Abstract
Purpose
The objective of this study is to describe a method for estimating the number of cancer survivors requiring different types of cancer care in the future.
Methods
Colon cancer data (1972–2007) from the New South Wales (NSW) Central Cancer Registry were used to estimate prevalence in 2008–2017, which was then divided into five phases of care (initial, post-treatment monitoring, treatment for recurrence and second colon cancer, long-term survivors and last year of life). Patterns of care study data were used to calculate the type and number of treatments required by patients in initial care.
Results
There were 17,375 patients living in NSW who had a past diagnosis of first primary colon cancer in 2007. Our statistical model suggests that by 2017, this number will have increased to 22,671. At least 2,430 patients are expected to require initial surgery for colon cancer in 2017, and of these, 753 will also require adjuvant chemotherapy. Furthermore, an additional 538 cases will require therapy due to cancer recurrence (307) or a second primary colon cancer (231).
Conclusion
Our proposed method provides more complete estimates of future cancer care needs. With some modifications, this method can be used to estimate the future prevalence of many major cancer types in many other jurisdictions.
Implications for Cancer Survivors
Our proposed method can be a useful tool for planning future cancer care with the goal of improving the cancer survivorship experience for survivors, their caregivers and their families.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cancer is an increasing burden for all populations worldwide, accounting for over 2.75 million deaths in developed countries in 2008 [1]. The burden of cancer is generally measured in terms of incidence (newly diagnosed cases) and death (mortality) rates. These cancer statistics can be used to plan health service needs for the care required immediately following a cancer diagnosis or for end of life and palliative care services, but do not provide information for the period following primary treatment, until cancer recurrence or before the end of life. Cancer prevalence (the number of people living in a community on a certain date who have had a diagnosis of cancer) is a more complete measure of the burden of a particular cancer in the population, so it is more useful for planning healthcare resource allocation.
Total prevalence is a crucial but crude measure of health service needs for cancer patients, as it covers all stages and levels of cancer care. This means that measures of total cancer prevalence will include people with a huge range of health service requirements, from recently diagnosed patients requiring initial treatment to people who require extensive care and have severe disabilities or long-term survivors who need only minimal care. Therefore, in terms of providing a meaningful and useful measure to inform health care planning, there would seem to be a great benefit in providing estimates of cancer prevalence for groups of patients based on the level of care they require. Population-based studies identifying these different groups and planning for their health care needs, however, are relatively rare. In 2006, Mariotto et al. [2] described a method to obtain such estimates, dividing the total prevalence into the following three different phases: initial care, monitoring and last year of life. However, as the authors acknowledged themselves, cases in the monitoring phase are a highly heterogeneous group in terms of health care needs [2] because they include patients who recently completed their initial therapy and require close follow-up, patients requiring treatment for cancer recurrence or second primary cancers, and those who have survived for a long period of time since their initial treatment and can be considered to be cured. It is particularly important to include recurrent cases and people with second primary tumours when estimating health care needs for cancer patients [3, 4], as a significant number of cancer patients will develop a second primary cancer [5] or tumour recurrence [6–8] and will therefore require much more intensive medical care than the monitoring required for long-term cancer survivors. Thus, Mariotto’s approach may be extended by dividing the continued monitoring phase further, so that patients in each phase of care will be more homogeneous in terms of predicting health care needs [3], an important area for additional research [9].
The aim of this study was to describe a new method for estimating cancer prevalence by phase of care and predicting health care needs for these prevalent cancer patients. Data on primary colon cancer from an Australian population-based cancer registry was used to illustrate the method. To estimate health service demands for those prevalent patients, we applied the proportions of patients requiring different types of treatment derived from a population-based pattern of care study in the same population to the projected prevalence.
Methods
Overview
There were three principal activities involved in this study as follows: estimation and projection of the prevalence of colon cancer (2008–2017), phase of care analysis and estimation of the type and number of services required in 2017. Briefly, we first estimated the prevalence of colon cancer in 1972–2007 and projected the future prevalence for 2008–2017. These prevalence estimates were calculated using the prevalence and incidence analysis model (PIAMOD) software, with the primary data input being colon cancer (ICD-O3 C18) [10] incidence for cases diagnosed in 1972–2007 in New South Wales (NSW). Second, we divided the estimate of the total prevalence in 2007, which was obtained in the first step, into five phases of care using data on time since diagnosis, disease stage at diagnosis and cause of death, as well as data for recurrence and second colon cancer. We then applied the resulting proportions in each phase in 2007 to the projected prevalence estimates for 2017 (also from the first step of the analysis) to obtain future phases of care prevalence. Third, we estimated the type and number of services that will be required for the initial treatment of colon cancer in 2017. Data from a population-based pattern of care study for colorectal cancer in 2000–2001 [11] in NSW were used to obtain the proportion of patients undergoing different initial cancer treatments, and then these proportions were applied to the projected estimates of initial care in 2017.
This study was approved by the NSW Population and Health Service Research ethics committee (reference number: 2009/03/139).
Estimation and projection of the prevalence of colon cancer
Incidence data for first primary colon cancer diagnosed in 1972–2007 were extracted from the NSW Central Cancer Registry database. The registry covers a population of 7.2 million, approximately one-third of the national population of Australia, and maintains a record of all cases of cancer diagnosed in NSW residents since 1972. We included cases aged 18–84 years at diagnosis, and excluded cases who were reported to the Registry through death certificate only or who were first identified post-mortem. For survival analysis, vital status was obtained to the end of 2007 by matching the cancer registry records with death certificate records from the NSW Register of Births, Deaths and Marriages. Data for all causes of mortality for NSW by single year of age (up to 84 years old), sex and year (1972–2007), and corresponding NSW mid-year residential population data by single year of age, sex and calendar year were obtained from the Australian Bureau of Statistics.
PIAMOD software
The PIAMOD software [12] was used to estimate the observed prevalence (1972–2007) and project future prevalence (2008–2017). The method forecasts prevalence with a deterministic relationship among cancer mortality, incidence and survival at one time. The PIAMOD method was described in detail by Verdecchia et al. [12]. Basically, it estimates and projects cancer prevalence as a function of modelled incidence and survival estimates. The steps required for the application of PIAMOD are illustrated in Fig. 1.
To apply PIAMOD, we first prepared the following input files required: population data, all-causes mortality, cancer incidence and model-based survival estimates. Except for the survival estimates, data must be provided for single year of age (up to 84) and calendar year for males and females separately.
Incidence modelling
We fitted age-cohort models to the incidence data (1972–2007) in PIAMOD to project the incidence for 2008–2017. In these models, parameters were estimated from a regression equation using the observed incidence data, where the cohort linear term was left to drift, and the logit link function was used to restrain the model from assuming exponential growth. We then selected the best model in a stepwise procedure using the likelihood ratio test and a graphical comparison of the observed versus predicted incidence. Once the model was selected, we projected future incidence by fitting it to the observed incidence data (1972–2007), with the assumption that the age and cohort effects will be constant beyond the observed data (2008–2017) [12].
Survival modelling
Model-based survival estimates for input into PIAMOD were obtained from a SAS programme. Relative survival, the ratio of the observed proportion surviving in a group of cancer patients to the expected proportion that would have survived in an age- and sex-comparable group of people from the general population, was used in this analysis because we used all cause mortality from a population-based cancer registry. To obtain the model-based survival estimates, we first calculated relative survival using a standard method [13]. These relative survival estimates were grouped by five age groups (18–44, 45–54, 55–64, 65–74 and 75–84 years) and six periods of diagnosis (1972–1977, 1978–1983, 1984–1989, 1990–1995, 1996–2001 and 2002–2007). We then fitted mixture cure models [14] to these tabulated relative survival data and extrapolated survival for 2008–2017 based on the assumption that cancer survival trends will continue as previously observed. The models assume that the patients are a mixture of two groups with different prognostic prospects, specifically cured and fatal cases. For patients who are cured, the models assume that this group of patients will experience the same mortality risk as the general population. For fatal cases, the models assume that this group will die of cancer eventually, and that their survival time follows a Weibull distribution [14]. Finally, we selected the best model based on both goodness-of-fit and graphical assessment and fitted it to the tabulated survival data to obtain model-based estimates of survival for input into PIAMOD.
Prevalence modelling
Using the PIAMOD software and the prepared input data from the modelled incidence and survival estimates, as well as all-causes mortality and population data (which were assumed to be stable over time, but allowing for a growing and ageing population [12]), we were then able to calculate the prevalence of first primary colon cancer for 1972–2007 and to project future prevalence (2008–2017).
To evaluate the resulting PIAMOD estimates, we compared the PIAMOD prevalence estimates for 2007 (using data for 1972–2006) with 2007 prevalence estimates calculated using the direct counting method [15], which is considered to provide the most reliable estimates for populations covered by a cancer registry for a sufficient length of time [16].
Phase of care analyses
The total predicted prevalence for 2017 estimated by the PIAMOD model was divided into five phases of care namely, initial care, long-term survivors, post-treatment monitoring, treatment for recurrence and second colon cancer and last year of life. We divided the total prevalence for 2007 (for which we have data on time since diagnosis, disease stage at diagnosis and cause of death, as well as data for recurrence and second colon cancer) into these five phases of care, and then applied the resulting proportions in each phase to the projected estimates of total prevalence for 2017 to obtain future prevalence by phases of care. We assumed that for the next decade, the composition of prevalent cases by phases of care would remain similar to that in 2007 (the last year for which data were available to us).
The initial care phase was defined as the care provided in the first 12 months after diagnosis (excluding cases who died within the first year of diagnosis), and the last year of life phase was defined as the last 12 months of life for those who died of colon cancer. Cases with short survival (less than 12 months) were considered to be in the last year of life phase. We used information on cause of death to identify those patients who had died from colon cancer, and who we would therefore categorise as being in the ‘last year of life’ phase of care. The post-treatment monitoring phase was defined as the period between initial care and being considered a long-term survivor. Among those in the post-treatment monitoring phase, some are likely to require more treatment at some point during follow-up due to recurrence or development of a second colon cancer; thus, an additional phase of care was included to account for such cases.
Prevalence of long-term survivors
We defined the long-term survivors as patients with minimal excess risk of death (less than 1 %) compared to the general population. We obtained the time to reach this criterion stratified by disease stage from empirical life table estimates of relative survival. Using this definition, we estimated the proportion of long-term survivors amongst the prevalent colon cancer cases in 2007. Then, this proportion was applied to the projected prevalence estimates in 2017 to estimate the number of long-term survivors in the future.
Prevalence of patients requiring care for recurrence or second colon cancer
Colon cancer recurrences and second colon cancer that had occurred in the period of 2000–2007 were incorporated into the phase of care prevalence estimates, so that the future (2017) prevalence of such events and additional treatment required could be estimated.
The NSW Central Cancer Registry collects data on second and subsequent colon cancers (both multiple and primary tumours) and episode data (consisting of notifications sent after initial diagnosis). In the analysis, we combined multiple tumours (diagnosed within an interval greater than 2 months of each other) and multiple primary cancers (of the same site only) as one group (second colon cancer). Recurrence (or subsequent metastasis) was identified using episode data. Extent of the disease at initial diagnosis was based on evidence from statutory notification forms and pathology reports received by the registry within 120 days of first diagnosis, while cases with recurrent disease were based on episode data from 121 days onwards after first diagnosis. As many of the tumours being counted as multiple primaries may actually be recurrences, we combined the counts of second colon cancer and recurrent tumours. This is also logical in terms of health service planning; as in all these cases, further therapy is likely to be required.
Cases (1972–2007) with first primary colon cancer were followed up for recurrence or second colon cancer to the end of 2007. To increase the stability of the estimates for these events, the average annual number of cases for the period of 2000–2007 was used to estimate health care needs for this group of patients in 2007. We chose to use more recent (2000–2007) recurrence and second cancer data because the advances in the treatment of colon cancer that were developed during the 1990s have dramatically reduced the recurrence rates for colon cancer, and these new developments have been standard care in Australia since 2000, and thus these more recent data are more likely to accurately predict future patterns. To obtain the number of these events in the future, we first calculated the proportion of these events (average annual number in 2000–2007) over the number of cases in the post-treatment monitoring phase in 2007. We then applied this proportion to the number of projected cases in the post-treatment monitoring phase for 2017. Those patients who survived at least 1 year since the diagnosis of a recurrence or new primary colon cancer were recategorised into the treatment for recurrence/second cancer phase (requiring either curative or palliative management). Those who died sooner after diagnosis after recurrence or new primary colon cancer were considered to be in the last year of life care phase.
Although over time, each patient can contribute to more than one phase of care; at any one specific point in time, a patient can only be in one phase of care.
Estimation of type and number of services required
Data on patterns of treatment, including surgery alone and surgery plus chemotherapy, from the NSW Colorectal Cancer Care Survey [11] were used to estimate the future cancer care needs for colon cancer patients. The survey is population-wide and covered all first primary incident colorectal cancer cases reported to the NSW Central Cancer Registry between February 1, 2000 and January 31, 2001 in NSW. The type and number of services that will be required in the future was estimated by applying the proportions of patients receiving each type of treatment observed in this survey [11] to the estimated numbers of patients in the initial care phase. In addition to these treatment estimates, it is possible that patients in the last year of life may also require surgery and/or chemotherapy, and patients with recurrence or second primary colon cancer will also need some treatment. Unfortunately, however, we cannot identify the patients who need such treatment from the patterns of care survey data as they were beyond the scope of the survey.
Results
Incidence trends
A total of 66,821 cases of first primary colon cancer were included in this analysis, with similar numbers of males (33,488) and females (33,333). Over the period of 1972–2007, the numbers of incident cases with first primary colon cancer increased for both males and females in NSW, and PIAMOD predicted that this trend would continue over the next 10 years up to 2017 (Fig. 2). Figure 2 also suggests that our incidence model, particularly for females, fitted the observed data well, which is important because the prevalence predictions are based on modelled incidence and survival trends. The PIAMOD software provides a measure of uncertainty (95 % confidence interval) for the predicted incidence for the period for which observed data are available but does not provide this measure for the period beyond the observed data. This increase in the number of incident cases was primarily due to the growth and ageing of the population, indicated by the generally stable age-standardised incidence rates for colon cancer in NSW over the last 15 years (http://www.statistics.cancerinstitute.org.au/prodout/trends/trends_incid_C18_extall_NSW.htm).
Survival trends
The survival trends were very similar for males and females, with 5-year relative survival increasing from 1972–1977 to 2002–2007, from 40 to 67 % for males and 41 to 67 % for females. These increasing trends were estimated to continue into the foreseeable future. Figure 3 shows the survival trends for those aged 55–64 years (observed versus predicted), and it suggests that the mixture cure models fitted the observed data very well.
Comparison of the modelled survival with life table estimates for the period 1984–1995 also indicated that the models were a very good fit for the two younger age groups, but yielded a slight (but not significant) underestimate for the oldest age group (Fig. 4).
Projected prevalence
Based on our estimates, there were 17,375 patients aged 18–84 years who had a past diagnosis of first primary colon cancer in NSW in 2007. As expected from the observed trends in incidence and survival over time, this number is estimated to have increased to 22,671 (an increase of 30.5 %) by 2017. The increase in the number of prevalent cases was the greatest for those aged 65–74 years with an almost 50 % increase from 2007 to 2017, followed by the oldest age group and then the youngest age group (Table 1). The effect of population ageing was also reflected in Table 1. The youngest age group made up about 29 % of the total prevalent cases in 2007, but this proportion had decreased to 25 % by 2017, while the proportion of prevalent cases aged 65–74 years increased from 33 to 38 % for males and from 30 to 35 % for females over the same period.
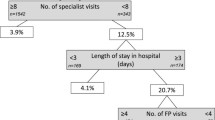
Type and number of services required
The expected numbers of patients requiring different levels of health care in 2017 are shown in Table 2. About 83 % of these prevalent cases with colon cancer will be either in the post-treatment monitoring phase (36.3 %) or will be in the long-term survivors (46.5 %). Of these prevalent cases, over 10 % will require initial care.
Based on the proportions of colon cancer patients receiving surgery and chemotherapy in the NSW Colorectal Cancer Care survey, we estimated that in 2017, there will be at least 1,303 men and 1,127 women in NSW requiring initial surgery for colon cancer, as shown in Table 3. Of these, 404 men and 349 women will also require adjuvant chemotherapy.
Care for recurrence or second colon cancer
Among 66,821 patients diagnosed with first primary colon cancer between 1972 and 2007, 8,554 cases (12.8 %) had recurrence or developed metastatic disease (to end of 2007), 43 % (3726) of which occurred during 2000–2007. The average annual number of recurrences in 2000–2007 was 466. Among these recently diagnosed recurrences, 50 % died within 12 months of diagnosis, while the remainder (233) would have required therapy for recurrence. The average annual number represented 7.0 % of those in the post-treatment monitoring phase in 2007.
In addition, 3,555 cases (5.3 %) had either a second tumour or a second primary colon cancer, with 45 % (1,601) of these occurring during 2000–2007. Thus, the average annual number of patients being diagnosed with second colon cancers in 2000–2007 was 200. In patients with second colon cancers, 12 % died within 12 months of diagnosis of their second colon cancer, whereas the remainder (176) would have required active treatment. The average annual number represented 3.0 % of those in the post-treatment monitoring phase in 2007.
Applying these two proportions (7.0 and 3.0 %) to the predicted number (8,767) of cases in the post-treatment monitoring phase in 2017 results in a predicted 614 recurrences and 263 cases with second colon cancers. Because 50 % of recurrent cases and 88 % of patients diagnosed with a second colon cancer are predicted to survive at least 1 year after diagnosis of these events, the estimated numbers of cases requiring treatment for recurrence or second colon cancer for 2017 will be 307 and 231, respectively (Table 2).
Validation of the prevalence model
As shown in Fig. 5, there was good agreement between the model and the counting method for estimates of prevalence (for males) in 2007 at 0–5 years and 20–35 years of follow-up, but between 5 and 20 years, the estimates from PIAMOD were lower than those from the counting method. From our previous experience, we know that death matching with the registry records is usually higher in the first 5 years after diagnosis, which probably explains the good level of agreement between the modelled and counting methods in the first 5 years of follow-up. The reasons for the good agreement after 20 years follow-up may be because older prevalent cases were excluded from follow-up once they reached 85 years of age, and because some of the prevalent cases were censored at the end of the study (2007). Thus, we believe that the underestimate of prevalence in the period 5 to 20 years after diagnosis may be due to incomplete death matching for prevalent cancer cases in this interval. The patterns for females were similar (results not shown).
Discussion
We have described a method for estimating future numbers of people at different stages of their cancer journey, with a view towards general application in providing evidence-based guidance for health service planning. Over the coming decades, both the numbers of new cancer cases and patients’ years of life living with cancer will increase significantly in most developed countries [1, 3, 17–20], and as a consequence, demand for cancer health services will rise substantially. The method described here could be a useful tool in planning for this, as it divides the patient population into relatively homogeneous groups in terms of the required level of cancer care, and thus provides a more accurate and complete estimate of future health service needs for cancer patients than methods which predict only the overall cancer prevalence. Our method is a direct extension of those used in previous studies [2, 4], but addresses some of their limitations [2, 4], and was validated using historical data to compare the estimated with the observed prevalence. Therefore, the information it produces is an important supplement to existing incidence and mortality data, and will be essential for ensuring that future cancer patients have adequate access to the different types of care that may be required.
Dividing the prevalent population into clinically relevant phases of care is a step forward in the use of existing population-based data to provide useful information about the future health service needs for patients at different stages of their cancer journey [2, 4, 17, 18, 21–23]. Studies from Europe [4, 17] and the USA [2, 18] have also looked into ways to systematically calculate or project care prevalence by dividing the total cancer prevalence into clinically relevant phases of care. Using data from the European cancer registries, Gatta et al. [4] apportioned the total prevalence of colon cancer into the following phases of care: initial care, intensive follow-up, non-intensive follow-up and the terminal phase. With a similar method and using SEER data with information on time after diagnosis, Mariotto et al. [2] divided the total prevalent colorectal cancer patients into three phases of care as follows: initial care, end-of-life care and monitoring care. As the monitoring phase included patients with a range of cancer care needs, this broad categorizations may over- or underestimate the proportion of patients who require active medical treatment. To distinguish the different health care needs for patients in the monitoring phase of care, data on recurrence and second cancers are needed, as well as an estimate of the number of patients who were cured of their cancer. Gatta et al. [4] addressed these two concerns in their study by applying ‘cure’ models to their data and collecting recurrence data. However, their estimate of the prevalence of recurrent cases in Europe was based on data collected in a single year (1990) from a local Italian cancer registry, which was then extrapolated to data from the European cancer registries, and may therefore not be entirely reliable.
In an attempt to provide a more complete and meaningful assessment of the impact on cancer resources [20, 24–26], we extended Mariotto’s approach in three ways. First, we split the continued monitoring phase into those who are long-term survivors and those requiring post-treatment monitoring. By introducing the phase for long-term survivors, we effectively separated patients who need close monitoring after initial treatment from those who require only minimal cancer care. We found that about 46 % of patients living with colon cancer were effectively cured of their cancer, so their need for colon cancer care should be minimal [18], although care for late or lasting effects of cancer treatment may still be needed, and their psychosocial needs may be higher than the general population.
Second, we used data on recurrence and occurrence of multiple primary colon cancers to refine the proportion of patients who require additional active treatment after initial treatment. It is important to include these groups of patients when estimating future health service needs for colon cancer because they will have a large impact on the required cancer care. It is known that about 10 to 50 % of patients with surgically treated colon cancer will have a recurrence [7, 27–30], and a considerable proportion (4.5–10 %) will develop a second primary at some stage after their initial diagnosis and treatment [5, 28]. Our results were in line with these previously reported findings, with about 13 % of patients previously diagnosed with primary colon cancer having a recurrence or developing metastatic disease, and 5 % being diagnosed with a second tumour or a second primary colon cancer. Regarding the care needs for these patients, it was estimated that 409 cases (with either recurrence or second colon cancer) would have had therapy for these events in 2007, and this number is expected to increase to 538 in 2017. The real number of recurrences is probably even greater if you consider the issue of incomplete episode data that we have identified in another study [31]. Thus, ignoring these two groups of patients in the estimation of care needs will significantly underestimate the need for active treatment. Similar to a previous study [7], we found that most recurrences (over 90 %) happened in the first 5 years after diagnosis, which suggests that after 5 years from initial diagnosis, focus should be shifted to long-term adverse effects of adjuvant therapy or second cancers. Therefore, we believe that estimates that combine all this information will be more complete and accurate in predicting cancer care requirements.
Third, we included patterns of care data from the same population, allowing us to specify the type and amount of treatment required for colon cancer patients in NSW. This study was population-based and covered the same population as the other data used, including incidence and recurrence data. The strengths of the survey included a very high participation rate—data were received for more than 90 % of eligible patients, and the high quality of the self-reported data from the treating practitioners [32], which made the results from this survey representative of the whole population. While it would be desirable to have more recent data on the patterns of care for colon cancer, we believe that the use of data from the early 2000s does not make our study less useful, as the primary focus has been to illustrate the methods proposed.
Cancer prevalence is a complex product of many factors. It is challenging to completely separate the contribution of each of these factors in projecting cancer prevalence, as it is not simply an additive relationship. Nevertheless, we conducted a sensitivity analysis to begin to investigate the sensitivity of the projected prevalence to different factors. In this sensitivity analysis, we tried to separate the effect of population growth and ageing from that of changes in incidence and survival on the increase in the number of prevalent cases of colon cancer in 2017. We applied the age-specific prevalence rates in 2007 to the projected age-specific population in 2017 (Table 4), yielding a total of 21,135 survivors of colon cancer for 2017. This suggests that, of the projected increase in prevalence (5,296 cases) from 2007 to 2017, about 71 % (3,760 cases) will be due to population growth and ageing, while the remaining 29 % may be attributable to changes in incidence and survival between 2007 and 2017. However, we would emphasise here that it is extremely difficult to accurately isolate the effect of individual factors, and the results of this sensitivity analysis only provide a rough indication of the contribution of each of these variables.
In line with the results from Europe and the US, our estimates indicate that there will be a great increase in demand for health care for colon cancer in NSW over the next few years, as the number of patients living with colon cancer is predicted to increase by over 30 % in the 10 years from 2007 to 2017. Moreover, these estimates are likely to be underestimated (as shown in Fig. 5), especially for patients requiring post-treatment monitoring and long-term survivors. Actually, this may be an even larger problem than we predicted for two reasons. First, cancer care needs are likely to be doubled in the near future due to the introduction of new anticancer therapies [20], while in our modelling, we assumed that the care needs for cancer patients in the future will be the same as they were in the early 2000s. Second, our estimates did not include the number of patients with second or later primary colon cancers of different cancer types, and this number is likely to be larger than the number with multiple colon cancers where the site is the same [33]. In addition to those who had initial care and treatment for recurrence, some patients with short survival after diagnosis, who we have included in the last year of life care phase, would receive surgery and/or chemotherapy. Unfortunately, however, we have no way of identifying the number of patients in the last year of life phase from the survey data available to us. This means that our results will underestimate the numbers and types of services required to treat colon cancer patients in 2017. It is also likely that we have underestimated the number of patients in the last year of life phase because some deaths from unknown causes may in fact be due to colon cancer, which then means there may be an even larger number of cases in the last year of life that will require treatment for colon cancer.
With an increasing number of people being diagnosed, treated and living as a cancer survivor, planning of sufficient services to meet their healthcare needs is vital in providing optimal care. Recent studies [24, 25] suggest that if this problem is not dealt with now, there will be an acute shortage of medical oncologists to care for cancer patients in the US in the near future, and a similar shortage of cancer care professionals is evident in Australia [26]. Indeed, the consequences of not providing appropriate cancer care for individuals diagnosed with cancer are already being felt [34], and the shortfall in the oncology workforce could threaten the quality of patient care and safety [35]. Therefore, it is necessary for the health systems to be ready to supply sufficient numbers of relevant medical specialists and services to ensure that those patients living with cancer have adequate access to the different types of care required throughout the phases of their disease. The method described here should be a useful tool for health service planners facing this problem. This method can be applied to the data from other jurisdictions, so that they may develop their own estimates, plan for their local needs, develop health service goals and have a means of tracking progress towards them.
We chose to illustrate these methods using colon cancer data because all the required registry data were available, much is known about survival patterns for the disease, and we had access to detailed information regarding treatment patterns. These methods can, however, be applied to other cancer types, although each will need to be treated as a separate model, and not all these data are required for all major cancers. For instance, it is rare to have a second primary or multiple tumours for prostate cancer, thus only data on recurrent disease would be needed when estimating care needs for those who are in the post-treatment monitoring phase.
It is likely that in many instances, some of the data required to estimate the future care requirements using these methods will not be available, but there are several ways in which this difficulty may be overcome. For example, where cancer registries do not routinely collect data on cancer recurrence, literature on recurrence rates for the cancer type under study may be used as a proxy to estimate the proportion of patients in the post-treatment monitoring phase who will at some stage need further active treatment. Also, for populations where patterns of treatment are unknown, literature on major treatment types and the proportions of patients who would be suitable for each type could be used. The PIAMOD software and the SAS code for fitting mixture cure models can be obtained by requesting one copy from the developer at no charge. (http://www.eurocare.it/MiamodPiamod/tabid/60/Default.aspx#courses). This website also provides some related supporting documents and references.
While this study and the methods proposed have many strengths, including the high quality of the registry data, and the unique aspects of the use of recurrence and treatment data to more accurately predict cancer care requirements, there are some limitations which must be considered, if the method is to be applied to data from other jurisdictions. First, the PIAMOD software has substantial data demands (requiring detailed, specially-formatted input data that includes externally modelled survival estimates). Second, the process involves many decisions to be made, such as selecting a high-dimensional polynomial incidence model and mixture cure model for relative survival based on different assumptions for future trends. All of these decisions must be informed by a high level of cancer epidemiological and statistical knowledge, and the resulting prevalence estimates are highly dependent on these modelling decisions and assumptions. Third, as a consequence, there are some uncertainties in the projected prevalence, but the PIAMOD software does not provide measures of uncertainty for projections of relative survival, population size and mortality. This could be due to issues with uncertainty in further assumptions for the projections. The use of bootstrapping with PIAMOD warrants further investigation and may be an area for further development. Fourth, a mixture of cure models may not be appropriate for some cancer types (for example, female breast cancer) or for some subgroups of the patient population [36]. Finally, the continuum from initial diagnosis and treatment, from post-treatment monitoring to end of life care, is oversimplified. Although the phases of care categorization used here is useful, the processes are not so discrete, and some of them are cross-cutting, so that there are many different possible paths cancer patients may experience from diagnosis to survival or end of life.
Conclusion
Cancer incidence and survival will increase over the coming decades, resulting in a substantial increase in the number of patients living with cancer in most developed countries. Thus, the successful planning and development of a healthcare system able to respond to this increased demand will be required, if people who will live with cancer for the remainder of their lives are to have positive health outcomes. Our proposed methods can provide evidence-based guidance for health service planners and policy makers faced with this challenge.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Mariotto AB, Yabroff KR, Feuer EJ, De Angelis R, Brown M. Projecting the number of patients with colorectal carcinoma by phases of care in the US: 2000–2020. Cancer Causes Control. 2006;17:1215–26.
Capocaccia R, Colonna M, Corazziari I, et al. Measuring cancer prevalence in Europe: the EUROPREVAL project. Ann Oncol. 2002;13:831–9.
Gatta G, Capocaccia R, Berrino F, Ruzza MR, Contiero P. Colon cancer prevalence and estimation of differing care needs of colon cancer patients. Ann Oncol. 2004;15:1136–42.
Hayat MJ, Howlader N, Reichman ME, Edwards BK. Cancer statistics, trends and multiple primary cancer analyses from the surveillance, epidemiology and end results (SEER) programme. Oncologist. 2007;12:20–37.
Brawley OW, Ankerst DP, Thompson IM. Screening for prostate cancer. CA Cancer J Clin. 2009;59:264–73.
Scheer A, Auer RA. Surveillance after curative resection of colorectal cancer. Clin Colonrectal Surg. 2009;22:242–50.
Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365:1687–717.
Yabroff KR, Warren JL, Schrag D, et al. Comparison of approaches for estimating incidence costs of care for colorectal cancer patients. Med Care. 2009;47:S56–63.
Fritz A, Percy C, Jack A, et al., editors. International classification of diseases for oncology. 3rd ed. Geneva, Switzerland: World Health Organisation; 2000.
Armstrong K, O’Connell DL, Leong D, Spigelman A, Armstrong BK. The New South Wales colorectal cancer care survey—Part 1 surgical management. Sydney: Cancer Council New South Wales; 2004.
Verdecchia A, De Angelis G, Capocaccia R. Estimation and projections of cancer prevalence from cancer registry data. Stat Med. 2002;21:3511–26.
Ederer F, Axtell LM, Cutler SJ. The relative survival rate: a statistical methodology. Natl Cancer Inst Monogr. 1961;6:101–21.
Verdecchia A, De Angelis R, Capocaccia R, et al. The cure for colon cancer: results from the EUROCARE study. Int J Cancer. 1998;77:322–9.
Krogh V, Micheli A. Measure of cancer prevalence with a computerised programme: an example on larynx cancer. Tumori. 1996;82:287–90.
Gail MH, Kessler L, Midthune D, Scoppa S. Two approaches for estimating disease prevalence from population-based registries of incidence and total mortality. Biometrics. 1999;55:1137–44.
Chauvenet M, Lepage C, Jooste V, Cottet V, Faivre J, Bouvier AM. Prevalence of patients with colorectal cancer requiring follow-up or active treatment. Eur J Cancer. 2009;45:1460–5.
Mariotto A, Warren JL, Knopf KB, Feuer EJ. The prevalence of patients with colorectal carcinoma under care in the US. Cancer. 2003;98:1253–61.
Quon H, Loblaw A, Nam R. Dramatic increase in prostate cancer cases by 2021. BJU Int. 2011;108:1734–8.
Shulman LN, Jacobs LA, Greenfield S, et al. Cancer care and cancer survivorship care in the United States: will we be able to care for these patients in the future? J Oncol Pract. 2009;5:119–23.
Baili P, Hoekstra-Weebers J, Van Hoof E, et al. Cancer rehabilitation indicators for Europe. Eur J Cancer. 2013;49:1356–64.
Baili P, Vicentini M, Tumino R, et al. A method for differentiating cancer prevalence according to health status, exemplified using a population-based sample of Italian colorectal cancer cases. Acta Oncol. 2013;52:294–302.
Maddams J, Utley M, Moller H. Levels of acute health service use among cancer survivors in the United Kingdom. Eur J Cancer. 2011;47:2211–20.
Warren JL, Mariotto AB, Meekins A, Topor M, Brown ML. Current and future utilisation of services from medical oncologists. J Clin Oncol. 2008;26:3242–7.
Erikson C, Salsberg E, Forte G, Bruinooge S, Goldstein M. Future supply and demand for oncologists: challenges to assuring access to oncology services. J Oncol Pract. 2007;3:79–86.
Scott IA. Health care workforce crisis in Australia: too few or too disabled? Med J Aust. 2009;190:689–92.
Tjandra JJ, Chan MK. Follow-up after curative resection of colorectal cancer: a meta-analysis. Dis Colon Rectum. 2007;50:1783–99.
Cluze C, Delafosse P, Seigneurin A, Colonna M. Incidence of second cancer within 5 years of diagnosis of a breast, prostate or colorectal cancer: a population-based study. Eur J Cancer Prev. 2009;18:343–8.
O’Connell MJ, Campbell ME, Goldberg RM, et al. Survival following recurrence in stage II and III colon cancer: findings from the ACCENT data set. J Clin Oncol. 2008;26:2336–41.
Rodriguez-Moranta F, Salo J, Arcusa A, et al. Postoperative surveillance in patients with colorectal cancer who have undergone curative resection: a prospective, multicenter, randomised, controlled trial. J Clin Oncol. 2006;24:386–93.
Clements MS, Roder DM, Yu XQ, Egger S, O’Connell DL. Estimating prevalence of distant metastatic breast cancer: a means of filling a data gap. Cancer Causes Control. 2012;23:1625–34.
Young JM, Leong DC, Armstrong K, et al. Concordance with national guidelines for colorectal cancer care in New South Wales: a population-based patterns of care study. Med J Aust. 2007;186:292–5.
Mariotto AB, Rowland JH, Ries LA, Scoppa S, Feuer EJ. Multiple cancer prevalence: a growing challenge in long-term survivorship. Cancer Epidemiol Biomarkers Prev. 2007;16:566–71.
Maher EJ, Makin W. Life after cancer treatment—a spectrum of chronic survivorship conditions. Clin Oncol (R Coll Radiol). 2007;19:743–5.
Levit L, Smith AP, Benz EJ, Ferrell B. Ensuring quality cancer care through the oncology workforce. J Oncol Pract. 2010;6:7–11.
Lambert PC. Modelling of the cure fraction in survival studies. Stata J. 2007;7:351–75.
Acknowledgments
We would like to thank the NSW Colorectal Cancer Care survey for providing the treatment data, and the NSW Central Cancer Registry for providing the incidence data for this study. The registry is managed by the Cancer Institute NSW under an agreement with the NSW Ministry of Health. We also thank Qingwei Luo for assistance with producing the graphs and verifying the results, Clare Kahn for editorial assistance, and the two reviewers for the constructive suggestions and insightful comments which, we believe have led to significant improvements in the manuscript. Xue Qin Yu is supported by a National Health & Medical Research Council Training Fellowship (ref 550002), and Mark Clements is supported by Cancerfonden and the Swedish eScience Research Centre.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yu, X.Q., Clements, M. & O’Connell, D. Projections of cancer prevalence by phase of care: a potential tool for planning future health service needs. J Cancer Surviv 7, 641–651 (2013). https://doi.org/10.1007/s11764-013-0303-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-013-0303-9