Abstract
Purpose
Fear of cancer recurrence (FCR) is prevalent among survivors. However, a comprehensive and universally accepted theoretical framework of FCR to guide intervention is lacking. This paper reviews theoretical frameworks previously used to explain FCR and describes the formulation of a novel theoretical framework for FCR.
Methods
A systematic review of the literature was undertaken to identify conceptual frameworks or theories applied to FCR. MEDLINE, PubMED, CINAHL, AMED, PsycINFO and Web of Science were searched. Identified conceptual frameworks were reviewed for strength of evidence supporting their validity.
Results
Of 558 papers initially identified, 16 made reference to six different conceptual frameworks relating to FCR. The most comprehensive and evidence-based theoretical approach is the Common Sense Model (CSM). Other approaches have limited evidence supporting their application to FCR. Two theoretical approaches developed in the context of emotional disorders that appear to be highly relevant to FCR: the Self-Regulatory Executive Function (S-REF) model and Relational Frame Theory were combined with the CSM to produce a novel cognitive processing account of FCR.
Conclusions
Few conceptual frameworks have been used consistently to guide FCR research, and not all frameworks are empirically well supported, suggesting that further discussion regarding the conceptualisation of FCR is needed. The novel theoretical framework for FCR presented highlights the multidimensional nature of FCR and the importance of cognitive processing and metacognitions in the development and maintenance of FCR.
Implications for Cancer Survivors
The novel theoretical formulation of FCR outlined here provides a much-needed comprehensive framework to further investigate and address FCR in cancer survivors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Receiving a cancer diagnosis, making treatment decisions and coping with treatment and its side effects may be all-consuming, and it is often only after completing treatment that an individual has time to reflect on what has happened and consider the implications for their future. For many, this is the first time that uncomfortable thoughts and a sense of unease or worry about the possibility of cancer recurrence emerge. Many patients report that adjustment to the possibility of a recurrence is more problematic than adjustment to the initial diagnosis of cancer [1]. As contact with the medical team diminishes, many survivors find they feel insecure, isolated, afraid and abandoned, rather than feeling a sense of relief, moving forward and ‘getting back to normal’ [2, 3].
Transient fear of cancer recurrence (FCR) is an almost ubiquitous experience for cancer survivors [4–6]. However, for 40–70 % of survivors, these fears can become chronic and disabling [7, 8]. High FCR can negatively affect mood, relationships, work, goal-setting and overall quality of life [9, 10], as well as increase health care costs [8, 11]. Furthermore, FCR is persistent and does not appear to decrease with time, even when the objective risk of recurrence is low [12–14].
When faced with expressions of FCR, family and friends often offer reassurance, possibly discouraging the individual from expressing their concerns. Similarly, individuals may be reluctant to discuss FCR with health professionals, lest they seem ungrateful. Inability to discuss such concerns can lead to a sense of disconnection from others and impaired capacity for enjoyment [15]. Help managing FCR is one of the most prevalent unmet needs reported by cancer survivors [16, 17].
Despite a growing body of research and several systematic reviews exploring factors that influence FCR and its outcomes [14, 18, 19], little fundamental theoretical work has been undertaken regarding FCR since the seminal 1997 publication by Lee-Jones, Humphris, Dixon and Hatcher [20]. The need for specific theoretical foundations for FCR has been highlighted in a recent comprehensive review [19]. Therefore, this paper aims to further discussion around the conceptualisation of FCR by providing an overview of previous theoretical frameworks of FCR and presenting a novel cognitive processing theoretical formulation of FCR that leads to specific therapeutic strategies and goals.
Methods
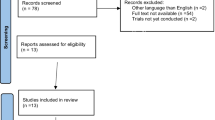
A systematic literature search was undertaken using the methodology of Simard et al. [19] (see search terms in Table 1) and expanded to include literature published in English up to October 2014. Once this search was completed, only papers containing the terms fear of cancer recurrence or fear of cancer progression (FoP) in the title or abstract were considered further. This strategy was chosen to limit papers to those with FCR or FoP as the primary and named outcome. It was reasoned that papers with FCR or FoP as a secondary outcome and therefore not the focus of the research were unlikely to use theory to explain FCR. To be included in this review, papers needed to explicitly mention a theoretical or conceptual framework employed in developing the study and interpreting the results. Primary sources or references for the theoretical approaches that were found in included papers were then obtained and further considered for inclusion and review.
Results
Of 558 papers initially identified by the search, 68 papers made reference to fear of cancer recurrence or fear of cancer progression in the title or abstract. Sixteen of these papers mentioned six different theoretical approaches to understanding FCR, which are listed in Table 2.
The existing theories and formulations that have been proposed and applied to FCR are all drawn from the cognitive behavioural paradigm and as such there is considerable commonality between theories. Most theories employed to understand FCR have incorporated (to varying degrees) an appraisal of health threat in the context of pre-existing beliefs or cognitive schemas, which can be triggered by either internal or external events, cues or stimuli and coping responses to the threat, both cognitive and emotional. These commonalities are summarised in Table 2. Early conceptualisations, for example Leventhal’s (1970) Parallel Process Model, have generally been expanded upon and incorporated into modern accounts of FCR. In particular, the Common Sense Model which incorporates aspects of Leventhal’s Parallel Process Model was expanded by Lee-Jones et al. [20]. These models, and their evidence base, are described below.
Theoretical perspectives as applied to FCR
1) Extended Parallel Process Model
The Extended Parallel Process Model (EPPM) [21] was developed to explain the results of fear appeals and expands on Leventhal’s Parallel Process Model by incorporating elements of Protection Motivation Theory and fear-as-drive models. According to the EPPM, whether a person experiences fear in response to a threat is determined by an initial appraisal of their susceptibility to the threat and the severity of the consequences associated with the threat (i.e. perceived threat). If this results in moderate to high perceived threat, then fear is elicited. Subsequent appraisal of the likely efficacy of potential response to the threat and perceived ability to carry out that response (i.e. perceived efficacy or coping) determines whether the response occurs. If the person perceives there is an effective response that they can undertake, fear is reduced. The applicability of EPPM has been evaluated in a single study, which examined how perceived threat, perceived efficacy and the interaction between the two were related to FCR in a sample of early-stage breast cancer patients who had completed treatment 6–24 months ago [22]. Findings indicated that threat appraisal was significantly related to FCR but coping appraisal was not, although the interaction between the two did explain a small amount of variance over and above threat appraisal. Thus, the results provide some support for the EPPM, although the contribution of coping appraisal seemed to be relatively weak.
2) Protection Motivation Theory
Protection Motivation Theory is similar to the EPPM in that information/stimuli initiate two appraisal processes: a threat appraisal and a coping appraisal, which are influenced by the severity of the threat and vulnerability to it as well as intrinsic/extrinsic rewards associated with responding to it and the perceived efficacy of a response and perceived efficacy to carry out that response, respectively [23]. According to this theory, the higher the perceived vulnerability to the threat (i.e. cancer recurrence), the higher you would expect FCR levels to be.
Several studies have found high subjective risk of recurrence is associated with higher FCR and worry about cancer more generally [12, 19, 24–28]. However, not all have found evidence in support of an association between risk perception and FCR. Liu et al. found that overestimation of perceived risk of recurrence 2 years after surgery was not significantly associated with FCR levels at the same time point in multivariable linear regression [29]. Thus, while other aspects of the PMT model have not been tested, taken together, these results suggests that the perceived vulnerability aspect of PMT (i.e. risk perceptions) may not fully account for level of FCR without consideration of other individual factors.
3) Theory of uncertainty in illness
Although uncertainty is not the same as specific fears about cancer recurrence, aspects of Mishel’s [30] theory of uncertainty in illness have been applied to understanding FCR [31, 32]. According to this theory, uncertainty is the inability to determine the meaning of illness-related events. It is generated when there is inconsistency, randomness, complexity, unpredictability and little information about the illness, its treatment and related events (e.g. symptoms). Integration of uncertainty into one’s life or life view, and directing it in a desired direction (e.g. reduced uncertainty), is seen as essential to adaption [30]. Illness uncertainty after cancer is associated with FCR [28, 33, 34], and uncertainty about the possibility of cancer recurrence is similarly triggered by events which are intrusive, unpredictable and random [32].
Additional evidence in support of this theoretical approach to FCR comes from a single-arm pilot study investigating a 6-week cognitive-existential group intervention targeting FCR, based on Mishel’s uncertainty in illness theory, the Common Sense Model (see below), cognitive models of worry and components of cognitive-existential group therapy [31]. Lebel et al. found that participating breast or ovarian cancer survivors experienced reductions in FCR up to 3 months after completion of the intervention. Importantly, the reduction in FCR was accompanied by a reduction in uncertainty. However, the relationship between change in FCR and uncertainty was not explicitly tested and so it is unclear whether the reduction in uncertainty contributed to the reported reduction in FCR.
What is not clear from this formulation is how uncertainty necessarily leads to fears about cancer recurrence or conversely whether FCR may in fact precede illness uncertainty as others have suggested [33]. That is, some degree of uncertainty about recurrence likely exists for all cancer survivors, yet not all cancer survivors develop clinically significant levels of FCR. A possible important explanatory factor may be individual variability in the degree of tolerance of uncertainty [c.f. 34]. Those who are tolerant of uncertainty associated with risk of cancer recurrence are unlikely to develop FCR, while those who are intolerant of such uncertainty are more likely to develop FCR. Thus, uncertainty may be an important contributor in determining the presence of FCR, but this is yet to be formally tested.
4) The Self-Regulation of Illness or Common Sense Model
The Common Sense Model (CSM) proposes that when individuals are confronted with a health threat, an illness representation is activated consisting of two motivational processing systems (cognitive and emotional) that act in parallel to inform a person’s response [35]. The activation of the cognitive system by a health threat leads to a coping response. The response is then appraised, leading to a feedback loop where people are likely to continue using coping strategies they find helpful. Problems can arise, however, if the health threat is coupled with heightened emotional arousal (as in the case of a cancer diagnosis) and the system to manage emotional distress overrides the cognitive system [36]. In this instance, coping strategies invoked have the primary aim of dealing with distress (e.g. reassurance seeking, checking the body for signs of disease). As with the cognitive system, these coping efforts are appraised as helpful as the distress is temporarily relieved, hence reinforcing these coping strategies. Unfortunately, in the long term, these strategies can act to maintain anxiety, as the actual triggers for distress are not addressed and the coping strategies are viewed as temporarily successful [36].
This model was originally proposed to explain adherence to medical regimens and further expanded by Lee-Jones et al. [20] in the most comprehensive theoretical formulation of FCR to date. Consistent with the CSM, the authors proposed that FCR comprises cognitions and emotions, where the cognitive system consists of perceived risk of recurrence and is influenced by factors such as past experiences with cancer and beliefs about the eradication of cancer [20]. On the other hand, the emotional processing system is associated with worry about the cancer returning, anxiety about cancer and regret about treatment decisions. Lee-Jones et al. [20] hypothesised that an individual’s illness representation is key in determining the level of FCR experienced, with those that view cancer as a chronic illness with uncontrollable negative consequences likely to have high FCR. Illness representations may change over time due to personal experiences, myths and media. Crucial to this formulation, behavioural responses to high FCR, such as anxious preoccupation with checking for signs and symptoms of cancer, may increase FCR through misinterpretation of neutral bodily symptoms.
There is good evidence that the CSM is relevant to FCR. This review found 10 papers that explicitly utilised the CSM to understand FCR. As reviewed above, research suggests that individuals who believe they are at greater personal risk of cancer recurring and are more emotionally aroused by somatic stimuli, display higher FCR [12, 20, 27, 28]. Illness perceptions have consistently been associated with higher FCR and worry about cancer more generally [19, 24–26]. For example, a study of early-stage breast cancer patients found women who viewed their cancer as a chronic or cyclical illness that was ‘hiding somewhere in their body’ were more anxious, depressed and had greater worry about their cancer coming back than those who felt their cancer was an acute short term illness [37]. Others have reported similar results: women who still viewed themselves as cancer patients had higher FCR levels [38]. However, not all research suggests a simple relationship between illness perceptions and FCR. Although illness perceptions were significantly associated with FCR levels in head and neck cancer patients, Llewellyn et al. [12] reported that optimism was the strongest predictor of FCR, independent of level of anxiety and fear prior to treatment. The authors suggested that dispositional optimism might moderate patient beliefs and levels of anxiety, but that their sample was too small to detect such a relationship. Others have found level of worry influences judgments of absolute risk of getting breast cancer in the general population rather than judgments of risk influencing level of worry [39]. Lipkus et al. [39] suggested level of pre-existing worry exacerbated biases, particularly pessimistic ones, and leads to increased perceived risk of developing breast cancer. Also consistent with the model, those with high FCR are more likely to engage in maladaptive cognitive and behavioural coping responses, for example avoidance of cancer related information and/or excessive symptom checking behaviours [8].
Further tentative evidence for this model comes from the AFTER intervention (adjustment to fear, threat or expectation of recurrence), which was based on the CSM formulation of FCR [40, 41]. This intervention led to improvements in FCR and anxious preoccupation with cancer in head and neck cancer patients immediately post-intervention compared to usual care control participants. Unfortunately, as the control group did not receive any psychological care, it is not clear whether specific CSM-based components of the intervention or more general therapeutic factors lead to the reductions in FCR in the intervention group. In particular, it is unclear whether changes in illness representations due to the intervention lead to reductions in FCR, as this was not measured. As mentioned above, Lebel et al’s [31] intervention for FCR was based on several theoretical models including the CSM. However, as with uncertainty, illness representations and other aspects of the CSM were not explicitly tested in this pilot study. As such reductions in FCR experienced by study participants cannot be clearly attributed to possible causal mechanisms as stipulated by the CSM.
5) Self-Regulatory Executive Function model of anxiety disorders
The Self-Regulatory Executive Function (S-REF) model [42] may be useful to understanding FCR as it (a) addresses factors that contribute to the development and maintenance of anxiety disorders, (b) is an effective approach for treating health anxiety [43] and (c) suggests specific cognitive factors as targets for effective treatment. The model proposes that a cognitive attentional syndrome (CAS), consisting of self-focused attention; worry and rumination; attentional bias to threat-related information; and maladaptive coping behaviours (e.g. suppression, avoidance, minimisation), contributes to anxiety. The S-REF model argues that beliefs about one’s thoughts (i.e. metacognitive beliefs) underlie the activation of CAS. That is, those who believe worry is important and may impact the outcome (e.g. ‘if I worry I will be prepared’ or ‘bad thoughts can make bad things happen’) are more likely to engage in CAS, which in turn intensifies fears and worries and prevents more adaptive emotional processing.
Fear of cancer recurrence consists of worry about symptoms, recurrence and the implications of cancer recurrence, together with excessive and inflexible monitoring for threatening signs and symptoms, consistent with the CAS. The S-REF model appears particularly applicable to FCR for a number of reasons. Firstly, it is trans-diagnostic, and like constructs such as worry, FCR is not a specific diagnosis but rather appears to be a normal concern after a diagnosis of cancer and treatment that exists on a continuum. Secondly, after treatment for cancer, there is uncertainty and a real chance of the feared outcome eventuating, such that the content of the beliefs is not entirely irrational, and hence, a focus on cognitive processes rather than disputing their content could be advantageous and more acceptable to patients compared with many more traditional cognitive behaviour therapy approaches which test the rationality of beliefs [44]. Thirdly, it explains why elevated emotional responses after cancer diagnosis (initially a normal response) are maintained for subset of individuals.
There are some studies supporting the validity of the S-REF model in the context of FCR. Anxious cancer patients display an attentional bias to threatening stimuli [45–47], and metacognitions and beliefs about cancer vulnerability are associated with FCR [12, 20, 27, 28]. Level of general health worry appears to be important in determining FCR [25], and maladaptive metacognitions have also been found to cause and maintain distress after a cancer diagnosis by both directly and indirectly driving worry [48, 49]. This has led some to speculate this tendency to worry may be embedded, consistent with pre-existing cognitive processing styles [25]. Maladaptive avoidance-based coping strategies are associated with FCR in the literature [12, 13, 50], and there is some indication targeting underlying worry and maladaptive coping strategies by teaching alternative adaptive coping strategies may be beneficial [31]. However, evidence around the importance of the use of these coping strategies in predicting FCR is currently weak with only one study reported to find a significant association [19, 51].
Accordingly, therapy based on the S-REF model, termed Metacognitive Therapy (MCT), may be useful in treating FCR. In particular, the attention training technique (ATT) and detached mindfulness (DM) aspects of MCT, may help manage uncontrollable FCR. ATT has been shown to alter habitual responses to intrusive thoughts, images and worries about health [43] and works through interrupting unhelpful information processing routines rather than challenging their declarative content (e.g. the specific thoughts about cancer coming back). On the other hand, DM allows awareness about these intrusive thoughts without requiring further actions such as avoidance, suppression or control of these thoughts [52]. There is evidence that mindfulness-based interventions help cancer patients in improving overall emotional outcomes. These studies found significant reductions in FCR (reported as a secondary outcome) immediately following a 6–8 session mindfulness-based stress reduction (MBSR) group, but no long-term data have been published [53–55]. While mindfulness has many meanings with limited consensus, it is important to note that the definition of DM as proposed in MCT is specific. In contrast to mindfulness-based strategies that use specific points of attention such as body-focused or breath-focused attention, DM has been described as a state of awareness of internal events, without responding to them with sustained evaluation, attempts to control or suppress them or responds to them behaviourally [52].
6) Relational Frame Theory and Acceptance and Commitment Therapy
Treatment completion marks a point at which many cancer survivors begin to engage in reflective thinking around the core aspects of their existence, and fears or concerns about cancer recurrence can emerge among other concerns surrounding death, isolation, freedom and meaningless [3]. Thus, while both the CSM and S-REF have particular features that make them useful frameworks for understanding FCR, neither explicitly addresses these well-documented existential issues that arise. Acceptance and Commitment Therapy [ACT; 56, 57], based on Relational Frame Theory (RFT), which focuses on the importance of accepting cognitive events, may be particularly relevant in this context. In brief, RFT posits that arbitrarily learned and contextually controlled relations between events or stimuli are at the core of language and cognition [56]. Psychopathology is thought to result from cases where excessive or improper use of these verbal and cognitive processes results in an inability to engage in behaviour directed towards valued outcomes. The result is experiential avoidance where the individual undertakes actions to deliberately avoid and/or escape from feelings, thoughts, memories and bodily sensations that are experienced as aversive [58]. In the context of FCR, RFT would suggest that some individuals, because of past traumatic experiences related to cancer or uncertainty, may be more vulnerable to FCR than others.
Like MCT, ACT seeks to change the function of these cognitive processes and an individual’s relationship with them rather than the content. The primary goal of ACT is to increase psychological flexibility to enable an individual to fully engage in the present moment and choose behaviour for any given situation that is consistent with their chosen values [58]. As such, ACT aims to help people develop more clarity about what is important to them (i.e. their values) and to establish goal-directed action. By choosing life directions that are meaningful, the individual is able to disengage from language and cognitions that result in psychopathology [56].
Psychosocial health professionals in oncology settings have identified ACT as offering clinically useful strategies for treating FCR [59], and ACT has been applied in the cancer context with promising results [60, 61]. For example, Feros et al. [60] found that nine sessions of ACT increased psychological flexibility and lead to improvements in QOL, distress and mood among a group of cancer patients with mixed diagnoses.
A novel theoretical approach to FCR
Synthesis of theories: a cognitive processing approach to FCR
Both MCT and ACT emphasise the problem of ‘cognitive fusion’, ‘getting caught up with’ thoughts or using rumination; directing excessive attention towards worry and unhelpful thoughts; and experiential avoidance or suppression of problematic thoughts. In addition, both MCT and ACT aim to equip the client with new skills to help them accept the presence of unpleasant thoughts and emotions while simultaneously giving them less importance or attention. Therefore, we present a novel theoretical framework (see Fig. 1), which is a distillation of CSM, S-REF and RFT.
The key features of the model are that:
-
1)
Certain life experiences such as past losses (particularly those involving cancer), past traumatic life events, caring roles and other sources of psychological stress can increase vulnerability to FCR.
-
2)
Beliefs about the chronic nature and severity of cancer and the existential impact of cancer can generate strong emotions, leading to high FCR.
-
3)
Certain beliefs, particularly those about the nature and importance of worry, can underlie a particular style of coping with worry that is problematic.
-
4)
This problematic style of dealing with worry includes rumination, attention towards threat-related information, self-focused attention and attempts to control, avoid or suppress thoughts about potential recurrence. These strategies all worsen FCR.
-
5)
Lack of information about how best to monitor health and stay healthy after a cancer diagnosis leads to uncertainty and confusion about appropriate checking behaviours.
-
6)
Furthermore, FCR can make it difficult to plan for the future, which can lead to poor self-concept, as the person can feel rudderless and with little to direct their energies towards. This can make it difficult to stay in touch with core life values and goals and to direct energy towards achieving those goals.
Like the formulation of Lee-Jones et al. [20], we conceptualise FCR as a multidimensional construct consisting of beliefs about the chronicity and severity of cancer with attendant strong emotions about recurrence. Our framework suggests these beliefs exist alongside beliefs about the importance and/or uncontrollability of worrying about cancer coming back, as well as self-focused sensitivity or hypervigilance to signs that cancer may have returned. Together with individual vulnerability factors, such as previous losses [62], concurrent stressors [6] and uncertainty due to lack of information [32], the presence or absence of these metacognitive beliefs (established through previous life experiences) are central to understanding why some individuals go on to develop clinically significant levels of FCR that are maintained and others do not. Furthermore, rather than reducing levels of FCR, coping strategies for dealing with high levels of worry centred around controlling, avoiding or suppressing thoughts about cancer recurrence lead to increased FCR and help maintain high levels of FCR.
From this formulation, we can see that an individual who has a background of previous losses, for example losing a parent to cancer, and has coped with their own cancer diagnosis and treatment by avoiding specific information about their condition may go on to develop FCR. Clinically significant FCR may develop and persist over time when the individual is unable to shift their focus from internal events that may indicate the return of cancer, such as fatigue or pain, due to beliefs about the importance of worrying about cancer in order to ‘be prepared’. These thoughts and fears about their cancer returning may become increasingly intrusive in the face of attempts to suppress or avoid thinking about the possibility of a cancer recurrence. In turn, these cognitive, metacognitive and emotional responses to the possibility of a cancer recurrence lead to greater impact on day-to-day life and it becomes increasingly difficult for the individual to engage in activities that they previously derived enjoyment and meaning from. This formulation is depicted in Fig. 1.
This framework allows the development of an explanatory model for people with high FCR, which links their previous life experience with their current fears, clarifies how core values and life goals can become lost when dealing with ongoing uncertainty and explains why some individual but not others may develop FCR despite objectively low objective risk of recurrence. The framework indicates that psycho-education about signs and symptoms of recurrence can reduce uncertainty and provides a behavioural template for appropriate levels of self-checking. The framework acknowledges that FCR is a rational and reasonable response to cancer, but identifies that avoidance of FCR is unhelpful, and challenges negative and positive beliefs about worry. By incorporating elements of S-REF and RFT, the framework specifies teaching skills in attentional flexibility and mindful awareness of thoughts without engagement, as possible therapeutic tools.
Discussion
The paper presents the results of a review of theoretical frameworks for understanding FCR. At present, no single formulation of FCR is widely accepted, though six approaches were identified in the review. The CSM is the most widely utilised theoretical formulation. However, not all predictions associated with the model have been tested and not all are supported. This is only the second paper to describe a specific and comprehensive theoretical framework for understanding FCR [c.f. 20]. The theoretical framework combines elements of S-REF [42], RFT [57] and the CSM [35] and is able to explain the development and maintenance of fear, anxiety and worry about the possibility of cancer returning. This framework improves on earlier explanations and investigations by broadening the clinical formulation of how FCR develops to include vulnerability factors and providing clear cognitive and behavioural targets for treatment. It may also be more acceptable to patients, as treatment does not challenge the content of FCR-related beliefs, but rather how the individual responds to them [44].
Research suggests that FCR is both multi-factorial and has multiple outcomes [18, 19]. A significant strength of the current theoretical framework is that it is also multi-factorial. For example, this model suggests that psychological stress (such as pre-existing anxiety, depression or distress due to previous losses), a lack of information about how to best monitor for recurrence, together with beliefs about risk perception and disease vulnerability, and the importance of worry, all contribute to the way a person is able to cope with the distress and anxiety experienced as a result of a cancer diagnosis and treatment (see Fig. 1). Crucially whether this distress and worry subsides with time or manifests as more severe levels of FCR that are maintained is thought to be a function of an individual’s beliefs about worry and how they regulate and respond to intrusive thoughts about recurrence. Negative and positive beliefs about worry can underlie a particular style of coping with uncertainty that is problematic and includes rumination, attention towards threat-related information, self-focused attention and attempts to control, avoid or suppress thoughts about potential recurrence, factors known to be associated with high levels of FCR [18–20].
This model has some commonalities with the theoretical accounts of FCR described above. For example, this model is consistent with Mishel’s [63] theory of uncertainty in illness, which suggests that a lack of information and education about an illness can lead to uncertainty and ambiguity in interpreting physical symptoms. In our formulation, together with other vulnerability factors, this uncertainty can lead to heightened FCR.
Almost all of the theoretical accounts reviewed above make reference to illness representations together with appraisal of coping capacity. High subjective risk of recurrence and illness perceptions have consistently been associated with higher FCR and worry about cancer more generally [19, 24–26]. However, as reviewed above, risk perception and illness representations alone do not appear to fully account for level of FCR. Consistent with this interpretation, the theoretical framework presented here places less emphasis on illness representations and risk perceptions as causal factors of FCR. Similar to the Lee-Jones et al. [20] framework of FCR, this model places an emphasis on cognitive processing. However, the model argues that metacognitions about worry are particularly important in explaining why some, but not all, cancer survivors develop clinical levels of FCR, and not the illness representation per se.
Importantly, the model leads to specific testable hypothesis about FCR. Firstly, those with unhelpful beliefs about the importance of worry, together with individual vulnerability factors and a lack of information, are more likely to develop clinically significant FCR. Secondly, those that continue to experience heightened FCR long after treatment are more likely to engage in unhelpful coping strategies focused on self-attention, rumination and controlling, avoiding and suppressing worry. Finally, those with high FCR are more likely to face existential challenges that lead to difficulties planning for the future and deriving meaning from their life.
Implications for clinical practice
Lee-Jones et al. [20] suggested treatment for FCR would need to be structured and contain both psychotherapeutic and educational components. The theoretical formulation proposed here provides a model for practicing psycho-oncology clinicians to formulate cases that present with clinically significant levels of FCR and indicates psychotherapeutic strategies that may be useful in this context. We have developed an intervention that builds on this framework and targets these factors that influence the development and maintenance of FCR [64]. It is not a goal of this intervention to eliminate FCR altogether, as some degree of vigilance for signs of recurrence is adaptive. Our goal is to equip survivors with the skills to cope with living amid uncertainty and fears about cancer recurrence and to allow them to move forward with their lives. That is, our intervention seeks to address FCR directly through the processes hypothesised to maintain high levels of FCR.
Future directions
There is currently a growing evidence base to support the proposed cognitive processing model. Several studies confirm the association between unhelpful metacognitions and FCR and distress [24, 48, 49, 65, 66]. Worry and rumination appear important when assessed explicitly [67]. Few studies to date have investigated the role of implicit processes such as attentional biases in establishing and maintaining FCR, and at present, the results of these studies are inconclusive. Methodological limitations related to the assessment of implicit processes affect this field of research [68], but there is growing interest and several more studies of this issue are currently underway [e.g. 69].
Further research is required to investigate the antecedents of FCR proposed in this model: the relationships between vulnerability factors, lack of information and FCR has not been explicitly investigated. There is evidence of an association between uncertainty and FCR [28, 33, 34], and lack of information about disease more generally is thought to contribute to uncertainty [32]. However, the association between lack of information about risk of recurrence and appropriate checking behaviours and ongoing high levels of FCR is yet to be tested.
We recently published a small pilot study that evaluated an intervention based on this novel theoretical formulation and reported positive results with highly significant reductions in FCR post therapy and at 2-month follow-up [70]. Overall, the results of this pilot support the validity and therapeutic utility of the theoretical framework proposed here. However, the pilot did not aim to test any specific predictions of this novel conceptualization and further research is needed. A large RCT of a treatment programme based on this approach is currently underway [64]. This trial will provide data to test further elements of the novel cognitive processing framework proposed here.
Conclusions
FCR is one of the most common difficulties reported by cancer survivors [19], and psycho-oncology clinicians report dealing with high FCR levels as challenging [59]. However, there are currently no universally accepted theoretical accounts of FCR to guide the development of targeted interventions and existing theoretical frameworks for understanding FCR fall short in explaining what factors are causal in the development and maintenance of clinically significant FCR. Here, we present a comprehensive novel theoretical approach to FCR, which has been synthesised from existing theories applied to FCR. The proposed theoretical framework leads to clear treatment pathways and goals; it incorporates aspects of the CSM, [20] together with S-REF [42] and RFT [57], and importantly provides a more holistic approach to FCR development and maintenance.
References
Cella DF, Mahon SM, Donovan MI. Cancer recurrence as a traumatic event. Behav Med. 1990;16:15–22.
Halldórsdóttir S, Hamrin E. Experiencing existential changes: the lived experience of having cancer. Cancer Nurs. 1996;19:29–36.
Lagerdahl ASK, Moynihan M, Stollery B. An exploration of the existential experiences of patients following curative treatment for cancer: reflections from a UK sample. J Psychosoc Oncol. 2014;32(5):555–75.
Simard S, Savard J. Fear of cancer recurrence inventory: development and initial validation of a multidimensional measure of fear of cancer recurrence. Support Care Cancer. 2009;17:241–51.
Kim Y, Carver CS, Spillers RL, et al. Dyadic effects of fear of recurrence on the quality of life of cancer survivors and their caregivers. Qual Life Res Int J Qual Life Asp Treat Care Rehab. 2012;21:517–25.
Mellon S, Kershaw TS, Northouse LL, Freeman-Gibb L. A family-based model to predict fear of recurrence for cancer survivors and their caregivers. Psycho-Oncology. 2007;16:214–23.
Simard S, Savard J. Screening and psychiatric comorbidity of clinical fear of cancer recurrence. 4th Canadian breast cancer research alliance reasons for hope scientific conference. Vancouver, Canada. 2008.
Thewes B, Butow P, Bell ML, et al. Fear of cancer recurrence in young women with a history of early-stage breast cancer: a cross-sectional study of prevalence and association with health behaviours. Support Care Cancer. 2012;20:2651–9.
Hodges L, Humphris G. Fear of recurrence and psychological distress in head and neck cancer patients and their carers. Psycho-Oncology. 2009;18:841–8.
Hart S, Latini D, Cowan J, et al. Fear of recurrence, treatment satisfaction, and quality of life after radical prostatectomy for prostate cancer. Support Care Cancer. 2008;16:161–9.
Lebel S, Tomei C, Feldstain A, et al. Does fear of cancer recurrence predict cancer survivors’ health care use? Support Care Cancer. 2013;21:901–6.
Llewellyn C, Weinman J, McGurk M, Humphris GM. Can we predict which head and neck cancer survivors develop fears of cancer recurrence? J Psychosom Res. 2008;65:525–32.
Skaali T, Fossa SD, Bremnes R, et al. Fear of recurrence in long-term testicular cancer survivors. Psycho-Oncology. 2009;18:1273–80.
Koch L, Jansen L, Brenner H, Arndt V. Fear of recurrence and disease progression in long-term (>5 years) cancer survivors—a systematic review of quantitative studies. Psycho-Oncology. 2013;22:1–11.
Hodgkinson K. What is the psychosocial impact of cancer? In: Hodgkinson K, Gilchrist J, editors. Psychosocial care of cancer patients: a health professionals guide to what to say and do. Melbourne: Ausmed Publications; 2008.
Armes J, Crowe M, Colbourne L, et al. Patients’ supportive care needs beyond the end of cancer treatment: a prospective, longitudinal survey. J Clin Oncol. 2009;27:6172–9.
van den Beuken-van Everdingen MHJ, Peters ML, de Rijke JM, et al. Concerns of former breast cancer patients about disease recurrence: a validation and prevalence study. Psycho-Oncology. 2008;17:1137–45.
Crist JV, Grunfeld EA. Factors reported to influence fear of recurrence in cancer patients: a systematic review. Psycho-Oncology. 2013;22:978–86.
Simard S, Thewes B, Humphris G, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Survivorship. 2013;7:300–22.
Lee-Jones C, Humphris G, Dixon R, Hatcher MB. Fear of cancer recurrence—a literature review and proposed cognitive formulation to explain exacerbation of recurrence fears. Psycho-Oncology. 1997;6:95–105.
Witte K. Putting the fear back into fear appeals: the extended parallel process model. Commun Monogr. 1992;59:329–49.
McGinty HL, Goldenberg JL, Jacobsen PB. Relationship of threat appraisal with coping appraisal to fear of cancer recurrence in breast cancer survivors. Psycho-Oncology. 2012;21:203–10.
Rippetoe PA, Rogers RW. Effects of components of protection-motivation theory on adaptive and maladaptive coping with a health threat. J Pers Soc Psychol. 1987;52:596–604.
Corter AL, Findlay M, Broom R, et al. Beliefs about medicine and illness are associated with fear of cancer recurrence in women taking adjuvant endocrine therapy for breast cancer. Br J Health Psychol. 2013;18:168–81.
Park CL, Cho D, Blank TO, Wortmann JH. Cognitive and emotional aspects of fear of recurrence: predictors and relations with adjustment in young to middle-aged cancer survivors. Psycho-Oncology. 2013;22:1630–8.
Phillips KM, McGinty HL, Gonzalez BD, et al. Factors associated with breast cancer worry 3 years after completion of adjuvant treatment. Psycho-Oncology. 2013;22:936–9.
Easterling DV, Leventhal H. Contributions of concrete cognition to emotion: neutral symptoms as elicitors of worry about cancer. J Appl Psychol. 1989;74:787–96.
Hilton BA. The relationship of uncertainty, control, commitment, and threat of recurrence to coping strategies used by women diagnosed with breast cancer. J Behav Med. 1989;12:39–54.
Liu Y, Pérez M, Schootman M, et al. Correlates of fear of cancer recurrence in women with ductal carcinoma in situ and early invasive breast cancer. Breast Cancer Res Treat. 2011;130:165–73.
Mishel MH. Uncertainty in chronic illness. Annu Rev Nurs Res. 1999;17:269–94.
Lebel S, Maheu C, Lefebvre M, et al. Addressing fear of cancer recurrence among women with cancer: a feasibility and preliminary outcome study. J Cancer Survivorship. 2014;8:485–96.
Mishel MH, Germino BB, Gil KM, et al. Benefits from an uncertainty management intervention for African-American and Caucasian older long-term breast cancer survivors. Psycho-Oncology. 2005;14:962–78.
Mast ME. Survivors of breast cancer: illness uncertainty, positive reappraisal, and emotional distress. Oncol Nurs Forum. 1998;25:555–62.
Eisenberg SA, Kurita K, Taylor-Ford M, et al. Intolerance of uncertainty, cognitive complaints, and cancer-related distress in prostate cancer survivors. Psycho-Oncology. 2015;24:228–35.
Leventhal H, Diefenbach M, Leventhal EA. Illness cognition: using common sense to understand treatment adherence and affect cognition interactions. Cogn Ther Res. 1992;16:143–63.
Sharpe L, Curran L. Understanding the process of adjustment to illness. Soc Sci Med. 2006;62:1153–66.
Rabin C, Leventhal H, Goodin S. Conceptualization of disease timeline predicts posttreatment distress in breast cancer patients. Health Psychol. 2004;23:407–12.
Koch L, Bertram H, Eberle A, et al. Fear of recurrence in long-term breast cancer survivors-still an issue. Results on prevalence, determinants, and the association with quality of life and depression from the cancer survivorship—a multi-regional population-based study. Psycho-Oncology. 2014;23:547–54.
Lipkus IM, Klein WMP, Skinner CS, Rimer BK. Breast cancer risk perceptions and breast cancer worry: what predicts what? J Risk Res. 2005;8:439–52.
Humphries G, Rogers S. AFTER and beyond: cancer recurrence fears and test of an intervention in oropharyngeal patients. Soc Sci Dent. 2012;2:29–38.
Humphris GM, Ozackinci G. The AFTER intervention: a structured psychological approach to reduce fears of recurrence in patients with head and neck cancer. Br J Health Psychol. 2008;13:223–30.
Wells A, Matthews G. Modelling cognition in emotional disorder: the S-REF model. Behav Res Ther. 1996;34:881–8.
Cavanagh M, Franklin J. Attention training and hypochondriasis: preliminary results of a controlled treatment trial. World congress of cognitive and behavioral therapy. Vancouver, Canada 2000.
Baker P, Beesley H, Dinwoodie R, et al. ‘You’re putting thoughts into my head’: a qualitative study of the readiness of patients with breast, lung or prostate cancer to address emotional needs through the first 18 months after diagnosis. Psycho-Oncology. 2013;22:1402–10.
Macleod C, Hagan R. Individual differences in the selective processing of threatening information, and emotional responses to a stressful life event. Behav Res Ther. 1992;30:151–61.
Taylor L, Espie C, White C. Attentional bias in people with acute versus persistent insomnia secondary to cancer. Behav Sleep Med. 2003;1:200–12.
Chan MW, Ho SM, Tedeschi RG, Leung CW. The valence of attentional bias and cancer-related rumination in posttraumatic stress and posttraumatic growth among women with breast cancer. Psycho-Oncology. 2011;20:544–52.
Cook S, Salmon P, Dunn G et al. A prospective study of the association of metacognitive beliefs and processes with persistent emotional distress after diagnosis of cancer. Cogn Ther Res. 2014: 1–10.
Cook SA, Salmon P, Dunn G et al. The association of metacognitive beliefs with emotional distress after diagnosis of cancer. Health Psychol. 2014: No Pagination Specified.
Stanton AL, Danoff-burg S, Huggins ME. The first year after breast cancer diagnosis: hope and coping strategies as predictors of adjustment. Psycho-Oncology. 2002;11:93–102.
Deimling GT, Bowman KF, Sterns S, et al. Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psycho-Oncology. 2006;15:306–20.
Wells A. Detached mindfulness in cognitive therapy: a metacognitive analysis and ten techniques. J Ration Emot Cogn Behav Ther. 2005;23:337–55.
Lengacher C, Jonhson-Mallard V, Post-White J, et al. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psycho-Oncology. 2009;18:1261–72.
Lengacher CA, Johnson-Mallard V, Barta M, et al. Feasibility of a mindfulness-based stress reduction program for early-stage breast cancer survivors. J Holist Nurs. 2011;29:107–17.
Lengacher CA, Shelton MM, Reich RR, et al. Mindfulness based stress reduction (MBSR(BC)) in breast cancer: evaluating fear of recurrence (FOR) as a mediator of psychological and physical symptoms in a randomized control trial (RCT). J Behav Med. 2014;37:185–95.
Hayes SC, Luoma JB, Bond FW, et al. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44:1–25.
Hayes S, Strohsahl K, Wilson K. Acceptance and commitment therapy; an experiential approach to behaviour change. New York: Guildford Press; 2003.
Fletcher L, Hayes S. Relational frame theory, acceptance and commitment therapy, and a functional analytic definition of mindfulness. J Ration Emot Cogn Behav Ther. 2005;23:315–36.
Thewes B, Brebach R, Dzidowska M, et al. Current approaches to managing fear of cancer recurrence; a descriptive survey of psychosocial and clinical health professionals. Psycho-Oncology. 2014;23:390–6.
Feros DL, Lane L, Ciarrochi J, Blackledge JT. Acceptance and commitment therapy (ACT) for improving the lives of cancer patients: a preliminary study. Psychooncology. 2013;22:459–64.
Rost AD, Wilson K, Buchanan E, et al. Improving psychological adjustment among late-stage ovarian cancer patients: examining the role of avoidance in treatment. Cogn Behav Pract. 2012;19:508–17.
Zakowski SG, Valdimarsdottir HB, Bovbjerg DH, et al. Predictors of intrusive thoughts and avoidance in women with family histories of breast cancer. Ann Behav Med. 1997;19:362–9.
Mishel MH. Uncertainty in illness. Image J Nurs Sch. 1988;20:225–32.
Butow P, Bell M, Smith A, et al. Conquer fear: protocol of a randomised controlled trial of a psychological intervention to reduce fear of cancer recurrence. BMC Cancer. 2013;13:201.
Butow P, Kelly S, Thewes B, et al. Attentional bias and metacognitions in cancer survivors with high fear of cancer recurrence. Psycho-Oncology. 2015;24:416–23.
Thewes B, Bell ML, Butow P. Fear of cancer recurrence in young early-stage breast cancer survivors: the role of metacognitive style and disease-related factors. Psycho-Oncology. 2013;22:2059–63.
Persoskie A, Ferrer RA, Klein WM. Association of cancer worry and perceived risk with doctor avoidance: an analysis of information avoidance in a nationally representative us sample. J Behav Med. 2014;37:977–87.
Sharpe L, Thewes B, Butow P. Attentional biases in cancer survivors: directions for future research. Psycho-Oncology. 2015;24:496.
Lichtenthal WG, Tuman M, Beard C, et al. Development of attention and interpretation modification for fear of breast cancer recurrence (AIM-FBCR): preliminary findings. Psycho-Oncology. 2013;22:72–3.
Smith AB, Thewes B, Turner J et al. Pilot of a theoretically grounded psychologist-delivered intervention for fear of cancer recurrence (Conquer Fear). Psycho-Oncology 2015: n/a-n/a.
Acknowledgments
The work presented in this paper was co-funded by beyondblue, National Breast Cancer Foundation and Cancer Australia (CAPdCCRS 1022584).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This review was co-funded by Cancer Australia, beyondblue and National Breast Cancer Foundation (grant number 1022584).
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
No studies with human participants or animals were performed by any of the authors as part of this review.
Rights and permissions
About this article
Cite this article
Fardell, J.E., Thewes, B., Turner, J. et al. Fear of cancer recurrence: a theoretical review and novel cognitive processing formulation. J Cancer Surviv 10, 663–673 (2016). https://doi.org/10.1007/s11764-015-0512-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-015-0512-5