Abstract
Introduction
Despite proven benefits of regular physical activity, estimates indicate that few cancer survivors meet physical activity guidelines. The purpose of this paper is to identify and compare exercise barriers among cancer survivors, both cross-sectionally and longitudinally as they undergo home-based behavioral interventions.
Methods
Data on a sample of 452 breast and prostate cancer survivors who completed the FRESH START trial were analyzed collectively, as well as separately by cancer type.
Results
More total barriers (3.5 vs. 2.4; p < 0.01) were reported among breast cancer survivors compared with prostate cancer survivors. Commonly reported baseline exercise barriers among both groups were “too busy” (breast, 52% and prostate, 45%) and “no willpower” (breast, 51% and prostate, 44%). At baseline, breast cancer survivors who reported “no willpower” also reported 18.7 fewer minutes of physical activity compared with those not reporting this barrier (p < 0.01). Among prostate cancer survivors, this difference was 39.5 min (p < 0.01). Change in barriers was not associated with change in minutes of physical activity from baseline to post-intervention in either cancer survivor group.
Conclusions
This is the largest study evaluating barriers and physical activity over time among cancer survivors. There are similarities and differences that both need to be taken into consideration when promoting physical activity among subgroups of survivors.
Implications for cancer survivors
Knowledge concerning barriers associated with reported physical activity may be helpful in designing optimally targeted physical activity interventions among breast and prostate cancer survivors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 1.5 million Americans are diagnosed with cancer annually [1]. Breast and prostate cancers are among the most commonly diagnosed malignancies among women and men, and 5-year survival rates for both early stage cancers now exceed 90% [1, 2]. Among a roughly 12 million cancer survivors in the USA, the largest segment is composed of these two cancer subtypes.
Cancer survivors face many physical and emotional challenges throughout their treatment and recovery. Participation in physical activity has been suggested to reduce undesirable sequelae associated with diagnosis and treatment and to reduce comorbidities [3]. Physical activity has been shown to improve quality of life, vitality, self-esteem, and physical functioning among cancer survivors [4–7].
The American Cancer Society recommends at least 150 min/week of moderate-to-vigorous physical activity among adult cancer survivors [8]. However, the percent of survivors meeting these guidelines is reportedly as low as 29.6% [9]. Thus, more research is necessary to understand barriers to being physically active in this growing population. An understanding of the specific factors limiting physical activity in cancer survivors will help in designing effective interventions to ultimately reduce cancer recurrence and comorbidities in this population [10, 11].
Previous investigations report the following exercise barriers among cancer survivors: lack of time and enjoyment, treatment side effects, and fatigue [12–14]. Investigations have generally been cross sectional and have focused on breast cancer survivors. Less is known about barriers in other cancer survivors and how these barriers change during recovery and over the course of intervention.
The primary research aims of this study were to: (1) identify and compare baseline exercise barriers among breast and prostate cancer survivors, (2) evaluate the association between baseline barriers and levels of physical activity in both groups, and (3) identify the change in exercise barriers and reported physical activity longitudinally in response to a home-based physical activity intervention. Based on strong gender-related differences in the practice of physical activity [15], it was hypothesized that breast cancer survivors (women) would report more barriers and less physical activity compared with prostate cancer survivors (men). It was also hypothesized that these exercise barriers would decrease among participants in the tailored intervention arm compared with the attention control arm of FRESH START.
Methods
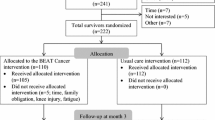
Secondary data analyses were conducted using baseline and 1-year follow-up data from participants who enrolled and completed FRESH START, a home-based randomized controlled trial to promote physical activity and a healthy diet among cancer survivors. This trial had two arms: a tailored intervention, which distributed sequentially tailored diet and exercise materials based on participant’s characteristics, and an attention control, which distributed (nontailored) standardized diet and exercise brochures. Participants in the tailored intervention arm received two of the following three intervention modules: increasing fruit and vegetable consumption, restricting total and saturated fats, and/or increasing physical activity. Within the exercise intervention module, participants received mailed newsletters that provided information on how to overcome their specific exercise barriers. At 1-year follow-up, more participants in the tailored intervention arm significantly reported practicing two or more goal behaviors (≥150 min/week of exercise, consumption of ≥5 daily servings of fruits and vegetables, or consumption of a low-fat diet) compared with the attention control arm [16]. Other details of the original study and main outcomes have been described previously [16, 17]. The Duke University Medical Center’s Institutional Review Board approved this trial conducted from July 2002 to October 2005.
Sample
FRESH START recruited cancer survivors from several cancer registries and oncologic practices throughout North America. Participants provided written consent and were screened for eligibility; criteria included the following: (1) diagnosis of locoregionally staged prostate or female breast cancer within the past 9 months, (2) free of conditions limiting adherence to physical activity (congestive heart failure, recent myocardial infarction, severe breathing difficulties, mobility problems, kidney failure, and progressive cancer), (3) English speaking/writing, and (4) not engaging in two of three goal behaviors (i.e., ≥150 min/week of exercise, consumption of ≥5 daily servings of fruits and vegetables, or consumption of a low-fat diet). The study sample resided in 39 US states and two Canadian provinces. The current analyses included participants who (1) received standardized (attention control arm) or exercise intervention materials (72 excluded) and (2) completed baseline and 1-year measures (an additional 19 excluded; N = 452).
Exercise barriers
Exercise barriers were assessed by telephone interview using a checklist which included 14 personal, social, and environmental barriers previously reported in the literature to be associated with physical inactivity in survivors or the general population [12–14]. Individuals were asked to respond affirmatively if the barrier applied to them or negatively if it did not (yes/no). Barrier change was calculated as either one whose barriers decreased from baseline to 1 year versus one whose number of barriers increased or remained the same.
Minutes of physical activity
Minutes of physical activity were assessed by telephone interview using the 7-day physical activity recall (PAR), a validated instrument with proven reliability [18]. Participants reported their occupational and leisure activity (in minutes) during the previous week. Previous analyses in a subsample of FRESH START participants observed a moderate association between the subjective 7-day PAR and an objective measure of the RT3 triaxial accelerometer [19].
Covariates
Information was collected on participants’ age, race, education, body mass index (BMI), number of comorbidities (Older Americans Resources and Services scale) [20], cancer stage, treatment modality, cancer coping style (mini-mental adjustment to cancer) [21], and stage of readiness to exercise (transtheoretical model outlined by Prochaska et al.) [22]. These variables were obtained at baseline through cancer registries and self-reported responses from telephone surveys.
Statistical analysis
Because cancer site was confounded by gender, and several differences in reported barriers were observed between cancer sites, the analyses were stratified by site (breast and prostate). When appropriate, demographic and clinical characteristics among breast and prostate cancer survivors were compared using t tests and Chi-square tests. Chi-square tests were used to compare barriers between survivor groups. t tests were used to compare minutes of physical activity among those reporting and not reporting specific exercise barriers at baseline. The number of participants who reported change in barriers from baseline to 1 year (decrease vs. increase or same) was calculated. Intervention assignment and barrier change were assessed using a Chi-square test. A t test was used to evaluate the association between barrier change and change in minutes of physical activity from baseline to 1 year. Given the exploratory nature of this study, no modifications were made for multiple comparisons; thus, all significance levels were set at p < 0.05 (two-sided tests).
Results
From the original FRESH START sample of 543, the current sample of 452 participants was composed of 259 breast cancer survivors and 193 prostate cancer survivors. The current sample did not differ statistically from those excluded with respect to age, BMI, number of comorbidities, race, cancer stage, education, cancer coping style, treatment, or stage of readiness for exercise.
Participant characteristics
Table 1 presents characteristics of this study sample. At baseline, prostate cancer survivors reported more minutes of physical activity, were significantly older, included fewer racial-ethnic minorities, and had higher proportions reporting a fatalist coping style and precontemplative exercise stages of readiness than breast cancer participants.
Baseline exercise barriers among breast and prostate cancer survivors
The top three exercise barriers reported among both groups of survivors were “too busy,” “no willpower,” and “don’t like to exercise in bad weather” (Fig. 1). “Too busy” was the leading barrier reported among both breast and prostate cancer survivors (breast, 52% and prostate, 45%). Barriers reported less frequently included “nowhere to exercise” and “worry about injury.”
Overall, more breast cancer survivors endorsed each exercise barrier compared with prostate cancer survivors and also reported more total barriers (3.5 vs. 2.4, p < 0.01). There were significant differences between survivor groups for seven individual barriers (Fig. 1).
Associations between baseline barriers and minutes of physical activity
Table 2 compares the average minutes of physical activity for participants who did and did not report specific exercise barriers at baseline. Among breast cancer survivors, participants who reported the barriers of “no one to exercise with,” “nowhere to do it,” “not sure about what to do,” “don’t want to get sore,” “don’t enjoy it,” “don’t like to sweat,” and “no willpower” reported significantly fewer minutes of physical activity than those who did not report these barriers. Among prostate cancer survivors, differences in physical activity were observed in the barriers “no access to gym or exercise equipment,” “not sure about what to do,” “worry about injury,” “don’t like to sweat,” and “no willpower.”
Changes in exercise barriers and physical activity throughout the intervention period
Overall, 37% of breast and 36% of prostate cancer survivors reduced barriers from baseline to 1-year follow-up. Intervention assignment was associated with barrier change among prostate cancer survivors, with 42% in the attention control arm reducing barriers, compared with 25% in the tailored intervention arm (p = 0.02). Among breast cancer survivors, those whose number of exercise barriers were reduced (regardless of what intervention arm they were assigned to) reported an increase of 91 min of activity from baseline to 1 year, compared with an increase of 68 min among those who reported the same number or increased barriers (this was a nonsignificant increase between barrier change groups, p = 0.19) (Fig. 2). Among prostate cancer survivors, those whose barriers were reduced from baseline to 1 year increased minutes by 43, compared with an increase of 33 min among those who reported the same number or increased in number of barriers (p = 0.64).
Discussion
This study is the first to characterize and compare exercise barriers in both breast and prostate cancer survivors who participated in a home-based physical activity intervention. It provides much needed information about the type of barriers reported by these two prevalent survivor groups and their association with levels of physical activity, as well as changes in physical activity that occur longitudinally in response to a home-based intervention.
Compared with prostate cancer survivors, breast cancer survivors reported more barriers, and consistently greater endorsement of each individual barrier. However, both breast and prostate cancer survivors had similar rankings of their top three barriers (too busy; no willpower; and don’t like to exercise in bad weather). “Too busy” has been reported as a major exercise barrier among samples of head and neck (30%), breast cancer (73%), and colorectal cancer patients (32%) [12, 14, 23]. Lack of willpower and issues with weather also have been reported as substantial exercise barriers in both cancer and noncancer samples [24–27].
More breast as compared with prostate cancer survivors responded affirmatively to each barrier. Given that breast cancer survivors tended to be middle-aged or older women, this finding could be attributed to social norms against exercise and perceptions that it is unfeminine. Also, women may cite lack of time as a reason for limiting activity based on family and caregiving responsibilities [28, 29]. Another possibility is that women may more readily divulge barriers and health-related information than men.
Several different exercise barriers were associated with baseline levels of physical activity in the two survivor groups, three of which were significant (not sure about what to do, don’t like to sweat, and no willpower). No willpower was also one of the most commonly reported exercise barriers among both survivor groups, suggesting that this is an important barrier to address in future interventions. This may be difficult though, as “no willpower” is a fairly abstract internal construct and it may be difficult to measurably increase willpower in individuals. Instead, a successful intervention strategy may be to intervene on barriers associated with activity such as “not sure what to do,” as this is more tangible and participants can be educated on a variety of exercises and activities, and how to perform them. The most commonly reported barrier, “too busy,” was not associated with minutes of baseline physical activity, suggesting that time constraints are an acknowledged barrier among those who are sedentary, but that lack of time is also perceived and felt to influence exercise behavior even among those who exercise regularly.
Approximately 36–37% percent of breast and prostate cancer survivors, respectively, reduced their exercise barriers from baseline to 1 year. Interestingly, intervention assignment was associated with barrier change among prostate cancer survivors but in the opposite direction of our hypothesis. Fewer individuals in the tailored intervention arm, as compared with the attention control arm reduced exercise barriers over time. Previous studies have also reported this counterintuitive finding and posit that those who continue to be the most active over time have increased awareness of symptoms and side effects [30, 31].
Gains in reported physical activity were observed in both survivor groups regardless of barrier change direction. Thus, this suggests that a possible consequence of physical activity interventions is an actual increase in exercise barriers. Physical activity interventions are likely to have a mix of participants, including those, who, after reducing barriers will increase activity, as well as those who after increasing activity, will report more exercise barriers. The important message from this analysis is that at any snapshot in time, exercise barriers appear to influence activity levels, and they are different according to cancer type and, or gender. Those who report certain barriers typically report less activity. However, in the setting of a physical activity intervention, increasing activity may actually lead to higher reporting of exercise barriers.
Strengths and limitations
The primary limitations of this study are as follows: (1) participants in FRESH START may have had greater motivation to adopt healthy behaviors compared with the overall survivor population; (2) the majority of measures were based on self report, and the psychometric properties of the barriers checklist are unknown; and (3) this trial was not powered for this secondary analysis. These limitations are mitigated by the fact that the response and retention rates of FRESH START were excellent (42% and 8%, respectively), the barriers checklist was composed of a compendium of items that have been validated in other studies, and self report of exercise was validated via accelerometry [19]. In addition, given the fact that FRESH START was one of the largest lifestyle interventions ever conducted among a diverse sample of cancer survivors, our power to detect differences and associations is better than in most studies conducted to date. Furthermore, given the wide geographic distribution of FRESH START, these findings have the potential to generalize to a broader population and evaluates barriers at the time of participation, thereby reducing recall bias, and assesses changes in exercise barriers prospectively which few studies have done. Thus, this study provides important data where a current void exists.
Conclusions
Breast cancer survivors consistently reported a greater number of exercise barriers compared with prostate cancer survivors. Several exercise barriers were significantly inversely associated with reported physical activity at baseline; however, the overall change in barriers was not associated with physical activity change throughout the FRESH START trial. In addition to knowledge gained from this study, future longitudinal research is still needed to investigate these ideas: (1) further explore differences between cancer types, as well as gender differences in regards to exercise barriers and (2) explore the combination of exercise barriers that may act synergistically to impact physical activity.
References
American Cancer Society. Cancer Facts & Figures 2010. Atlanta: American Cancer Society; 2010. Available at: http://www.cancer.org/acs/groups/content/@nho/documents/document/acspc-024113.pdf.
SEER Cancer Statistics Review. Age-adjusted SEER incidence and U.S. death rates and 5-year relative survival rates by primary cancer site, sex and time period (Table 1.4). National Cancer Institute; 1975–2003. Available at: http://seer.cancer.gov/csr/1975_2006/results_merged/topic_survival.pdf.
Alfano CM, Rowland JH. Recovery issues in cancer survivorship: a new challenge for supportive care. Cancer J. 2006;12(5):432–43.
McNeely ML, Campbell KL, Rowe BH, et al. Effects of exercise on breast cancer patients and survivors: a systematic review and meta-analysis. CMAJ. 2006;175(1):34–41.
Pinto BM, Frierson GM, Rabin C, et al. Home-based physical activity intervention for breast cancer patients. J Clin Oncol. 2005;23(15):3577–87.
Thorsen L, Courneya KS, Stevinson C, et al. A systematic review of physical activity in prostate cancer survivors: outcomes, prevalence, and determinants. Support Care Cancer. 2008;16(9):987–97.
Segal RJ, Reid RD, Courneya KS, et al. Resistance exercise in men receiving androgen deprivation therapy for prostate cancer. J Clin Oncol. 2003;21(9):1653–9.
Doyle C, Kushi LH, Byers T, et al. Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA Cancer J Clin. 2006;56:323–53.
Bellizzi KM, Rowland JH, Jeffery DD, et al. Health behaviors of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol. 2005;23(34):8884–93.
Holmes MD, Chen WY, Feskanich D, Kroenke CH, Colditz GA. Physical activity and survival after breast cancer diagnosis. JAMA. 2005;293:2479–86.
Meyerhardt JA, Heseltine D, Niedzwiecki D, Hollis D, Saltz LB, Mayer RJ, et al. Impact of physical activity on cancer recurrence and survival in patients with stage III colon cancer: findings from CALGB 89803. J Clin Oncol. 2006;24(22):3535–41.
Rogers LQ, Courneya KS, Robbins KT, et al. Physical activity correlates and barriers in head and neck cancer patients. Support Care Cancer. 2008;16(1):19–27.
Satia JA, Walsh JF, Pruthi RS. Health behavior changes in white and African American prostate cancer survivors. Cancer Nurs. 2009;32(2):107–17.
Leddy SK. Incentives and barriers to exercise in women with a history of breast cancer. Oncol Nurs Forum. 1997;24:885–90.
Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults' participation in physical activity: review and update. Med Sci Sports Exerc. 2002;34(12):1996–2001.
Demark-Wahnefried W, Clipp EC, Lipkus IM, et al. Main outcomes of the FRESH START trial: a sequentially tailored, diet and exercise mailed print intervention among breast and prostate cancer survivors. J Clin Oncol. 2007;25(19):2709–18.
Demark-Wahnefried W, Clipp EC, McBride C, et al. Design of FRESH START: a randomized trial of exercise and diet among cancer survivors. Med Sci Sports Exerc. 2003;35(3):415–24.
Blair SN, Haskell WL, Ho P, Paffenbarger Jr RS, Vranizan KM, Farquhar JW, et al. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1985;122(5):794–804.
Sloane R, Snyder DC, Demark-Wahnefried W, et al. Comparing the 7-day physical activity recall with a triaxial accelerometer for measuring time in exercise. Med Sci Sports Exerc. 2009;41(6):1334–40.
Fillenbaum GG. Multidimensional Functional Assessment of Older Adults. Hillsdale: Lawrence Erlbaum Associates; 1988.
Watson MM, Law M, dos Santos M, et al. The mini-MAC further development of the mental adjustment to cancer scale. J Psychosoc Oncol. 1994;12(3):33–45.
Prochaska JO, Velicer WF, Rossi JS, et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychol. 1994;13(1):39–46.
Courneya KS, Friedenreich CM, Quinney HA, Fields AL, Jones Lee W, Vallance JK, et al. A longitudinal study of exercise barriers in colorectal cancer survivors participating in a randomized controlled trial. Annals Behav Med. 2005;29:147–53.
Clark DO. Identifying psychological, physiological, and environmental barriers and facilitators to exercise among older low income adults. J Clin Geropsychol. 1999;5(1):51–62.
Mancuso CA, Sayles W, Robbins L, et al. Barriers and facilitators to healthy physical activity in asthma patients. J Asthma. 2006;43(2):137–43.
Sánchez ZV, Cashion AK, Cowan PA, et al. Perceived barriers and facilitators to physical activity in kidney transplant recipients. Prog Transplant. 2007;17(4):324–31.
Rye JA, Rye SL, Tessaro I, et al. Perceived barriers to physical activity according to stage of change and body mass index in the west virginia wisewomen population. Women’s Health Issues. 2009;19(2):126–34.
Artazcoz L, Borrell C, Benach J. Gender inequalities in health among workers: the relation with family demands. J Epidemiol Community Health. 2001;55(9):639–47.
Verhoef MJ, Love EJ, Rose MS. Women's social roles and their exercise participation. Women Health. 1992;19(4):15–29.
Lynch B, Owen N, Hawkes A, et al. Perceived barriers to physical activity for colorectal cancer survivors. Support Care Cancer. 2010;18(6):729–34.
Dawson J, Hillsdon M, Boller I, Foster C. Perceived barriers to walking in the neighbourhood environment and change in physical activity levels over 12 months. Br J Sports Med. 2007;41(9):562–8.
Acknowledgments
The original FRESH START trial was supported by grants R01 CA81191, CA74000, CA63782, and M01-RR-30 from the National Institutes of Health and also by the American Institute of Cancer Research and the Susan G. Komen Foundation. This material is the result of work supported with resources and the use of facilities at the Durham VA medical center. The authors declare no financial disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ottenbacher, A.J., Day, R.S., Taylor, W.C. et al. Exercise among breast and prostate cancer survivors—what are their barriers?. J Cancer Surviv 5, 413–419 (2011). https://doi.org/10.1007/s11764-011-0184-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-011-0184-8