Abstract
Introduction
As children complete cancer treatment and enter survivorship, follow-up care is critical to monitor for and treat relapses, secondary malignancies, and late effects of treatment. Relative contributions of cancer and treatment variables and sociodemographic factors in engagement with follow-up care are not fully understood. This study aimed to identify risk factors for inadequate follow-up care.
Methods
The sample included a cohort of 173 children (birth–18 years) diagnosed with cancer in 2004 and treated at a children’s hospital. Sociodemographics (gender, patient current age, ethnic minority status, distance from hospital, type of insurance), cancer and treatment variables (patient age at diagnosis, type of cancer, treatment modality, time off treatment, relapse, on clinical trial protocol), and follow-up care through 2009 were gathered via the hospital tumor registry and medical charts.
Results
In simultaneous linear regression analysis (full model: F(12, 160) = 3.49, R 2 = 0.21, p = 0.001), having a liquid tumor (p < 0.05), presence of relapse (p = 0.009), and shorter distance from hospital (p = 0.006) predicted total number of follow-up visits between completion of treatment and 5 years post-diagnosis. In simultaneous logistic regression analysis (full model: χ 2 (12, N = 173) = 53.27, p < 0.001), being male (p = 0.077), having a brain tumor (p = 0.055), longer time off treatment (p = 0.004), and greater distance from hospital (p = 0.003) decreased the likelihood of completing a follow-up or survivorship visit between completion of treatment and 5 years post-diagnosis. In simultaneous linear regression analysis (full model: F(12, 160) = 4.52, R 2 = 0.25, p = 0.001), non-White race (p = 0.001) and having public insurance (p = 0.002) predicted total number of no shows between completion of treatment and 5 years post-diagnosis.
Discussion/conclusions
These results extend knowledge of health disparities in pediatric cancer follow-up care suggesting that cancer and treatment-related variables (type of cancer, relapse, number of treatment modalities) and sociodemographic factors (distance from treatment center, non-White race, public insurance) are important predictors of engagement in follow-up care.
Implications for cancer survivors
Survivors at risk for poor engagement may benefit from targeted interventions designed to increase likelihood of follow-up care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood cancer survivors are at risk for a variety of late effects associated with cancer and its treatment, including secondary malignancies and endocrine, cardiovascular, and cognitive dysfunction [1]. In fact, more than 70% of childhood cancer survivors will develop a chronic medical condition in their lifetime [2, 3]. The Institute of Medicine considers it imperative for all survivors to continue follow-up care to monitor and treat late effects, address secondary and tertiary prevention strategies, and manage chronic conditions [4]. However, the Childhood Cancer Survivor Study (CCSS) reported only 42% of survivors attended a cancer-related medical appointment in the last 2 years, suggesting the majority of survivors are not receiving the recommended risk-based care [5].
Reasons for this lack of engagement in follow-up care are still unclear, but health disparities may be a contributing factor. In fact, the Director of the National Cancer Institute’s (NCI) Office of Cancer Survivorship noted certain cultural and sociodemographic factors may lead to disparities in cancer survivorship and encouraged future research efforts that examine the causes and consequences of these disparities [6]. The NCI’s Overcome Cancer Health Disparities Strategic Plan aims to identify factors contributing to disparities, develop culturally sensitive approaches to address these disparities, and disseminate interventions across the cancer control continuum [7].
Although the significance of examining health disparities is clear, assessment of health disparities among pediatric cancer populations is a growing area of research, especially among long-term survivors. Findings from the CCSS have revealed that survivors of older age, of African-American race, and those who lacked adequate health insurance were less likely to receive risk-based, survivor-focused care [8]. However, minority status was not shown to relate to adverse health outcomes [9]. Similarly, Klosky and colleagues [10] observed that older age, non-White race, and insufficient medical insurance as well as lower socioeconomic status, traveling by car, and living closer to clinic were associated with missed survivorship clinic appointments. Moreover, longer time since diagnosis has also been documented as a barrier to consultations with an oncologist or other healthcare practitioners [11], and reduced access to follow-up oncology care has been identified for adolescent and young adult survivors of cancer compared to children currently on treatment for cancer [9, 11, 12].
The current study aimed to clarify findings regarding relative roles of cancer and treatment variables and sociodemographic factors in follow-up care after the completion of treatment for childhood cancer. Knowing how these factors contribute to engagement in oncology follow-up care is important for identifying children and families who may not be receiving follow-up care essential to monitoring for and treating relapses, secondary malignancies, and late effects of treatment and for addressing related disparities in care. Consistent with NIH’s commitment to research regarding multilevel (biologic, individual, social, and institutional/social policies) determinants of health disparities (i.e., The National Institutes of Health-sponsored Centers for Population Health and Health Disparities [13]), this study evaluated factors that contribute to follow-up care within a cohort of pediatric cancer patients diagnosed in 2004, specifically examining the individual, societal, and population level factors. We expected that cancer and treatment variables (shorter time since diagnosis, more intensive treatment, relapse, and treatment on a clinical trial protocol) would be associated with better engagement in follow-up after the completion of treatment and up to 5 years post-diagnosis. Alternatively, sociodemographic variables (younger age, race, farther distance from hospital, and public insurance) would be associated with less engagement in follow-up visits. Factors that contribute to no shows to follow-up visits after the completion of treatment and up to 5 years post-diagnosis, defined as instances in which patient/family did not arrive for a scheduled follow-up visit and did not call to reschedule follow-up on the day of the scheduled visit, were also examined as an indicator of lack of engagement.
Methods
Sample
A cohort of 259 pediatric patients diagnosed with cancer in 2004 and treated at The Children’s Hospital of Philadelphia (CHOP) were identified through the hospital tumor registry. After excluding 86 patients due to death prior to 2009 (n = 35), never on active treatment (n = 11), never disease-free (n = 8), lost to follow-up before completing treatment (n = 9), and diagnosed at CHOP but followed elsewhere (n = 23), the final sample included 173 patients. Patients were diagnosed with a broad range of malignancies. See Table 1 for a description of variables included in analysis.
Measures
Cancer and treatment variables
Age at diagnosis (in years), type of cancer (leukemia/lymphoma, solid tumors other than brain tumors, brain tumors), number of treatment modalities (surgery, chemotherapy, radiation, stem cell transplantation), length of time off treatment (in years), relapse, and whether or not patient was treated on a clinical trial were abstracted from the tumor registry and medical chart review.
Sociodemographic variables
Information regarding patients’ gender, current age (in years), race (White, non-White), distance from hospital in 2009 (in kilometers), and insurance in 2009 (private, public) was identified in the hospital tumor registry and medical chart.
Follow-up care variables
Based on medical chart review, we calculated: (1) total number of follow-up visits at our oncology clinic from the completion of treatment to 5 years post-diagnosis and (2) whether or not patient was seen for an off treatment follow-up or survivorship visit when off treatment for at least 2 and around 5 years post-diagnosis (any visit occurring at or after 4.5 years post-diagnosis). We also calculated total number of no shows for follow-up appointments (i.e., instances in which patient/family did not arrive for a scheduled follow-up visit and did not call to reschedule follow-up on the day of the scheduled visit) from the completion of treatment to 5 years post-diagnosis.
Procedures
Using the hospital tumor registry and retrospective medical chart review, information on cancer and treatment, sociodemographic, and follow-up variables was abstracted by two research assistants trained to identify target variables. Data were documented on a file review sheet and then entered into an Excel database. Research assistants’ questions regarding diagnosis, treatment, or follow-up were discussed with the authors to improve accuracy of information. The study protocol was approved by the CHOP Institutional Review Board (IRB). The CHOP IRB also granted a waiver of informed consent due to the retrospective nature of the data collection.
Statistical analyses
As a first step, data were reviewed to examine distributions and describe frequencies/means as appropriate. Dichotomous variables were coded as follows: 0 = no relapse, 1 = relapse; 0 = not on a clinical trial, 1 = on a clinical trial; 0 = male, 1 = female; 0 = white, 1 = non-White; and 0 = private insurance, 1 = public insurance, and solid tumors and brain tumors were compared to leukemia/lymphoma using two variables. Because the range of geographical distance was large (3.50–3773.80 km), distance from hospital was re-coded into a dichotomous variable based on median distance (0 = within 57.60 km of the hospital, 1 = farther than 57.60 km from the hospital).
Simultaneous regressions were employed as we aimed to examine the relative contribution of each of the independent variables to predicting engagement in follow-up care. Simultaneous linear regression analysis, entering all cancer, treatment, and sociodemographic variables of interest, was conducted to predict the total number of follow-up visits after completion of treatment up to 5 years post-diagnosis and for total no shows during the same time period. In addition to full model statistics, standardized regression weights (β) and their associated statistical test are reported for each independent variable. Simultaneous logistic regression was used to evaluate predictors of attending an off treatment follow-up or survivorship visit at 5 years after diagnosis. Reference variables were leukemia/lymphoma, no relapse, not treated on clinical trial, male, White, less distance from hospital, and private insurance. Full model statistics as well as the odds ratio and associated confidence interval for each independent variable are reported. Statistical significance was defined as a p value < 0.05, but information on variables with p < 0.10 was also highlighted. Power was adequate for the proposed regression analyses based on sample size and number of predictor variables in each regression [14].
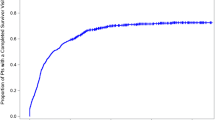
Results
In the simultaneous linear regression analysis predicting total number of follow-up visits off treatment, the full model was significant [F(12, 160) = 3.49, R 2 = 0.21, p < 0.001] with type of cancer, number of treatment modalities, relapse, and distance from hospital making significant contributions to the variance (see Table 2). Patients with solid tumors and brain tumors attended fewer follow-up visits off treatment than did patients with leukemia/lymphoma (β = −0.29, p = 0.006) for solid tumors (β = −0.23, p = 0.010) for brain tumors. Patients who experienced a relapse (β = 0.21, p = 0.009) attended more follow-up visits, and those who lived farther away from the hospital (β = −0.21, p = 0.006) attended fewer follow-up visits off treatment. Number of treatment modalities showed a trend to significance (β = 0.15, p = 0.073) in that more treatment modalities were associated with more follow-up visits off treatment. For further illustration, Figs. 1, 2, 3, and 4 depict change in the total number of follow-up visits over time for each significant predictor.
In the simultaneous logistic regression analysis predicting any off treatment follow-up or survivorship visit 5 years post-diagnosis, the full model was significant (χ 2 (12, N = 173) = 53.27, p < 0.001) with type of cancer, length of time off treatment, gender, and distance from hospital emerging as predictors (see Table 3). Patients with brain tumors were less likely to attend a follow-up or survivorship visit compared to patients with leukemia/lymphoma (odds ratio (OR) = 0.24, p = 0.055). Patients who were off treatment for a longer period of time were about half as likely to attend a follow-up or survivorship visit as those more recently off treatment (OR = 0.44, p = 0.004). Patients who lived farther than 57.6 km of the hospital were less likely to attend a follow-up or survivorship visit as patients who lived closer (OR = 0.24, p = 0.003). Females were also twice as likely as males to attend a follow-up or survivorship clinic visit 5 years post-diagnosis (OR = 2.20, p = 0.077).
In the simultaneous linear regression analysis for total number of no shows after completion of treatment and up to 5 years post-diagnosis, the full model was significant [F(12, 160) = 4.52, R 2 = 0.25, p < 0.001] with total number of treatment modalities, ethnicity, and type of insurance making significant independent contributions (see Table 4). Patients of ethnic minority status (β = 0.27, p = 0.001) and those with public insurance (β = 0.25, p = 0.002) had more no shows. Also, patients who were treated with a higher number of treatment modalities (β = 0.14, p = 0.085) had more no shows.
Discussion
The critical role of follow-up care for childhood cancer survivors is well-established [15]. Yet, engaging survivors of cancer in follow-up health care has proved challenging. Within this cohort, 25% of patients who completed treatment for cancer were not seen for care in our clinics between the end of treatment and 5 years post-diagnosis. Emerging studies predicting follow-up cancer care report a number of barriers to engagement including sociodemographic variables (age, ethnicity, distance from hospital) and treatment variables (time off treatment). Our findings confirm the important contribution of sociodemographic factors, particularly non-White race, greater distance from the hospital, male gender, and public insurance as risk factors for reduced engagement in follow-up care. Cancer and treatment variables were replicated as important contributors to greater engagement in follow-up care.
These findings expand understanding of cancer and treatment-related variables associated with risk for insufficient follow-up care, allowing for the targeting of efforts to maintain engagement in care to particular subgroups of children and adolescents with cancer. Specifically, results of this study highlight the importance of type of cancer (leukemia/lymphoma), experience of relapse, and more complicated treatment regimens for greater engagement in follow-up care. For example, relapse of childhood cancer is associated with extended treatment and more late effects [16]. Phipps and colleagues [17, 18] documented that relapsed survivors of childhood cancer and their parents were more likely to develop posttraumatic stress symptoms than survivors of childhood cancer who had not relapsed. It is then likely that children who survive cancer after relapse and their parents may already experience health problems requiring follow-up, are more educated about possible late effects, have greater worry about subsequent relapse or second cancers, and are more integrated into their health care clinics.
Of concern, however, is that the greater length of time off treatment the less likely survivors were to attend a follow-up visit 5 years post-diagnosis, although we do not know if survivors accessed care in other settings. Also, although patients with more complex treatment regimens presented for greater follow-up visits, those with cancers such as brain tumors or treatments (stem cell transplant) associated with late effects were not more likely to engage in follow-up care nor were survivors treated on clinical trials for whom we might expect clearly established protocols for follow-up care. It is important to keep in mind, however, that variation in standard recommendations for frequency of follow-up visits across types of cancer may explain the findings of this study regarding leukemia/lymphoma versus other types of cancer. That is, patients with leukemia/lymphoma, for whom frequent follow-up is recommended particularly as they initially move off treatment, had higher rates of follow-up visits than those with solid tumors or brain tumors for whom recommended follow-up is more widely spaced. Also, more scheduled follow-up visits may result in greater appointment attendance but also more rescheduling or missed appointments/no shows.
Findings regarding the contribution of sociodemographic variables are consistent with the current literature. The model proposed by Warnecke and colleagues [13] for the National Institutes of Health-sponsored Centers for Population Health and Health Disparities provides a workable framework for our findings regarding sociodemographics in its presentation of individual, social, and population/societal factors that explain health disparities. Consistent with this model, individual demographic risk factors of non-White race, social/environmental factors of distance from the hospital, and the societal factor of type of insurance were linked to level of engagement in follow-up care. The finding that females are more likely than males to attend a follow-up or survivorship visit 5 years post-diagnosis is novel. The average age of our sample was almost 14 years old in 2009 with many patients in this sample being adolescents or young adults. It is possible that males who were treated have similar risk for poor health behaviors as the general population of adolescents and young adults, for which males are less likely to have health insurance and engage in the healthcare system [19].
Analysis of total number of no shows to follow-up appointments is particularly interesting in that no shows suggest inconsistent engagement in follow-up care. Non-White race and public insurance were the primary significant predictors of no shows (in addition to living close to the hospital and higher total number of treatment modalities). This result is consistent with other findings regarding insurance, which are mixed but generally suggest that although having insurance increases access, it does not eliminate disparities in health care [20]. It is also important to note that all participants in this study had health insurance, which has not been demonstrated in other studies of childhood cancer survivors [21, 22]. Klosky and colleagues noted that those who live closer to the hospital are more likely to miss clinic appointments [10]. In contrast, our analyses suggested that living farther away from the hospital was associated with fewer no shows but also fewer follow-up visits in general. It may be that those who live farther away put greater effort into clearing their schedules for a follow-up clinic visit but schedule fewer return visits to our tertiary care center. Patient and families who live closer to the hospital feel a greater ease in missing appointments and rescheduling later.
Based on these findings, at risk pediatric patients and their families may be targeted for educational and supportive interventions as they complete treatment to increase engagement in critical follow-up care. Patients and families may benefit from a host of specific preventive interventions designed to increase likelihood of follow-up care (e.g., targeted doctor–patient communication, help overcoming barriers to coming to clinic such as transportation, education about long-term risks). One suggested intervention is the use of an educational brochure, but no studies to date have examined the acceptability, feasibility, or effectiveness of this type of intervention in improving attendance of follow-up visits [23, 24]. However, one study demonstrated the use of an educational booklet and treatment summary led to an increase in survivors’ willingness to change their behavior and their self-efficacy, which may be associated with more positive attitudes regarding follow-up care [25].
Survivorship clinics provide specialized, coordinated, multidisciplinary care focused on screening for and treatment of medical, cognitive, and psychosocial late effects of cancer and its treatment. The number of survivors seen in survivorship clinic in this cohort of patients diagnosed with cancer in 2004 was under 50% of the sample so that analysis of variables that contribute to follow-up in survivorship clinic could not be reliably achieved. Efforts to enhance engagement will necessitate commitment of health care providers to the process of communication about follow-up care, ensuring health care access, and providing supportive interventions for the anxiety associated with return to clinic [26]. Extending this endeavor, evaluation of strategies for successfully referring patients into survivorship clinics is required. Some suggested, but not empirically tested, strategies include tailoring follow-up visit guidelines by treatment modality [27], scheduling follow-up visits before patients leave clinic and sending postcard reminders about upcoming appointments [28], and partnering with oncologists who participated in patients’ care during active treatment to contact them after a missed survivorship appointment [10].
In the current study, individual, social, and societal level variables contributed to follow-up care. This study utilized retrospective data from the tumor registry and medical charts; prospective, multisite studies may be required to more accurately identify relevant variables that contribute to engagement in follow-up care after completion of treatment. Findings from these studies may inform development of interventions to ensure that health disparities in pediatric cancer follow-up care are minimized and that patients and families remain active participants in risk-based follow-up care following cancer treatment.
References
Oeffinger KC, Hudson MM. Long-term complications following childhood and adolescent cancer: foundations for providing risk-based health care for survivors. CA Cancer J Clin. 2004;54:208–36.
Geenen MM, Cardous-Ubbink MC, Kremer LC, et al. Medical assessment of adverse health outcomes in long-term survivors of childhood cancer. JAMA. 2007;297:2705–15. doi:10.1001/jama.297.24.2705.
Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows MT, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355:1572–82. doi:10.1056/NEJMsa060185.
Hewitt M, Weiner SL, Simone JV. Childhood cancer survivorship: improving care and quality of life. Washington, DC: National Academies; 2003.
Oeffinger KC, Mertens AC, Hudson MM, Gurney JG, Casillas J, Chen H, et al. Health care of young adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Ann Fam Med. 2004;2:61–70. doi:10.1370/afm.26.
National Cancer Institute. A conversation with Julia Rowland. National Cancer Bulletin 2006; 3(40): 7. Available from: http://www.cancer.gov/aboutnci/ncicancerbulletin/archive/2006/101706
National Cancer Institute. The NCI strategic plan for leading the nation: to eliminate the suffering and death due to cancer. Washington, DC: National Institutes of Health; 2006. 76 p. NIH Publication No.: 06-5773.
Nathan PC, Greenberg ML, Ness KK, Hudson MM, Mertens AC, Mahoney MC, et al. Medical care in long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2008;26:4401–9. doi:10.1200/JCO.2008.16.9607.
Castellino SM, Casillas J, Hudson MM, Mertens AC, Whitton J, Brooks SL, et al. Minority adult survivors of childhood cancer: a comparison of long term outcomes, health care utilization, and health-related behaviors from the Childhood Cancer Survivor Study. J Clin Oncol. 2005;23:6499–507. doi:10.1200/JCO.2005.11.098.
Klosky JL, Cash DK, Buscemi J, Lensing S, Garces-Webb DM, Zhao W, et al. Factors influencing long-term follow-up clinic attendance among survivors of childhood cancer. J of Cancer Surviv. 2008;2:225–32. doi:10.1007/s11764-008-0063-0.
Shaw AK, Pogany L, Speechley KN, Maunsell E, Barrera M, Mery LS. Use of health care services by survivors of childhood and adolescent cancer in Canada. Cancer. 2006;106:1829–37. doi:10.1002/cncr.21798.
Thompson K, Palmer S, Dyson G. Adolescents and young adults: issues in transition from active therapy into follow-up care. Eur J of Oncol Nurs. 2009;13:207–12. doi:10.1016/j.ejon.2009.05.001.
Warnecke RB, Oh A, Breen N, Gehlert S, Paskett E, Tucker KL, et al. Approaching health disparities from a population perspective: the National Institutes of Health Centers for Population Health and Health Disparities. Am J Public Health. 2008;98:1608–15. doi:10.2105/AJPH.2006.102525.
Knofczynski GT, Mundfrom D. Sample sizes when using multiple linear regression for prediction. Educ Psychol Meas. 2008;68:431–42. doi:10.1177/0013164751407310131.
Bhatia S, Meadows AT. Long-term follow-up of childhood cancer survivors: future directions for clinical care and research. Pediatr Blood Cancer. 2006;46:143–8. doi:10.1002/pbc.20613.
Hudson MM, Mertens AC, Yasui Y, Hobbie W, Chen H, Gurney JG, et al. Health status of adult long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. JAMA. 2003;290:1583–92. doi:10.1001/jama.290.12.1583.
Phipps S, Jurbergs N, Long A. Symptoms of post-traumatic stress in children with cancer: does personality trump health status? Psychooncology. 2009;18:992–1002. doi:10.1002/pon.1496.
Jurbergs N, Long A, Ticona L, Phipps S. Symptoms of post-traumatic stress in parents of children with cancer: are they elevated relative to parents of healthy children? J Pediatr Psychol. 2009;34:4–13. doi:10.1093/jpepsy/jsm119.
National Adolescent Health Information Center. A health profile of adolescent and young adult males 2005. San Francisco: Author, University of California, San Francisco; 2005.
Lille-Blanton M, Paradise J, Thomas M, Stewart SL. Racial/ethnic disparities in access to care among children: how does Medicaid do in closing the gaps? Washington, DC: The Henry J Kaiser Family Foundation; 2009. 18 p. Report No.: 8031.
Martin S, Ulrich C, Munsell M, Taylor S, Lange G, Bleyer A. Delays in cancer diagnosis in underinsured young adults and older adolescents. Oncologist. 2007;12:816–24. doi:10.1634/theoncologist.12-7-816.
Park ER, Li FP, Liu Y, Emmons KM, Ablin A, Robison LL, et al. Health insurance coverage in survivors of childhood cancer: the Childhood Cancer Survivor Study. J Clin Oncol. 2005;23:9187–97. doi:10.1200/JCO.2005.01.7418.
Duffey-Lind EC, O’Holleran E, Healey M, Vettese M, Diller L, Park ER. Transitioning to survivorship: a pilot study. J Pediatr Oncol Nurs. 2006;23:335–43. doi:10.1177/1043454206293267.
Hobbie WL, Ogle SK, Reilly M, Ginsberg JG, Rourke M, Ratcliffe S, et al. Identifying the educational needs for parents at the completion of their child’s cancer therapy. J Pediatr Oncol Nurs. 2010;27:190–5. doi:10.1177/1043454209360778.
Eiser C, Hill JJ, Blacklay A. Surviving cancer: what does it mean for you? An evaluation of a clinic based intervention for survivors of childhood cancer. Psychooncology. 2000;9:214–20.
Ginsberg JP, Hobbie WL, Carlson CA, Meadows AT. Delivering long-term follow-up care to pediatric cancer survivors: transitional care issues. Pediatr Blood Cancer. 2006;46:169–73. doi:10.1002/pbc.20610.
Wallace WHB, Blacklay A, Eiser C, Davies H, Hawkins M, Levitt GA, et al. Developing strategies for long term follow up of survivors of childhood cancer. BMJ. 2001;323:271–4.
Johnson R, Horne B, Feltbower RG, Bulter GE, Glaser AW. Hospital attendance patterns in long term survivors of cancer. Arch Dis Child. 2004;89:374–7. doi:10.1136/adc.2002.021816.
Acknowledgments
The authors would like to thank Karole Collier for her assistance in completing the medical record reviews.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barakat, L.P., Schwartz, L.A., Szabo, M.M. et al. Factors that contribute to post-treatment follow-up care for survivors of childhood cancer. J Cancer Surviv 6, 155–162 (2012). https://doi.org/10.1007/s11764-011-0206-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-011-0206-6