Abstract
Purpose
Survivorship care plans (SCPs) provide cancer patients and health care providers with a treatment summary and outline of recommended medical follow-up. Few studies have investigated the information needs and preferred sources among long-term cancer survivors.
Methods
Cancer survivors of the ten most common cancers enrolled in the longitudinal Study of Cancer Survivors-I (SCS-I) completed a survey 9 years post-diagnosis (n = 3138); at time of diagnosis of the SCS-I cohort, SCPs were not considered usual care. We assessed participants’ current desire and preferred sources for information across ten SCP items and evaluated factors associated with information need 9 years after diagnosis.
Results
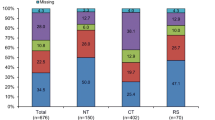
The proportion of long-term cancer survivors endorsing a need for cancer and health information 9 years post-diagnosis ranged from 43 % (cancer screening) to 9 % (consequences of cancer on ability to work). Print media and personalized reading materials were the most preferred information sources. Younger age, higher education, race other than non-Hispanic white, later cancer stage, having breast cancer, having ≥2 comorbidities, and self-reporting poor health were associated with greater informational need (p < 0.05).
Conclusions/Implications for Cancer Survivors
Long-term cancer survivors continue to report health information needs for most SCP items and would prefer a print format; however, level of need differs by socio-demographic and cancer characteristics. Cancer survivors who did not previously receive a SCP may still benefit from receiving SCP content, and strategies for enabling dissemination to long-term survivors warrant further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although incidence rates are declining for many cancers, an aging population, earlier diagnosis, and better treatment have led to a rapidly increasing number of long-term cancer survivors in the USA and worldwide [1–3]. The majority of people diagnosed with cancer now survive 5 years or more [4]. Long-term cancer survivors, most of whom will be aged >65 years in the next decade, continue to encounter physical, emotional, social, and financial challenges as they transition through the cancer survivorship trajectory, yet little is known about the health information needs of this population from the patients’ perspective [5]. In the past, cancer survivors have not systematically received written information regarding recommendations for long-term follow-up that address these challenges. However, accreditation standards from the Commission on Cancer (CoC) of the American College of Surgeons require that by 2015, all cancer centers seeking CoC accreditation must provide a survivorship care plan (SCP) or treatment summary and follow-up plan after completion of primary treatment [6, 7]. SCPs summarize multiple health information domains, including describing cancer diagnosis and treatment and their potential long-term side effects, providing a cancer surveillance plan and advice on health promotion, and highlighting supportive community resources [8]. As the content and format of SCPs continue to evolve and their use becomes more widespread, an accurate representation of information needs from the patients’ perspective is critical.
Providing cancer and health-related information that is understandable from the patient’s perspective improves patient involvement in health care decision-making, satisfaction with health care, coping skills, and communication with family and caregivers and reduces anxiety and mood disturbance [9]. Satisfaction with cancer-related information provision is associated with better overall health-related quality of life and psychosocial health outcomes including depression [10–12]. In contrast, cancer survivors with unmet information needs are more likely to experience psychological distress [13] and lower emotional, functional, social or family well-being, and perception of health competence [10]. Consequently, understanding and meeting the informational needs of cancer survivors is of high public health importance.
Health information needs of cancer survivors may change following active treatment [14–16]. However, the majority of the literature on this topic has focused on information needs and sources in short-term cancer survivors at diagnosis and treatment; few studies have assessed if SCP domains align with the information needs and preferences of long-term cancer survivors in the post-recovery and remission phases of the cancer trajectory [9]. Additionally, the preferred mode of delivery for this information is unclear, yet some research suggests that both needs and preferred information sources shortly after cancer diagnosis and treatment differ by socio-demographic groups and cancer type [13, 17–28]. Characterization of the factors associated with long-term cancer survivors’ information needs and preferred sources would support a better understanding of the suitability of SCPs for the most diverse group of cancer survivors. This information would support future investigations of the impact of SCPs on outcome measures that are consistent with SCP content, such as uptake of cancer screening and cancer-related comorbidity, which have been limited to date [29]. Improving understanding of patient preferences for content and dissemination methods may also advance implementation and acceptability of SCPs in practice [30].
We assessed health information needs specific to SCP domains and preferences for various information sources among a nationwide, population-based sample of cancer survivors 9 years post-diagnosis who participated in the longitudinal American Cancer Society Study of Cancer Survivors-I (SCS-I). This group of cancer survivors, who did not receive SCPs at the time of their primary cancer since SCPs were not considered usual care, was asked to assess their current cancer information needs. Specifically, we asked them what type (content) of cancer information and delivery modalities would be most helpful 9 years after diagnosis. We also examined variation in the above needs and preferences by socio-demographic, clinical, and lifestyle characteristics.
Methods
Study population
We utilized data from the full national sample of the American Cancer Society’s longitudinal SCS-I to evaluate health information-seeking behaviors of a population-based sample of cancer survivors, described in detail previously [31]. A total of 6305 adult (>18 years) cancer survivors with the ten most common cancers (breast, prostate, colorectal, lung, ovarian, melanoma, uterine, non-Hodgkin’s lymphoma, kidney, and bladder) were identified and enrolled from central cancer registries in 11 states. Samples were age-stratified (<55 and over 55 at diagnosis), and racial/ethnic minorities, those under 55 years old, and certain cancers were over-sampled [31]. At baseline, participants who were approximately 1 year post-diagnosis completed a mailed, self-administered questionnaire on a wide range of characteristics, including socio-demographic factors, medical history, cancer treatment, lifestyle factors, and psychosocial measures. Clinical characteristics, such as cancer stage and date of diagnosis, were obtained from the state cancer registries. Institutional review board (IRB) approval was obtained from Emory University. Additional IRB approvals were obtained from each state’s cancer registry [32].
The study has administered three surveys in total: the baseline (individuals enrolled at approximately 1 year post-diagnosis) and two follow-up surveys (approximately 2 and 9 years post-diagnosis) (Fig. 1). The majority of the three surveys were completed by mail, with a small number administered via telephone. The current analysis focuses on data gathered from the third survey completed by 3138 survivors in the national sample (70 % response rate for eligible participants) approximately 9 years post-diagnosis.
Assessment of health information needs and preferences
The outcomes of interest were level (% responding yes) of need for ten health information domains. All participants were asked about their current information needs at 9 years post-diagnosis for topics derived from the recommended components of a SCP and its method of development (response options: yes, no-receive adequate information, no-do not need information). The topics were (1) possible long-term side effects of the treatment you received, (2) tests and examinations you should have following completion of treatment, (3) cancer screening tests you should have for other types of cancer, (4) behaviors you should adopt to be more healthy (e.g., diet, exercise), (5) possible consequences of having had cancer on your health insurance or finances, (6) possible consequences of having had cancer on your ability to continue to work in your job, (7) cancer-related resources and information, (8) impact of the psychological burden of cancer on yourself and your family, (9) information on the skills family and caregivers can use to support you, and (10) a cancer survivorship care plan you and your doctor would create together. Preferences for health and cancer-related information sources/format were assessed in the national sample using survey questions based on the Health Information National Trends Survey (HINTS) [33].
Statistical analysis
Selected participant characteristics, current information needs, and preferred information sources were evaluated using basic descriptive statistics. We assessed unadjusted associations with the number of informational needs (≥2 vs <2 needs—dichotomized at the mean) identified at 9 years post-diagnosis and (1) demographic characteristics [age (<55/≥55 years at diagnosis; this age cut point was selected as those <55 were oversampled in the original design), sex, race/ethnicity (non-Hispanic white/other), education (high school or less/some college/college/graduate degree), employment (employed/unemployed/retired), income (<$40,000/$40,000–$75,000/>$75,000 per year), marital status (married/separated or divorced/single/widowed), health insurance (yes/no)] and medical care provision within the previous 2 years (both primary and specialist care/primary care only/specialist care only/neither primary nor specialist care/missing or unsure); (2) clinical characteristics [cancer type (breast/prostate/colorectal/lung/ovarian/melanoma/uterine/non-Hodgkin’s lymphoma/kidney/bladder), primary cancer stage (in situ or local/regional/distant), cancer status (cancer-free/cancer), cancer diagnosis or treatment past 5 years (yes/no), number of chronic conditions (0/1/≥2), and self-reported health (excellent/very good/good/fair or poor)]; and (3) lifestyle characteristics [(alcohol intake (none/up to one drink per week/up to five drinks per week/up to three drinks per day), body mass index (<18.5/18.5–<25/25–<30/30–<35/35–<40/≥40 kg/m2), physical activity level (none/<150 min per week/≥150 min per week), smoking (never/former/current), fruit and vegetable intake (≤1 day per week/2–3 days per week/4–5 days per week/6–7 days per week)] using X 2 tests. Demographic and cancer characteristics were derived from the baseline questionnaire. Income in the previous year, health insurance coverage, time since cancer diagnosis and current cancer status, comorbidities, self-reported health, diet, exercise, alcohol, body mass index, and smoking status were derived from the third survey at 9 years post-diagnosis. Multivariate logistic regression analyses were conducted to determine the independent effects of any characteristics that were significantly associated with level of need (<2 needs vs ≥2 needs) in univariate analyses with α< 0.05. We derived the most parsimonious multivariate model using backwards elimination, and we retained only those variables that were associated with level of need with an α< 0.05. All analyses were conducted using SAS (version 9.2, Cary, NC).
Results
The mean age of the 3138 long-term cancer survivors in the current analysis was 65.8 ± 11.6 years (Table 1), and they were an average of 8.9 ± 0.7 years since diagnosis. The majority was female (59.7 %) and non-Hispanic white (88 % non-Hispanic white, 6 % non-Hispanic black, 3 % Hispanic, 2 % other). Over half of participants had at least some college education (60.5 %) and an annual income >$40,000 (53.3 %). Almost all participants had health insurance (97 %). The majority of participants were treated by both primary and specialist care providers within the previous 2 years (50 %); overall, 86 % had seen a primary care provider (PCP) within this period. Approximately one fifth (22.2 %) of survivors had a cancer recurrence or received further treatment during the 5-year period prior to completing the follow-up questionnaire. Two thirds of long-term cancer survivors had ≥2 chronic conditions (68.9 %), although most (80 %) self-reported that they were in good to excellent health.
Approximately 9 years post-diagnosis, 42.5 % cancer survivors reported that they would currently like to have more information on cancer screening tests for other types of cancers; 33.1 % would like more information on long-term cancer side effects, while 31.9 % would currently like more information on healthy lifestyle behaviors (Table 2). A similar proportion would like more information on possible consequences of having had cancer on health insurance or finances (28.2 %) and tests and examinations they should receive following cancer treatment (27.0 %).
Participants reported on how they would like to receive cancer information (Table 3). Reading a book, magazine, or other printed publication was most popular (60.9 %), followed by personalized reading materials (57.6 %). Meeting in person with a health care professional was the third preferred source of cancer information (44.4 %), and receiving information by email or internet was ranked lower (40.1 %). Overall, 84 % of responders were internet users (of these, 55 % were aged <55 years, and 45 % were aged ≥55 years at diagnosis). Preference for each type of information source differed by age and education level (p < 0.05). Those aged <55 years at diagnosis and those with higher educational attainment were more likely to indicate a preference for each source in comparison with those aged >55 years at diagnosis (data not shown).
We evaluated factors associated with greater informational need (≥2 vs <2 needs) 9 years post-diagnosis (Table 4). In multivariate analyses, age, race/ethnicity, education level, cancer type and stage, number of chronic conditions, and self-reported health were significantly associated with number of information needs. Those aged <55 at diagnosis were twice as likely to have a greater number of information needs compared with the older age group (≥55 years at diagnosis) (OR 0.45, 95 % CI 0.38, 0.54). Participants of race/ethnicity other than non-Hispanic white were 79 % more likely to have greater information needs compared with non-Hispanic whites (OR 1.79, 95 % CI 1.36, 2.36). Education level was also associated with greater information need. Participants with some college (OR 1.55, 95 % CI 1.25, 1.93), who completed college (OR 1.55, 95 % CI 1.23, 1.96), or a graduate degree (OR 1.62, 95 % CI 1.27, 2.06) reported greater informational needs compared with those that completed high school or less. Prostate (OR 0.61, 95 % CI 0.48, 0.77) and colorectal cancer survivors (OR 0.56, 95 % CI 0.42, 0.75) and survivors of uterine (OR 0.62, 95 % CI 0.44, 0.89), melanoma (OR 0.50, 95 % CI 0.35, 0.73), kidney (OR 0.59, 95 % CI 0.41, 0.84), and lung cancer (OR 0.46, 95 % CI 0.29, 0.72) were less likely to report more long-term information needs compared with breast cancer survivors. Participants diagnosed with regional and distant cancer stage were 67 % (95 % CI 1.30, 2.14) and 81 % (95 % CI 1.28, 2.55) more likely, respectively, to identify ≥2 long-term information needs compared with those diagnosed with in situ or local disease. Participants that self-reported worse health also had greater informational needs long term. Those with fair/poor self-reported health were more than twice as likely to report greater need compared with those reporting excellent health (OR 2.37, 95 % CI 1.66, 3.36).
Discussion
The results of this study suggest that long-term cancer survivors in the USA who were diagnosed prior to the development of and thus never received SCPs have substantial unmet health information needs that could be addressed through topics covered in SCPs. Greatest interest was for information on cancer screening tests, followed by long-term treatment side effects, recommended healthy behaviors, tests and examinations post-cancer treatment, and possible consequences of having had cancer on health insurance or finances, respectively. A number of socio-demographic and clinical characteristics were associated with level of informational need 9-years post-diagnosis, including age, race/ethnicity, education level, cancer type and stage, number of comorbid conditions, and self-reported health. The two most preferred sources for obtaining cancer information were print media and personalized reading materials, such as a SCP, whereas email/internet was ranked fourth after meeting in person with a health care professional to receive cancer information.
Comparing long-term versus short-term need for information contained in SCPs
SCPs are intended for dissemination upon completion of active treatment or early in the cancer trajectory; however, our study suggests that long-term cancer survivors who did not receive SCPs after diagnosis may also benefit from this information. The information needs of cancer survivors at various stages in their cancer trajectory have been investigated in a number of studies. Information-seeking behavior of cancer survivors at all stages of the cancer trajectory were assessed in a population-based telephone survey of 411 participants, post-cancer diagnosis. Prevalence of health/cancer information-seeking was highest for those ≥11 years post-diagnosis compared with earlier in the trajectory [34]. Conversely, colon, breast, and prostate cancer survivors participating in a longitudinal cohort (n = 2013) reported highest levels of need at 1 year post-diagnosis, with decreasing need over the subsequent 2 years, although level of need differed by cancer type and information topic [35]. Another cross-sectional survey among 187 cancer survivors found that trend scores for information need decreased with time since diagnosis [36]. In an analysis of cross-sectional data from the Study of Cancer Survivors-II, overall information need was less for those with a longer time since diagnosis for women (11 vs 3 years) but need did not differ for men based on time since diagnosis [37].
The 9-year cancer survivors in this study who were diagnosed prior to routine use of SCPs identified current unmet need for the information that is provided in a SCP. Overall, our results were comparable to the few studies that have assessed health information needs ≥9 years post-cancer diagnosis that indicated a need for information regarding late cancer/treatment effects, health promotion, ongoing tests and treatments, interpersonal/emotional support, financial issues, and screening/surveillance [11, 18, 34, 37–39]. Those at least 5 years post-diagnosis have indicated similar needs [24, 27, 40], although recently treated cancer patients have also indicated a desire for information on lifestyle and long-term treatment and disease effects in some studies [41]. Our findings are consistent with those reported in another large long-term (up to 14 years post-diagnosis) study of 1197 cancer survivors in California where participants reported a high prevalence of unmet health information need, particularly those that had not previously received a written treatment summary [11]. The ACS Study of Cancer Survivors II (n = 1514; 25 % were 10-year survivors) identified 16 themes of unmet needs based on open-ended responses. The top ranked themes encompassed needs identified in our analysis, including physical problems (symptoms, diet, and exercise) and education/information needs (follow-up care, self-care, cancer/health research, cancer risks, causes, and prevention) [38].
A previous systematic review of the literature on health informational needs and sources of cancer survivors up through 2003 found that the majority of studies assessed needs during or shortly post-treatment; thus, highly ranked needs included treatment-related, prognosis, and rehabilitation information [9]. In this group of studies, only 3.4 % of participants indicated a need for cancer surveillance or health information, which contrasts our findings for longer term cancer survivors. A more recent systematic review up through February 2012 assessed informational need and priorities among primarily newly diagnosed cancer patients or survivors <5 years post-treatment. The 30 studies in this review similarly highlighted that patients prioritized information on prognosis, diagnosis, and treatment information [42].
Some long-term information domains that were assessed may reflect unmet medical needs as opposed to informational needs per se, for example, stress management encompassed within the psychological burden domain, which is difficult to address in a general clinical setting and may require referral for psychological services [39]. However, disentangling how access to medical care influences informational need was beyond the scope of the data collected in our population.
With widespread encouragement of adoption of SCPs in 2015 as recommended by the Institute of Medicine (IOM) [2, 7, 43], the Cancer Survivorship Committee within the American Society of Clinical Oncology (ASCO) [7], and the Commission on Cancer [6], the informational needs of newly diagnosed patients are more likely to be met. The SCP was designed to be an evolving document [30]. Our data suggests a need to provide SCPs for all cancer survivors, which would give individuals who did not previously receive a SCP access to a document that may be able to address some of their unmet informational needs.
Current specific health information needs
Screening information was identified as the top unmet health information need of long-term cancer survivors in the SCS-I cohort. While long-term cancer survivors are more likely to receive ongoing surveillance of their primary cancer type, a recent prospective study found that people diagnosed with cancer were less likely to receive ongoing screening for other types of cancer compared with those without a cancer diagnosis, despite higher risk for second primary cancers [44]. Other data support the lack of enhanced screening for certain cancer types in this higher risk population compared with the general population [45]. A population-based, retrospective study of 21,111 cancer survivors found that two thirds of breast cancer survivors had never been screened for colorectal cancer, while half of female colorectal cancer survivors had never been screened for breast or cervical cancer [46]. Greater dissemination of long-term screening and surveillance recommendations or national screening guidelines specific to long-term cancer survivors may be warranted to enhance uptake of screening services for early detection of recurrent and second cancers.
We also found that long-term cancer survivors want more information on long-term side effects of cancer treatment. A third of all cancer survivors report ongoing side effects after treatment completion [47]. That proportion is higher for some leading cancers, for example, up to two thirds of breast cancer survivors report ongoing treatment-related effects such as osteopenia and osteoporosis, twice the proportion of the general population [48].
Information on recommended healthy behaviors ranked highly as an unmet area of need. Cancer survivors’ dissatisfaction with available health promotion resources has been reported elsewhere [49, 50]. A national survey found close to a third of cancer survivors were obese and had conducted no leisure time physical activity during the previous 30 days [51]. The increasing evidence that energy balance and related comorbidities play a role in cancer recurrence and survival merits greater emphasis on healthy lifestyle behaviors through SCP content [51–54].
Participants also expressed a need for information on tests and examinations they should have following cancer treatment. Previous surveys have highlighted a desire by cancer survivors for clinical support with respect to prevention and early detection of cancer recurrence [55] and tests for cancer and treatment-related comorbidity. In a British study of 26,213 long-term cancer survivors matched 1:4 to non-cancer controls, breast cancer survivors had a higher risk of heart failure, coronary artery disease, hypothyroidism, and osteoporosis compared with controls [56]. Colorectal cancer survivors were at increased risk for dementia, diabetes, and osteoporosis, while prostate cancer survivors had higher risk of osteoporosis compared with controls [56]. Receipt of follow-up care instructions was associated with better medical follow-up attendance, cancer surveillance, and preventive cancer screening, as well as fewer late/long-term side effects in a 2010 survey of 3541 cancer survivors post-treatment [57].
Many of the information needs reported by participants could be provided by a PCP, including information on cancer screening and healthy behaviors. Long-term survivors in remission are more likely to receive care from a PCP [58], unlike those with recurrence and receiving treatment. The level of resources for cancer survivors in primary care is unclear, although the ACS and ASCO continue to develop consensus guidelines [59–61]. We found that half of long-term cancer survivors recently utilized both primary and specialist care and most had recent access to a PCP. However, utilizing primary versus specialist care was not associated with level of informational need in our analysis. Data on visits to care providers was based on self-report, as was information on whether participants were currently cancer free, which could have influenced our findings. Additionally, reasons for visiting an oncologist as opposed to a PCP may vary widely.
Preferred delivery format for health information
With widespread adoption of SCPs, the dissemination method may begin to encompass modalities beyond an in-person meeting between patients and their health care providers. Our findings suggest that overall, the highest proportion of cancer survivors rated reading a book, magazine, or other printed material as a preferred source for cancer information, followed by personalized reading materials, although participants identified multiple preferences that may differ depending on circumstance. The Cancer Information Service Research Consortium recently presented data from three randomized controlled trials of web-based multi-media programs to support cancer treatment and post-treatment decisions. While 50–67 % of participants reported using multimedia, up to 90 % reported using print materials [62]. In the Michigan Prostate Cancer Survivor Study, the top five sources of information were health care provider, someone with prostate cancer, brochures/pamphlets, National Cancer Institute/American Cancer Society, and the internet. Half of prostate cancer survivors visited their primary care provider first for information; 18 % searched on the internet [63]. Another cross-sectional survey of 411 patients (from those undergoing treatment to ≥5 years post-treatment) attending cancer clinic post-treatment follow-up found that the most preferred source of health information was the internet, followed by health provider [64]; the opposite was true for 865 cancer survivors up to ≥11 years post-diagnosis that completed a population-based telephone survey [34]. However, those at least 1 year post-treatment have reported seeking cancer-related information from an average of five sources, suggesting that offering a variety of sources may be preferable [65]. Although many organizations are moving towards digital-only content, our data supports the print format currently adopted for SCP dissemination, particularly for this older population of longer term cancer survivors. The fact that print material was ranked more highly than in-person information exchange warrants further investigation, as well as preferred information sources specific to each identified health information need.
The internet was the fourth preferred information source in the current analysis. Confusion with regards to the information available via the internet [34, 66, 67] and skepticism of unknown internet sources could be a barrier to this mode of delivery [68]. The HINTS survey highlighted that cancer survivors used the internet at a lower rate than the general population [69]. Frameworks that use patient-level data to personalize electronic communication between practitioners and cancer patients are currently under development [70] and may offer new avenues for delivering SCP-related information in the future, yet more work is needed to understand if these technology-driven formats will be acceptable.
Demographic and clinical factors associated with health information need
We observed differences in number of informational needs by socio-demographic characteristics (age, race/ethnicity, education), cancer characteristics (type, stage), and health status (number of comorbid conditions, self-reported health), underscoring the need to individualize the information provided in SCPs. Information needs of cancer survivors earlier in the cancer trajectory have been shown to differ significantly by demographic, psychosocial, clinical, and cancer characteristics in a number of studies [11, 50, 71–73]. We found that younger people were more likely to indicate informational needs 9 years post-diagnosis. Earlier in the cancer trajectory, younger age has previously been shown to predict greater informational needs [40]. However, level of need may also differ by informational topic, such as sexuality or social life, for younger compared with older cancer survivors [42]. In a large cluster analysis of cancer patients 2 years post-diagnosis, high information seekers were highly educated, whereas constrained information seekers were of lower socio-economic status [74]. Our analysis similarly highlighted that highly educated long-term cancer survivors were more likely to report greater information needs compared with those less educated. Other studies have reported discordant findings, where low educational attainment, but not health literacy, was associated with greater cancer informational need [75]. We also found that minority participants reported greater informational need, but we did not identify differences by income status. Minority ethnic groups that do search for health information are more likely to specifically seek support service information and psychosocial support compared with non-Hispanic whites [37, 71]. A recent cross-sectional survey of breast and prostate cancer survivors (>2 years post-treatment) showed that African Americans reported greater informational needs compared with other races [76]. The National Cancer Institute’s 2003 HINTS Survey similarly found that cancer information seekers were younger, female, had higher income, and a regular health care provider [73]. Among men in the Michigan Prostate Cancer Survivor Study, whether informational needs were addressed also differed by age and race; older men and white survivors were more likely to report receiving adequate information from a health care provider [63]. Needs may also differ by level of health insurance [77], although we could not evaluate this association since the majority of the study population had health insurance coverage [40].
Longer term informational needs differed by cancer type as addressed in previous studies [78, 79]. Compared with breast cancer survivors, prostate, colorectal, uterine, melanoma, kidney, and lung cancer survivors identified fewer informational needs. A cross-sectional analysis of informational needs of 2010 cancer survivors in Pennsylvania also found that information-seeking behavior differed by cancer type, although differences were reduced at later cancer stages [79]. We observed that those diagnosed at the regional cancer stage and those with worse self-reported health were more likely to have a higher number of health informational needs 9 years post-diagnosis; few previous studies have examined differences in health information needs of cancer survivors by cancer stage.
Strengths and limitations
Strengths of this study include the large number of long-term cancer survivors and population-based sampling. Our current cohort was largely composed of breast, prostate, and colorectal cancer survivors, which is representative of the broader population of cancer survivors in the USA [80]. However, a few limitations should be noted. Although demographic and clinical data were collected longitudinally, questions about specific informational needs and preferred sources of information were developed after the baseline questionnaire, and therefore, analysis was cross-sectional. A further consideration is the fact that one fifth of participants had a cancer recurrence or required further cancer treatment during the follow-up period. This population may have different information needs to the broader population of long-term cancer survivors, and it is unclear whether they received a SCP following completion of treatment for their recurrence or second cancer. Although minorities were oversampled in the original design, the sample was still predominantly non-Hispanic white, with similar representation of minorities in the third survey compared with the first (baseline) survey. Therefore, our results may not generalize to cancer survivors of other race/ethnicity. While we explored the number of informational needs by demographic and cancer characteristics separately, we did not assess how different combinations of these characteristics influenced number of information needs, for example, for individuals of certain race/ethnicity and education level. The drivers of differences in level of need for these subgroups are an interesting potential area of future research. Future large, observational, longitudinal studies that assess the changing needs of cancer survivors across the cancer survivorship continuum are warranted.
Conclusion
Long-term cancer survivors in our population had unmet informational needs, particularly with regards to screening, long-term cancer and treatment effects, and healthy lifestyle behaviors. Number of informational needs differed by socio-demographic, clinical, and cancer characteristics. Long-term cancer survivors preferred a print format for health information dissemination. Our findings indicate that cancer survivors who did not previously receive a SCP reported a desire for its contents 9 years post-diagnosis, supporting delivery of SCP content to this population. As the unmet needs evaluated in our study reflect the current content of survivorship care plans, our findings support the plan for their wider implementation and suggest that dissemination should also be expanded to long-term cancer survivors.
References
DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, et al. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64(4):252–71. doi:10.3322/caac.21235.
Hewitt M GS, Stovall E. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: The National Academies Press; 2006.
Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62(4):220–41. doi:10.3322/caac.21149.
de Moor JS, Mariotto AB, Parry C, Alfano CM, Padgett L, Kent EE, et al. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22(4):561–70. doi:10.1158/1055-9965.EPI-12-1356.
Rowland JH, Bellizzi KM. Cancer survivorship issues: life after treatment and implications for an aging population. J Clin Oncol. 2014;32(24):2662–8. doi:10.1200/JCO.2014.55.8361.
Commission on Cancer. Cancer Program Standards 2012: Ensuring Patient-Centered Care. Chicago: American College of Surgeons; 2012.
McCabe MS, Bhatia S, Oeffinger KC, Reaman GH, Tyne C, Wollins DS, et al. American Society of Clinical Oncology statement: achieving high-quality cancer survivorship care. J Clin Oncol. 2013;31(5):631–40. doi:10.1200/JCO.2012.46.6854.
Salz T, Oeffinger KC, McCabe MS, Layne TM, Bach PB. Survivorship care plans in research and practice. CA Cancer J Clin. 2012. doi:10.3322/caac.20142.
Rutten LJ, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: a systematic review of research (1980–2003). Patient Educ Couns. 2005;57(3):250–61. doi:10.1016/j.pec.2004.06.006.
Arora NK, Johnson P, Gustafson DH, McTavish F, Hawkins RP, Pingree S. Barriers to information access, perceived health competence, and psychosocial health outcomes: test of a mediation model in a breast cancer sample. Patient Educ Couns. 2002;47(1):37–46.
Kent EE, Arora NK, Rowland JH, Bellizzi KM, Forsythe LP, Hamilton AS, et al. Health information needs and health-related quality of life in a diverse population of long-term cancer survivors. Patient Educ Couns. 2012. doi:10.1016/j.pec.2012.08.014.
Husson O, Mols F, van de Poll-Franse LV. The relation between information provision and health-related quality of life, anxiety and depression among cancer survivors: a systematic review. Ann Oncol. 2011;22(4):761–72. doi:10.1093/annonc/mdq413.
Booth K, Beaver K, Kitchener H, O’Neill J, Farrell C. Women’s experiences of information, psychological distress and worry after treatment for gynaecological cancer. Patient Educ Couns. 2005;56(2):225–32. doi:10.1016/j.pec.2004.02.016.
Gansler T, Kepner J, Willacy E, Soloe C, Rupert D, Jarblum M, et al. Evolving information priorities of hematologic cancer survivors, caregivers, and other relatives. J Cancer Educ. 2010;25(3):302–11. doi:10.1007/s13187-009-0034-9.
Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ. What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer. 2009;17(8):1117–28. doi:10.1007/s00520-009-0615-5.
McDowell ME, Occhipinti S, Ferguson M, Dunn J, Chambers SK. Predictors of change in unmet supportive care needs in cancer. Psycho-Oncology. 2010;19(5):508–16. doi:10.1002/Pon.1604.
Baravelli C, Krishnasamy M, Pezaro C, Schofield P, Lotfi-Jam K, Rogers M, et al. The views of bowel cancer survivors and health care professionals regarding survivorship care plans and post treatment follow up. J Cancer Surviv. 2009;3(2):99–108. doi:10.1007/s11764-009-0086-1.
Brennan ME, Butow P, Marven M, Spillane AJ, Boyle FM. Survivorship care after breast cancer treatment—experiences and preferences of Australian women. Breast. 2011;20(3):271–7. doi:10.1016/j.breast.2010.12.006.
Burg MA, Lopez ED, Dailey A, Keller ME, Prendergast B. The potential of survivorship care plans in primary care follow-up of minority breast cancer patients. J Gen Intern Med. 2009;24 Suppl 2:S467–71. doi:10.1007/s11606-009-1012-y.
Hewitt ME, Bamundo A, Day R, Harvey C. Perspectives on post-treatment cancer care: qualitative research with survivors, nurses, and physicians. J Clin Oncol. 2007;25(16):2270–3. doi:10.1200/JCO.2006.10.0826.
Marbach TJ, Griffie J. Patient preferences concerning treatment plans, survivorship care plans, education, and support services. Oncol Nurs Forum. 2011;38(3):335–42. doi:10.1188/11.ONF.335-342.
Royak-Schaler R, Passmore SR, Gadalla S, Hoy MK, Zhan M, Tkaczuk K, et al. Exploring patient-physician communication in breast cancer care for African American women following primary treatment. Oncol Nurs Forum. 2008;35(5):836–43. doi:10.1188/08.ONF.836-843.
Hodgkinson K, Butow P, Hobbs KM, Wain G. After cancer: the unmet supportive care needs of survivors and their partners. J Psychosoc Oncol. 2007;25(4):89–104. doi:10.1300/J077v25n04_06.
Cappiello M, Cunningham RS, Knobf MT, Erdos D. Breast cancer survivors: information and support after treatment. Clin Nurs Res. 2007;16(4):278–93. doi:10.1177/1054773807306553. discussion 94–301.
Cohn WF, Ropka ME, Jones SM, Miesfeldt S. Information needs about hereditary breast cancer among women with early-onset breast cancer. Cancer Detect Prev. 2003;27(5):345–52.
Mosavel M, Sanders K. Needs of low-income african american cancer survivors: multifaceted and practical. J Cancer Educ. 2011;26(4):717–23. doi:10.1007/s13187-011-0253-8.
Khan NF, Evans J, Rose PW. A qualitative study of unmet needs and interactions with primary care among cancer survivors. Br J Cancer. 2011;105 Suppl 1:S46–51. doi:10.1038/bjc.2011.422.
Tanna N, Buijs H, Pitkin J. Exploring the breast cancer patient journey: do breast cancer survivors need menopause management support? Menopause Int. 2011;17(4):126–31. doi:10.1258/mi.2011.011101.
Parry C, Kent EE, Forsythe LP, Alfano CM, Rowland JH. Can’t see the forest for the care plan: a call to revisit the context of care planning. J Clin Oncol. 2013;31(21):2651–3. doi:10.1200/JCO.2012.48.4618.
Mayer DK, Nekhlyudov L, Snyder CF, Merrill JK, Wollins DS, Shulman LN. American Society of Clinical Oncology clinical expert statement on cancer survivorship care planning. J Oncol Pract. 2014;10(6):345–51. doi:10.1200/JOP.2014.001321.
Smith T, Stein KD, Mehta CC, Kaw C, Kepner JL, Buskirk T, et al. The rationale, design, and implementation of the American Cancer Society’s studies of cancer survivors. Cancer. 2007;109(1):1–12. doi:10.1002/cncr.22387.
Ferrucci LM, McCorkle R, Smith T, Stein KD, Cartmel B. Factors related to the use of dietary supplements by cancer survivors. J Altern Complement Med. 2009;15(6):673–80. doi:10.1089/acm.2008.0387.
Nelson DE, Kreps GL, Hesse BW, Croyle RT, Willis G, Arora NK, et al. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun. 2004;9(5):443–60. doi:10.1080/10810730490504233. discussion 81–4.
Hesse BW, Arora NK, Burke Beckjord E, Finney Rutten LJ. Information support for cancer survivors. Cancer. 2008;112(11 Suppl):2529–40. doi:10.1002/cncr.23445.
Tan AS, Nagler RH, Hornik RC, DeMichele A. Evolving information needs among colon, breast, and prostate cancer survivors: results from a longitudinal mixed-effects analysis. Cancer Epidemiol Biomarkers Prev. 2015;24(7):1071–8. doi:10.1158/1055-9965.EPI-15-0041.
Mistry A, Wilson S, Priestman T, Damery S, Haque M. How do the information needs of cancer patients differ at different stages of the cancer journey? A cross-sectional survey. JRSM short reports. 2010;1(4):30. doi:10.1258/shorts.2010.010032.
McInnes DK, Cleary PD, Stein KD, Ding L, Mehta CC, Ayanian JZ. Perceptions of cancer-related information among cancer survivors: a report from the American Cancer Society’s Studies of Cancer Survivors. Cancer. 2008;113(6):1471–9. doi:10.1002/cncr.23713.
Burg MA, Adorno G, Lopez ED, Loerzel V, Stein K, Wallace C, et al. Current unmet needs of cancer survivors: analysis of open-ended responses to the American Cancer Society Study of Cancer Survivors II. Cancer. 2015;121(4):623–30. doi:10.1002/cncr.28951.
Geller BM, Vacek PM, Flynn BS, Lord K, Cranmer D. What are cancer survivors’ needs and how well are they being met? J Fam Pract. 2014;63(10):E7–E16.
Beckjord EB, Arora NK, McLaughlin W, Oakley-Girvan I, Hamilton AS, Hesse BW. Health-related information needs in a large and diverse sample of adult cancer survivors: implications for cancer care. J Cancer Surviv. 2008;2(3):179–89. doi:10.1007/s11764-008-0055-0.
Hawkins NA, Pollack LA, Leadbetter S, Steele WR, Carroll J, Dolan JG, et al. Informational needs of patients and perceived adequacy of information available before and after treatment of cancer. J Psychosoc Oncol. 2008;26(2):1–16.
Tariman JD, Doorenbos A, Schepp KG, Singhal S, Berry DL. Information needs priorities in patients diagnosed with cancer: a systematic review. J Adv Pract Oncol. 2014;2014(5):115–22.
Adler NE PA. Cancer care for the whole patient: meeting psycosocial health needs. Washington, DC: The National Academies Press; 2008.
Schumacher JR, Witt WP, Palta M, Loconte NK, Heidrich SM, Trentham-Dietz A, et al. Cancer screening of long-term cancer survivors. J Am Board Fam Med. 2012;25(4):460–9. doi:10.3122/jabfm.2012.04.110118.
Mayer DK, Terrin NC, Menon U, Kreps GL, McCance K, Parsons SK, et al. Screening practices in cancer survivors. J Cancer Surviv. 2007;1(1):17–26. doi:10.1007/s11764-007-0007-0.
Grunfeld E, Moineddin R, Gunraj N, Del Giudice ME, Hodgson DC, Kwon JS, et al. Cancer screening practices of cancer survivors: population-based, longitudinal study. Canadian family physician Medecin de famille canadien. 2012;58(9):980–6.
Wu HS, Harden JK. Symptom burden and quality of life in survivorship: a review of the literature. Cancer Nurs. 2015;38(1):E29–54. doi:10.1097/NCC.0000000000000135.
Hill DA, Horick NK, Isaacs C, Domchek SM, Tomlinson GE, Lowery JT, et al. Long-term risk of medical conditions associated with breast cancer treatment. Breast Cancer Res Treat. 2014;145(1):233–43. doi:10.1007/s10549-014-2928-4.
Arora NK, Reeve BB, Hays RD, Clauser SB, Oakley-Girvan I. Assessment of quality of cancer-related follow-up care from the cancer survivor’s perspective. J Clin Oncol. 2011;29(10):1280–9. doi:10.1200/JCO.2010.32.1554.
Zebrack B. Information and service needs for young adult cancer survivors. Support Care Cancer. 2009;17(4):349–57. doi:10.1007/s00520-008-0469-2.
Underwood JM, Townsend JS, Stewart SL, Buchannan N, Ekwueme DU, Hawkins NA, et al. Surveillance of demographic characteristics and health behaviors among adult cancer survivors--Behavioral Risk Factor Surveillance System, United States, 2009. Morbidity and mortality weekly report Surveillance summaries. 2012;61(1):1–23.
Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV, et al. American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2012;62(1):30–67. doi:10.3322/caac.20140.
Mayer DK, Terrin NC, Menon U, Kreps GL, McCance K, Parsons SK, et al. Health behaviors in cancer survivors. Oncol Nurs Forum. 2007;34(3):643–51. doi:10.1188/07.ONF.643-651.
Mason C, Alfano CM, Smith AW, Wang CY, Neuhouser ML, Duggan C, et al. Long-term physical activity trends in breast cancer survivors. Cancer Epidemiol Biomarkers Prev. 2013;22(6):1153–61. doi:10.1158/1055-9965.EPI-13-0141.
Harrison SE, Watson EK, Ward AM, Khan NF, Turner D, Adams E, et al. Primary health and supportive care needs of long-term cancer survivors: a questionnaire survey. J Clin Oncol. 2011;29(15):2091–8. doi:10.1200/JCO.2010.32.5167.
Khan NF, Mant D, Carpenter L, Forman D, Rose PW. Long-term health outcomes in a British cohort of breast, colorectal and prostate cancer survivors: a database study. Br J Cancer. 2011;105 Suppl 1:S29–37. doi:10.1038/bjc.2011.420.
Jabson JM. Follow-up care instructions, treatment summaries, and cancer survivors’ receipt of follow-up health care and late/long term effects. Support Care Cancer. 2014. doi:10.1007/s00520-014-2532-5.
Pollack LA, Adamache W, Ryerson AB, Eheman CR, Richardson LC. Care of long-term cancer survivors: physicians seen by Medicare enrollees surviving longer than 5 years. Cancer. 2009;115(22):5284–95. doi:10.1002/cncr.24624.
El-Shami K, Oeffinger KC, Erb NL, Willis A, Bretsch JK, Pratt-Chapman ML, et al. American Cancer Society Colorectal Cancer Survivorship Care Guidelines. CA Cancer J Clin. 2015;65(6):427–55. doi:10.3322/caac.21286.
Resnick MJ, Lacchetti C, Penson DF. Prostate cancer survivorship care guidelines: American Society of Clinical Oncology practice guideline endorsement. J Oncol Pract. 2015;11(3):e445–9. doi:10.1200/JOP.2015.004606.
Skolarus TA, Wolf AM, Erb NL, Brooks DD, Rivers BM, Underwood 3rd W, et al. American Cancer Society prostate cancer survivorship care guidelines. CA Cancer J Clin. 2014;64(4):225–49. doi:10.3322/caac.21234.
Marcus AC, Diefenbach MA, Stanton AL, Miller SM, Fleisher L, Raich PC, et al. Cancer patient and survivor research from the cancer information service research consortium: a preview of three large randomized trials and initial lessons learned. J Health Commun. 2013;18(5):543–62. doi:10.1080/10810730.2012.743629.
Darwish-Yassine M, Berenji M, Wing D, Copeland G, Demers RY, Garlinghouse C, et al. Evaluating long-term patient-centered outcomes following prostate cancer treatment: findings from the Michigan Prostate Cancer Survivor study. J Cancer Surviv. 2014;8(1):121–30. doi:10.1007/s11764-013-0312-8.
Shea-Budgell MA, Kostaras X, Myhill KP, Hagen NA. Information needs and sources of information for patients during cancer follow-up. Curr Oncol. 2014;21(4):165–73. doi:10.3747/co.21.1932.
Blanch-Hartigan D, Blake KD, Viswanath K. Cancer survivors’ use of numerous information sources for cancer-related information: does more matter? J Cancer Educ. 2014;29(3):488–96. doi:10.1007/s13187-014-0642-x.
van de Poll-Franse LV, van Eenbergen MC. Internet use by cancer survivors: current use and future wishes. Support Care Cancer. 2008;16(10):1189–95. doi:10.1007/s00520-008-0419-z.
Arora NK, Hesse BW, Rimer BK, Viswanath K, Clayman ML, Croyle RT. Frustrated and confused: the American public rates its cancer-related information-seeking experiences. J Gen Intern Med. 2008;23(3):223–8. doi:10.1007/s11606-007-0406-y.
LaCoursiere SP, Knobf MT, McCorkle R. Cancer patients’ self-reported attitudes about the Internet. J Med Internet Res. 2005;7(3):e22. doi:10.2196/jmir.7.3.e22.
Chou WY, Liu B, Post S, Hesse B. Health-related Internet use among cancer survivors: data from the Health Information National Trends Survey, 2003–2008. J Cancer Surviv. 2011;5(3):263–70. doi:10.1007/s11764-011-0179-5.
Vickers AJ, Salz T, Basch E, Cooperberg MR, Carroll PR, Tighe F, et al. Electronic patient self-assessment and management (SAM): a novel framework for cancer survivorship. BMC Med Inform Decis Mak. 2010;10:34. doi:10.1186/1472-6947-10-34.
Squiers L, Finney Rutten LJ, Treiman K, Bright MA, Hesse B. Cancer patients’ information needs across the cancer care continuum: evidence from the cancer information service. J Health Commun. 2005;10 Suppl 1:15–34. doi:10.1080/10810730500263620.
Husson O, Thong MS, Mols F, Oerlemans S, Kaptein AA, van de Poll-Franse LV. Illness perceptions in cancer survivors: what is the role of information provision? Psychooncology. 2012. doi:10.1002/pon.3042.
Mayer DK, Terrin NC, Kreps GL, Menon U, McCance K, Parsons SK, et al. Cancer survivors information seeking behaviors: a comparison of survivors who do and do not seek information about cancer. Patient Educ Couns. 2007;65(3):342–50. doi:10.1016/j.pec.2006.08.015.
Protiere C, Moumjid N, Bouhnik AD, Le Corroller Soriano AG, Moatti JP. Heterogeneity of cancer patient information-seeking behaviors. Med Decis Making. 2012;32(2):362–75. doi:10.1177/0272989X11415114.
Matsuyama RK, Wilson-Genderson M, Kuhn L, Moghanaki D, Vachhani H, Paasche-Orlow M. Education level, not health literacy, associated with information needs for patients with cancer. Patient Educ Couns. 2011;85(3):e229–36. doi:10.1016/j.pec.2011.03.022.
O’Malley DM, Hudson SV, Ohman-Strickland PA, Bator A, Lee HS, Gundersen DA, et al. Follow-up care education and information: identifying cancer survivors in need of more guidance. J Cancer Educ. 2014. doi:10.1007/s13187-014-0775-y.
Knobf MT, Ferrucci LM, Cartmel B, Jones BA, Stevens D, Smith M, et al. Needs assessment of cancer survivors in Connecticut. J Cancer Surviv. 2012;6(1):1–10. doi:10.1007/s11764-011-0198-2.
Ness S, Kokal J, Fee-Schroeder K, Novotny P, Satele D, Barton D. Concerns across the survivorship trajectory: results from a survey of cancer survivors. Oncol Nurs Forum. 2013;40(1):35–42. doi:10.1188/13.ONF.35-42.
Nagler RH, Gray SW, Romantan A, Kelly BJ, DeMichele A, Armstrong K, et al. Differences in information seeking among breast, prostate, and colorectal cancer patients: results from a population-based survey. Patient Educ Couns. 2010;81(Suppl):S54–62. doi:10.1016/j.pec.2010.09.010.
Howlander N NA, Krapcho M, Garshell J, Neyman N, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatlovich Z, Cho H, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975–2010, National Cancer Institute. . National Cancer Institute, Bethesda. 2013. http://seer.cancer.gov/csr/1975_2010/. Accessed 11/22/2013.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by the National Cancer Institute at the National Institutes of Health (grant number CA105666). The American Cancer Society (ACS) Studies of Cancer Survivors (SCS) were funded as an intramural program of research conducted by the ACS Behavioral Research Center.
Conflicts of interest
None
The authors assume full responsibility for analyses and interpretation of these data.
Certain data used in this study were obtained from the Connecticut Tumor Registry located in the Connecticut Department of Public Health. The authors also assume full responsibility for analyses and interpretation of the data collected from the Connecticut Tumor Registry. We thank all the study participants; the physicians of the participants; Rajni Mehta, Director of the Rapid Case Ascertainment Shared Resource of the Yale Cancer Center; and the following Connecticut hospitals: Charlotte Hungerford Hospital, Bridgeport Hospital, Danbury Hospital, Hartford Hospital, Middlesex Hospital, New Britain General Hospital, Bradley Memorial Hospital, Yale/New Haven Hospital, St. Francis Hospital and Medical Center, St. Mary’s Hospital, Hospital of St. Raphael, St. Vincent’s Medical Center, Stamford Hospital, William W. Backus Hospital, Windham Hospital, Eastern Connecticut Health Network, Griffin Hospital, Bristol Hospital, Johnson Memorial Hospital, Day Kimball Hospital, Greenwich Hospital, Lawrence and Memorial Hospital, Milford Hospital, New Milford Hospital, Norwalk Hospital, Sharon Hospital, and Waterbury Hospital.
Rights and permissions
About this article
Cite this article
Playdon, M., Ferrucci, L.M., McCorkle, R. et al. Health information needs and preferences in relation to survivorship care plans of long-term cancer survivors in the American Cancer Society’s Study of Cancer Survivors-I. J Cancer Surviv 10, 674–685 (2016). https://doi.org/10.1007/s11764-015-0513-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-015-0513-4