Abstract
Purpose
We compare breast and colorectal cancer survivors’ annual receipt of preventive care and office visits to that of age- and gender-matched cancer-free controls.
Methods
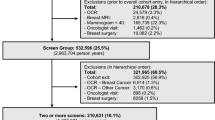
Automated data, including tumor registries, were used to identify insured individuals aged 50+ at the time of breast or colorectal cancer diagnosis between 2000 and 2008 as well as cancer-free controls receiving care from four integrated delivery systems. Those with metastatic or un-staged disease, or a prior cancer diagnosis were excluded. Annual visits to primary care, oncology, and surgery as well as receipt of mammography, colorectal cancer, Papanicolaou, bone densitometry, and cholesterol screening were observed for 5 years. We used generalized estimating equations that accounted for repeated observations over time per person to test annual service use differences by cancer survivor/cancer-free control status and whether survivor/cancer-free status associations were moderated by patient age <65 years and calendar year of diagnosis.
Results
A total of 3743 breast and 1530 colorectal cancer survivors were identified, representing 12,923 and 5103 patient-years of follow-up, respectively. Compared to cancer-free controls, breast and colorectal cancer survivors were equally or more likely to use all types of office visits and to receive cancer screenings and bone densitometry testing. Both breast and colorectal cancer survivors were less likely than cancer-free controls to receive cholesterol testing, regardless of age, year of diagnosis, or use of primary care.
Implications for Cancer Survivors
Programs targeting cancer survivors may benefit from addressing a broad range of primary preventive care needs, including recommended cardiovascular disease screening.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
By 2022, the number of US cancer survivors is projected to be approximately 18 million, with almost a third being breast or colorectal cancer survivors [1]. Because of advances in early detection and treatment, many survivors will live for decades. For many survivors, the risk of mortality from other health conditions—particularly cardiovascular disease—will exceed the risk from cancer [2, 3]. Routine preventive care, independent of care related to cancer follow-up, is therefore at least as important among cancer survivors as among the general population.
Studies conducted with self-reported health care data among US adults have generally found that survivors are equally or more likely to report receipt of recommended preventive care than adults with no history of cancer [4–8]. Findings from claims-based studies have had more mixed results. For example, Earle and Neville [9] found elderly colorectal cancer survivors diagnosed between 1991 and 1992, compared to cancer-free controls, significantly less likely to receive recommended preventive care (e.g., cervical cancer screening, cholesterol testing, influenza vaccinations, and bone densitometry testing) 6–7 years following their cancer diagnosis. But members of the same team found the opposite to be true among a cohort of breast cancer survivors that were similarly identified [10]. Since then, two additional studies [11, 12] have found elderly breast cancer survivors less likely to receive recommended preventive care relative to matched controls. Among these claims-based studies, none has reported on individuals diagnosed within the past 10 years or those diagnosed prior to their 65th birthdays.
To bridge these gaps, we evaluated annual receipt of preventive care screenings among HMO-insured patients aged 50 years and older diagnosed with incident breast or colorectal cancer between 2000 and 2008. For comparison, we identified an age-, gender-, and distribution-matched sample of cancer-free controls receiving care from the same delivery systems. Of interest was the identification of evidence-based preventive care that survivors may be at risk of not receiving relative to cancer-free controls. We also evaluated whether the relationship between preventive care use and survivor/control status was modified by patient age and year of diagnosis. Of particular interest was whether similar relationships existed for those under age 65 as those aged 65 years and older.
Methods
Setting and patient selection
Survivors and cancer-free controls were identified from among insured patients receiving care from four non-profit integrated health systems: Group Health Cooperative, Health Alliance Plan/Henry Ford Health System, and Kaiser Permanente Colorado and Northwest. Each organization is a member of the Cancer Research Network (CRN), an initiative of the National Cancer Institute designed to conduct research on cancer prevention, early detection, treatment, long-term care, surveillance, and cancer communication as well as dissemination and implementation research [13].
Data available from these organizations’ tumor registries were used to identify cancer survivors aged 50 years and older who were diagnosed between January 1, 2000, and December 31, 2008, with non-metastatic breast or colorectal cancer. Eligible survivors were those treated with curative intent and continuously enrolled in the delivery system-affiliated health plan for the 1-year periods preceding and following the date of cancer diagnosis. Those without information on disease stage, with metastatic disease, or with a prior cancer diagnosis were excluded. Males were excluded from the breast cancer sample.
We used distribution matching on birth year, diagnosis year, and sex to over sample controls (5:1) from cancer-free study-eligible patients. Controls were randomly assigned to a diagnosis month to match the distribution of diagnosis months in the same stratum of survivors. Eligible controls had continuous health plan enrollment for 1 year preceding and following their randomly assigned diagnosis date.
Survivors and controls were followed for each 12-month period for which they contributed complete information following an “index date” defined by the date 3 months following diagnosis/matched diagnosis date. We elected to use a relatively short time period (i.e., 3 months) to minimize the likelihood of missing service receipt in the first year of follow-up and because our prior research has shown that results and conclusions were not sensitive to whether index dates of 3 or as long as 9 months were used [14, 15]. Observations were censored at the first of the month for deaths, health plan disenrollment, 5 years post-index dates, or end of follow-up (December 31, 2008). Using a previously developed algorithm [16], survivors were also censored at recurrence or diagnosis of a second primary cancer. Each survivor and cancer-free control therefore contributed between 1 and 5 years of observation. Institutional review boards at each participating organization approved all aspects of the study protocol.
Preventive care receipt and data sources
We assessed annual receipt of five preventive care services that are recommended by the US Preventive Services Task Force (USPSTF) [17]. For women, this included screening for (1) breast cancer via mammography if aged 50–74 years; (2) cervical cancer via Papanicolaou (Pap) testing if aged 50–65 years; (3) cardiovascular disease with a lipid profile if aged 50+ years; (4) osteoporosis via bone densitometry testing if aged 65+ years; and (5) colorectal cancer via colonoscopy, sigmoidoscopy, barium enema, or fecal occult blood test (FOBT) or fecal immunohistochemical test (FIT) if aged 50–74 years. For men, this included screening for (1) cardiovascular disease with a lipid profile if aged 50+ years and (2) colorectal cancer via colonoscopy, sigmoidoscopy, barium enema, or FOBT/FIT if aged 50–74 years. We evaluated annual service receipt, regardless of the recommended screening interval, because the recommended screening interval is quite long for some services (e.g., 10 years for colonoscopy) and not well specified for others (e.g., osteoporosis screening) [18]. In so doing, we are assuming service use is distributed uniformly across years of eligibility. Receipt of each service was considered among only those individuals who were age- and gender-eligible and for each complete patient-year of observation with two exceptions: we did not evaluate mammography use among breast cancer survivors or their controls, and we did not evaluate colorectal cancer screening use among colorectal cancer survivors or their controls because, for breast and colorectal cancer survivors, receipt of mammograms and colorectal cancer screening, respectively, would be considered surveillance for recurrence and not receipt of general preventive care [19].
Office visit use was evaluated via annual frequency of visits to primary care (including family medicine, general internal medicine, geriatrics, and gynecology), surgery, and, among survivors only, oncology. Information on visits and procedures were obtained from the Virtual Data Warehouse (VDW) maintained by the CRN. The VDW contains information derived from electronic medical records, health insurance claims, and other administrative data systems and is routinely used for research purposes [20]. Age at diagnosis and gender were also obtained from the VDW along with diagnostic codes from the 12 months preceding diagnosis/matching-diagnosis date. The latter were used to construct the Charlson Comorbidity Index as adapted for studying cancer patients [21]. The VDW also contains county-level ecological surrogates for median family income obtained from geo-coded information on patients’ residential street address and the US Census [22].
Statistical analysis
We calculated the proportion of survivors and controls receiving each service in each year following their index date. To account for repeated observations over time within patients, differences in care by survivor/cancer-free control status were evaluated using generalized estimating equations. Unadjusted and adjusted logistic regression models were estimated with the SAS procedure PROC GENMOD.
Adjusted models were estimated in three variations. First, for each preventive service, we fit models that, in addition to survivor/cancer-free control status, included patient age, gender, comorbidity score, neighborhood household income, and the number of years since diagnosis as well as fixed effects for health plan and the calendar year of diagnosis (model 1). Second, to this model, we added a variable reflective of the count of the number of primary care visits incurred during the year (model 2). For the final models (model 3), we used results from this latter model (i.e., model 2) to evaluate pairwise interactions between survivor/cancer-free control status and both age and calendar year of diagnosis. Models that included pairwise interactions were estimated only for those combinations for which both variables had significant (p < 0.05) main effects. Furthermore, pairwise interactions were maintained in these final models only if the overall test of statistical significance was significant (p < 0.05).
Results
Cancer survivors and non-cancer controls
On average, 3 years of continuous follow-up was available for survivors and cancer-free controls, resulting in 12,923 complete survivor-years and 100,851 complete control-years of observation for the breast sample, and 5103 complete survivor-years and 59,448 complete control-years of observation for the colorectal sample. The mean age at the time of diagnosis among the breast sample was 66.5 years, and among the colorectal cancer sample 71.5 years. Among the breast sample, 47 % were under the age of 65 compared to 27 % of the colorectal sample (Table 1).
Preventive care use
Regardless of year or cancer site, the proportion of survivors receiving each of the preventive care services was almost always higher than that among cancer-free controls (Table 2). Two exceptions were lipid profile testing (both breast and colorectal samples) and bone densitometry testing (colorectal sample only): breast and colorectal cancer survivors were less likely to receive lipid testing compared to controls (albeit by a relatively small amount) in all 5 years of follow-up, and colorectal cancer survivors were less likely to receive bone densitometry testing in some years relative to controls.
For both breast and colorectal cancer survivors, the proportion who incurred visits to oncology and surgery dropped dramatically between years 1 and 2 of follow-up (from 86.3 to 58.7 % and from 58.3 to 31.3 %, respectively, for oncology, and from 93.7 to 34.5 % and from 88.5 to 40.9 %, respectively, for surgery) and then continued to decrease steadily between the second and fifth years of follow-up (Table 3). A similar pattern was seen with the average number of annual visits to oncology and surgery among those with at least one visit. Despite these decreases, in the fifth year of follow-up, about one half of breast cancer survivors and one fifth of colorectal cancer survivors had at least one visit to oncology. On the other hand, both the proportion of survivors being seen in and the annual average number of visits to primary care remained relatively constant and always above that of cancer-free controls, across the 5 years of follow-up.
Relative to survivors, breast and colorectal cancer-free controls were significantly less likely to receive a Pap test and significantly more likely to receive cholesterol testing prior to controlling for other factors (Table 4). Similarly, relative to survivors, breast cancer-free controls were significantly less likely to use both colorectal cancer screening and bone densitometry testing. No difference was observed in receipt of bone densitometry or mammography testing by survivor/cancer-free control status among the colorectal cancer sample. Once patient factors were controlled, each of these associations still held (model 1, Table 4). We next added the number of annual primary care visits to each model (model 2, Table 4). That variable was statistically significant (p < 0.0001) in each model with associated odds ratios that ranged from 1.05 for bone densitometry testing among age-eligible females in both the breast and colorectal cancer samples to 2.01 for Pap testing among age-eligible females in the breast sample and 2.15 for Pap testing among age-eligible females in the colorectal sample (data not shown). Nonetheless, inclusion of that variable did not change either the statistical significance or the magnitude of the observed associations between survivor/cancer-free control status and preventive care use.
In the final set of models, we included a pairwise interaction between survivor/cancer-free control status and both age and year of diagnosis (as warranted by significant main effects). The only relationship between survivor/cancer-free control status and preventive service use that was modified by age was that for lipid profile testing among both the breast cancer and colorectal cancer samples. Furthermore, the only relationship between survivor/cancer-free control status and preventive service use that was modified by year of diagnosis was that for bone densitometry testing among the breast cancer sample. Results are available via online Appendix Tables A-1 and A-2.
Discussion
Using data from 2000 to 2008, we found HMO-insured breast and colorectal cancer survivors to be equally or more likely to receive recommended cancer screenings and bone densitometry testing when compared to age- and gender-matched cancer-free controls. On the other hand, we found both breast and colorectal cancer survivors to be less likely to receive cholesterol testing when compared to cancer-free controls. These differences existed regardless of patient age or year of diagnosis.
Most early- and mid-stage cancer survivors, especially those treated with curative intent, are expected to live for many years, and many will die from something else, often cardiovascular disease [2, 3]. It is important, therefore, that survivors receive not only recommended surveillance for recurrence but also the evidence-based preventive care services appropriate to their age and gender. On one hand, our findings reflect a glass half full: survivors, regardless of age, are generally more likely than their counterparts without a cancer diagnosis to receive routine screening for other cancers. On the other hand, our findings illustrate how even relatively simple, non-cancer-related health care needs, such as routine cholesterol testing, may be overlooked among survivors—even among those survivors being seen in the primary care clinics within integrated health systems known for their delivery of relatively high quality primary care [23]. Findings from prior studies among Medicare enrollees—where stage of disease at diagnosis is less likely to be localized [24]—point to similar challenges in caring for the chronic care needs of cancer survivors [9]. Overcoming the shortcomings in non-cancer-related preventive and chronic care delivery is critical to ensuring the well-being and longevity of those whose cancer has been successfully treated.
Patterns of high and low preventive screening use among breast and colorectal cancer survivors relative to cancer-free controls identified here existed even after controlling for primary care visit use. Given prior findings of associations between primary care visit use and receipt of preventive care [25–28], we expected the relationship between cancer survivor/cancer-free control status and preventive care use to be attenuated when primary care visit use was controlled. Instead, we found no change in the relationships. This implies that the use of preventive care among cancer survivors is influenced by more than realized access to primary care. Certainly, the oncologists or other specialists survivors are seeing, especially in the initial years following a diagnosis, could be a driving factor behind the relatively higher use of cancer screening services. Speculating the reasons behind the relatively lesser use of cholesterol testing is not as obvious. Perhaps the focus of visits to primary care made by cancer survivors is dominated by cancer-related needs, or perhaps cancer survivors are relatively less adherent to a primary care physician’s recommendation for routine cholesterol testing.
Similar to prior studies [10, 29], we found that the proportion of survivors with visits to an oncologist and surgeon decreased with each passing year following diagnosis. Nonetheless, 5 years following their treatment completion, almost half of breast cancer survivors and just over a fifth of colorectal cancer survivors were still being seen in oncology. On the other hand, and also similar to previous findings [8], we found insured cancer survivors to have consistent access to primary care: over 80 % of survivors were seen in primary care in each the five follow-up years. Although the seemingly large proportions of survivors being seen by oncologists (and surgeons) are likely consistent with patient preferences [30], whether this pattern of utilization is sustainable as the population of cancer survivors grows is unclear, nor is it well understood what services—preventive or otherwise—are being delivered during these visits. What is increasingly understood, however, is that the health care and other needs of cancer survivors are routinely not being met despite such relatively high use of ambulatory care visits [31].
To our knowledge, this is the first study not relying on self-reported use that has included a cancer survivor population under the age of 65. We had a large, geographically diverse population that spanned multiple years. Our primary data source was the electronic health record systems of the participating health plans, and we were able to control for realized access to primary care.
Our results, however, should be considered in light of a number of limitations. The use of automated encounter and claims data precluded knowledge of care indication as well as of patient preferences and of other psychosocial factors that may influence preventive care use. As such, some services may not have been received for screening but for other indications (e.g., diagnosis), and it may have been some patients’ choice not to receive preventive care. Furthermore, we were not able to identify a specific date for treatment completion. Although we have previously found that results and conclusions regarding service receipt are not sensitive to altering this window of observation [19], for cancer survivors, the first year of observation may include some time in which the patient was still undergoing active cancer treatment. Furthermore, because we evaluated annual preventive health service receipt (and not receipt within guideline-recommended intervals), we cannot draw conclusions regarding the appropriateness of observed use—only the relative differences in use over time and between cancer survivors and their cancer-free controls. It is also worth noting that previous studies have found results sensitive to the selection process used to identify cancer-free controls [11, 12]. As observations were limited to those insured and receiving care from four integrated health systems, care should be taken when generalizing to other settings and populations.
Our findings highlight the successes and challenges in delivering evidence-based routine preventive care to breast and colorectal cancer survivors. In the first 5 years following treatment, cancer survivors are equally or more likely to receive cancer screening tests and bone densitometry testing compared to cancer-free controls. Yet, regardless of their age and despite heavy use of ambulatory visits, including visits to primary care, cancer survivors relative to non-cancer controls receive cholesterol testing less often than cancer-free controls, particularly those survivors under the age of 65 years. While the health implications of these relative differences in service use warrant additional attention, our findings, combined with those of others, highlight the need to consider the full complement of health needs that exist among cancer survivors.
References
National, Cancer, and Institute. Survivorship-related statistics and graphs. 2013 [cited 2013 May 2, 2013]; Available from: http://dccps.nci.nih.gov/ocs/prevalence/.
Schonberg MA et al. Causes of death and relative survival of older women after a breast cancer diagnosis. J Clin Oncol. 2011;29(12):1570–7.
Mandel JS et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. N Engl J Med. 1993;328(19):1365–71.
Duffy CM, Clark MA, Allsworth JE. Health maintenance and screening in breast cancer survivors in the United States. Cancer Detect Prev. 2006;30(1):52–7.
Bellizzi KM et al. Health behaviors of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol. 2005;23(34):8884–93.
Trask PC et al. Cancer screening practices among cancer survivors. Am J Prev Med. 2005;28(4):351–6.
Findley PA, Sambamoorthi U. Preventive health services and lifestyle practices in cancer survivors: a population health investigation. J Cancer Surviv. 2009;3(1):43–58.
Yabroff KR, Machlin SPS, et al. Access to preventive health care for cancer survivors. Am J Prev Med. 2013;45(3):304–12.
Earle CC, Neville BA. Under use of necessary care among cancer survivors. Cancer. 2004;101(8):1712–9.
Earle CC et al. Quality of non-breast cancer health maintenance among elderly breast cancer survivors. J Clin Oncol. 2003;21(8):1447–51.
Snyder CF et al. Comparing care for breast cancer survivors to non-cancer controls: a five-year longitudinal study. J Gen Intern Med. 2009;24(4):469–74.
Snyder CF et al. Prevention, screening, and surveillance care for breast cancer survivors compared with controls: changes from 1998 to 2002. J Clin Oncol. 2009;27(7):1054–61.
The HMO SCR: Cancer Research Network. [cited 2013 May 5, 2013]; Available from: http://crn.cancer.gov/.
Cooper GS et al. The utility of administrative data for measuring adherence to cancer surveillance care guidelines. Med Care. 2007;45(1):66–72.
Elston Lafata J et al. Routine surveillance care after cancer treatment with curative intent. Med Care. 2005;43(6):592–9.
Lamont EB et al. Measuring disease-free survival and cancer relapse using Medicare claims from CALGB breast cancer trial participants (companion to 9344). J Natl Cancer Inst. 2006;98(18):1335–8.
U.S. Preventive Services Task Force. [cited 2013 May 6, 2013]; Available from: (http://www.uspreventiveservicestaskforce.org/).
Screening for osteoporosis: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med, 2011. 154(5): p. 356–64.
Salloum RG et al. Adherence to surveillance care guidelines after breast and colorectal cancer treatment with curative intent. Cancer. 2012;118(22):5644–51.
Hornbrook MC et al. Building a virtual cancer research organization. J Natl Cancer Inst Monogr. 2005;35:12–25.
Klabunde CN et al. A refined comorbidity measurement algorithm for claims-based studies of breast, prostate, colorectal, and lung cancer patients. Ann Epidemiol. 2007;17(8):584–90.
US, Census, and Bureau. Small area income and poverty estimates. State and county estimates for 2000 [cited 2013 May 6, 2013]; Available from: http://www.census.gov/did/www/saipe/data/statecounty/data/2000.html.
Health insurance rankings: how does your plan compare? 2012 [cited 2013 6/13/2013]; Available from: http://www.consumerreports.org/cro/magazine/2012/11/health-insurance-rankings/index.htm.
Fishman PA et al. The challenge of conducting comparative effectiveness research in cancer: the impact of a fragmented U.S. health-care system. J Natl Cancer Inst Monogr. 2013;2013(46):99–105.
Fenton JJ et al. Influence of primary care use on population delivery of colorectal cancer screening. Cancer Epidemiol Biomarkers Prev. 2009;18(2):640–5.
Zimmerman RK et al. Predictors of colorectal cancer screening in diverse primary care practices. BMC Health Serv Res. 2006;6:116.
Shires DA et al. Colorectal cancer screening use among insured primary care patients. Am J Manage Care. 2011;17(7):480–8.
McCarthy BD et al. Screening mammography use: the importance of a population perspective. Am J Prev Med. 1996;12(2):91–5.
Snyder CF et al. Preventive care for colorectal cancer survivors: a 5-year longitudinal study. J Clin Oncol. 2008;26(7):1073–9.
Hudson SV et al. Adult cancer survivors discuss follow-up in primary care: ‘not what i want, but maybe what i need’. Ann Fam Med. 2012;10(5):418–27.
Institute of Medicine, N.R.C.o.t.N.A., From cancer patient to cancer survivor: lost in transition. 2006: Washington DC.
Conflict of interest
The authors have no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lafata, J.E., Salloum, R.G., Fishman, P.A. et al. Preventive care receipt and office visit use among breast and colorectal cancer survivors relative to age- and gender-matched cancer-free controls. J Cancer Surviv 9, 201–207 (2015). https://doi.org/10.1007/s11764-014-0401-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-014-0401-3