244–50.
Guimaraes-Ferreira L, Cholewa JM, Naimo MA, Zhi XI, Magagnin D, de Sá RB, et al. Synergistic effects of resistance training and protein intake: practical aspects. Nutrition. 2014;30:1097–103.
Vereeck L, Wuyts FL, Truijen S, De Valck C, Van de Heyning PH. The effect of early customized vestibular rehabilitation on balance after acoustic neuroma resection. Clin Rehabil. 2008;22:698–713.
Bekkering WP, Vliet Vlieland TP, Koopman HM, Schaap GR, Beishuizen A, Anninga JK, et al. A prospective study on quality of life and functional outcome in children and adolescents after malignant bone tumor surgery. Pediatr Blood Cancer. 2012;58:978–85.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Funding
This study was funded by Grant CA 21765 from the National Cancer Institute and ALSAC.
Animal rights
No animals were involved.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Fernandez-Pineda, I., Hudson, M.M., Pappo, A.S. et al. Long-term functional outcomes and quality of life in adult survivors of childhood extremity sarcomas: a report from the St. Jude Lifetime Cohort Study. J Cancer Surviv 11, 1–12 (2017). https://doi.org/10.1007/s11764-016-0556-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-016-0556-1