Abstract
Purpose
A critical initial step in work re-entry involves the determination of work readiness. Cancer survivors have requested increased health care provider involvement in their work readiness decisions. However, there has been no exploration of current practices in determining work readiness, and thus no specific recommendations regarding how to assist survivors in answering the question: Am I ready to return to work?
Methods
To explore return to work following cancer and the workplace supports survivors require, we completed an exploratory qualitative study. We conducted semi-structured interviews with (i) cancer survivors (n = 16) and (ii) health care/vocational service providers (n = 16). Data were analyzed using thematic analysis. Themes specific to work readiness are discussed.
Results
Three key processes were deemed relevant to determining work readiness by health care providers and survivors: (1) assessing functional abilities in relation to job demands; (2) identifying survivor strengths and barriers to return to work; and (3) identifying supports available in the workplace. Challenges to work readiness determinations, were described by survivors and providers, related to: (i) the complexity of cancer, (ii) the accuracy of work readiness determinations, and (iii) the lack of established processes for addressing work goals.
Conclusions
Health care providers need to work collaboratively with survivors to determine if they are physically, cognitively, and emotionally ready to return to work, and with workplaces to determine if they are prepared to provide the necessary supports. Further stakeholder collaboration is also warranted.
Implications for Cancer Survivors
Supports from health care providers in determining work readiness can ensure survivors do not return to work either “too early” or “too late.”
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Advancements in cancer screening, diagnosis, and treatment have led to increases in the numbers of individuals surviving cancer, with 63 % surviving at least 5 years following diagnosis [1]. For persons under 65 years of age, an indicator of working age, the overall survival rate is 70 % [2–4]. As such, the ability to return to work following cancer is now considered a key indicator of quality of life [5–14], with enhanced interest in determining how best to facilitate successful return to work [15]. Cancer survivors have expressed a motivation to return to work, citing many benefits to working including: (i) enhanced social engagement, competency, and control [6, 7, 10, 14, 16–20]; (ii) the ability to financially support oneself and one’s families [6, 10, 13, 16, 17, 20–27]; and (iii) the resumption of one’s worker role and identity [7, 10, 12, 14, 16–18, 23, 28–30].
However, despite strong motivations to work, cancer survivors continue to experience a 37 % higher risk of unemployment when compared with individuals without health concerns [31]. This may in part be due to on-going physical, cognitive, and psychosocial challenges that can affect their work abilities [2, 21, 26, 31–33] and in part due to the limited attention paid to providing work-related supports to cancer survivors across the cancer continuum [31, 34]. Studies have shown that cancer survivorship support services do not routinely address work-related goals, and that oncologists, and primary care physicians rarely provide adequate work-related advice, leaving cancer survivors to navigate and negotiate return to work issues independently [35, 36]. Similarly, survivors have reported receiving either no, or very limited, employment advice [6, 8, 16, 29, 37] and occupational health physicians have reported limited knowledge of how cancer may impact work abilities, and how to provide specific return to work recommendations [38, 39]. In Canada, where this study was conducted, there is great variability in the work-related supports that cancer survivors may be eligible to receive or have access to. Survivors who have access to private disability benefits, provided through their employer, may have access to a rehabilitation consultant or return to work facilitator. Survivors receiving income replacement supports through the publically funded national Canada Pension Plan disability or provincially funded programs (such as the Ontario Disability Support Program) may be able to access vocational rehabilitation services. Survivors who have acquired their cancer as a result of work-related environmental exposures can receive supports through the workplace compensation system (e.g., the Workplace Safety and Insurance Board in Ontario). Others may access vocational information or supports through community-based support programs, such as Wellspring, or hospital-based cancer services, where available.
An initial and critical step in work re-entry involves the determination of work readiness. Research with other populations, such as brain injury, has revealed that determining work readiness following an injury or an illness can be a complex process, and one that requires the integration of information on a worker’s abilities, the demands of his specific job, and the supports that can be made available at the workplace [40]. Cancer survivors have identified the determination of work readiness as a key priority in their return to work decision-making process [6, 8, 9, 13, 16, 19, 26, 28, 38, 39] and have requested that health care providers be more involved in advising them on their work readiness [19, 38, 39].
Decisions related to the timing of return to work can be made more difficult for a cancer survivor whose sense of responsibility and loyalty may lead them to return to work “too early,” or for cancer survivors whose prognosis and recovery process is unclear [16, 19, 27, 38]. Returning to work “too early” may create health and safety concerns, for some workers, and enhance the chance that the return to work process is unsuccessful [41–44]. On the other hand, returning to work “too late” may jeopardize an individual’s access to his/her pre-injury employment, and negatively affect resumption of his/her occupational role and financial stability; thus underscoring the importance of timely return to work and accurate determinations of work readiness.
Some key national and international cancer organizations, including Macmillan Cancer Support in the UK [45], and the Canadian Partnership Against Cancer in Canada [46] have recognized the importance of encouraging health care providers to discuss work issues as part of their treatment regime and have developed a work-related tool to guide survivors in understanding the types of questions they should be asking regarding work, as well as to whom specific questions should be directed [47]. It has also been suggested that cancer survivors achieve earlier and more successful return to work if physicians become aware of their patients work-related goals [48, 49], and if other health care and vocational service providers, such as occupational therapists and vocational counselors (trained in work and health issues), be employed more regularly to enhance work re-integration [36, 50]. In a Canadian context (in which this study takes place), determinations of work readiness are most frequently made between health care providers (e.g., physicians, occupational/vocational service providers) and cancer survivors. While recommendations for enhanced health care provider engagement in work-related decision have been made, there has been no direct exploration of current practices in relation to determining work readiness following cancer. Thus, there are no specific recommendations on how health care providers can work collaboratively with cancer survivors to determine when indeed they are ready to return to work. To fill this gap, in this study, we drew upon the perspectives of both health care service providers and cancer survivors to gain an understanding of the elements relevant to determining work readiness. Our two research questions were:
-
1.
What processes do health care providers, who address work-related goals, employ to determine work readiness in collaboration with cancer survivors?
-
2.
What challenges do health care providers, vocational service providers, and cancer survivors report experiencing when determining work readiness?
Method
Ethics approval for completion of this study was provided by research ethics review boards at the University Health Network and the University of Toronto. An exploratory qualitative research design was employed and data gathered using semi-structured interviews. Interviews were conducted either in-person, or by telephone, in accordance with the participant’s preference and to enhance availability as per participants’ work schedules.
Recruitment and inclusion criteria
Participants were recruited through hospital and community-based cancer survivorship programs, rehabilitation facilities, disability management and insurance companies, and snowballing techniques. As opposed to random sampling procedures, purposive sampling was utilized to draw upon the diverse experiential expertise of each of our three stakeholder groups. Purposive sampling is congruent with the aim of selecting individuals and situations where aspects of the phenomenon one wishes to consider are most prevalent [51]. Cancer survivors included individuals of working age (18–65) with various types of cancer, and those who had either stayed at work during their treatment, or returned to work following treatment. Service providers (e.g., health care providers, vocational service providers, community service providers/advocates) were included if they had assisted at least one cancer survivor to remain, or transition back to work. By engaging representatives from these varied perspectives, we aimed to build a comprehensive understanding of the elements relevant to determining work readiness and preparing cancer survivors to re-enter the workplace.
Sample description
Sixteen cancer survivors, three health care providers, and thirteen vocational service providers completed in-depth interviews (lasting between 60 and 150 min each). Participant demographic, employment characteristics, and cancer survivors’ diagnoses, are summarized in Table 1. Code numbers are assigned to protect participant confidentiality and preserve anonymity.
Data collection
Semi-structured interview guides were developed to collect data within each group. This semi-structured approach allowed the interviewer to focus discussions on the return to work process while remaining open to more specific participant insights regarding their roles in the process. More specifically, we asked survivors to discuss their cancer journey and decision-making in relation to work (including how they went about determining when they were ready to return to work), their experiences of working/returning to work, experiences with supervisors and co-workers at the workplace, and the supports, modification and/or accommodations they requested and were provided/not provided at the workplace. We asked providers to discuss how they assist survivors with their work-related goals, determining work readiness, if they have any concerns about cancer survivors’ abilities to work, how they assist in determining the most appropriate workplace supports and accommodations, and their successes and challenges when assisting cancer survivors with their work goals.
Data analysis
Interviews were digitally recorded and transcribed verbatim by a professional transcriptionist to ensure accuracy. Demographic and employment-related data, gathered at commencement of the interviews, was analyzed descriptively and utilized to characterize the study sample. An inductive thematic analysis approach was used to analyze the transcripts and identify themes within and across the interviews. This involved six key steps: (1) becoming familiar with the data by reviewing both audio tapes and transcribed interviews; (2) generating initial codes utilizing a line-by-line coding method; (3) categorizing codes into initial themes; (4) identifying the key themes related to the research objective and questions; (5) defining and naming the key themes; and (6) producing a scholarly report of the analysis [52]. To ensure a rigourous analysis process we employed the following trustworthiness strategies. Two qualitative researchers were involved in all stages of the data collection, coding and analysis [53]. Weekly meetings were held to discuss the interviews as they were completed, to explore emerging codes and to develop, refine, and reach consensus on key codes and themes. In addition, the collective expertise of our team drew on fields of occupational therapy, sociology, work rehabilitation, medicine, and cancer survivorship to enrich our interpretation of our data. Atlas Ti 5.0, a qualitative data management software program, was used to code the interviews and reflective memoing employed to make analytical decisions transparent [53–55].
Results
In this paper, we discuss two themes. In the first, we summarize current processes that health care providers engage in when determining work readiness. In the second, we illustrate the prominent challenges to determining work readiness as described by participants across our cancer survivor and provider groups.
Theme 1: processes relevant to determining work readiness
Three key processes were identified as relevant to determining work readiness: (1) assessing functional abilities in relation to job demands; (2) identifying survivor strengths and potential barriers to return to work; and (3) identifying supports available in the workplace. Each process is described below, with an explanation of its importance to determining work readiness and the approaches or tools used to gather relevant information at each step in the process.
Assessing functional abilities in relation to job demands
Gaining an understanding of cancer survivors’ functional abilities was at the forefront of providers’ evaluation processes when determining work readiness with cancer survivors. Functional abilities needed to be understood in relation to three domains—physical abilities, cognitive abilities and emotional capabilities. Health care providers explained how they needed to gain an understanding of whether or not a cancer survivors’ current abilities matched/fit the requirements of the essential tasks and duties of the job they would be returning to, as described by the following health care provider.
P9: I try and get a sense [of the] essential tasks and non-essential [elements of the job] and the physical environment … Are they standing all day long? Are they sitting? Are they having to lift something heavy? Are they having to bend? So I try and get into the details, break the job down into demands. And then looking at where the patient is at, and what’s the fit, between where the patient is at right now and what’s required of them [at the job].
An understanding of the fit between functional abilities and job demands was deemed relevant to determining additional skills that may need to be developed, or strategies that could be employed, prior to an individual being deemed ready to return to work. The following health care provider describes how she encourages survivors to identify issues they may experience in relation to their specific job demands, and strategies that can be applied to enhance their functional performance:
P13: [A survivor may say] “I [need to] give presentations and I can’t speak, what can I do?” Or it might be, “I just can’t speak, help!” So then I may have them think about how it [the challenge they are experiencing] would impact particular tasks that they have to do when they get back to work, [and] what [strategies] have they used in the past, what’s worked for them before? As opposed to sort of “Here’s general memory tips.”
Several approaches or tools were identified as being used by health care providers to assess functional abilities. The first included tools that assessed the level of impairment or disability, in physical and psychosocial domains as discussed below:
P9: In our clinics we use the DASH, the disability to arm and hand questionnaire [to assess upper extremity physical abilities]. It’s a very basic screen. It’s not necessarily an outcome measure in and of itself. But it can be used in that capacity [and] for new patients coming in they fill out that questionnaire for us. In other clinics they use the ESAS [Edmonton Symptom Assessment System], to look at different symptoms, like pain, like tiredness, like depression, anxiety. Cause these components’ can affect someone’s ability to go back to work.
Second, providers described utilizing cancer survivors’ self-reported abilities in relation to the performance of everyday activities, and monitoring physical tolerances and energy levels through journaling techniques:
P9: So again they [survivors] would have to keep some journals in terms of diaries of their energy level [throughout the day] … Or if [for example] they are walking they can count the number of steps they take.
Third, providers reported relying on family members’ accounts of cancer survivors’ functional capacity in day-to-day activities as a method of estimating a survivors’ potential capacity in the workplace:
P6: And then sometimes I have actually also found it helpful when people bring their spouses because the spouse [is] often a good person to comment on what things the person is doing at home. That could also be translated into what they could do at the workplace.
Identifying survivor strengths and potential barriers to return to work
In addition to assessing functional abilities, providers described the importance of gaining an understanding of the particular strengths a survivor was bringing to his/her work, any self-perceived barriers to returning to work, and/ or medically related limitations or restrictions (as identified by medical professionals) that would need to be adhered to. Due to perceived lack of detail in most medical documentation of restrictions, providers reported that they also specifically relied on discussions with survivors of any concerns they may have about returning to work and symptoms they believed may impair their abilities to return to work. Discussions of barriers were balanced with discussions of strength, in order to prepare survivors to focus more positively on the tasks they could perform, to build their confidence, and to envision themselves in a worker role, as described below:
P6: I view my role as understanding from the person, how work ready they feel [they are], and trying to improve their perception of work readiness. Often they will come in and [say] they can’t do anything - there is nothing that they can do when they go back to work. And by having a discussion and piecing out all the different tasks that they [currently] do, [they realize] there are some things that, maybe yes, I can do. And then I’m hoping by the end of our appointment they feel a bit more confident about what they can do.
Identifying supports available at the workplace
The need to determine if the workplace (and employers) would be able to support cancer survivors’ restrictions or accommodation needs was also deemed essential. Health care providers explained how direct communication with employers was optimal, but not necessarily standard practice for them due to cancer survivors’ concerns related to stigma and discrimination, and their own uncertainty about what information should or should not be shared with employers. The following provider explains how she does not communicate directly with employers:
P6: I’ve never called an employer to ask what someone’s job duties are …. [And] I’m really clear up front [with survivors that] what we talk about is not going to go to your employer, so don’t worry.
In the absence of direct communication with employers, providers explained determining workplace supports by relying on survivors perceptions of their work environment, supervisors/managers, and past employee/employer experiences with the return to work process:
P6: So I always ask people what they think will be possible in their workplace. For example some employers will never be open to the idea of working from home. So if this person tells me that this is not going to be possible, I wouldn’t suggest that. I hear what the issues are. I hear what the concerns are. I figure out what the person thinks is feasible in the workplace and then together with the patient we come up with some ideas of things that they could do. I also usually ask [the following]: Has anybody else at your workplace been off with a disability? How did that go? Do you know of any supports that are commonly used at your workplace?
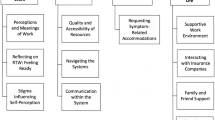
Theme 2: challenges to determining work readiness
While health care providers aimed to complete thorough evaluations, they also acknowledged multiple challenges that hampered the accuracy with which they could advise survivors as to their work readiness. These challenges were echoed by survivors and other vocational service providers in our sample and included the following: (i) challenges related to the complexity of cancer; (ii) challenges related to the accuracy of work readiness determinations (and best timing for return to work); and (iii) challenges related to a lack of established processes for addressing cancer survivors’ work goals. See Table 2 for an overview of challenges and descriptions below for details
Complexity of cancer
As health care providers stressed, the complexity of cancer (which often included physical, psychological/emotional, and cognitive trauma as well at the long-term side-effects of treatment) could make it difficult to accurately determine work readiness. Service providers, including vocational rehabilitation providers in both private (insurance) and public (community wellness centers) fields, also agreed that determining work readiness was more difficult with cancer survivors than other illness or injury groups:
P1: Sometimes it can be quite straightforward if it’s just a simple physical restriction and, you can go back to work once you can lift 20 pounds 10 times an hour. You can measure that, you can get a physio … you can sort of say yes you should be able to do that. But it is more complicated with cancer because there are a lot of levels [and] you want to make sure that all those gaps are addressed
Determinations of work readiness could be further challenged, as the following survivors explained, by a cancer survivors’ uncertain emotional state, the need to establish a “new normal” following cancer, and the need to balance the complexity of work while simultaneously managing one’s illness and restoring one’s health.
S14: I wasn’t even in a position to self-judge how bad it was. I wasn’t aware of where I was. Unfortunately nobody at either hospital I was treated at made any mention whatsoever about my mental health or psychological support or these [vocational and wellness] kind of programs.
S12: I’m back at work now. And the only thing that I feel literally [I need to do] every day is maintaining a far more rigid balance between sleep, food intake, and just being far more aware of what my body is telling me. I have to go to many more doctor appointments than I ever did before. And so it’s another reminder that it isn’t all about my job- it is also about looking after myself. So I think that there’s been a real shift internally around how I view my body and view my work life, and [the need to] get the balance back into play … Now I am very aware of the fact that there are times when my job requires me to be far more physical [and] my body is not quite there yet. Or it may never be again the same way it was prior to [cancer and] surgery. The new normal.
Accuracy of work readiness determinations
Challenges were also identified in relation to determining the best time to return to work and the accuracy of return to work determinations. Accuracy was perceived to be potentially hampered by five factors. First, many survivors reported challenges in identifying the best time to return to work due to vague messaging regarding their recovery process, and non-specific recommendations upon which to make realistic decisions.
S3: So when I was at the doctor’s, [I asked] what’s the normal recovery for this? And they [the doctors] would give me this wide range [of potential recovery time]. Once I was at the beginning of that range, I was like okay I should be better; I should be able to go back to work. ..It’s just really hard to tell… So I ended up going back when there was a sales conference and it was like getting thrown in the deep end.
Second, accuracy could be influenced by a tendency for survivors to over-estimate their work readiness when determinations were based exclusively on self-evaluation. Many survivors explained how their self-perceptions of their work readiness, in hindsight, were frequently unrealistic and an inaccurate reflection of their abilities. Inaccurate self-determinations of work readiness could in turn result in struggles to adhere to over-ambitious return to work plans, as described by the following survivor:
S1: I should have waited a little bit more. It was very difficult, my workplace wasn’t far from where I live, it was a 10 or 15 minute bus ride but I was basically leaving in the morning and then almost blacking out on the buses trying to get into work. So when I look back on it, I’m like, what was I thinking?
Third, strong personal motivations to return to work, arising from a desire to return to normal, a strong identity with one’s worker role, financial necessity, or concerns regarding job security could also influence cancer survivors’ decisions to return to work, frequently before they were fully ready, as illustrated by the following survivors:
S3: You are getting through that recovery … You are getting further away from the cancer diagnosis … [You say] okay that’s behind me now I want to go forward and have my normal life again. And that includes work.
S10: When the surgeon came into my room and said “You’re cancer free”, that was like a second lease on life. If I’m cancer free, you bet I want to go back to work because that’s who I am.
S2: I had to go back to work. There was no choice. Financially I have to work.
S15: I wanted to return to work as soon as possible. I felt the need to [return to work] because I wasn’t there for that long. But then at the same time, I didn’t really take that time to, I guess, adjust to my disability. I just kind of threw myself in there.
Fourth, cancer survivors’ personal motivations could be further re-enforced by messaging, within the cancer community, that return to work is a key indicator of success, and that one cannot let cancer control one’s life:
P11: The advice [I give survivors is] that by not getting back to their regular life, they are letting the cancer beat them, even though they are remitted at this point in time, they are a survivor. They [can’t] let cancer control their life. [They need to] learn, [and] find ways to change that mind set. [Move] towards getting back control of their life again [and] getting back to the way things were.
Fifth, the perceived inability to objectively assess functional work abilities was viewed as an additional limitation by health care providers:
P6: I don’t have the luxury of seeing them do their job which would be much more objective. So I just ask them what they do, ask them what they think they can do, what they think they can’t do. So it’s really just their perceptions that I’m getting. I’m not getting an accurate, objective assessment.
Lack of established processes for addressing survivors’ work goals
Three key larger systemic barriers were also identified as hampering work readiness decision-making. The first related to the lack of standardized tools, guidelines, or processes for evaluating work readiness within the current Canadian health care/hospital system. Health care provider 6 explains below that while the clinical templates she uses has a question or two pertaining to work and return to work, little instruction is provided on how to follow-up with survivors who express work-related concerns. Follow-up on work concerns became a matter of discretion, and providers whose training may be more suitably apt to addressing vocational issues (e.g., occupational therapy) are more likely to provide additional follow-up care.
P6: So standard [practice] is [that] there’s a section in our [reporting] template that says return to work. So I know all of us ask about it, but I think just because I’m more interested in this, I probably delve into it more than other [providers] would.
Recommendations regarding work readiness could also be hampered by the lack of available resources (such as funding) to complete more in-depth functional abilities evaluations, as discussed by the following vocational service provider
P3: In some cases I encourage doctors to ask for assessments, physical, functional capacity evaluations. But right now in our health care system it’s not provided. We don’t have that access [to functional capacity evaluations], [unless] it has to be asked for from a third party insurance provider. So I encourage physicians to say I am not going to clear this person [to return to work]… I think he needs to get this [additional] opinion [functional evaluation]. But sadly that’s not available for someone who doesn’t have LTD [long-term disability coverage].
The second challenge related to inconsistencies in health care providers’ understanding of how the complexity of cancer could impact their work abilities. This could in turn result in similar recommendations made for all cancer survivors or inconsistent messaging regarding work readiness between different health care providers as illustrated below:
P6: The message I hear a lot is, [the] oncologist, who is not wrong, but will tell patients the sooner you go back to work, to full time duties, full time hours, the easier it’s going to be. And there is not always that understanding of what a person’s actual activities are in the workplace. So they [oncologists] are making that recommendation, obviously with good intentions, but they don’t always, I feel, understand the repercussion on the patient and how they take that doctor’s word so seriously.
Third, were expressed concerns about poor support for communication and collaborations between health care providers and community vocational support programs that could fill the current gaps in work-related supports. Survivors frequently explained that physicians had a responsibility, as their primary care providers within the cancer continuum, to refer them to providers and/or programs that assist with return to work concerns. For example, the following survivor discussed the importance of knowing his rights in advance of beginning the return to work process, and the importance of survivorship support programs, such as Wellspring, in facilitating the acquisition of work-related knowledge:
S14: I would never let anybody I know around me settle with an insurance company without first talking to a counsellor, even if I had to drag them into Wellspring myself and say you don’t have to do anything else that this place offers but you need to have an hour with like somebody who knows [about your rights to be accommodated]. Because that single decision to sign a return to work[plan] impacts not just the duration of the return to work but whether it’s months or years after, it’s just a huge thing. So that would be my big advice.
Discussion
To the best of our knowledge this is the first in-depth exploration of current processes employed to determine work readiness from health care provider and survivor perspectives that also employs a thorough investigation of the challenges to this process, as identified by health care providers, vocational service providers’ and survivor perspectives. Our findings reveal a number of factors that require consideration when evaluating work readiness following cancer. First, we have learned that the complexity of cancer requires providers and survivors to carefully consider how on-going physical, cognitive and psychosocial challenges may interact to impact work success following cancer. Research evidence examining the association between specific physical, cognitive and psychosocial impairments and successful work outcomes following cancer may provide a good starting point in mitigating existing knowledge gaps and assisting health care providers in understanding the key elements that require in-depth assessment (see references [21, 26, 31–33] for examples).
Second, we have learned that it is important that health care providers and survivors build a shared understanding of whether or not a survivor’s functional abilities (in physical, cognitive, and emotional domains) currently align with his/her specific job demands. This is in line with investigations of work readiness determinations in other complex disability groups, such as brain injury [40]. Establishing an understanding of work readiness requires health care providers to evaluate both the survivor’s functional abilities and his/her job demands, prior to recommending that a survivor is indeed ready to return to work. Blanket recommendations that all survivors will be able to return to full time work, once treatment has been completed, may prove detrimental to some survivors.
Third, a survivor’s functional abilities needs to be considered in relation to the survivor’s perceived barriers to returning to work, the personal strengths he/she brings to the situation, and the specific supports that can be made available in the workplace to compensate for on-going, long-term challenges. While work readiness has predominately been conceptualized (in the broader occupational injury and illness literature) as a motivational issues that requires injured or ill workers to make behavioral changes in order to be motivated to return to work [56], our findings suggest that motivation may not be the primary issue influencing cancer survivors’ work readiness. In fact, based on our findings, we postulate that work readiness may be a much more complex and multifactorial construct following cancer—one that requires careful consideration of a survivor’s physical, cognitive, and emotional readiness, and the supports that can be made available within the workplace. In addition, our data suggests it may be necessary for us to begin to ask not only, “Is this survivor ready to return to work?” but also “Is the workplace ready to support the survivor back to work?” This may in turn require health care providers and survivors to initially communicate with relevant workplace parties to identify key supports that can be made available within the workplace. Care must be taken to ensure communication is completed in accordance with one’s work context and jurisdiction-specific privacy policies. Survivors and providers can subsequently integrate information related to the workplace to guide their work readiness decision-making processes.
By drawing on the perspectives of various stakeholders, our findings also enliven the many challenges or pitfalls that can be encountered in current evaluation processes, and thus should be considered when determining work readiness with cancer survivors. First and foremost, our findings illustrate that work readiness determinations can be challenging for survivors to make on their own, and that such determinations frequently require the assistance of health care or vocational service providers, and the use of a variety of tools, approaches and perspectives (e.g., survivors, family, provider, objective assessments) to enhance accuracy.
Second, we have learned how strong motivations to return to work, enhance the probability that many survivors will choose to return to work before they are fully ready. Relying solely on cancer survivors’ self-evaluations may enhance the likelihood that survivors return to work “too early.” This was clearly illustrated in survivors’ reflections that, in hindsight, they should have remained off work longer. For some, delaying return to work may have resulted in a less stressful return to work process and additional time to feel emotionally ready to return to work. Evidence in the broader return to work literature also cautions against returning to work “too early” citing a number of potential negative consequences to workers’ health including enhanced psychological stress, and increased risk of re-injury [41–44]. Lastly, our findings emphasize the importance of consistent communication, and messaging between the various members of the health care team, as well as between health care and community service providers, to improve both the accuracy of work readiness determinations and the specificity of return to work recommendations. The significance of team communication and collaborations to successful work outcomes is also strongly supported by research evidence [57–60].
Recommendations
Based on our study findings, we offer several key recommendations to health care and vocational service providers who work in collaboration with cancers survivors to determine their work readiness. We begin by suggesting that increased contact with employers and direct communication with the workplace can ensure that health care providers have the most up to date knowledge regarding job demands and specific details as to the workplace culture and the supports that can be made available in the workplace. This will ensure that work readiness determinations not only focus on the cancer survivors’ readiness but also understanding the workplace’s preparedness to facilitate a successful transition back to work. Since emotional readiness was viewed by the majority of our survivors as a key indicator to their potential work success, we would also like to suggest that much greater attention be paid to assessing emotional health and functional ability in determining work readiness. This echoes many cancer survivors’ suggestions that further attention be directed to informing and referring survivors to community-based psychosocial and vocational support programs, such as Wellspring.
As indicated by other researchers and organizations interested in work following cancer (see, for example, references [36, 41, 42, 45]), we identify the need to develop more systematic processes for advising survivors regarding work readiness and assisting them in addressing their work-related goals. This should include multi-disciplinary services, referrals for specialized functional and work abilities evaluations and community-based vocational support services. A collaborative approach that includes physicians to provide medical guidance, psychologists to address emotional health concerns, neuropsychologists to assist with cognitive issues, occupational therapists to evaluate functional abilities, and vocational counselors to evaluate alternative vocational options is also recommended. Lastly, from a motivational perspective it is important for both providers and survivors to understand how strong motivations to return to work (and a desire to have one’s life return to normal), can lead some individuals to return to work “too early.” We recommend that work readiness decisions be carefully discussed with survivors and evidence from various sources be utilized to enhance the accuracy of decisions made.
Strengths, limitations, and recommendations for future research
A key strength of this study is that it draws on the expertise and perspective of survivors themselves and health care providers who, as part of their role, assist survivors with assessing their work readiness. Building on this expertise and knowledge we have identified a number of concrete factors that should be considered when making decisions regarding work readiness following cancer that can be utilized to guide clinical practice. There are however some limitations that readers need to be aware of when applying these findings. First, due to the limited number of cancer survivorship programs that exist across Canada (where this study took place), that address work related issues in a systematic fashion, we had a very select number of health care providers to draw from. As such, the perspectives of other service providers are used to supplement our understanding of the challenges of the work readiness evaluation process. Future studies will need to validate our findings with a larger sample of health care providers and survivors and explore decision-making processes across varied countries, as return to work policies may vary across jurisdictions. Second, as our health care provider participants represent those with specific interest and expertise in cancer and work, the services they provide may be an over-estimate of work-related services that all cancer survivors may receive. Third, as our survivor participants included individuals that were relatively well-educated and involved primarily in non-manual occupations, further research is required to explore work readiness decisions amongst survivor across occupational categories. In addition, further research is required to test and validate the processes identified in this study in order to evaluate their ability to effectively and accurately identify cancer survivors’ work readiness. Fourth, despite efforts to recruit physicians, and more specifically oncologists, no oncologist chose to participate. As such future studies should examine oncologists’ practices in relation to determining work readiness and fitness to return to work. Lastly, while employer representative were also interviewed to gain their perspective on how they support cancer survivors’ return to work, employers did not discuss their role in determining work readiness in this study. Hence, no data were available in this study from which to discuss employers’ roles specific to work readiness determinations. Future research needs to explore further the role, or potential role of employers in assisting with return to work decision-making processes following cancer.
Conclusions
To date, there has been no direct exploration of current practices in relation to determining work readiness following cancer, and thus no specific recommendations on how health care providers can assist cancer survivors to determine when indeed they are ready to return to work. In this paper, we describe key processes that health care providers deem relevant to determining work readiness. Building on further discussions across health care providers, vocational service providers and cancer survivors we also elucidate challenges associated with determining work readiness. Key stakeholder discussions of processes and challenges are subsequently used to inform specific recommendations to help ensure that cancer survivors do not return to work either “too early” or “too late.” These include recommendations for enhancing inter-stakeholder evaluation, and collaborations between health care providers, employers, and community support programs.
References
Canadian Cancer Society. Cancer Statistics at a Glance. 2015. Available at http://www.cancer.ca/en/cancer-information/cancer-101/cancer-statistics-at-a-glance/?region=on
Neary D. Epidemiology. In: Feuerstein M, editor. Work and cancer survivors. New York: Springer; 2011. p. 3–23.
Farley Short P, Vasey J, Tunceli K. Employment pathways in a large cohort of adult cancer survivors. Cancer. 2005;103(6):1292–301.
Spelten E, Sprangers M, Verbeek J. Factors reported to influence the return to work of cancer survivors: a literature review. Psycho-Oncology. 2002;11:124–31.
Morrison T, Thomas R. “Bored out of my gourd”: a cancer Survivor’s return to work experience. Curr Oncol. 2014;21(1):e169–71. doi:10.3747/co.21.1665.
Amir Z, Neary D, Luker K. Cancer survivors’ views of work 3 years post diagnosis: a UK perspective. Eur J Oncol Nurs. 2008;12(3):190–7.
Frazier LM, Miller VA, Horbelt DV, Delmore JE, Miller BE, Averett EP. Employment and quality of survivorship among women with cancer: domains not captured by quality of life instruments. Cancer Control. 2009;16(1):57–65.
Groeneveld IF, de Boer AG, Frings-Dresen MHW. Physical exercise and return to work: cancer survivors’ experiences. J Cancer Surviv. 2013;7(2):237–46.
Grunfeld EA, Drudge-Coates L, Rixon L, Eaton E, Cooper AF. “The only way I know how to live is to work”: a qualitative study of work following treatment for prostate cancer. Health Psychol. 2013;32(1):75–82.
Grunfeld EA, Cooper AF. A longitudinal qualitative study of the experience of working following treatment for gynaecological cancer. Psychooncology. 2012;21(1):82.
Munir F, Kalawsky K, Lawrence C, Yarker J, Haslam C, Ahmed S. Cognitive intervention for breast cancer patients undergoing adjuvant chemotherapy: a needs analysis. Cancer Nurs. 2011;34(5):385–92.
Nachreiner NM, Dagher RK, McGovern PM, Baker BA, Alexander BH, Gerberich SG. Successful return to work for cancer survivors. AAOHN J. 2007;55(7):290–5.
Nilsson M, Olsson M, Wennman-Larsen A, Petersson L, Alexanderson K. Return to work after breast cancer: women’s experiences of encounters with different stakeholders. Eur J Oncol Nurs. 2011;15(3):267–74.
Picard C, Agretelis J, DeMarco RF. Nurse experiences as cancer survivors: part II—professional. Oncol Nurs Forum. 2004;31(3):537–42.
Aziz NM. Cancer survivorship research: state of knowledge, challenges and opportunities. Acta Oncol. 2007;46(4):417–32.
Kennedy F, HaslamC MF, Pryce J. Returning to work following cancer: a qualitative exploratory study into the experience of returning to work following cancer. Eur J Cancer Care (Engl). 2007;16(1):17–25.
McKay G, Knott V, Delfabbro P. Return to work and cancer: the Australian experience. J Occup Rehabil. 2013;23(1):93–105.
Tiedtke C, Dierckx de Casterlé B, de Rijk A, Christiaens M, Donceel P. Breast cancer treatment and work disability: patient perspectives. Breast (Edinburgh, Scotland). 2011;20(6):534–8.
Tiedtke C, de Rijk A, Donceel P, Christiaens M, de Casterle BD. Survived but feeling vulnerable and insecure: a qualitative study of the mental preparation for return to work after breast cancer treatment. BMC Public Health. 2012;12(1):538.
Johnsson A, Fornander T, Rutqvist LE, Olsson M. Factors influencing return to work: a narrative study of women treated for breast cancer. Eur J Cancer Care. 2010;19(3):317–23.
Tamminga SJ, de Boer AG, Verbeek JH, Frings-Dresen MH. Breast cancer survivors’ views of factors that influence the return-to-work process—a qualitative study. Scand J Work Environ Health. 2012;38(2):144–54.
Amir Z, Wilson K, Hennings J, Young A. The meaning of cancer: implications for family finances and consequent impact on lifestyle, activities, roles and relationships. Psychooncology. 2012;21(11):1167–74.
Blinder VS, Murphy MM, Vahdat LT, Gold HT, de Melo-Martin I, Hayes MK, et al. Employment after a breast cancer diagnosis: a qualitative study of ethnically diverse urban women. J Community Health. 2012;37(4):763–72.
Ferrell BR, Smith SL, Ervin KS, Itano J, Melancon C. A qualitative analysis of social concerns of women with ovarian cancer. Psychooncology. 2003;12(7):647–63.
Fu MR. Women at work with breast cancer-related lymphoedema. J Lymphoedema. 2008;3(1):20–5.
Main DS, Nowels CT, Cavender TA, Etschmaier M, Steiner JF. A qualitative study of work and work return in cancer survivors. Psychooncology. 2005;14(11):992–1004.
Timmons A, Gooberman-Hill R, Sharp L. The multidimensional nature of the financial and economic burden of a cancer diagnosis on patients and their families: qualitative findings from a country with a mixed public-private healthcare system. Support Care Cancer. 2013;21(1):107–17.
Parsons J, Eakin JM, Bell RS, Franche RL, Davis AM. So, are you back to work yet? Re-conceptualizing ‘work’ and ‘return to work’ in the context of primary bone cancer. Soc Sci Med. 2008;67(11):1826–36.
Schmalenberger S. Working after breast cancer treatment: lessons from musicians. Med Probl Perform Art. 2012;27(4):175–80.
Tan FL, Loh SY, Su TT, Veloo VW, Ng LL. Return to work in multiethnic breast cancer survivors—a qualitative inquiry. Asian Pac J Cancer Prev APJCP. 2012;13(11):5791–7.
de Boer AG, Taskila T, Ojajarvi A, Van Dijk FJ, Verbeek JH. Cancer survivors and unemployment: a meta-analysis and meta-regression. JAMA. 2009;301(7):753–62.
de Boer A, Verbeek J, Uitternoeve A, Ansink A, de Reijke T, Mameijer M, et al. Work ability and return-to-work in cancer patients. Br J Cancer. 2008;98(8):1342–7.
Mehnert A. Employment and work-related issues in cancer survivors. Clin Rev Oncol Hematol. 2011;77:109–30.
Hoving JL, Broekhulzen ML, Frings-Dresen MH. Return to work of breast cancer survivors: a systematic review of intervention studies. BMC Cancer. 2009;9:117–27.
Morrison T, Thomas R, Guitard P. Physicians’ perspectives of cancer survivors’ work integration. Can Fam Phys. 2015;61:e36–42.
Morrison T, Thomas R. Survivors’ experiences of return to work following cancer: a photovoice study. Can J Occup Ther. 2014;81(3):163–72.
Bains M, Yarker J, Amir Z, Wynn P, Munir F. Helping cancer survivors return to work: what providers tell us about the challenges in assisting cancer patients with work questions. J Occup Rehabil. 2012;22(1):71–7.
Tiedtke C, Donceel P, Knops L, Désiron H, Désiron H, Dierckx De Casterlé B, et al. Supporting return-to-work in the face of legislation: stakeholders’ experiences with return - to- work after breast cancer in Belgium. J Occup Rehabil. 2012;22(2):241–51.
Stergiou-Kita M, Grigorovich A, Tseung V, Milosevic E, Hebert D, Phan S, et al. Qualitative meta-synthesis of survivors’ work experiences and the development of strategies to facilitate return to work. J Cancer Surviv. 2014;8(4):657–70.
Stergiou-Kita M, Rappolt S, Kirsh B, Shaw L. Evaluating work readiness following acquired brain injury: building a shared understanding. Can J Occup Ther. 2009;78(4):276–84.
MacEachen E, Ferrier S, Kosny A, Chambers L. A deliberation on ‘hurt versus harm’ logic in early-return-to-work policy. Pol Prac Health Saf. 2007;5(2):41–62.
Eakin JM, MacEachen E, Clarke J. ‘Playing it smart’ with return to work: small workplace experience under Ontario’s policy of self-reliance and early return. Policy Pract Health Saf. 2003;1(2):19–41.
Mansfield E, Stergiou-Kita M, Kirsh B, Colantonio A. After the storm: the social relations of return to work following electrical injury. Qual Health Res. 2014;24(9):1183–97.
Mansfield E, Stergiou-Kita M, Cassidy D, Bayley M, Mantis S, Kristman V, et al. Return-to-work challenges following a work-related mild TBI: the injured worker perspective. Brain Inj. 2015;29(11):1362–9.
MacMillan Cancer Support. Work and Cancer. Available at http://www.macmillan.org.uk/information-and-support/organising/work-and-cancer
Nitkins P, Parkinson M, Schultz I. Cancer and work: a Canadian perspective. 2011. Available at http://www.capo.ca/pdf/CancerandWork-ACanadianPerspective.pdf.
Munir F, Kalawsky K, Wallis D, Donaldson-Feilder E. Using intervention mapping to develop a work-related guidance tool for those affected by cancer. BMC Public Health. 2013;13(6):1–13.
Verbeek J, de Boer A, Taskila T. Primary and occupational health care pro- viders. In: Feuerstein M, editor. Work and cancer survivors. New York: Springer; 2011. p. 191–209.
Wada K, Ohtsu M, Aizawa Y, Tanaka H, Tagaya N, Takahashi M. Awareness and behavior of oncologists and support measures in medical institutions related to ongoing employment of cancer patients in Japan. Jpn J Clin Oncol. 2012;42(4):295–301.
Desiron H, Donceel P, de Rijk A, Van Hoof E. A conceptual-practice model for occupational therapy to facilitate return to work in breast cancer patients. J Occup Rehabil. 2013;23(4):516–26.
Creswell JW. Research design: qualitative, quantitative, and mixed methods approaches. 3rd ed. Los Angeles: Sage Publications, Inc; 2009.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Seale C. Quality in qualitative research. Qual Inq. 1999;5.
Charmaz K. Constructing grounded theory. Thousand Oaks: Sage; 2006.
Mays N, Pope C. Qualitative research in health care: assessing quality in qualitative research. BMJ. 2000;320(7226):50–2.
Franche R, Krause N. Readiness to return to work following injury or illness: conceptualizing the interpersonal impact on health care, workplace and insurance factors. J Occup Rehabil. 2002;12(4):233–56.
Larsson A, Gard G. How can the rehabilitation planning process at the workplace be improved? A qualitative study from employers’ perspective. J Occup Rehabil. 2003;13(3):169–81.
Young AE. Return to work stakeholders’ perspectives on work disability. In: Loisel P, Anema JR, editors. Handbook of work disability. New York: Springer; 2013. p. 409–23.
Young A, Wasiak R, Roessler R, McPherson T, Anema K, van Poppel J. Return -to- work outcomes following work disability: stakeholder motivations, interests and concerns. J Occup Rehabil. 2005;15(4):543–56.
Stahl C, Svensson T, Petersson G, Ekberg K. A matter of trust? A study of coordination of Swedish stakeholders in return-to-work. J Occup Rehabil. 2010;20(3):299–310.
Acknowledgments
This study was supported by a grant through the Dean’s Fund, Faculty of Medicine, University of Toronto. We would like to express our gratitude to the cancer survivors and service providers who shared their time, expertise and experiences to help us understand work readiness. We would also like to acknowledge the assistance of Well spring for their assistance with recruitment.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in this study, involving human participants, were in accordance with the ethical standards and approval from the ethics review boards at the University of Toronto and the University Health Network, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Funding
This study was supported by a grant through the Dean’s Fund, Faculty of Medicine, University of Toronto (award no. DF-2013-17).
Conflict of interest
All authors of this paper have no conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Stergiou-Kita, M., Pritlove, C., Holness, D.L. et al. Am I ready to return to work? Assisting cancer survivors to determine work readiness. J Cancer Surviv 10, 699–710 (2016). https://doi.org/10.1007/s11764-016-0516-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-016-0516-9