Abstract
Purpose
We investigated the association of physical activity with survival for 601 Hispanic women and 682 non-Hispanic white women who participated in the population-based breast cancer case-control New Mexico Women’s Health Study.
Methods
We identified 240 deaths among cases diagnosed with a first primary invasive breast cancer between 1992 and 1994, and 88 deaths among controls. Follow-up extended through 2012 for cases and 2008 for controls. Multivariable hazard ratios (HRs) and 95 % confidence intervals (CIs) were estimated using Cox proportional hazards regression.
Results
Higher levels of total physical activity were inversely associated with all-cause mortality among Hispanic cases (Quartile (Q)4: HR = 0.55, 95 % CI 0.31–0.99). A non-significant trend was observed for recreational activity in Hispanic cases also (Q4: HR = 0.50, 95 % CI 0.23–1.09, p for trend = 0.08). No significant associations were noted for non-Hispanic white cases or for controls.
Conclusions
The results suggest that increasing physical activity may be protective against mortality in Hispanic women with breast cancer, despite reporting lower levels of recreational activity than non-Hispanic white women or Hispanic controls.
Implications for Cancer Survivors
Public health programs in Hispanic communities should promote physical activity in women as a means of decreasing breast cancer risk and improving survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Breast cancer is the most common form of cancer diagnosed among women [1]. With advances in early detection and breast cancer treatment, the population of long-term survivors is growing. Breast cancer survivors are often interested in modifying health behaviors, including increasing physical activity, which could positively influence cancer prognosis [1, 2]. Potential biological mechanisms influencing the association of physical activity with cancer risk and prognosis include shifts in insulin, sex hormones, and inflammation levels [3].
Accumulating epidemiological evidence indicates that moderate to vigorous intensity levels of physical activity are positively associated with improved survival in women diagnosed with breast cancer [4–18]. While the magnitude of estimates were similar, these studies differed in the timing of measured physical activity; some reported activity before breast cancer diagnosis [4, 8–10, 17, 18], others after diagnosis [5–7, 11, 12, 15, 16], and the remaining presented separate analyses for pre- and post-diagnostic levels [13, 14]. Ballard-Barbash et al. [19] conducted a systematic review summarizing 17 reports published through August 2011, and concluded that pre-diagnosis (9 studies) or post-diagnosis (8 studies) physical activity consistently showed a reduction in both breast cancer-specific and all-cause mortality. A recent meta-analysis [20] reported summary estimates that were significantly reduced for the association between pre-diagnosis physical activity and breast cancer-specific mortality (hazard ratio (HR) = 0.77, 95 % confidence interval (CI) 0.66–0.90) and total mortality (HR = 0.77, 95 % CI 0.69–0.88). Summary estimates for post-diagnosis were similar for breast cancer-specific mortality; however, results were stronger for total mortality (HR = 0.52, 95 % CI 0.42–0.64). No heterogeneity among studies was observed [20].
Previous studies also vary on the specific types of activity considered. Few studies examined a full range of physical activity [10, 16], with most restricted to recreational or leisure activities. The type of physical activity also may be important when evaluating differences in effects across race or ethnicity. Slattery et al. [21] found that the most frequently reported activities among Hispanic women were walking, housework, and gardening, while non-Hispanic white women most frequently reported sports-based activities. In a study conducted by Neighbors et al. [22], levels of leisure-time physical activity were lower in Hispanic versus non-Hispanic white women. These findings suggest that studies including Hispanic women should examine non-recreational activities.
The focus of most studies investigating the association of physical activity and breast cancer survival has been based predominantly on non-Hispanic white populations. Hispanic participants, when included, are few in number. Several studies have adjusted for ethnicity in analysis [4, 5, 9, 13, 14, 18, 16]; however, the Breast Cancer Family Registry, a multinational study of participants in the USA, Canada, and Australia, was the only previous study to present a subgroup analysis by ethnicity, including a small sample of Hispanic women (n = 148) diagnosed with estrogen receptor positive breast cancer [18]. Lastly, few studies have compared associations of physical activity with mortality in cases with a sample of population-based, matched controls. Such a comparison would better establish whether breast cancer diagnosis affects patterns of physical activity to alter associations with mortality.
The present report investigated the association of pre-diagnostic total, recreational, and non-recreational physical activity with breast cancer-specific, all-cause, and non-cancer mortality among Hispanic and non-Hispanic white women who participated in the New Mexico Women’s Health Study (NMWHS). Previous results from this study found an association with pre-diagnosis physical activity levels and reduced risk of breast cancer in Hispanic women but not non-Hispanic white women [23].
Methods
Study participants
The NMWHS was a population-based case-control study designed to investigate risk factors for breast cancer in Hispanic and non-Hispanic white women and has been previously described [24]. Briefly, women were eligible to be included in the study if they were diagnosed with an invasive or in situ breast cancer from 1992 to 1994. Cases were ascertained through the New Mexico Tumor Registry, a member of the Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute. All Hispanic cases and 33 % of non-Hispanic white cases, randomly selected by age-group and geographical region, were considered eligible. A total of 722 cases completed in-person interviews, including a risk factor and a food frequency questionnaire. We excluded cases from the current analysis if they had an unknown first cancer diagnosis or their diagnosis was misclassified or if they had a prior breast cancer diagnosis (n = 30), if they were diagnosed with in situ breast cancer (n = 110), if their stage of disease was classified as unknown (n = 5), or if there were missing data for physical activity (n = 22) or menopausal status, estrogen use, daily energy intake, or body mass index (BMI) (n = 15). A total of 540 cases were eligible for the present analyses.
Random-digit dialing was used to select the controls. They were matched to cases based on ethnicity, age-group, and geographic region. A total of 844 controls completed interviews. Controls were included in analyses to determine if the survival benefit of physical activity differed in a population of women with breast cancer versus those without. Controls were excluded if they had a previous breast cancer diagnosis (n = 60) including four breast cancer deaths, if they were missing physical activity data (n = 13) or were missing estrogen use, daily energy intake, or BMI data (n = 28). A total of 743 controls were eligible for the present analyses.
The NMWHS was approved by the Human Research Protections Office at the University of New Mexico. A follow-up study of survival and quality of life in both cases and controls was conducted and approved by the Institutional Review Board for Human Subjects at the University of Louisville.
Mortality ascertainment
Women were followed from date of diagnosis for cases, and date of baseline interview for controls to date of death or last available date of death information (December 31, 2012 for cases; December 31, 2008 for controls), whichever came first. Date of death and the underlying cause of death were verified through linkage to the National Death Index for controls and the New Mexico Tumor Registry for cases.
Physical activity assessment
Women were asked in the baseline interview to report activities performed regularly during the year (for at least 6 months) preceding study eligibility, as well as the average time spent in those activities during a week. Activities included: walking/hiking, running/jogging, exercise class, biking, dancing, lap swimming, tennis, squash/racquetball, calisthenics/rowing, bowling, golf, softball/baseball, basketball, volleyball, housework, and yard work/gardening. Duration was reported as the number of hours per week (<1, 1.5, 2–3, 4–6, 7–10, >10 h) spent engaged in the activity.
Each activity was assigned a metabolic equivalent task (MET) as a measure of the relative energy expenditure and was based on the 2011 classification by Ainsworth et al. [25]. Sitting is equivalent to 1.0 MET; walking at an average pace for an hour (2.5 MPH) is equivalent to 3.0 METs. Moderate scores were selected for activities with multiple MET values (e.g. walking, hiking, swimming, tennis, calisthenics, rowing, yard work, gardening, housework). To compute the average weekly expenditure for each activity, the MET was multiplied by the midpoint of the selected range of hours per week, except the highest category, which was multiplied by 12. These were summed to obtain total MET-hours/week (MET-h/week).
Total physical activity, recreational physical activity, and non-recreational physical activity were categorized into quartiles based on the distribution within each stratum for cases and controls separately. This ensured an adequate comparison of women participating in higher levels of physical activity to those with lower levels of activity.
Covariates
Covariates were selected for inclusion based on independent associations with mortality in univariate analyses or a change >10 % in the effect estimates in the multivariable analyses. Clinical and tumor characteristic data were obtained from the New Mexico Tumor Registry, and included SEER summary stage (local [referent] vs. regional and distant), breast cancer treatment (surgery only [referent], surgery with radiation, surgery with chemotherapy, surgery with radiation and chemotherapy, and no surgery), and age at diagnosis.
Baseline characteristics were obtained from the risk factor questionnaire. Ethnicity was self-reported. BMI was computed using self-reported height (meters) and weight (kilograms) and calculated as kilograms per square meter. Women were asked questions regarding menstruation and menopausal history. Based on the responses, subjects were classified as pre-menopausal, post-menopausal, or surgical unknown. Women who responded that they were pregnant, had a period in the last 12 months without hormone-replacement therapy, or were younger than 44 years, and had a hysterectomy with intact ovaries were classified as pre-menopausal. “Surgical unknown” was assigned to women between the ages of 44 and 53 who reported a hysterectomy with intact ovaries. The remaining subjects were identified as post-menopausal. Women were asked to report all periods of estrogen use, which was summed and categorized for analyses (never [referent], ≤1 year, 1 to ≤4 years, 4 to ≤10 years, >10 years). Baseline energy intake (kilocalories per day) was collected using a standardized food frequency questionnaire and categorized by quartiles based on the distribution of eligible cases.
Other covariates considered but not included in the final models due to <10 % change in effect were years of oral contraceptive use (never used [referent], <1.5 years, 1.5 to <5 years, 5+ years), age at first live birth (≤18 years, 19–20, 21–22, 23–26, ≥27, nulliparous [referent]), parity (nulliparous, 1, 2, 3, ≥4 [referent]), years of breast feeding (nulliparous; parous, 1–12 months; parous, >12 months; parous, never [referent]), first- and second-degree family history (yes/no), estrogen receptor status (positive versus negative), educational level (<12 years, 12 years [referent], >12 years), employment status (employed versus unemployed), and smoking status (ever versus never).
Statistical analysis
Cox proportional hazards models [26] were calculated separately by ethnicity to estimate hazard ratios and 95 % confidence intervals of death classified as any cause, breast cancer-specific, and non-breast cancer-specific mortality. The underlying time metric was follow-up time calculated as date of diagnosis for cases or date of baseline interview for controls to date of death or last date of available death information, whichever came first. The average follow-up time was 14.7 years in cases and 13.3 years in breast cancer-free controls. For the analyses involving breast cancer-specific outcomes or non-breast cancer-specific outcomes, deaths due to other causes were censored at date of death. Except where noted, all models were adjusted for potential confounders. The hazard ratios were stratified by quartiles of MET-h/week with the lowest quartile of activity as the reference group. The median value for each category was used to calculate the P value for the linear test of trend [27]. The proportional hazards assumption was tested statistically by interacting covariates with time [26]. These effects were not significant in our models and we determined there were no violations. All analyses were performed using SAS version 9.3 with a significance level of <0.05.
Results
A total of 240 (44 %) cases died during the follow-up period. The primary cause of death was breast cancer (n = 132), accounting for 55 % of all deaths. The remaining 108 deaths were other cancers (n = 38), heart disease (n = 21), accidental death (n = 6), chronic obstructive pulmonary disease (n = 6), diabetes (n = 4), stroke (n = 4), liver disease or cirrhosis (n = 3), and miscellaneous other deaths (n = 26). The total person-years of follow-up were 7,947 years. Among those who died, the average follow-up time was 8.9 years for death by any cause, 6.8 years for death from breast cancer, and 11.4 years for non-breast cancer-specific causes.
There were 88 non-breast cancer-specific deaths among the 743 breast cancer-free controls during the follow-up period. These included heart disease (n = 25), other cancer (n = 25), chronic pulmonary lung disease (n = 9), and miscellaneous other deaths (n = 29). Controls were followed for a total of 9,903 person-years. The average follow-up time among those who died was 8.6 years.
Age-standardized descriptive characteristics and covariates are presented in Table 1 according to quartiles of physical fitness and ethnicity for cases and controls. In general, Hispanic cases were younger at diagnosis than non-Hispanic white cases, and non-Hispanic white cases were more likely to be post-menopausal at baseline. While total physical activity was similar, recreational activity tended to be lower and non-recreational activity higher in Hispanic compared to non-Hispanic white cases. In contrast, controls were of similar age, regardless of ethnicity, and Hispanic controls in the lowest quartile of exercise were more likely to be post-menopausal at baseline than non-Hispanic white controls in the same quartile. Levels of total, recreational, and non-recreational activity were closely similar in Hispanic and non-Hispanic white controls, and levels were higher for controls than for cases. Hispanic women had a higher BMI than non-Hispanic white women. In contrast to the non-Hispanic white women, BMI did not significantly decrease with increasing physical activity level in Hispanic cases. Hispanic women reported a higher caloric intake at the highest level of physical activity than non-Hispanic white women.
Age-standardized clinical characteristics by level of physical activity and ethnicity for cases are presented in Table 2. Hispanic cases were diagnosed with more advanced stage of disease and were less likely to receive radiation therapy. Chemotherapy was used more often in Hispanic cases with higher levels of physical activity. Non-Hispanic white cases with higher levels of total physical activity were more likely to have ER-positive tumors.
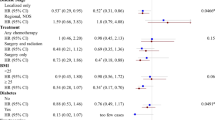
Table 3 presents the multivariable-adjusted hazard ratios of all-cause and breast cancer-specific mortality in cases and non-breast cancer-specific mortality in cases and controls by level of total, recreational, and non-recreational physical activity, stratified by ethnicity. Stage of disease was coded as local versus a combined regional and distant stage because results did not change significantly (data not shown) when women diagnosed with distant stage were excluded (n = 16). The results indicate that higher levels of total physical activity are associated with decreased risk of all-cause mortality in Hispanic cases. In contrast, there was no association in non-Hispanic white cases. Compared with women in the lowest category of total physical activity, Hispanic cases in the highest levels of activity had a multivariable hazard ratio of 0.55 (95 % CI 0.31–0.99) for all-cause mortality, 0.49 (95 % CI 0.23–1.04) for breast cancer-specific mortality, and 0.78 (95 % CI 0.29–2.11) for non-breast cancer-specific mortality. For the non-Hispanic white cases, the hazard ratios for total physical activity were 0.99 (95 % CI 0.58–1.68), 0.66 (95 % CI 0.31–1.43), and 1.35 (95 % CI 0.60–3.02) for all-cause, breast cancer-specific, and non-breast cancer-specific mortality, respectively. There was a non-significant trend toward a protective association for recreational activity with all-cause (0.50, 95 % CI 0.23–1.09, p for trend = 0.08) and breast cancer-specific mortality (0.48, 95 % CI 0.19–1.27, p for trend = 0.06) for Hispanic cases also, but not for non-Hispanic cases. There were no associations with non-recreational activity in either Hispanic or non-Hispanic white cases with all-cause, breast cancer-specific, or non-breast cancer mortality. Hispanic controls at the highest level of total physical activity had a multivariable hazard ratio of 0.38 (95 % CI 0.12–1.27) but did not have a statistically significant linear trend of increased survival (p trend = 0.10). There were no statistically significant associations with either recreational or non-recreational activity.
Discussion
Our results suggest that total physical activity in the year before diagnosis is associated with improved all-cause survival in Hispanic women with breast cancer. A similar protective association was not apparent in more active breast cancer-free Hispanic women. Additionally, our results suggest that the protection of physical activity may be stronger for recreational than non-recreational physical activities for Hispanic women. Taken together, these results suggest that physical activity is associated with better survival for Hispanic women with a history of breast cancer. This association was not apparent in non-Hispanic white women.
There are some distinct differences between the present study and previous ones of the association of physical activity with survival in women diagnosed with breast cancer. The current study is the largest to date to examine the association of physical activity and mortality after breast cancer diagnosis in Hispanic women. While most studies suggest that vigorous recreational activity is associated with lower mortality in women with breast cancer, our study suggests that the strength of this association may be ethnic-specific. Despite the fact that Hispanic women in our study reported more household and less recreational activity than non-Hispanic white women, associations of total and recreational activity with all-cause and breast cancer mortality were stronger in Hispanic than non-Hispanic white women. Most studies have examined only associations with all-cause and breast cancer-specific mortality and have not examined non-breast cancer-specific mortality separately. Our results suggest that physical activity is not associated with non-breast cancer-specific mortality in either Hispanic or non-Hispanic white women. Moreover, there were no associations between physical activity and non-breast cancer mortality in controls. These findings strengthen the evidence for a direct effect of physical activity on survival in women with breast cancer, rather than an indirect effect on mortality due to other causes. To our knowledge, our study is the only one derived from a population-based case-control study to report parallel analyses comparing the associations of physical activity with mortality in women with and without diagnosed breast cancer.
In the present study, Hispanic and non-Hispanic white women differed in the strength and statistical significance of association of physical activity with both breast cancer risk and survival. This difference cannot be ascribed to statistical power because the study design ensured that the ethnic groups were of similar size and the number of deaths did not differ substantially between groups. The current results for survival are consistent with the ethnic difference in the association of physical activity with breast cancer risk reported previously for the NMWHS [23]. Although the previous analysis used METs-h/week values based on the 1993 compendium [28], we believe the association cannot be attributed to recalculation of the MET values with the updated 2011 compendium because recalculation did not greatly change the previously observed trend (Hispanic: original estimate: odds ratio (OR) = 0.30, 95 % CI 0.18–0.49 [23]; recalculated estimate: OR = 0.31, 95 % CI 0.18–0.53; non-Hispanic white: original estimate [23]: OR = 0.67, 95 % CI 0.43–1.06; recalculated estimate: OR = 0.76, 95 % CI 0.48–1.22). Taken together, these results appear to suggest that Hispanic women may be more sensitive to the beneficial effects of physical activity on breast cancer survival as well as risk than non-Hispanic white women.
The ethnic difference in the strength of the associations does not appear to be attributable to different patterns of physical activity. The five most frequently reported activities in the NMWHS were housework, yard work/gardening, walking/hiking, and exercise classes for all women, dancing for Hispanic women, and biking for non-Hispanic white women. Household activities accounted for 62.2 % of total activity in Hispanic cases versus 52.9 % in non-Hispanic white cases. The 4-Corners Breast Cancer Study also indicated that Hispanic women in the southwestern USA are more likely to report housework than non-Hispanic white women [21]. Nonetheless, non-recreational activities were not associated with all-cause or breast cancer-specific mortality in either ethnic group. Thus, it remains unclear whether ethnic differences in the associations of total physical activity are due to different patterns of physical activity.
Several previous studies have investigated the associations of physical activity before diagnosis with mortality in women with breast cancer. The majority, however, mainly considered only recreational activities and few stratified analyses by race or ethnicity. Although occupational and household activities were measured in the Health, Eating, Activity and Lifestyle (HEAL) Study, results were only reported for recreational activity for which non-significant protective associations were observed at the highest level of activity (≥9 MET-h/week/year) for breast cancer-specific (HR = 0.83, 95 % CI 0.49–1.38) and all-cause mortality (HR = 0.69, 95 % CI 0.45–1.06) [14]. While the HEAL Study included Hispanic women, the number was too small to provide precise estimates for this ethnic group. The Life After Cancer Epidemiology (LACE) Study combined household, occupational, recreational, and transportation activities, and graded these as moderate and vigorous using both MET-hours/week and hours/week. A statistically significant protective trend (p = 0.04) was observed only between hours/week of moderate physical activity and all-cause mortality (HR = 0.66, 95 % CI 0.42–1.03) for > 6 h/week [16]. Similar to the present study design, Friedenreich et al. [10] followed cases from a population-based case-control study conducted in Canada for all-cause and breast cancer-specific mortality over a 10-year period. Physical activity was defined in terms of MET hours/week of total, recreational, occupational, and household activities. Decreased risk of all-cause (HR = 0.73, 95 % CI 0.53–1.00) and breast cancer-specific (HR = 0.54, 95 % CI 0.36–0.79) mortality was observed only for the highest levels of recreational activity. In contrast to our results, they reported an increased risk of all-cause mortality for the highest level of non-recreational, household activity (HR = 1.46, 95 % CI 1.02–2.09). The Collaborative Women’s Longevity Study reported an inverse association between total recreational physical activity and both breast cancer-specific and all-cause mortality [11]. The National Institutes of Health (NIH)-American Association of Retired Persons (AARP) Diet and Health Study concluded that routine activity during the day, including household activities, may be associated with a reduced risk of breast cancer [29].
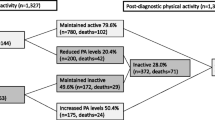
A few studies have examined associations of survival with physical activity after diagnosis also. Holmes et al. [12] analyzed the association of physical activity measured within 2 years following breast cancer diagnosis with mortality in women in the Nurses’ Health Study, and reported statistically significant protective trends with increasing MET-hours/week for both all-cause and breast cancer mortality. The associations of physical activity measured before diagnosis and 2 years after diagnosis with mortality were compared in the HEAL Study [14]. There were statistically significant (p < 0.05) protective trends for all-cause, but not breast cancer-specific mortality with increasing physical activity both before and after diagnosis. Moreover, compared to women who were relatively inactive at both time points, women who decreased activity following diagnosis had increased risk of both all-cause and breast cancer mortality, while women who increased their activity had decreased risk. Bradshaw et al. [30] recently reported that among women categorized in the highest physical activity tertile (>9.0 yearly MET h/week) in the Long Island Breast Cancer Study, the association in the first 2 years post-diagnosis for physical activity with all-cause mortality (HR = 0.14, 95 % CI 0.03–0.44) and breast cancer-specific mortality (HR = 0.18, 95 % CI 0.05–0.59) was stronger than in the follow-up period greater than 2 years (HR = 0.37, 95 % CI 0.25–0.55; HR = 0.30, 95 % CI 0.16–0.56, respectively).
In a cohort of women diagnosed with breast cancer, all-cause mortality includes both breast cancer-specific and non-breast cancer deaths. It is not possible in this design to determine whether a breast cancer diagnosis alters the association of physical activity with non-breast cancer mortality. Results from some previous studies for associations with all-cause, but not breast cancer-specific mortality, could be due to beneficial effects of physical activity on non-breast cancer mortality; in other words, improvements in mortality associated with comorbidity such as cardiovascular disease. Our study design allowed us to compare the associations of physical activity with non-breast cancer mortality in women with and without breast cancer. There were no associations in either cases or controls for non-breast cancer mortality. This result should be taken with caution, however, until replicated by other studies with follow-up for population-based samples of women without breast cancer who are appropriately matched for age, geographic region, and ethnicity to women diagnosed with breast cancer.
The main strengths of the present study included the population-based design with follow-up of Hispanic and non-Hispanic white women with breast cancer and women without a breast cancer diagnosis matched for age and geographic region, and the analysis of non-recreational household activity in addition to recreational and total activity. The primary limitations were the sample size and the collection of self-reported physical activity before diagnosis (or enrollment for controls) only. Thus, despite having one of the largest cohorts of Hispanic women to date, our results are somewhat imprecise and unstable and need to be replicated in a larger study. In addition, we were unable to examine protective effects of post-diagnosis physical activity or changes in physical activity over time. We believe, however, that the pre-diagnosis level of activity in our population is an adequate measure because in studies where both pre- and post-diagnostic levels of activity have been examined, inverse associations or trends are found in both measures [13, 14], and while breast cancer survivors may decrease their activity during the treatment period, particularly obese patients and those treated with chemotherapy [31], pre-diagnostic levels of physical activity generally predict post-diagnostic activity [32].
Another limitation is potential differential information bias, which may occur when groups being compared differ systematically in the accuracy of self-reported information. Some studies suggest that overweight women may overreport physical activity [33]. However, while the mean BMI of Hispanic women was higher than in non-Hispanic white women in our study, self-reported total physical activity was lower. Additionally, the overall mean BMI is comparable to that reported for Hispanic women in the Health, Eating, Activity, and Lifestyle study (27.7, SD = 6.2) [34], and in the 4-Corners Breast Cancer Study (28.0, SD = 0.25) [35]. Self-reported behaviors, including physical activity may be influenced by cultural beliefs, and Hispanic and non-Hispanic white women may value types of physical activities, such as non-recreational or recreational activities, differently leading to differential reporting bias. Self-reported behavior can also be influenced by an informant’s knowledge of reported associations of a behavior or exposure with an outcome of interest. However, we think that this is an unlikely influence in this study given that data were collected between 1994 and 1996. Although there was one study published prior to this in 1985 on the association between physical activity and breast cancer [36], other reports on the benefits of physical activity in relation to cancer occurred after the 1996 Surgeon General’s Report, which found results to be inconsistent [37]. More definitive results were later released in 2002 by the American Cancer Society [38], World Health Organization [39], and International Agency for Research on Cancer [40].
In conclusion, increased levels of physical activity were inversely associated with mortality in Hispanic women. Although we were unable to detect a significant association among non-Hispanic white women, physical activity may be beneficial to breast cancer survivors for other reasons including quality of life and higher levels of physical fitness. Similar to previous studies, our findings indicate that Hispanic women report lower levels of recreational physical activity than non-Hispanic white women [22]. However, levels of non-recreational physical activity were somewhat higher in Hispanic than non-Hispanic white women in our study, resulting in closely similar levels of total physical activity. Future studies should examine more closely ethnic differences in physical activity literacy, barriers to exercise, as well as types of self-reported activities as these differences may influence results. It is important to look at factors that may increase the probability of participation in physical activity [41, 42], and design interventions that are culturally tailored to address perceived barriers for initiating physical activity [43]. Additionally, comparison to appropriate samples of controls without breast cancer should be made to determine if a diagnosis of breast cancer alters the association of physical activity with subsequent mortality as well as comorbidity and quality of life. These studies will provide data for evidence-based recommendations for interventions to promote physical activity among Hispanic women.
Abbreviations
- AARP:
-
American Association of Retired Persons
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- HEAL:
-
Health, Eating, Activity and Lifestyle Study
- HR:
-
Hazard ratio
- LACE:
-
Life After Cancer Epidemiology
- MET:
-
Metabolic equivalent task
- MET-h/week:
-
Metabolic equivalent task in hours per week
- NIH:
-
National Institutes of Health
- NMWHS:
-
New Mexico Women’s Health Study
- Q:
-
Quartile
- SEER:
-
Surveillance, Epidemiology, and End Results
References
DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, et al. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64(4):252–71.
Cancer survivors: living longer, and now, better. Lancet. 2004;364(9452):2153-4.
McTiernan A. Mechanisms linking physical activity with cancer. Nat Rev Cancer. 2008;8(3):205–11.
Abrahamson PE, Gammon MD, Lund MJ, Britton JA, Marshall SW, Flagg EW, et al. Recreational physical activity and survival among young women with breast cancer. Cancer. 2006;107(8):1777–85.
Beasley JM, Kwan ML, Chen WY, Weltzien EK, Kroenke CH, Lu W, et al. Meeting the physical activity guidelines and survival after breast cancer: findings from the after breast cancer pooling project. Breast Cancer Res Treat. 2012;131(2):637–43.
Bertram LA, Stefanick ML, Saquib N, Natarajan L, Patterson RE, Bardwell W, et al. Physical activity, additional breast cancer events, and mortality among early-stage breast cancer survivors: findings from the WHEL Study. Cancer Causes Control. 2011;22(3):427–35.
Chen X, Lu W, Zheng W, Gu K, Matthews CE, Chen Z, et al. Exercise after diagnosis of breast cancer in association with survival. Cancer Prev Res. 2011;4(9):1409–18.
Cleveland RJ, Eng SM, Stevens J, Bradshaw PT, Teitelbaum SL, Neugut AI, et al. Influence of prediagnostic recreational physical activity on survival from breast cancer. Eur J Cancer Prev. 2012;21(1):46–54.
Enger SM, Bernstein L. Exercise activity, body size and premenopausal breast cancer survival. Br J Cancer. 2004;90(11):2138–41.
Friedenreich CM, Gregory J, Kopciuk KA, Mackey JR, Courneya KS. Prospective cohort study of lifetime physical activity and breast cancer survival. Int J Cancer. 2009;124(8):1954–62.
Holick CN, Newcomb PA, Trentham-Dietz A, Titus-Ernstoff L, Bersch AJ, Stampfer MJ, et al. Physical activity and survival after diagnosis of invasive breast cancer. Cancer Epidemiol Biomarkers Prev. 2008;17(2):379–86.
Holmes MD, Chen WY, Feskanich D, Kroenke CH, Colditz GA. Physical activity and survival after breast cancer diagnosis. JAMA. 2005;293(20):2479–86.
Irwin ML, McTiernan A, Manson JE, Thomson CA, Sternfeld B, Stefanick ML, et al. Physical activity and survival in postmenopausal women with breast cancer: results from the Women's Health Initiative. Cancer Prev Res. 2011;4(4):522–9.
Irwin ML, Smith AW, McTiernan A, Ballard-Barbash R, Cronin K, Gilliland FD, et al. Influence of pre- and postdiagnosis physical activity on mortality in breast cancer survivors: the Health, Eating, Activity, and Lifestyle Study. J Clin Oncol. 2008;26(24):3958–64.
Pierce JP, Stefanick ML, Flatt SW, Natarajan L, Sternfeld B, Madlensky L, et al. Greater survival after breast cancer in physically active women with high vegetable-fruit intake regardless of obesity. J Clin Oncol. 2007;25(17):2345–51.
Sternfeld B, Weltzien E, Quesenberry Jr CP, Castillo AL, Kwan M, Slattery ML, et al. Physical activity and risk of recurrence and mortality in breast cancer survivors: findings from the LACE study. Cancer Epidemiol Biomarkers Prev. 2009;18(1):87–95.
West-Wright CN, Henderson KD, Sullivan-Halley J, Ursin G, Deapen D, Neuhausen S, et al. Long-term and recent recreational physical activity and survival after breast cancer: the California Teachers Study. Cancer Epidemiol Biomarkers Prev. 2009;18(11):2851–9.
Keegan TH, Milne RL, Andrulis IL, Chang ET, Sangaramoorthy M, Phillips KA, et al. Past recreational physical activity, body size, and all-cause mortality following breast cancer diagnosis: results from the Breast Cancer Family Registry. Breast Cancer Res Treat. 2010;123(2):531–42.
Ballard-Barbash R, Friedenreich CM, Courneya KS, Siddiqi SM, McTiernan A, Alfano CM. Physical activity, biomarkers, and disease outcomes in cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104(11):815–40.
Schmid D, Leitzmann MF. Association between physical activity and mortality among breast cancer and colorectal cancer survivors: a systematic review and meta-analysis. Ann Oncol. 2014;25(7):1293–311.
Slattery ML, Sweeney C, Edwards S, Herrick J, Murtaugh M, Baumgartner K, et al. Physical activity patterns and obesity in Hispanic and non-Hispanic white women. Med Sci Sports Exerc. 2006;38(1):33–41.
Neighbors CJ, Marquez DX, Marcus BH. Leisure-time physical activity disparities among Hispanic subgroups in the United States. Am J Public Health. 2008;98(8):1460–4.
Gilliland FD, Li YF, Baumgartner K, Crumley D, Samet JM. Physical activity and breast cancer risk in Hispanic and non-Hispanic white women. Am J Epidemiol. 2001;154(5):442–50.
Gilliland FD, Hunt WC, Baumgartner KB, Crumley D, Nicholson CS, Fetherolf J, et al. Reproductive risk factors for breast cancer in Hispanic and non-Hispanic white women: the New Mexico Women's Health Study. Am J Epidemiol. 1998;148(7):683–92.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett Jr DR, Tudor-Locke C, et al. Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–81.
Cox DR. Regression models and life-tables. J R Stat Soc B Stat Methodol. 1972;34(2):187–220.
Selvin S. Statistical tools for epidemiologic research. New York: Oxford University Press; 2011.
Ainsworth BE, Haskell WL, Leon AS, Jacobs Jr DR, Montoye HJ, Sallis JF, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25(1):71–80.
George SM, Irwin ML, Matthews CE, Mayne ST, Gail MH, Moore SC, et al. Beyond recreational physical activity: examining occupational and household activity, transportation activity, and sedentary behavior in relation to postmenopausal breast cancer risk. Am J Public Health. 2010;100(11):2288–95.
Bradshaw PT, Ibrahim JG, Khankari N, Cleveland RJ, Abrahamson PE, Stevens J, et al. Post-diagnosis physical activity and survival after breast cancer diagnosis: the Long Island Breast Cancer Study. Breast Cancer Res Treat. 2014;145(3):735–42.
Kwan ML, Sternfeld B, Ergas IJ, Timperi AW, Roh JM, Hong CC, et al. Change in physical activity during active treatment in a prospective study of breast cancer survivors. Breast Cancer Res Treat. 2012;131(2):679–90.
Mason C, Alfano CM, Smith AW, Wang CY, Neuhouser ML, Duggan C, et al. Long-term physical activity trends in breast cancer survivors. Cancer Epidemiol Biomarkers Prev. 2013;22(6):1153–61.
Irwin ML, Ainsworth BE, Conway JM. Estimation of energy expenditure from physical activity measures: determinants of accuracy. Obes Res. 2001;9(9):517–25.
Baumgartner KB, Hunt WC, Baumgartner RN, Crumley DD, Gilliland FD, McTiernan A, et al. Association of body composition and weight history with breast cancer prognostic markers: divergent pattern for Hispanic and non-Hispanic White women. Am J Epidemiol. 2004;160(11):1087–97.
Slattery ML, Sweeney C, Herrick J, Wolff R, Baumgartner K, Giuliano A, et al. ESR1, AR, body size, and breast cancer risk in Hispanic and non-Hispanic white women living in the Southwestern United States. Breast Cancer Res Treat. 2007;105(3):327–35.
Frisch RE, Wyshak G, Albright NL, Albright TE, Schiff I, Jones KP, et al. Lower prevalence of breast cancer and cancers of the reproductive system among former college athletes compared to non-athletes. Br J Cancer. 1985;52(6):885–91.
United States Public Health Service. Office of the Surgeon General, National Center for Chronic Disease Prevention and Health Promotion (U.S.). Physical activity and health: a report of the Surgeon General. Atlanta, Ga., 1996.
Byers T, Nestle M, McTiernan A, Doyle C, Currie-Williams A, Gansler T, et al. American Cancer Society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2002;52(2):92–119.
World Health Organization. The World Health Report 2002. Reducing risk, promoting healthy life. Geneva: Switzerland; 2002.
International Agency for Research on Cancer (IARC). Weight control and physical activity. Lyon, France. 2002.
Bautista L, Reininger B, Gay JL, Barroso CS, McCormick JB. Perceived barriers to exercise in Hispanic adults by level of activity. J Phys Act Health. 2011;8(7):916–25.
Eyler AE, Wilcox S, Matson-Koffman D, Evenson KR, Anderson BS, Thompson J, et al. Correlates of physical activity among women from diverse racial/ethnic groups. J Womens Health. 2002;11(3):239–53.
Ickes MJ, Sharma M. A systematic review of physical activity interventions in Hispanic adults. J Environ Public Health. 2012;156435. doi:10.1155/2012/156435.
Acknowledgments
The work was supported by the following grants: NIH/NCI, R01-CA55730 The New Mexico Women’s Health Study and NIH/NCI, R01-CA105266 Ethnicity, Breast Cancer Recurrence and Long-Term Quality of Life.
Conflicts of interest
All authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pinkston, C.M., Baumgartner, R.N., Connor, A.E. et al. Physical activity and survival among Hispanic and non-Hispanic white long-term breast cancer survivors and population-based controls. J Cancer Surviv 9, 650–659 (2015). https://doi.org/10.1007/s11764-015-0441-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-015-0441-3