Abstract
Background
Cancer survivors need high-quality follow-up care that addresses long-term problems related to cancer and their treatment. With growing numbers of cancer patients transitioning from oncological treatment to survivorship care, primary care physicians (PCPs) will play a major role in the delivery of survivorship care.
Objective
This pilot study was undertaken to provide initial insights into internal medicine (IM) and family medicine (FM) residents’ educational experience, training, and preparedness for practice as healthcare providers of adult cancer survivors (ACS).
Design
This study utilizes an anonymous cross-sectional, electronic survey of a sample of US IM and FM residents.
Participants
A total of 77 residents in their PGY-3 year of training responded to the survey, including 53 IM (69 %) and 24 FM (31 %) residents.
Results
The majority (97 %) of respondents performed as PCPs for ACS during their training, and 81 % expected to take care of such patients in the future. However, only a minority reported feeling very comfortable in this role or very confident of identifying cancer recurrence and potential long-term effects of cancer treatment (13 %, 21 %, and 15 %, respectively). Formal education in survivorship care was reported by 27 % of residents and was modestly associated with knowledge responses. High clinical exposure (defined as having ≥10 opportunities to perform as the PCP for ACS) was significantly associated with self-reported knowledge, comfort level, and self-confidence in being able to evaluate and manage potential long-term effects of cancer treatment and their symptoms.
Conclusions
Our results suggest there is a substantial disconnect between resident’s educational experience, training, and self-reported preparedness for practice in cancer survivorship in both IM and FM training specialties.
Implications for Cancer Survivors
Inadequate training in cancer survivorship represents a barrier to providing adequate cancer follow-up. Inexperience or unawareness of essential survivorship issues could lead to mistakes which affect survivors’ health and timely assessment of long-term cancer-associated morbidity. As PCPs will play a key role in the delivery of survivorship care, effective educational opportunities and achievement of competencies in adult cancer survivorship care by primary care trainees are needed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In 2012, 13.7 million cancer survivors in the USA represented approximately 4 % of the total US population [1, 2], and it is expected that the population of cancer survivors will reach almost 18 million by 2022 because of the rising incidence of cancer and improving survival rates for most types of cancer [3, 4]. Unfortunately, once patients survive their cancer, they continue to be at risk for a unique set of physical and mental problems that can negatively impact their quality of life and subsequent health care needs [5–9]. Acknowledging this, in 2006, the Institute of Medicine published a detailed report on cancer survivorship which recommends comprehensive follow-up care for all cancer survivors, including the prevention and early detection of secondary malignancies, as well as identification of changes in health status related to physical and psychosocial problems that might develop years after completion of treatment [10].
Due to the projected shortage of oncologists [11, 12], it is expected that more cancer survivors will shift to their primary care physicians (PCPs) for long-term survivorship care. Prior research has shown that PCPs are willing to assume exclusive responsibility for routine follow-up care after completion of active cancer treatment, if they are provided with relevant information from their oncologist colleagues in the form of survivorship care plans [13–15]. However, PCPs may feel unprepared or uncomfortable in this role and have reported being unfamiliar with current survivorship care guidelines, perceiving they lack sufficient knowledge and confidence to assume responsibility for survivors’ cancer-related needs [15–19].
Inadequate training in cancer survivorship represents a barrier to providing adequate cancer follow-up. Lack of knowledge and understanding about survivorship issues may significantly interfere with the physicians’ ability to effectively assess and treat the myriad of physical and emotional issues cancer survivors may face in the future, as well as their capacity to provide counseling on long-term cancer-associated morbidity.
In the current literature, several studies have addressed the concerns and opinions of oncologists, PCPs, and patients regarding cancer survivors’ long-term care. Nonetheless, to the best of our knowledge, there is almost no information regarding PCPs’ academic preparation and preparedness to practice as health care providers for cancer survivors. The present study was conducted to provide initial insights about internal medicine (IM) and family medicine (FM) residents’ educational experience as PCPs for adult cancer survivors (ACS), their training in this area, and self-reported preparedness and expectations for practice in this role.
Methods
Sample
Our goal for this study was to capture a representative sample of US IM and FM residents’ perceptions about this topic. There is no published information regarding the number of programs that provide training in survivorship care for primary care medicine programs, nor are there studies examining residents’ perceptions about these issues. We invited residents who were in their last year of training (PGY-3) at the end of the academic year, in hopes of obtaining the most reliable information about residents’ educational experiences in adult cancer survivorship. As this was a pilot study, we aimed to obtain 100 responses from a representative sample of US resident physicians. To do this, we first downloaded a list of the AAMC-affiliated medical schools (which was posted on the AAMC website in February 2013), and then stratified the list by AAMC region (Southern, Central, Northeast, and Western). We then randomized the list of schools within region and initially selected the first two schools from each region, with the expectation that a 30 % response rate would result in our target of 100 responses. We contacted a residency program representative in each of these initial eight IM and eight FM programs (Program Director or Coordinator) and asked them about their willingness to share the survey invitation with their PGY-3 residents. If a school declined to participate, we sequentially proceeded down the randomized list of schools to invite the next school on the list (e.g., two of the initial 16 programs declined due to concerns about resident survey burden, and two others were nonresponsive to emails or phone calls). After approximately 15 days of tracking survey responses (n = 24), it became clear this strategy would not likely result in our initial goal of 100 respondents. We then modified our IRB protocol and sent e-mail invitations directly to eligible residents themselves. We did this by using the randomized list of schools to contact residents via e-mail if their emails accounts were available on their program’s website. If their e-mail addresses were not available, the e-mail invitation was sent to the program director or program coordinator asking them to forward it to their PGY-3 residents. In total, 71 programs from the randomized list of schools were contacted, but we were unable to track whether emails were forwarded along to residents by program directors/coordinators. A total of 77 residents in their PGY-3 year of training responded to the survey, including 53 IM (68 %) and 24 FM (32 %) residents.
Instrument
A brief 13-item survey was developed after reviewing the literature relevant for PCP surveys in survivorship care and physician residents’ surveys regarding their preparedness for practice [15–20]. Because all areas of interest for our study were not covered in existing questionnaires, additional questions were created. The questionnaire assessed participant’s experience, training received, and self-reported knowledge and preparedness for practice as PCPs for ACS. Core survey items to assess resident physicians’ knowledge and their preparedness for practice (measured as comfort and confidence performing as PCPs for ACS) contained Likert-type scale response options. In the survey invitation for this study, we defined ACS as a patient with a history of cancer not undergoing active oncological treatment and 18 years of age or older. The instrument was pretested with PGY-3 IM and FM residents (n = 11) at the authors’ home institution, and no edits to the items were needed after pretesting.
Procedures
The study was conducted from mid-March 2013 to June 30, 2013. All survey responses were anonymous, and no institutionally identifying information was collected. No incentives were provided for participation in the survey. The study and subsequent protocol modification were reviewed and approved by the University of Arkansas for Medical Sciences’ Institutional Review Board.
Statistical analysis
Descriptive statistics were calculated using SPSS software. Variations in responses by specialty (FM vs. IM) and by level of clinical exposure (dichotomized into high vs. low; ≥10 versus <10 opportunities to act as PCP for ACS) were explored using parametric statistics for continuously scaled items (t tests for independent samples) and nonparametric techniques (chi-square analyses) for categorically scaled response items. Spearman correlations were computed to assess relationships between items (e.g., knowledge and education). Because no statistical differences were found between IM and FM residents’ responses to survey items for comfort, confidence, and formal training (detailed results not reported herein, but available if desired), all of the following results present analyses combining both specialties.
Results
Residents’ experience and training as primary care providers for ACS
As shown in Table 1, a total of 97 % of the residents reported having the opportunity to act as the primary care provider for adult cancer survivors during their training. The majority (81 %) reported experiencing these encounters in their continuity care clinic. High clinical exposure was reported by 57 % residents. Formal education in adult cancer survivorship care was reported by 27 % of the respondents, most (90 %) were in the form of some type of didactic delivery method.
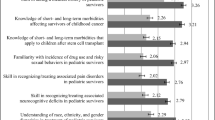
Resident’s preparedness for practice as primary care providers for ACS
As shown in Table 2, the vast majority of residents (81 %) expected to take care of adult cancer survivors in the future. However, only 13 % of respondents reported feeling very comfortable as PCPs of these patients. Assessment of self-reported competencies indicated that few residents (21 %) felt very confident in their ability to identify symptoms that may be a sign of cancer recurrence, 15 % felt very confident in their ability to evaluating and managing potential long-term effects of cancer treatment, and 5 % felt very knowledgeable in long-term follow-up care (when to schedule follow-up visits, tests, and cancer screening in ACS).
Experience in acting as the PCP for ACS was significantly associated with knowledge (χ 2 = 8.18, df = 3, p = 0.04), self-reported comfort level (χ 2 = 5.87, df = 2, p = 0.05), and with one’s clinical self-confidence in being able to evaluate and manage potential long-term effects of cancer treatment and their symptoms, e.g., chronic pain, emotional distress, lymphedema, etc (χ 2 = 7.22, df = 2, p = 0.03); but not for confidence in identifying symptoms or signs of cancer recurrence (χ 2 = 4.05, df = 2, p = 0.13). However, formal education about caring for ACS patients was only modestly associated with the survey item that assessed knowledge (Spearman r = 0.19, p = 0.047) and was not statistically associated with items assessing one’s comfort level in providing primary care for adult cancer survivors (r = 0.15, p = 0.10); nor with one’s clinical self-confidence to identify symptoms that may be a sign of cancer recurrence (r = 0.08, p = 0.23) or their confidence in being able to evaluate and manage potential long-term effects of cancer treatment and their symptoms (r = 0.16, p = 0.08).
Discussion
Due to improvement in cancer diagnosis and treatment, cancer has become a chronic disease and it is expected that approximately 1 of every 30 Americans will become a cancer survivor during their lifetime [21]. As PCPs will take care of a growing number of cancer survivors, actions to ensure they are ready for this task should be implemented.
Results of this pilot study provide initial insights about IM and FM residents’ experience as PCPs for ACSs, training, levels of preparedness, and expectations for practice as healthcare providers of this population. We found that most of the surveyed residents had provided care for adult cancer survivors in primary care continuity clinic settings, which is not surprising given the increasing population of cancer survivors. Most residents also expected to take care of adult cancer survivors after completing their residency training, but only a minority of respondents felt prepared and knowledgeable in providing adult survivorship care. These results are in accordance with previous studies reporting that most PCPs did not feel confident in their knowledge of testing for recurrence [20], were not familiar with current surveillance guidelines [15], felt inadequately trained in survivorship care, and were prone to order excessive tests/treatments as malpractice protection [22].
Similar to previous studies of residents in other areas of medicine [23, 24], our results indicated that clinical exposure was positively associated with self-reported preparedness for practice (for two of the three items assessing comfort and confidence in treating long-term effects of cancer and its treatment). However, there might be some hidden challenges inherent in caring for survivors (e.g., high anxiety on the part of the both patient and provider regarding the possibility of recurrence; the need for both parties to “hold” this anxiety together in a productive way without ordering an undue number of tests, etc.) which requires much more than simple exposure to patients. The educational gap in cancer survivorship care for primary care trainees represents an important threat to the delivery of high quality of care for cancer survivors. Inexperience or unawareness of essential survivorship issues could lead to mistakes which affect patients’ health and timely assessment of long-term cancer-associated morbidity. This may explain why clinical exposure was not associated with confidence in identifying cancer recurrence in our resident sample. We also suspect that either a lack of or inadequate training in cancer survivorship care might explain the low levels of confidence in providing adult survivorship care in primary care trainees in comparison to their confidence levels in caring for patients with other chronic disease, such as DM and HTN (confidence levels ranging between 80 and 94 %) [23]. The low levels of self-reported preparedness and knowledge in survivorship care found in our study might be just a reflection of lack of familiarity with fundamental survivorship concepts, as the majority of residents reported little or no formal training in cancer survivorship during residency training. Our findings are consistent with prior reports where senior medical students and oncology fellows were found to have poor knowledge in basic cancer survivorship terminology and in long-term treatment consequences [25], and with research showing PCPs have limited awareness of long-term effects of chemotherapy used in the treatment of high prevalent malignancies like breast and colon cancers [19].
In this study, residents’ reports of formal education in survivorship care was only modestly associated with knowledge, and was not statistically associated with ones’ confidence or comfort level. This lack of association between education and preparedness is not surprising given that only 27 % of residents reported formal education in this area. Nonetheless, this relationship highlights the need to consider how best to provide high-quality educational opportunities in ACS care for PC trainees. We believe the educational gap for cancer survivorship care could be improved if there were more standardized cancer survivorship training in medical school curricula and postgraduate training. Cancer education curricula likely need to include exploration of these themes, with opportunities for self-reflection and development of mindful practice. As reported in this study, education in ACS was primarily didactic (81 %); it is possible there is room for improvement in the way cancer survivorship is taught, to ensure practical, interactive, relevant survivorship learning experiences founded on practice-based learning and systems-based assessment through group projects and review of their own patient outcomes. Furthermore, since objective assessment of competency is known to be a major driver of learning, survivorship curricula should incorporate relevant measures of competency achievement either by observing the resident in direct patient encounters or via high-fidelity simulations, in order to stimulate the process of learning itself. Nonetheless, initiatives to begin addressing these educational needs have been published. For example, Uijtdehaage et al. [26] describe a portable framework for a cancer survivorship curriculum that was successfully implemented at their medical school level and that resulted in improvement in both knowledge in survivorship issues and self-reported comfort in patient care activities. Also, Shayne et al. [27] presented a workshop to improve cancer survivorship education into the curriculum of a hemato-oncology and radiation oncology fellowship. Their six-session workshop showed statistically significant improvement in provider’s comfort discussing survivorship issues with patients, their knowledge in this area, and their confidence in their ability to explain a survivorship care plan to patients. These initiatives are encouraging and have the potential to eventually improve the overall quality of care delivered to cancer survivors.
Our study has several limitations which should be acknowledged. First, this was a small pilot study, which limits our ability to draw definitive conclusions regarding the observed frequencies and relationships between variables examined in the study. Although we believe the sample provides a representative snapshot of US FM and IM resident physicians at the time of completing their training, our study results have limited generalizability in that the survey was sent only to US medical schools that have both FM and IM residency programs. Despite these limitations, we have few reasons to believe that resident physicians in other FM and IM programs in the USA would report a different profile of survey responses, but we did not collect demographic data that would allow us to definitively state such an assertion. Likewise, it would have been helpful to collect data on residents’ personal exposure to/experience of cancer as certain learner characteristics—in particular a personal history of cancer—may impact knowledge regarding survivorship care [28]. Similarly, it is possible that residents who are more experienced or interested in cancer survivorship responded to the survey than those who are less interested or experienced, in which case the survey results probably reflect an overestimate in all areas measured compared to the average resident sample. Another limitation of this study is the reliance on self-reported data based on residents’ perceptions of their preparedness. It is possible that residents’ low levels of comfort and confidence in providing survivorship care are an underestimation of their competencies, as trainees may underrate themselves compared with the ratings of their supervisors [29, 30]. Nonetheless, we consider these levels with respect to survivorship care to be substantially lower than those experienced with respect to care of patients with other chronic conditions (e.g., hypertension or diabetes) [23], though we cannot assure this statement as the survey did not include comparison items.
Also, we encountered methodological challenges in obtaining an adequate number of responses with our initial sampling plan which would have allowed for calculating response rates. In balancing the need to quickly obtain responses before residents graduated in June, we resorted to a strategy that would increase response rates, but with concurrent loss of the ability to estimate true survey response rates. To improve responses in future studies of residents, it may be useful to provide lottery-based incentives, or to partner with existing board-related associations who have the information and ability to capture a more representative national sample of residents. Similarly, we were unable to address any concerns about potential nonresponse bias, due to the anonymous nature of the survey and the minimal collection of demographic and institutional data.
Conclusions
In summary, our results suggest there is a substantial disconnect between academic preparation, self-reported preparedness, and expectations for practice as healthcare providers of ACS among trainees of both training specialties. These findings provide potentially important information regarding a need to establish effective formal educational opportunities and achievement of basic competencies in adult cancer survivorship care by internal medicine and family medicine residents. Although calls for improving education in cancer survivorship have been published since the 2006 IOM “lost in transition” report, further efforts to address this gap are clearly needed.
References
U.S. Department of Commerce, Census Bureau. State and county quick facts. Available at: http://quickfacts.census.gov/qfd/states/00000.html.
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29.
Altekruse SF, Kosary CL, Krapcho M, et al. Surveillance, epidemiology, and end results cancer statistics review, 1975-2007. Bethesda, MD: National Cancer Institute; 2010.
Siegel R, Desantis C, Virgo K, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62:220–41.
Hewitt M, Rowland JH. Mental health service use among adult cancer survivors: Analyses of the national health interview survey. J Clin Oncol. 2002;20:4581–90.
Gotay CC, Muraoka MY. Quality of life in long-term survivors of adult-onset cancers. J Natl Cancer Inst. 1998;90:656–67.
Ganz PA. Late effects of cancer and its treatment. Semin Oncol Nursing. 2001;17:241–8.
Macmillan Cancer Support: It’s no life: study of the health and wellbeing of cancer survivors—follow up survey of awareness of late effects and use of health services for ongoing health problems. Available at http://www.macmillan.org.uk/Documents/GetInvolved/Campaigns/Campaigns/itsnolife.pdf.
Carver JR, Shapiro CL, Ng A, et al. American Society of Clinical Oncology clinical evidence review on the ongoing care of adult cancer survivors: Cardiac and pulmonary late effects. J Clin Oncol. 2007;25:3991–4008.
Hewitt M, Greenfield S, Stovall E. eds., IOM, NRC. From cancer patient to cancer survivor: lost in transition. Washington, DC: National Academies Press; 2006.
Hortobagyi GN. A shortage of oncologists? The American Society of Clinical Oncology workforce study. J Clin Oncol. 2007;25:1468–9.
Kirkwood MK, Kosty MP, Bajorin DF, et al. Tracking the workforce: the American Society of Clinical Oncology workforce information system. J Oncol Pract. 2013;9:3–8.
Grunfeld E, Mant D, Vessey MP, et al. Specialist and general practice views on routine follow-up of breast cancer patients in general practice. Fam Pract. 1995;12:60–5.
Del Giudice ME, Grunfeld E, Harvey BJ, et al. Primary care physicians’views of routine follow up care of cancer survivors. J Clin Oncol. 2009;27:3338–45.
Suh E, Daugherty CK, Wroblewski K, et al. General internists’ preferences and knowledge about the care of adult survivors of childhood cancer. A cross-sectional survey. Ann Intern Med. 2014;160:11–7.
Nissen MJ, Beran MS, Lee MW, et al. Views of primary care providers on follow-up of cancer patients. Fam Med. 2007;39:477–82.
Salz T, Oeffinger KC, Lewis PR, et al. Primary care providers’ needs and preferences for information about colorectal cancer survivorship care. J Am Board Fam Med. 2012;25:635–51.
Bober SL, Recklitis CJ, Campbell EG, et al. Caring for cancer survivors: a survey of primary care physicians. Cancer. 2009;115(18 suppl):4409–18.
Nekhlyudov L, Aziz NM, Lerro C, Virgo KS. Oncologists’ and primary care physicians’ awareness of late and long-term effects of chemotherapy: implications for care of the growing population of survivors. J Oncol Pract. 2013. Published online before print November 12, 2013, doi: 10.1200/JOP.2013.001121.
Potosky AL, Han PKJ, Rowland J, et al. Difference between primary care physicians’ and oncologists’ knowledge, attitudes and practices regarding the care of cancer survivors. J Gen Intern Med. 2011;26(12):1403–10.
Hong S, Nekhlyudov L, Didwania A, et al. Cancer survivorship care: exploring the role of the general internist. J Gen Intern Med. 2009;24 Suppl 2:S495–500.
Virgo KS, Lerro CC, Klabunde CN, et al. Barriers to breast and colorectal cancer survivorship care: perceptions of primary care physicians and medical oncologists in the United States. J Clin Oncol. 2013;31:2322–36.
Wiest FC, Ferris TG, Gokhale M, et al. Preparedness of internal medicine and family practice residents for treating common conditions. JAMA. 2002;288:2609–14.
Van der Leeuw RM, Lombarts KM, Arah OA, Heineman MJ. A systematic review of the effects of residency training on patient outcomes. BMC Med. 2012;10(1):65.
Uijtdehaage S, Hauer KE, Stuber M, et al. Preparedness for caring of cancer survivors: a multi-institutional study of medical students and oncology fellows. J Cancer Educ. 2009;24(1):28–32.
Uijtdehaage S, Hauer KE, Stuber M, et al. A framework for developing, implementing, and evaluating a cancer survivorship curriculum for medical students. J Gen Intern Med. 2009;24 Suppl 2:S491–4.
Shayne M, Culakova E, Milano MT, et al. The integration of cancer survivorship training in the curriculum of hematology/oncology fellows and radiation oncology residents. J Cancer Survivorship. 2013. Epub ahead of print. 2013 Dec 05. PMID: 24307557.
Kowalkowski MA, Hart SL, Du XL, Baraniuk S, Latini DM. Cancer perceptions: implications from the 2007 Health Information National Trends Survey. J Cancer Surviv. 2012;6:287–95.
Fincher RM, Lewis LA, Kuske TT. Relationships of interns’ performances to their self-assessments of their preparedness for internship and to their academic performances in medical school. Acad Med. 1993;68(2 suppl):S47–50.
Zonia SC, Stommel M. Interns’ self-evaluations compared with their faculty’s evaluations. Acad Med. 2000;75:742.
Conflict of interest
The author(s) indicated no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Susanibar, S., Thrush, C.R., Khatri, N. et al. Cancer survivorship training: a pilot study examining the educational gap in primary care medicine residency programs. J Cancer Surviv 8, 565–570 (2014). https://doi.org/10.1007/s11764-014-0366-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-014-0366-2